Abstract
Background
Worse health outcomes are consistently reported for First Nations people in Canada. Social, political and economic inequities as well as inequities in health care are major contributing factors to these health disparities. Emergency care is an important health services resource for First Nations people. First Nations partners, academic researchers, and health authority staff are collaborating to examine emergency care visit characteristics for First Nations and non-First Nations people in the province of Alberta.
Methods
We conducted a population-based retrospective cohort study examining all Alberta emergency care visits from April 1, 2012 to March 31, 2017 by linking administrative data. Patient demographics and emergency care visit characteristics for status First Nations persons in Alberta, and non-First Nations persons, are reported. Frequencies and percentages (%) describe patients and visits by categorical variables (e.g., Canadian Triage and Acuity Scale). Means, medians, standard deviations and interquartile ranges describe continuous variables (e.g., age).
Results
The dataset contains 11,686,288 emergency care visits by 3,024,491 unique persons. First Nations people make up 4% of the provincial population and 9.4% of provincial emergency visits. The population rate of emergency visits is nearly 3 times higher for First Nations persons than non-First Nations persons. First Nations women utilize emergency care more than non-First Nations women (54.2% of First Nations visits are by women compared to 50.9% of non-First Nations visits). More First Nations visits end in leaving without completing treatment (6.7% v. 3.6%).
Conclusions
Further research is needed on the impact of First Nations identity on emergency care drivers and outcomes, and on emergency care for First Nations women.
Similar content being viewed by others
Background
Poor health outcomes impact Indigenous peoples internationally, as both a consequence and mechanism of colonization [1, 2]. Within Canada, the term First Nations (FN) refers to one of the three Indigenous groups recognized as holding aboriginal and treaty rights by the Constitution Act, 1982, alongside Inuit and Metis [3, 4]. Health disparities for FN persons in Canada [5, 6] are recognized as related to persistent social, political and economic inequities, including inequities in health care services and delivery [6,7,8,9,10]. Academics and government inquiries agree that colonialism and racism have led to devastating impacts on FN health [7, 11,12,13]. Emergency medicine has an important role in providing care to marginalized populations that have limited access to other health care services, given its longstanding commitments to providing care to all comers [14]. Non-academic and academic literature shows that Indigenous persons rely more heavily on emergency services than non-Indigenous persons [15,16,17].
While it is laudable that emergency medicine provides accessible care for underserved groups, disparities in emergency care for racial and ethnic minorities are well documented [18, 19]. Indigenous patients specifically have been reported to leave emergency departments more often without being seen [16, 20,21,22], potentially indicating dissatisfaction with care. Canadian qualitative research documents patient concerns about differential treatment based on race and experiences of marginalization in health care [23, 24].
Recognizing that Indigenous populations are unique (with longstanding cultural traditions and sovereignty as original inhabitants of territories), there have been efforts to understand how best to serve Indigenous persons in emergency departments [25,26,27]. There have also been widespread calls for Indigenous communities to deliver or direct their own health services, notably within the United Nations Declaration of the Rights of Indigenous Peoples [28]. Yet work in the field of Indigenous emergency care is hindered by a relative lack of comprehensive peer-reviewed statistical analyses, which could impact system level considerations of resource distribution and health services organization.
The objective of this study is to report population rates of emergency care use for FN and non-FN populations, as well as quantitative differences in emergency visit characteristics, between FN and non-FN persons in Alberta, Canada. There are 45 First Nation communities within three treaty areas in Alberta [29], and the province is served by a single health authority [30, 31]. Ability to identify FN patients within emergency care data held by a provincial health authority provides an opportunity to examine system level emergency care statistics across a broad geography (inclusive of rural and urban areas) and varied facility sizes.
Methods
This project brings together Western and Indigenous research approaches and understandings [32,33,34]. We recognize that Indigenous knowledge systems encompass quantitative components [35], such as the Blackfoot Winter Count, and that statistical analysis methods can be utilized within research guided by Indigenous principles [36]. Ethics approval is granted by the University of Alberta Health Research Ethics Board Pro 00082440.
