Abstract
Background
One practice in healthcare implementation is patient engagement in quality improvement and systems redesign. Implementers in healthcare systems include clinical leadership, middle managers, quality improvement personnel, and others facilitating changes or adoption of new interventions. Patients provide input into different aspects of health research. However, there is little attention to involve patients in implementing interventions, especially in the United States (U.S.), and this might be essential to reduce inequities. Implementers need clear strategies to overcome challenges, and might be able to learn from countries outside the U.S.
Methods
We wanted to understand existing work about how patients are being included in implementation activities in real world U.S. healthcare settings. We conducted an environmental scan of three data sources: webinars, published articles, and interviews with implementers who engaged patients in implementation activities in U.S. healthcare settings. We extracted, categorized, and triangulated from data sources the key activities, recurring challenges, and promising solutions using a coding template.
Results
We found 27 examples of patient engagement in U.S. healthcare implementation across four webinars, 11 published articles, and seven interviews, mostly arranging patient engagement through groups and arranging processes for patients that changed how engaged they were able to be. Participants rarely specified if they were engaging a population experiencing healthcare inequities. Participants described eight recurring challenges; the two most frequently identified were: (1) recruiting patients representative of those served in the healthcare system; and (2) ensuring processes for equitable communication among all. We matched recurring challenges to promising solutions, such as logistic solutions on how to arrange meetings to enhance engagement or training in inclusivity and power-sharing.
Conclusion
We clarified how some U.S. implementers are engaging patients in healthcare implementation activities using less and more intensive engagement. It was unclear whether reducing inequities was a goal. Patient engagement in redesigning U.S. healthcare service delivery appears similar to or less intense than in countries with more robust infrastructure for this, such as Canada and the United Kingdom. Challenges were common across jurisdictions, including retaining patients in the design/delivery of implementation activities. Implementers in any region can learn from those in other places.
Similar content being viewed by others
Background
One emerging practice within implementation science is to engage patients or consumers of health care in implementing changes, system redesign, or quality improvement to ensure healthcare service delivery is more patient-centered [1]. Currently, patients provide input into different aspects of health research. As examples, patients make invaluable contributions to developing interventions, designing participant study recruitment approaches, and disseminating findings [2, 3]. However, there has been little attention on how to involve patients or the public in the process of implementing interventions in healthcare systems. It is possible patient engagement in design/delivery of implementation might result in strategies targeting an increase in patient buy-in or demand for certain interventions, which is one hypothesized mechanism to reduce health care inequities. Tailoring interventions or implementation for local context—which patients can help guide as end users with lived experience—might be another essential mechanism to reducing healthcare inequities, and ignoring their potential contributions might exacerbate disparities [4].
Research on engaging patients in implementation activities in the U.S. is known as patient engagement in design/delivery of implementation, quality improvement, and systems redesign, [5] participatory implementation science, [6] or community-engaged dissemination and implementation [1]. For the present analysis, we are not using the phrase patient engagement to refer to patient activation in their own health care, although it is possible that patient engagement in implementation might lead to strategies focused on patient activation. Implementers in healthcare systems can include clinical leadership, middle managers, quality improvement personnel, or other people facilitating changes or adoption of new interventions.
Although implementers can use multilevel strategies to increase adoption of interventions among providers, clinics, and healthcare systems (e.g., training providers, changing physical infrastructure), [7] engaging patients in implementation activities is currently rare. Implementers can engage patients in implementation activities in many ways [8]. A consensus process with implementation experts highlighted five categories of patient engagement in implementation activities: (1) involve patients/family members in implementation efforts; (2) intervene with patients to enhance uptake and adherence; (3) prepare patients to be active participants in their care (akin to “patient activation”); (4) increase demand among patients, so they ask for the intervention; and (5) use mass media to spread awareness of the intervention [9]. The expert panel suggested activities for including patients in the pre-implementation phase or training them in the intervention or how to advocate for it. Other suggestions were to increase awareness to enhance patient demand for the intervention (e.g., what pharmaceutical companies do) and prepare them to ask questions about their individual care, thus increasing pressure for adoption of the intervention.
In the U.S., despite increasing requirements by payers and organizations to engage patients in implementation or quality improvement, [10,11,12] the practice appears to be uncommon [13, 14]. Other countries, such as Canada and the United Kingdom (U.K.), have longer histories of “patient and public involvement” in healthcare implementation activities, supported by funding, personnel, training, and expectations to do so in their healthcare systems [15,16,17,18,19,20]. Yet, for U.S. settings, little detail is published on these strategies, and there are few well-documented examples in routine healthcare service delivery, despite the unique economic, political, regulatory, and social contexts of U.S. health care [19,20,21,22]. We need greater detail on how patients are engaged in implementation activities in U.S. healthcare systems, common challenges, and ways implementers overcome those challenges.
Limited work on this topic in the U.S. shows preliminary benefits, yet patient engagement in implementing routine healthcare service delivery is not adequately supported across the nation’s healthcare systems. For example, early work showcasing patient engagement in implementation activities has resulted in patient-centered systems redesign in healthcare settings, [23] greater uptake of effective interventions in community settings, [24] including those experiencing health care disparities in access and utilization, [25] improved patient health, [25] and increased sustainment of interventions [26]. Proposed mechanisms from early work suggest that the aforementioned outcomes improve due to increasing relevance or fit of interventions and implementation strategies to real-world settings, using patient-driven solutions to challenges, and/or building the capacity of all involved for implementation and sustainment [27]. Similarly, the Patient-Centered Outcomes Research Institute (PCORI) in the U.S. funds implementation research that engages patients and other end users but does not fund sustained implementation efforts directly in healthcare systems. The U.S. Agency for Healthcare Research and Quality produces some guidance on one specific strategy (e.g., patient advisory councils), [28] yet, does do not provide funding for these activities in U.S. healthcare systems.