This population-based retrospective cohort study examines all emergency care visits in Alberta from April 1, 2012 to March 31, 2017. Data on emergency care visits and urgent care visits are included in the analysis, including where these occur in ambulatory care centres. Three facility types (emergency departments, urgent care centres and ambulatory care centres) provide urgent unscheduled medical care in Alberta, but are not evenly distributed geographically throughout the province. Care that may be provided at an urgent care centre in Edmonton or Calgary could be provided at a small emergency department, or (where one exists) an ambulatory care centre, in a rural or remote area. As such, our provincial analysis of emergency care system use includes these three facility types.
De-identified quantitative administrative data was obtained from the provincial government Ministry ofHealth and the integrated provincial health services provider, Alberta Health Services (AHS) [30, 31], with person-level linkage between datasets complete prior to transfer of the data to researchers. Analytic results were shared regularly with FN partners for collaborative interpretation.
FN-identifying information is based on health care premium payments, which were charged in Alberta until 2009. The federal government paid these fees for registered FN persons, which permitted the identification of FN persons in the Alberta Health Care Insurance Plan (AHCIP) Population Registry. Additionally, an individual (e.g. child) is also flagged as a FN person if they have an AHCIP account for which the main registrant has been identified as a FN person at some point since 1983 [37]. This process of identifying FN persons residing in Alberta is used in government publications of FN health statistics (e.g. [38]) and in academic publications.(e.g. [39]) Alberta Health also provided annual population figures for FN and non-FN populations. “Non-status” FN persons, such as those who lost their federally recognized FN status through colonial policies (see [13] p. 53–55), and status FN persons who came to Alberta from another jurisdiction after 2009, are misidentified as non-FN in the data.
The National Ambulatory Care Reporting System (NACRS) collects information on emergency care encounters [40]. Patient age, sex, mode of arrival (e.g. ground ambulance), facility type (described in next paragraph), time and day of emergency care visit, and Canadian Triage Acuity Scale (CTAS) [41] are available within NACRS. CTAS is a triage system used to rate the acuity of the patients’ presenting health condition, in order to prioritize treatment to the most acute urgent cases [41].
Facility types are described by the seven level AHS Peer Groups, which categorize facilities from tertiary hospitals to community ambulatory sites. Tertiary hospitals provide access to specialized services such as organ transplants, high dose chemotherapy and nuclear medicine. Community hospitals provide emergency and inpatient services, and may provide ambulatory care, obstetrics and surgery [42]. Urgent and ambulatory care centres treat urgent conditions that could deteriorate. These centres have no inpatient capacity, and they transport more acute cases that are beyond their capacity to treat [42, 43].
Categorization of patient residence is derived from the AHS “Postal Code” dataset used for geographic analysis. The AHS Rural-Urban Continuum and AHS geographic zones [44] were utilized to analyze distribution of patient residences. The rural-urban continuum stratifies patient residences “by rural/urban status” [45]. The AHS zones are geographic areas organized from North to South. Zones have separate administrative structures, and are used by AHS to organize decision making and delivery of services. Two zones (Edmonton and Calgary) are composed of metropolitan cities and surrounding communities [46, 47], while three are larger geographic areas containing one to two regional centres each (North, Central and South Zones) [48,49,50].
AHS Distance Tables provide information on the distance in minutes of drive time between patient postal codes and emergency departments, based upon geographic analysis of Alberta’s road network [51]. Patient comorbidities are assessed using the Charlson Comorbidity Index, plus hypertension. The Charlson Index provides the relative “weight” of various combinations of comorbidities based on adjusted mortality and resource use [52]. The AHS Analytics team generated Charlson scores for this project for each emergency visit based on ICD-10 coding of diagnoses using inpatient and NACRS data from a 2 year retrospective time period.
3 M’s Episode Disease Category (EDC) [53] system is utilized to group emergency visit diagnoses. Related EDC categories have been grouped by a physician team member (CB) and the 45 resulting groupings were validated by a second physician team member (BRH; see Additional file 1: Appendix 1).