We also lack enough details or standards of optimal patient engagement in implementation activities in the U.S., limiting the knowledge other implementers could use in their efforts [22]. It is unclear whether implementers in U.S. healthcare settings face similar challenges or can enact similar solutions as those in other countries. As a first step to developing an approach to engaging patients in healthcare implementation activities, we piloted an environmental scan methodology derived from business literature. As described in Methods, we reviewed or “scanned” three data sources meeting industry standards for health services research. We also documented details of what, how, and in what contexts implementers engaged patients in implementation activities [29] in U.S. healthcare settings, describing challenges and solutions.
Methods
Design and procedures
Environmental scanning originated in the business field to document trends to assist in data-driven planning [30, 31]. We applied this approach to patient engagement in implementation in healthcare contexts. The goal of this approach is not to produce a comprehensive understanding but to capture a snapshot of trends through a variety of data. Our environmental scan also illustrates which cases focused on healthcare disparities or inequities. The conduct of the scan required openness, the anticipation of new gaps, and a willingness to revise existing knowledge based on the data reviewed [32]. This study is under regulation by the Central Arkansas Veterans Healthcare System Institutional Review Board, which deemed it not human subjects research. Thus, participants interviewed were not formally consented, but before deciding whether to participate, they were apprised of the study’s rationale and told the information they provided would be de-identified in dissemination.
Inclusion and exclusion criteria
We set the following a priori inclusion criteria for all data sources in this scan: (1) patients were engaged in implementation, service delivery, systems redesign, or quality improvement of an intervention, and could be engaged in dissemination if it was used as an implementation strategy; (2) the focus of the implementation effort was a health condition; (3) service delivery was conducted partially or completely in a U.S. healthcare setting; and (4) the study or activity used descriptive, qualitative, quantitative, or mixed-methods research. A case was excluded if the focus was: (1) patient engagement only in research, not implementation; (2) patient engagement in direct care that may only result in changes for one individual’s health; (3) guideline or instrument development, theoretical or conceptual articles, literature review, or protocol papers; or (4) outside the U.S.
Data sources
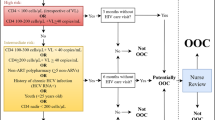
We captured data from three data sources for this environmental scan. We systematically searched existing and recent databases for published literature (rather than conducting a new systematic review) and webinars and interviewed implementers individually or observed them in a workgroup setting (i.e., interview participants). We completed our first round of data collection in 2018–2019 and updated literature and webinar searches in 2022. Figure 1 describes our systematic search and recruitment process.
Literature
We drew from two existing databases of articles: The PCORI Health Research Literature Explorer [33] and the Implementation Facilitation Literature Collection created by the VHA Behavioral Health Quality Enhancement Research Initiative [34]. Both databases were collections of articles populated using (1) systematic review methods, i.e., they applied a rigorously developed search strategy using a wide variety of search terms including keywords and MeSH terms; (2) applied the search in industry-standard, indexed search engines (i.e., PubMed/MEDLINE, CINAHL, and Thompson Scientific Web of Science); and (3) conducted a two-stage screening process applying relevant inclusion and exclusion criteria [33, 34]. Thus, instead of conducting a new systematic review, we relied on two databases that feature results of systematic review methods (i.e., articles). Then, within each database, we narrowed our search for articles more closely to our inclusion criteria—patient engagement (i.e., PCORI database) or changes in healthcare service delivery (i.e., Implementation Facilitation database). We imported selected articles into a systematic review software [35].
Updated through May 2021, the PCORI database contained literature focused on patient engagement in health research [33]. We searched for articles under the categories “dissemination” or “translation” phases of research, then under the categories “patients” and/or “caregivers” for patient involvement, and screened all titles and abstracts for patient engagement in healthcare implementation activities.
The second database was produced through a systematic review by Ritchie and colleagues [34] of peer-reviewed articles on Implementation Facilitation, an implementation strategy that includes relationship building, interactive problem solving, and other participatory approaches for supporting change. This database contained literature in any context (including outside VHA) from 1996 to 2020. We chose to use this Implementation Facilitation literature database because it aligned with our scan’s focus on making changes in healthcare service delivery or implementation in clinical care instead of only research studies. We searched and screened every abstract and title for patient engagement without narrowing by search terms.
Webinars
We searched webinars from the U.S. Veterans Health Administration (VHA) Health Services Research and Development archive, as this is the only database we identified of webinars with examples of implementation or changes in U.S. healthcare service delivery. We systematically searched these terms in webinar titles archived from the earliest possible date (January 1, 2016) through May 24, 2022:
-
1)
“patient”, “user”, “client”, “patient”, “veteran”, “caregiver”, “partner”, OR “family” AND
-
2)
“engag*”, “participat*”, “involv*”, OR “consult*”.
Interview Participants
We recruited implementers as interview participants—healthcare professionals who engaged patients in design/delivery of implementation activities and facilitated change in healthcare service delivery. To recruit a convenience sample, we distributed a flyer via email invitation sent to U.S. professional organizations with an implementation science affiliation (e.g., Implementation Research Institute, Mentored Training for Dissemination and Implementation in Cancer) and conducted outreach through Twitter. We engaged potential participants in snowball sampling, asking them to suggest other candidates for participation [36]. Through this approach, we contacted three workgroups we were alerted to by potential participants. After one round of interviews and analysis, we had not saturated results. Thus, we conducted a second round until we interviewed enough participants to saturate results [37].
Based on participant preference, we sent an electronic survey with open-ended text boxes for self-administration or conducted 45-minute telephone interviews with the same questions. As described in Additional file 1, questions included: “What structures or tools or practices have you used to do this work? What are some problems you encountered in engaging consumers in implementation? How did you solve them?” In one case, we were able to observe a workgroup of participants and coders used the same questions as in the survey/interview and populated responses into a coding template.
Data extraction using a coding template
We extracted and categorized data from all sources using a coding template informed by two theoretical frameworks chosen because of their content relevance to the research questions about patient engagement, implementation science, and health inequities (see Additional file 2) [38]. Goodman and Sanders Thompsons’ stakeholder engagement framework depicts intensity levels at which researchers engage patients, including methods not truly engaged to highly engaged participation [39]. The Health Equity Implementation Framework highlights domains relevant to implementation and healthcare disparities, such as the intervention being implemented, who is involved (recipients), and societal context [40]. We assessed whether participants mentioned specific disparities among patients. Coders 1 and 2 (AIMC, ENW) independently extracted a random sample from all data sources and met for consensus until 80% agreement was met between them, then extracted the remaining data independently. In some data sources, we identified more than one “case” or example of patient engagement in implementation activities and extracted each case.
Data integration and analysis
We merged all cases, or specific examples, of patient engagement in implementation activities from all three data sources into a final dataset. Our final dataset included specific examples with descriptions of each and patient engagement level according to Goodman and Sanders Thompsons’ framework (the latter was determined by Coders 1 and 2 and a third coder [JEK or CW] resolved disagreements). Next, coders synthesized descriptions of all data into a matrix of Health Equity Implementation Framework domains. They then reviewed each case for recurring challenges, grouping them into themes with 100% agreement, and extracted every potential solution mentioned for those challenges.
Results
Data description
We included 22 cases: four webinars, 11 literature articles, and seven interview participants in our final sample (see Fig. 1). From these, we identified 27 examples of implementers (from webinars, articles, or interviews) using patient engagement in healthcare service delivery implementation activities. All originated from the past decade. See Table 1 for descriptive information about what innovations were being implemented, in which settings, and for whom, according to the Health Equity Implementation Framework. One note is that, in describing elements of patient engagement in implementation activities, implementers rarely specified if they were engaging a population experiencing healthcare inequities.
Examples and intensity levels of patient engagement in implementation activities
We described how implementers operationalized patient engagement in implementation activities, sorting them by patient engagement intensity level according to Goodman and Sanders Thompson’s framework in Table 2.
Half of the examples featured implementers engaging patients in coordination, a medium-intensity level of patient engagement. Coordination typically involved convening patients in groups for the provision of unidirectional feedback, such as using recurring, monthly patient engagement groups that consulted with researchers (some of whom studied implementation) in the example by LaChapelle [53]. Sometimes patients were engaged individually, still at the “coordination” level, to provide unidirectional feedback, as showcased in the example in Participant Interview 2 in which patients completed surveys and interviews about how to adapt a psychotherapy after having exposure to the treatment. Between levels of intensity regarding engagement, sometimes the “how” patients were engaged were similar, yet processes or roles differed enough that patient engagement was made more meaningful. For example, many of the activities categorized under “coordination”—a lower intensity engagement activity—and “collaboration”—a higher intensity engagement activity—involved assembling patient advisory groups. Upon closer review, there were processes and roles in those activities we considered collaboration that signaled a deeper, longer, and more patient-centered approach, such as being involved in all phases of implementation (e.g., Browne 2020, literature article), [48] serving in roles with more power or voice (e.g., Participant Interview 1), and patients seeing how their input was incorporated (e.g., Gesell 2021, literature article) [51].
The most intensive patient engagement activity (Norman 2013, literature article), also shown in Table 2, involved a community advisory council consisting of patients who set priorities for implementation (e.g., which disease to focus on), brought in healthcare professionals, and helped those professionals develop and test dissemination strategies for several healthcare issues. In this case, healthcare professionals assisted with an ongoing community initiative and patients have initial decision making capability, dictated priorities, engaged repeatedly over long periods of time about design/delivery for better implementation, and were compensated for their time [42]. As shown in Fig. 2, the remaining examples featured cooperating or collaborating with patients, representing incrementally more intensive levels of patient engagement than coordinating with them.
Percentage of patient engagement examples in U.S. healthcare implementation activities by intensity, classified according to Goodman and Sanders Thompson (2017). Note. CBPR = community-based participatory research. Starting at coordination and moving clockwise, the levels range from least intensive to more intensive patient engagement, ending with CBPR
Recurring challenges and solutions
We identified eight recurring challenges mentioned as barriers in at least two examples. Recurring challenges included: (1) Lack of processes to communicate equitably among all people involved; (2) issues recruiting patients who had a demographic makeup consistent with actual patients served across different intensity levels of engagement; (3) inadequate logistic, financial, or educational resources to successfully incentivize or carry out patient engagement activities; (4) difficulty retaining patients over time in implementation effort; (5) risk of tokenism: asking one member of a patient population to represent all patients from that population; (6) patients were not in suitable roles, and wanted to do something other than implementation, such as disseminate results or be actual research participants; (7) lack of feedback given to patients about results of their engagement; and (8) patients were engaged too late in the implementation effort for their engagement to be useful or realized.
In Table 3, we describe in more detail challenges mentioned and matched challenges with promising solutions extracted from data. In this text, we describe the two most frequently mentioned challenges and promising solutions in depth.