Analysis
Age and sex standardized emergency care visit rates per person are derived using 2012/2013 figures as the reference population. Upper and lower 95% confidence interval limits are provided based on standard rates adjusted for recurrent events [54]. Two significant digits are given for population rates, to aid readers who wish to convert these rates to larger denominators (e.g. per 100 persons). Numerical summaries (i.e., means, medians, standard deviations [SDs], IQRs represented as [25th percentile, 75th percentile]) and counts (with percentages) describe emergency care patient demographics and visit data. Analyses at the patient-level use the first emergency visit for patients with multiple visits. All analyses are provided for the FN and non-FN populations separately. Linear mixed-effects models and generalized linear mixed-effects models assess differences between groups, adjusted for repeated emergency visits per patient. Statistical analyses were conducted in R [55] and SAS software [56].
Results
Alberta Health estimates Alberta’s non-FN population as 4,033,045 in 2017, having increased from 3,714,268 in 2013. Alberta Health estimates the FN population of Alberta as 162,868 in 2017, an increase from 160,123 in 2013. Table 1 shows emergency care visit population rates provincially and across regions of the province (AHS zones). Provincially the age and sex standardized emergency care visit rate is 2.86 times higher for FN.
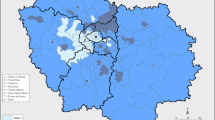
Figure 1 shows 2016/2017 emergency visit rates in the five AHS zones. Rates are higher for FN populations than non-FN populations in all zones. Rates for both population groups are notably higher in the South, Central and North zones compared to Edmonton and Calgary zones. “Rural-urban continuum” categories (e.g. remote, metro) were also examined and FN populations were found to use emergency care more than non-FN populations within all categories.
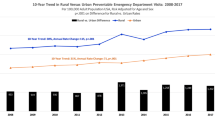
Figure 2 shows standardized emergency visit rates provincially and by zone over 5 years for both population groups. The large differences in emergency visit population rates do not narrow over the 5year study period.
Table 2 describes emergency visit categories. Our data set contains 3,024,491 unique patients, of whom 145,508 (4.8%) are FN. These FN patients made 1,099,424 (9.4%) of the 11,686,287 emergency care visits during the study period. Eighty-nine percent of all FN persons used emergency care at least once during our 5 year period (145,508 unique patients divided by 162,868 (2017 FN population)), compared to 71 % of all non-FN persons (2,878,983 unique non-FN patients divided by 4,033,045 (2017 non-FN population)). Individual FN patients who use emergency care utilize it more (median 4 visits per person, [IQR 2, 9]) compared to non-FN patients who utilized emergency care (median 2, [IQR 1, 4]).
Table 3 describes the geographic and facility type distribution of ED visits. One hundred and eleven facilities had emergency care visits during our study period. FN emergency visit numbers to individual facilities varied (median 3279, [IQR 960, 14,338]). Thirty-three (30% of 111) facilities saw 80% of all FN visits provincially. In four facilities, > 50% of visits were made by FN patients. The highest percentage of FN visits, as a proportion of visits to a facility, was 83% (43,739 of 52,844 total visits), while the lowest was 0.4% (70 FN visits of 18,358 total visits).
FN women (female sex) use the emergency care system proportionately more than their non-FN counterparts, while FN men use the emergency care system comparatively less than both FN women and non-FN men. Patient age across FN visits differs by a median of 6 years from patient age across non-FN visits (FN median 30, [IQR 17, 46]; non-FN median 36, [IQR 20, 57]). FN visits end more often in leaving without being seen or against medical advice (6.7% of FN visits vs. 3.6% of non-FN visits) and are more often in the evening (43.6% vs. 38.1%). See Additional file 1: Appendix 2 for a table of emergency visits by day of the week and by ED shift. FN visits arrive more often by ground ambulance (15.3% vs. 10%) relative to non-FN visits and are more commonly triaged as less acute (59% CTAS 4 (less urgent) and 5 (non-urgent), compared to 50.4% non-FN). The top 10 groups of episode disease categories by FN count comprise 78.9% of all FN visits during the study period. Among these ten categories, trauma and injury, gastrointestinal conditions, and musculoskeletal and arthritis conditions, make up a lower percent of FN than non-FN visits. FN emergency visits have higher comorbidity scores than non-FN emergency visits. Additional file 1: Appendix 3 presents the incidence of specific comorbidities across emergency visits. Additional file 1: Appendix 4 presents characteristics of unique patients (as opposed to emergency visits), based on a patient’s first visit. Patient level statistics show higher emergency care use by patients who are older, live closer to emergency facilities, and have higher comorbidity scores for both FN and non-FN patients. FN women do not make up as large a proportion of unique FN patients (50.7%), as they do of FN emergency visits (54.2%). This finding demonstrates that FN women who use emergency care had more visits per person than FN men.