Recurring challenge 1: lack of processes to communicate equitably among all people
Implementers described a dearth of informal and formal processes to ensure equitable communication between patients and healthcare professionals within existing power differentials. Equitable communication would consist of comfort sharing and receiving feedback bidirectionally, a nonjudgmental atmosphere, and shared opportunities for all to speak and listen. In one webinar, Asch [54] emphasized the difficulty healthcare professionals face in learning “to speak with [patients] effectively about research” and implementation. Communication processes were also needed to ensure the ‘right’ people for an issue could share feedback at their comfort level and that others could understand this feedback.
Promising solutions to a lack of processes to communicate equitably
Solutions for ensuring equitable communication centered on behaviors for patients or healthcare professionals.
Behaviors for Patients
Patients might take introductory research workshops or short courses, as they did in one effort, “so when they were at the table with researchers, they could have conversations” (Interview participant 6, 2019). Another patient-led solution was to create rules of engagement for meetings, suggesting:
“…one of those rules is confidentiality in the meeting and a right to pass…not only the right to pass if they don’t feel like mentioning or talking about a topic that would make them uncomfortable or disclosing any personal health information, but it’s also the right to pass somewhat on the question the [implementers] bring to the meetings and bring up other questions that they think might be more valuable” (LaChapelle, webinar, 2017) [53].
Behaviors for healthcare professionals
One implementer recommended asking professionals to make their presentations more patient-friendly, emphasizing the need to “spell out acronyms and do not use acronyms; also use layperson terms, not medical terms” (Fehling, webinar, 2016) [52]. Another implementer (who was also a patient) acknowledged that even having patients present changed the dynamic of communication: “Sometimes our [patient] influence is just our presence – they change the way the information is shared, and the way they operate because a patient is there” (Interview participant 5, 2019). Another presenter described this shift to consider:
“What [patient] groups tend to want is a lot more in the direction of practicality. What program or policy does the [healthcare system] need to do? How is this going to affect the program or policy? …You have to know who the individual across the table from you and figure out what it is that they want and they know.” (Asch, webinar, 2018) [54].
During the meetings, some implementers found it helpful to explicitly state that patients were experts there and their voice was highly valued, thereby empowering patients to educate the rest of the group on topics related to their lived experience (Barger et al.,2019) [47]. Further instructions for the person leading meetings were described:
“Be versed in group dynamics, allowing suggestions and comments to be made that are not always ‘pro healthcare.’…There would certainly be times not only for general roundtable discussion but also for direct questioning of less-vocal group members to ensure the broadest possible discussion of opinions.” (Angstman, literature article, 2009) [41].
Angstman et al. [41] also suggested limiting the size of groups to facilitate better communication “to approximately 15 members. A larger group may be intimidating and may limit discussion.”
Recurring challenge 2: recruiting a diversity of patients representative of actual patients served
Across engagement levels, many implementers described difficulties recruiting patients with a demographic makeup consistent with actual patients served. For example, one implementer discussed the challenges of engaging U.S. military veterans who were women or racially minoritized to serve on veteran advisory boards. Many data sources pointed to difficulty engaging people burdened by health problems or societal disadvantages such as poverty. For example, in a literature article concerning implementation of asthma interventions, Tapp [44] reported mostly engaging patients with advanced education or careers in healthcare that were not representative of the broader swath of patients living with asthma [60]. Implementers noted that the patients engaged were more homogenous than populations served in their settings.
Promising solution to recruiting a diversity of patients
One solution suggested in the data we scanned was to recruit a broader diversity of patients by compensating them for their time (Tapp 2017, literature article) [44], and aligning administrative logistics such that they could be paid financially (Fehling 2016, webinar) [52]. Although, financial compensation did not guarantee engagement, as exemplified in one example in which patients did not respond regularly to electronic messages or paper letters requesting feedback even after being oriented, agreeing to engage, being paid for their time (Participant Interview 3). Other solutions to ensure a diverse representation of patients included providing accommodations for their needs, such as providing childcare during meetings, convenient meeting times (which will vary based on life context), and transportation to meetings (Pérez Jolles, 2017, literature articles) [43].
Discussion
Through an environmental scan in the U.S., we identified 27 examples of patient engagement in healthcare service delivery implementation activities. Many examples of “how” implementers are doing this work included assembling patients in groups (“councils” or “steering committees”) to advise implementation or incorporating patients into existing implementation teams as participating members. There are certainly other ways to engage patients in design/delivery of implementation activities, including training them to facilitate change in healthcare systems, [61] sampling their viewpoints repeatedly through surveys, interviews, [49] or practice run-throughs as mock patients before, during, and after healthcare professionals make changes in clinical practice. Implementers described eight recurring challenges. The two most frequently identified challenges were: (1) a lack of processes that allowed for equitable communication among all people and (2) difficulty recruiting a diversity of patients representative of those served in the healthcare setting. In addition, we matched promising solutions described by implementers to recurring challenges. Implementers rarely specified if they were engaging a population experiencing healthcare inequities.
We compared examples in this scan to five patient engagement implementation strategies recommended by experts through a consensus process [9]. Most examples from this scan fell under “involve patients and family members,” a strategy rated by experts as very important and feasible. Interestingly, none of the examples in this scan were intentional to “increase demand” or “use mass media”— two strategies rated by experts as the least feasible [9].
Regarding the intensity of engagement, half the examples in our scan involved medium intensity level of engagement (“coordination”), such that implementers worked with patients to obtain unidirectional feedback on implementation but did not collaborate in ways such as paying patients, empowering them to make decisions, or asking them to assist with or lead tasks. This finding contrasts a systematic review of global examples, most outside the U.S., in which implementers frequently used higher intensity levels of engagement, including collaboration as partners and co-design of healthcare service delivery [22]. This is important because existing literature suggests that different intensities of engagement may yield different outcomes. In one study of patient engagement in primary care redesign across Ireland, researchers found activities similar to or less intensive than coordination (e.g., information events, one-time consultation with healthcare teams) to be more feasible than higher-intensity engagement. Engaging patients with higher intensity (e.g., integrating patients on primary care teams) proved more difficult, and its usefulness was less clear [62]. And yet, in a global systematic review, authors concluded that unidirectional patient engagement (e.g., consultation) usually led to more discrete products, like a toolkit. In contrast, collaborative and co-created patient engagement led to changes in the care process or structural outcomes [22]. Lower-intensity engagement may be more feasible. Yet, such engagement may produce outcomes with lower impact.
One implication from our findings is that the intensity and process of engaging patients fall on a continuum, [39] and there may not be one ideal intensity level for implementation efforts. Only one example in this scan used the most intensive community-based participatory research (CBPR) approach in implementation activities, emphasizing capacity building, equitable distribution of finances, co-ownership, and having patients collect and analyze information. A CBPR approach to implementation requires significantly more time and resources than coordination and will not always be feasible for implementers or patients. Indeed, Ramanadhan and colleagues suggested that implementers and patients evaluate their goals for an implementation activity to select the optimal patient engagement level [6]. It might be ideal to offer choices for how intensely any person wants and can engage.
The challenges we identified to patient engagement in U.S. implementation activities were consistent with and expanded upon barriers in existing literature from Canada, [63] the U.K., [22] and another U.S. institution [64]. This suggests that some challenges encountered across the U.S. are similar to those in other jurisdictions, despite structural differences between the U.S. and other countries in political and economic regulation of healthcare. Because some challenges are similar, implementers in any region can learn from those in other places. Some countries outside the U.S. appear to have long histories of patient engagement in implementation and higher intensity patient engagement [22, 61] and, thus, a wider range of solutions to those challenges than those identified in this scan [22, 65]. For example, these efforts are supported by financial funding in healthcare systems in Ireland, [62] Canada, [20] and the U.K [19]. Yet, even in countries with strong policy and financial support for patient engagement, variations in strategies and terminology and organizational structure and culture can lead to confusion [19, 62, 66]. Researchers found a prior history of engagement with patients promoted more substantial organizational changes—the longer places engaged with the same community groups or patients, the easier it was to build on existing relationships for ongoing change [62]. Situating our results from the U.S. within the global context of what is necessary for successful patient engagement in implementation activities, it appears two “levels” may be essential. The first level is that structural factors support patient engagement in implementation activities, such as organizational funding, personnel training, and policy support, and these are necessary alongside best practices at the interpersonal level between patients and professionals, such as inclusive recruitment strategies, equitable communication practices, and early engagement processes.
One specific challenge we identified was that implementers could not always engage patients burdened by societal barriers and experiences of healthcare disparities, consistent with findings elsewhere [64]. Engaging populations experiencing healthcare disparities means overcoming societal disadvantage and mistrust experienced by these populations and perpetuated by unjust structures in the U.S [64]. Implementers need to be proactive, creative, and intentional about engagement strategies for patients experiencing disparities. Most examples in this scan did not report patients’ demographic characteristics or lived experiences, making it difficult to determine whether they involved patients experiencing disparities. The absence of such critical information was also documented in a systematic review of patient engagement in implementation activities in the U.K [19]. Across jurisdictions, there might be less attention to inequities, power differentials during engagement, and strategies to overcome barriers for those experiencing disparities. Implementers might need to interrogate privileges and biases they bring to engagement encounters with people impacted by health disparities, akin to cultural humility [57]. A future research question is whether a more robust use of patient engagement in implementation activities reduces healthcare disparities.
Limitations
While we scanned literature and implementers from any U.S. healthcare system, within that, we scanned some data from webinars narrowed to one system. Although this was a thoughtful choice to extend a recent systematic review of global literature, [22] this approach limits the external validity of our findings. Interviewing a convenience sample of implementers also limits our ability to be comprehensive. Finally, we did not identify which implementation strategies were used (e.g., financial incentives, changing physical structure).
Conclusion
Despite patients being engaged in numerous implementation activities across healthcare settings, there are no clear guidelines on how to facilitate their participation or what level of engagement is recommended in the U.S. Our findings offer implementers ideas for how to engage patients in design/delivery of implementation activities, including considerations for more “light touch” or less intensive engagement depending on patient preference, resources, or prior implementer skills, and also more intensive engagement which might result in meaningful, patient-centered shifts on a larger scale. There may not be one ideal level of intensity, which policies on patient engagement in implementation should consider, although this is a topic for hypothesis testing in future research.
Compared to other countries, like the U.K., with longer histories and more structural support for patient engagement in implementing changes in healthcare service delivery, implementers in the U.S. appear to have similar challenges in recruitment, retention, and meaningful engagement. Thus, one practice implication is that implementers in the U.S. can learn from other countries that appear to have more varied solutions and experiences responding to challenges. However, across jurisdictions, no countries appear to have a robust focus or strong support for patients experiencing disparities to improve health equity.
One funding and policy suggestion is that patient engagement should be considered as another piece of the implementation puzzle in U.S. healthcare, along with implementation strategies targeting clinic staff, leadership, organizational structures, and policies. Patient engagement in implementation activities can potentially reduce inequities through local tailoring at the clinic-level that is more patient-centered and enhanced end user buy-in for interventions [4, 25]. If prior experience with engagement makes it easier to engage patients in the future, [62] leading to change, then the history of health inequality in the U.S [56, 58, 59] means we must double-down on efforts to engage patients experiencing disparities to move toward health equity.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request. Please contact the first, second, or last author.