Discussion
Explanation of findings
FN persons make up 4% of the Alberta population but 9.4% of all emergency visits. 89% of the FN population visited emergency care at least once during our study period compared to 71% of the non-FN population. This proportion shows that FN patients are an important patient group for emergency care.
Five FN Elder knowledge holders and five FN Health Directors co-interpreted data with researchers. They contextualized higher emergency care visit rates in terms of a lack of access to primary care. Our study did not examine primary care access in relation to ED use, and further research would be needed to examine links between primary care access and emergency care quantitatively. However, wider literature suggests a link between access to high quality primary care and emergency care use [57,58,59,60]. Studies also suggest that FN access to primary care is limited [61,62,63,64,65,66] and so a case may be made for the need for such further research. Indeed, a recent government inquiry into Indigenous health care in the neighboring province of British Columbia directly compares use of emergency care to primary care access, and found that Indigenous people who were not attached to primary care “were more likely to visit the ED and be hospitalized.” [60] Similarly, innovative analysis by Lavoie and colleagues shows that levels of primary health care in FN communities are associated with reductions in avoidable hospitalizations and premature mortality [65]. Further research reproducing their methods could be conducted to determine if emergency care use is similarly impacted by levels of primary care access within communities.
In our study, we also found that a large proportion of FN visits are triaged as lower acuity (CTAS 4 and 5), and this finding could be related to use of emergency care for primary care concerns. However, it should be noted that Zook and colleagues [67] have reported under-triage of American Indian patients based on race, and further research would be needed to explore triage of First Nations patients in Canada.
Our results also show that FN women present to emergency care more than non-FN women. Turpel-Lafond has similarly found that Indigenous women utilize emergency departments more than Indigenous men in British Columbia [60]. In meetings for our project, Elders hypothesized that FN men may present to emergency care less than FN women because of a greater reluctance to seek care among FN men. By contrast, Turpel-Lafond concluded that Indigenous women face unique forms of discrimination, and that their greater emergency care use is driven in part by greater avoidance of preventive and primary health care [60]. Turpel-Lafond also found that Indigenous women face a health care gap, compared to non-Indigenous women, in terms of such services as midwifery, obstetrician deliveries and antenatal visits [60]. Further research on FN women’s emergency care in Alberta is warranted.
FN team members contextualized presentations to emergency care in evenings and arrival by ambulance in terms of issues accessing transport to and from emergency facilities. A 2005 study by Wallace and colleagues similarly found that use of emergency care may be associated with lack of access to non-urgent medical transportation [68].
FN partners contextualized leaving without completing treatment in terms of experiences of discrimination within the health care system (see also [23, 69]), needing to leave when transport is available and leaving care to fulfill family responsibilities. Issues related to discrimination, transport and family responsibilities could be explored through survey or qualitative research with FN users of emergency care.
Findings of higher rates of FN patients leaving without being seen and leaving against medical advice are similar to earlier US findings for American Indian populations [22, 70], for FN Chronic Obstructive Pulmonary Disorder patients in Alberta emergency departments [21], and for FN abdominal pain patients in a Saskatchewan emergency department [20]. Patients who leave emergency care without completing treatment may be at risk of returning to emergency facilities [71] and admissions to hospital [71, 72]. To our knowledge, no studies have examined outcomes for FN patients who leave without completing treatment. This is an important area for future research.
High use of emergency care does not necessarily mean FN patients are using emergency care unnecessarily or inappropriately [73]. There is no agreed upon definition of what constitutes inappropriate or non-urgent emergency care use [74, 75]. Patients choose emergency care because it is the right care option from their perspective [76].