Abbreviations
- CINAHL:
-
Cumulative Index of Nursing and Allied Health Literature
- CBPR:
-
Community-based participatory research
- PCORI:
-
Patient-Centered Outcomes Research Institute
- U.K.:
-
United Kingdom
- U.S.:
-
United States
- VHA:
-
Veterans Health Administration
References
Holt CL, Chambers DA. Opportunities and challenges in conducting community-engaged dissemination/implementation research. Transl Behav Med. 2017;7(3):389–92.
Wilson P, Mathie E, Keenan J, McNeilly E, Goodman C, Howe A, et al. ReseArch with patient and public invOlvement: a RealisT evaluation – the RAPPORT study. Health Serv Deliv Res. 2015;3(38):1–176.
Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100(Suppl 1):40–6.
Cerdá M, Tracy M, Ahern J, Galea S. Addressing population health and health inequalities: the role of fundamental causes. Am J Public Health. 2014;104(S4):609–19.
Caplan W, Davis S, Kraft S, Berkson S, Gaines M, Schwab W, et al. Engaging patients at the front lines of primary care redesign: operational lessons for an effective program. Joint Comm J Qual Patient Saf. 2014;40(12):533–40.
Ramanadhan S, Davis MM, Armstrong R, Baquero B, Ko LK, Leng JC, et al. Participatory implementation science to increase the impact of evidence-based cancer prevention and control. Cancer Causes Control. 2018;29(3):363–9.
Kirchner JE, Waltz TJ, Powell BJ, Smith JL, Proctor EK. Implementation strategies. In: Brownson RC, Colditz GA, Proctor EK, editors. Dissemination and implementation research in health: translating science to practice. 2nd ed. New York: Oxford University Press; 2018.
Minkler M, Salvatore A. Participatory Approaches for Study Design and Analysis in Dissemination and Implementation Research. In: Dissemination and Implementation Research in Health: Translating Science to Practice. 1st ed. Oxford University Press; 2012. Available from: http://www.oxfordscholarship.com/view/10.1093/acprof:oso/9780199751877.001.0001/acprof-9780199751877. Cited 2017 Apr 15.
Waltz TJ, Powell BJ, Matthieu MM, Damschroder LJ, Chinman MJ, Smith JL, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci. 2015;10(1). Available from: http://implementationscience.biomedcentral.com/articles/10.1186/s13012-015-0295-0. Cited 2017 Feb 14.
Sessums LL, McHugh SJ, Rajkumar R. Medicare’s vision for advanced primary care: new directions for care delivery and payment. JAMA. 2016;315(24):2665.
National Committee for Quality Assurance. Standards and guidelines for NCQA’s patient-centered Medical Home (PCMH). Washington: National Committee for Quality Assurance; 2011.
Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. J Gen Intern Med. 2005;20(10):953–7.
Han E, Scholle SH, Morton S, Bechtel C, Kessler R. Survey shows that fewer than a third of patient-centered medical home practices engage patients in quality improvement. Health Aff. 2013;32(2):368–75.
Okun S, Schoenbaum D, Andrews P, Chidambaran V, Cholette J, Gruman S, et al. Patients and health care teams forging effective partnerships. Discussion paper. Washington: Institute of Medicine; 2014. Available from: http://www.iom.edu/patientsaspartners.
Wilson MG, Lavis JN, Travers R, Rourke SB. Community-based knowledge transfer and exchange: helping community-based organizations link research to action. Implement Sci. 2010;5:33.
Jull J, Giles A, Graham ID. Community-based participatory research and integrated knowledge translation: advancing the co-creation of knowledge. Implement Sci. 2017;12(1). Available from: https://implementationscience.biomedcentral.com/articles/10.1186/s13012-017-0696-3. Cited 2018 May 18.
National Health Service Accelerated Access Collaborative. Patient and public involvement. 2021. Available from: https://www.england.nhs.uk/aac/what-we-do/patient-and-public-involvement/.
Gremyr I, Elg M, Eriksson E, Halldórsson Á, Smith F, Gustavsson S. Exploring power shifts as an enabler for a strengthened patient role in quality improvements: a Swedish survey study. BMJ Open Qual. 2021;10(1):e001185.
Mockford C, Staniszewska S, Griffiths F, Herron-Marx S. The impact of patient and public involvement on UK NHS health care: a systematic review. Int J Qual Health Care. 2012;24(1):28–38.
Healtcare Excellence Canada. What We Do. 2021. Available from: https://www.cfhi-fcass.ca/what-we-do.
Baker R, Camosso-Stefinovic J, Gillies C, Shaw EJ, Cheater F, Flottorp S, et al. Tailored interventions to address determinants of practice. In: The Cochrane Collaboration, editor. Cochrane Database of Systematic Reviews. Chichester: John Wiley & Sons, Ltd; 2015. Available from: http://doi.wiley.com/10.1002/14651858.CD005470.pub3. Cited 2016 Aug 9.
Bombard Y, Baker GR, Orlando E, Fancott C, Bhatia P, Casalino S, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci. 2018;13(1). Available from: https://implementationscience.biomedcentral.com/articles/10.1186/s13012-018-0784-z. Cited 2018 Aug 28.
Lopatina E, Miller JL, Teare SR, Marlett NJ, Patel J, Barber CEH, et al. The voice of patients in system redesign: a case study of redesigning a centralized system for intake of referrals from primary care to rheumatologists for patients with suspected rheumatoid arthritis. Health Expect. 2019;22(3):348–63.
Ramanadhan S, Minsky S, Martinez-Dominguez V, Viswanath K. Building practitioner networks to support dissemination and implementation of evidence-based programs in community settings. Transl Behav Med. 2017;7(3):532–41.