Future directions
As noted above, links between FN emergency care use and access to other components of the health care system (especially primary care), emergency care of FN women, factors impacting emergency care use such as anti-Indigenous discrimination and access to non-emergency transport, and emergency care outcomes for FN patients (including those who leave without completing treatment) are important areas for future research. To address differences in patient demographics, future research should examine outcomes reported here stratified by sex and geography, and qualitative research should examine different groups’ understandings of quantitative findings (e.g. FN men and women, rural and urban FN persons). In addition, as many factors interact to determine FN patients’ emergency care visit characteristics and outcomes, further quantitative research should attempt to separate the impact of FN identity from factors such as diagnosis, distance traveled to care and size of facility presented to. Stratifying analysis by any of these variables would produce distinct descriptive statistical results, which may be of value for specific projects or more granular understanding of FN emergency care. The provincial analysis reported here may aid in making decisions about which variables to stratify by in such future analysis.
Limitations
Our data counts most non-status FN persons, status FN persons who came to Alberta after 2009, and potentially some status FN persons not identified in the data set for other unknown reasons, as non-FN persons. As such, differences between FN and non-FN statistics may be under-reported. Future research could overcome this limitation if access to the Federal “Indian Register” could be obtained [77]. However, our use of the provincial data identifiers that are relied upon by Alberta Health in its reporting on FN health outcomes provides comparability to provincial government analyses and so allows our work to better inform health system decision makers.
Métis and Inuit persons are also counted among the non-FN population, concealing any similarities in emergency care statistics among Indigenous populations. This limitation means that we cannot say how FN emergency care statistics compare to other Indigenous populations’ emergency care statistics. We chose to work with FN for this project, recognizing their distinct history, governance structures and governing relationships with Federal and Provincial jurisdictions compared to other Indigenous peoples in Alberta. If future research involved Métis governing bodies and appropriate Inuit partners, and data identifiers were available, this limitation could be overcome.
Geographic data represent only a point in time. Patients may move more frequently than this data is updated. When accessing emergency care, patients will not always be travelling from their residence or to the facility closest to their residence. If FN and non-FN patients differ systematically in frequency of moving residence or number of emergency care visits where the patient travels to the nearest emergency department from their residence, this would impact our results. We are not aware of quantitative data that suggests such systematic differences. Limitations on geographic data derive from provincial health administrative data relied on for this study. Future research with a smaller sample and utilizing primary data collection could overcome these limitations by verifying up to date residence information and by deriving travel distances between hospital addresses for specific emergency care visits and patient residences.
Conclusions
FN persons’ rely on the emergency care system more than non-FN persons in Alberta. High rates of FN visits ending without completing treatment are concerning as this outcome may indicate dissatisfaction with care, and has been found in some studies to expose patients to increased odds of hospital admission. Future research could productively examine emergency care outcomes for FN patients (including for those who leave emergency care without completing treatment), explore links between FN emergency care use and access to other health services (especially primary care), stratify quantitative results reported here by variables such as geography (e.g. rural vs urban) or facility type, and examine FN women’s emergency care. Qualitative research to obtain FN perspectives on quantitative findings will also be invaluable for better understanding emergency care of FN populations.
Availability of data and materials
The original data sources for this study are owned by Alberta Health Services and Alberta Health. Readers may contact the corresponding author for more information.
Abbreviations
- FN:
-
First Nations
- CTAS:
-
Canadian Triage Acuity Score
- AHS:
-
Alberta Health Services
- AHCIP:
-
Alberta Health Care Insurance Plan
- NACRS:
-
National Ambulatory Care Reporting System
- EDC:
-
Episodic Disease Category
References
Czyzewski K. Colonialism as a broader social determinant of health. The International Indig Pol J. 2011;2(1):1–16.
Daschuk J. Clearing the plains: disease, politics of starvation, and the loss of Aboriginal life. Regina: University of Regina Press; 2013.
The Constitution Act, 1982, Schedule B to the Canada Act 1982 (UK), 1982, c 11. https://www.canlii.org/en/ca/laws/stat/schedule-bto-the-canada-act-1982-uk-1982-c-11/latest/schedule-b-to-the-canada-act-1982-uk-1982-c-11.html.
Canadian Institutes of Health Research, Natural Sciences and Engineering Research Council of Canada, and Social Sciences and Humanities Research Council of Canada. Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans, Chapter 9: Research Involving the First Nations, Inuit and Métis Peoples of Canada. 2018.
Gracey M, King M. Indigenous health part 1: determinants and disease patterns. Lancet. 2009;374(9683):65–75. https://doi.org/10.1016/S0140-6736(09)60914-4.