Wells KB, Jones L, Chung B, Dixon EL, Tang L, Gilmore J, et al. Community-partnered cluster-randomized comparative effectiveness trial of community engagement and planning or resources for services to address depression disparities. J Gen Intern Med. 2013;28(10):1268–78.
Brookman-Frazee L, Stahmer A, Stadnick N, Chlebowski C, Herschell A, Garland AF. Characterizing the use of research-community partnerships in studies of evidence-based interventions in children’s community services. Adm Policy Ment Health. 2016;43(1):93–104.
Nápoles AM, Stewart AL. Transcreation: an implementation science framework for community-engaged behavioral interventions to reduce health disparities. BMC Health Servi Res. 2018;18(1). Available from: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-3521-z. Cited 2019 Jan 9.
Agency for Healthcare Research and Quality. Strategy 1: Working With Patients and Families as Advisors. Agency for Healthcare Research and Quality; 2017. Available from: https://www.ahrq.gov/patient-safety/patients-families/engagingfamilies/strategy1/index.html.
Glandon D, Paina L, Alonge O, Peters DH, Bennett S. 10 best resources for community engagement in implementation research. Health Policy Plann. 2017;32(10):1457–65.
Bartlett JA, Peterson JA. The uptake of human papillomavirus (HPV) vaccine among adolescent females in the United States: a review of the literature. J School Nurs. 2011;27(6):434–46.
Rabin BA, Lewis CC, Norton WE, Neta G, Chambers D, Tobin JN, et al. Measurement resources for dissemination and implementation research in health. Implement Sci. 2016;11. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4802882/. Cited 2016 Apr 19.
Choo CW. Environmental scanning as information seeking and organizational learning. Inform Res. 2001;7(1). Available from: http://www.informationr.net/ir/7-1/paper112.html.
Patient-Centered Outcomes Research Institute. Engagement in health research literature explorer. 2019 . Available from: https://www.pcori.org/engagement/engagement-literature. Cited 2019 May 6.
Ritchie MJ, Smith JL, Kim B, Woodward EN, Kirchner JE. Building a comprehensive collection of implementation facilitation literature to advance the science and practice of facilitation. Poster Presentation presented at: 15th Annual Conference on the Science of Dissemination & Implementation in Health. Washington: 2022.
Better Systematic Review Management. 2020. Covidence. Available from: https://www.covidence.org/.
Leighton K, Kardong-Edgren S, Schneidereith T, Foisy-Doll C. Using social media and snowball sampling as an alternative recruitment strategy for research. Clin Simul Nurs. 2021;55:37–42.
Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18(1):59–82.
Woodward EN, Matthieu MM, Uchendu US, Rogal SS, Kirchner JE. The Health equity implementation framework: proposal and preliminary study of hepatitis C virus treatment. Implement Sci. 2019;14:26.
Goodman MS, Sanders Thompson VL. The science of stakeholder engagement in research: classification, implementation, and evaluation. Behav Med Pract Policy Res. 2017;7(3):486–91.
Woodward EN, Singh RS, Ndebele-Ngwenya P, Melgar Castillo A, Dickson KS, Kirchner JE. A more practical guide to incorporating health equity domains in implementation determinant frameworks. Implement Sci Commun. 2021;2(1):61.
Angstman KB, Bender RO, Bruce SM. Patient Advisory Groups in Practice Improvement: Sample Case Presentation With a Discussion of Best Practices. J Ambul Care Manage. 2009;32(4):328–32.
Norman N, Bennett C, Cowart S, Felzien M, Flores M, Flores R, et al. Boot camp translation: a method for building a community of solution. J Am Board Family Med. 2013;26(3):254–63.
Pérez Jolles M, Martinez M, Garcia SJ, Stein GL, Mentor Parent Group Members, Thomas KC. Involving Latina/o parents in patient-centered outcomes research: Contributions to research study design, implementation and outcomes. Health Expect. 2017;20(5):992–1000.
Tapp H, Derkowski D, Calvert M, Welch M, Spencer S. Patient perspectives on engagement in shared decisionmaking for asthma care. FAMPRJ. 2017;34(3):353–7.
English AF, Dickinson LM, Zittleman L, Nease DE, Herrick A, Westfall JM, et al. A Community Engagement Method to Design Patient Engagement Materials for Cardiovascular Health. Ann Fam Med. 2018;16(Suppl 1):S58-64.
Dickinson WP, Nease DE, Rhyne RL, Knierim KE, Fernald DH, de la Cerda DR, et al. Practice Transformation Support and Patient Engagement to Improve Cardiovascular Care: From EvidenceNOW Southwest (ENSW). J Am Board Fam Med. 2020;33(5):675–86.
Barger S, Sullivan SD, Bell-Brown A, Bott B, Ciccarella AM, Golenski J, et al. Effective stakeholder engagement: design and implementation of a clinical trial (SWOG S1415CD) to improve cancer care. BMC Med Res Methodol. 2019;19(1):119.
Browne T, Swoboda A, Ephraim PL, Lang-Lindsey K, Green JA, Hill-Briggs F, et al. Engaging patients and family members to design and implement patient-centered kidney disease research. Res Involv Engagem. 2020;6(1):66.
Pandhi N, Jacobson N, Crowder M, Quanbeck A, Hass M, Davis S. Engaging patients in primary care quality improvement initiatives: facilitators and barriers. Am J Med Qual. 2020;35(1):52–62.
Pekmezaris R, Kozikowski A, Pascarelli B, Wolf-Klein G, Boye-Codjoe E, Jacome S, et al. A Telehealth-Delivered Pulmonary Rehabilitation Intervention in Underserved Hispanic and African American Patients With Chronic Obstructive Pulmonary Disease: A Community-Based Participatory Research Approach. JMIR Form Res. 2020;4(1):e13197.