Alberta Health, AFNIGC. Trends in life expectancy over time for First Nations in Alberta. 2016. Available from: http://www.afnigc.ca/main/includes/media/pdf/fnhta/HTAFN-2016-05-31-LifeExp2.pdf/. Accessed 28 Apr 2021.
King M, Smith A, Gracey M. Indigenous health part 2: the underlying causes of the health gap. Lancet. 2009;374(9683):76–85. https://doi.org/10.1016/S0140-6736(09)60827-8.
Cameron B, Carmargo Plazas MP, Salas AS, Bourque Bearskin RL, Hungler K. Understanding inequalities in access to health care services for Aboriginal people: a call for nursing action. Adv Nurs Sci. 2014;37(3):E1–16. https://doi.org/10.1097/ANS.0000000000000039.
Greenwood M, de Leeuw S, Lindsay N. Challenges in health equity for Indigenous peoples in Canada. Lancet. 2018;391(10131):1645–8. https://doi.org/10.1016/S0140-6736(18)30177-6.
Smylie J, Firestone M. Back to the basics: identifying and addressing underlying challenges in achieving high quality and relevant health statistics for Indigenous popluations in Canada. Stat J IAOS. 2015;31(1):67–87. https://doi.org/10.3233/SJI-150864.
Canada. People to people, nation to nation: highlights from the report of the Royal Commission on Aboriginal Peoples. 1996. Available from: https://www.rcaanc-cirnac.gc.ca/eng/1100100014597/1572547985018. Acccessed 13 Mar 2021.
Axelsson P, Kukutai T, Kippen R. The field of Indigenous health and the role of colonisation and history. J Popul Res. 2016;33(1):1–7. https://doi.org/10.1007/s12546-016-9163-2.
Truth and Reconciliation Commission of Canada. Honouring the truth, reconciling for the future: summary of the final report of the Truth and Reconciliation Commission of Canada. Winnipeg: Truth and Reconciliation Commission of Canada; 2015.
Zink BJ. Social justice, egalitarianism, and the history of emergency medicine. Virtual Mentor. 2010;12(6):492–4. https://doi.org/10.1001/virtualmentor.2010.12.6.mhst1-1006.
Alberta Health, AFNIGC. Top reasons for emergency department visits for first nations in Alberta 2010–2014: Alberta Health and AFNIGC; 2016. Available from: http://www.afnigc.ca/main/includes/media/pdf/fnhta/HTAFN-2016-07-26-ED-VISITS.pdf. Accecssed 28 Apr 2021.
Thomas DP, Anderson IP. Use of emergency departments by Aboriginal and Torres Strait Islander people. Emerg Med Australas. 2006;18(1):68–76. https://doi.org/10.1111/j.1742-6723.2006.00804.x.
First Nations Health Authority. First Nations Health Status & Health Services Utilization Summary of Key Findings: 2008/09–2014/15. Available from: https://www.fnha.ca/WellnessSite/WellnessDocuments/FNHA-First-Nations-Health-Status-and-Health-Services-Utilization.pdf#search=First%20Nations%20Health%20Status. Acccessed 10 May 2020.
Lee P, Le Saux M, Siegel R, Goyal M, Chen C, Ma Y, et al. Racial and ethnic disparities in the management of acute pain in US emergency departments: meta-analysis and systematic review. Am J Emerg Med. 2019;37(9):1770–7. https://doi.org/10.1016/j.ajem.2019.06.014.
Owens A, Holroyd B, McLane P. Patient race, ethnicity, and care in the emergency department: a scoping review. CJEM. 2020;22(2):245–53. https://doi.org/10.1017/cem.2019.458.
Batta R, Carey R, Sasbrink-Harkema MA, Oyedokun TO, Lim HJ, Stempien J. Equality of care between First Nations and non-First Nations patients in Saskatoon emergency departments. CJEM. 2019;21(1):111–9. https://doi.org/10.1017/cem.2018.34.
Ospina M, Rowe BH, Voaklander D, Senthilselvan A, Stickland MK, King M. Emergency department visits after diagnosed chronic obstructive pulmonary disease in Aboriginal people in Alberta, Canada. CJEM. 2016;18(6):420–8. https://doi.org/10.1017/cem.2016.328.