Gesell SB, Coleman SW, Mettam LH, Johnson AM, Sissine ME, Duncan PW. How engagement of a diverse set of stakeholders shaped the design, implementation, and dissemination of a multicenter pragmatic trial of Stroke transitional care: the COMPASS study. J Clin Trans Sci. 2021;5(1):e60.
Fehling K, Krawec-Paul C, Westmoreland W. Growing a Veteran Engagement Group (VEG): Examples from COINs. Cyberseminar. VA Health Services Research & Development; 2016 Available from: https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=1127.
LaChappelle. Veteran Engagement Three Ways: Insights and Lessons Learned from Engaging Veterans at Three VA Research Centers. Cyberseminar. VA Health Services Research and Development; 2017.
Asch S. Dancing with the Devil You Know: Partnered Implementation Science Research. Cyberseminar; 2017. VA Health Services Research & Development. Available from: https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=2316.
Elwy R. Utilizing Stakeholders as Communication Partners. Cyberseminar; 2018. VA Health Services Research & Development. Available from: https://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/video_archive.cfm?SessionID=2472.
Adler NE, Rehkopf DH. U.S. disparities in Health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235–52.
Tervalon M, Murray-García J. Cultural humility versus cultural competence: a critical distinction in defining physician training outcomes in multicultural education. J Health Care Poor Underserved. 1998;9(2):117–25.
Office of Minority Health and Health Equity. CDC Health Disparities & Inequalities Report (CHDIR). 2013. Available from: https://www.cdc.gov/minorityhealth/CHDIReport.html.
Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care (with CD). Washington: National Academies Press; 2003. Available from: http://www.nap.edu/catalog/12875. Cited 2017 Jul 18.
Tapp H, Derkowski D, Calvert M, Welch M, Spencer S. Patient perspectives on engagement in shared decision-making for asthma care. FAMPRJ. 2016;cmw122.
Duong DM, Bergström A, Wallin L, Bui HT, Eriksson L, Eldh AC. Exploring the influence of context in a community-based facilitation intervention focusing on neonatal health and survival in Vietnam: a qualitative study. BMC Public Health. 2015;15(1). Available from: http://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-015-2142-2. Cited 2019 Sep 13.
McEvoy R, Tierney E, MacFarlane A. Participation is integral’: understanding the levers and barriers to the implementation of community participation in primary healthcare: a qualitative study using normalisation process theory. BMC Health Serv Res. 2019;19(1):515.
Bellows M, Kovacs Burns K, Jackson K, Surgeoner B, Gallivan J. Meaningful and effective patient engagement: what matters most to stakeholders. Patient Exp J. 2015;2(1):18–28.
Bodison SC, Sankaré I, Anaya H, Booker-Vaughns J, Miller A, Williams P, et al. Engaging the community in the dissemination, implementation, and improvement of health-related research. Clin Transl Sci. 2015;8(6):814–9.
Absolom K, Holch P, Woroncow B, Wright EP, Velikova G. Beyond lip service and box ticking: how effective patient engagement is integral to the development and delivery of patient-reported outcomes. Qual Life Res. 2015;24(5):1077–85.
Bergerum C, Engström AK, Thor J, Wolmesjö M. Patient involvement in quality improvement – a ‘tug of War’ or a dialogue in a learning process to improve healthcare? BMC Health Serv Res. 2020;20(1):1115.
Acknowledgements
Thank you to the implementers we surveyed and interviewed! We are grateful to Dr. Yvonne Bombard who consulted with us on selecting a stakeholder engagement framework and published an important systematic review that inspired this work and to Dr. Kelsey Dickson who assisted in ideas for presenting mixed methods. Thank you to Dr. Mona Ritchie and Mr. Jeffrey Smith who shared literature and search methods from the Implementation Facilitation Literature Collection that served as one of our databases.
Funding
Locally Initiated Project, FY2019, Health Services Research and Development, Veterans Health Administration. The funder approved the project as described in this manuscript and had no role in the interpretation or writing of results.
Author information
Authors and Affiliations
Contributions
ENW conceptualized the study and designed study methods, conducted data collection and analysis, interpreted results and wrote and edited the manuscript; AIMC collected and analyzed data, interpreted results, and edited the manuscript; GT refined study methods, especially regarding sampling, and assisted in refining interpretation of results and editing the manuscript; CW refined study methods, interpreted results, wrote sections of the discussion, and edited the entire manuscript; JEK assisted in conceptualizing the study and methods, assisted in interpreting results, and edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study deemed exempt as not human subjects research by the Central Arkansas Veterans Healthcare System Institutional Review Board. Because this was not considered human subjects research by the ethics board, informed consent was deemed unnecessary by the regulating body. However, before implementers participated in interviews, they were given a rationale for the study and explained their information would be de-identified. All methods were carried out in accordance with relevant guidelines and regulations under the ethics board. There were no experimental protocols and no direct involvement of any patients in our study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Implementer Survey and Semi-structured Interview Questions. This is a document showcasing the survey questions we used in interviewing implementers for the scan
Additional file 2.
Coding Template of Patient Engagement Activities in Implementation, Systems Redesign, or Quality Improvement. This is a document of a blank coding template used to extract data from each case we identified in the environmental scan
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Woodward, E.N., Castillo, A.I.M., True, G. et al. Challenges and promising solutions to engaging patients in healthcare implementation in the United States: an environmental scan. BMC Health Serv Res 24, 29 (2024). https://doi.org/10.1186/s12913-023-10315-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-023-10315-y