Weber T, Ziegler KM, Kharbanda AB, Payne N, Birger C, Puumala S. Leaving the emergency department without complete care: disparities in American Indian children. BMC Health Serv Res. 2018;18(1):267. https://doi.org/10.1186/s12913-018-3092-z.
Browne A, Smye VL, Rodney P, Tang SY, Mussell B, O'Neil J. Access to primary care from the perspective of Aboriginal patients at an urban emergency department. Qual Health Res. 2011;21(3):333–48. https://doi.org/10.1177/1049732310385824.
Allan B, Smylie J. First peoples, second class treatment: the role of racism in the health and well-being of Indigenous peoples in Canada. Toronto: Wellesley Institute; 2015.
Berg K, McLane P, Eshkakogan N, Mantha J, Lee T, Crowshoe C, et al. Perspectives on Indigenous cultural competency and safety in Canadian hospital emergency departments: a scoping review. Int Emerg Nurs. 2019;43:133–40. https://doi.org/10.1016/j.ienj.2019.01.004.
Varcoe C, Bungay V, Browne AJ, Wilson E, Wathen CN, Kolar K, et al. EQUIP Emergency: study protocol for an organizational intervention to promote equity in health care. BMC Health Serv Res. 2019;19(687).
Gadsden T, Wilson G, Totterdell J, Willis J, Gupta A, Chong A, et al. Can a continuous quality improvement program create culturally safe emergency departments for Aboriginal people in Australia? A multiple baseline study. BMC Health Serv Res. 2019;19(222).
UN General Assembly. United Nations declaration on the rights of Indigenous peoples: resolution / adopted by the General Assembly, 2007, A/RES/61/295.
Indigenous and Northern Affairs Canada. First Nations in Alberta 2010 [Available from: https://www.aadnc-aandc.gc.ca/eng/1100100020670/1100100020675]. Accessed 13 Mar 2021.
Alberta Health Services. About AHS 2020 [Available from: https://www.albertahealthservices.ca/about/about.aspx]. Accessed 13 Mar 2021.
Alberta Health Services. Vision, Mission, Values & Strategies 2020 [Available from: https://www.albertahealthservices.ca/about/Page190.aspx]. Accessed 13 Mar 2021.
Ermine W. The ethical space of engagement. Ind Law J. 2007;6(1):193–203.
Martin D. Two-eyed seeing: a framework for understanding Indigenous and non-Indigenous approaches to Indigenous health research. Can J Nurs Res. 2012;44(2):20–42.
Hyett S, Marjerrison S, Gabel C. Improving health research among Indigenous peoples in Canada. CMAJ. 2018;190(20):E616–21. https://doi.org/10.1503/cmaj.171538.
Blackstock C. First Nations children count: enveloping quantitative research in an Indigenous envelope. First Peoples Child Family Rev. 2009;4(2):135–43.
Walter M, Andersen C. Indigenous statistics: a quantitative research methodology. Walnut Creek: Routledge; 2013.
Alberta Health Analytics, Performance Reporting Branch. Interactive health data application: First Nations indicators. 2019 [Available from: http://www.ahw.gov.ab.ca]. Accessed 13 Mar 2021.
Alberta Health, AFNIGC. Alberta Opioid Response Surveillance 2019 [Available from: https://www.alberta.ca/assets/documents/health-first-nations-opioid-surveillance.pdf]. Accessed 13 Mar 2021.
Moore S, Antoni S, Colquhoun A, Healy B, Ellison-Loschmann L, Potter JD, et al. Cancer incidence in Indigenous people in Australia, New Zealand, Canada, and the USA: a comparative population-based study. Lancet Oncol. 2015;16(15):1483–92. https://doi.org/10.1016/S1470-2045(15)00232-6.
Canadian Institute for Health Information. National ambulatory care reporting system metadata (NACRS). 2017. [Available from: https://www.cihi.ca/en/national-ambulatory-care-reporting-system-metadata]. Accessed 13 Mar 2021.
Beveridge R, Clark B, Janes L, Savage N, Thompson J, Dodd G, et al. Canadian emergency department triage and acuity scale: implementation guidelines. 1998 [Available from: https://www.colleaga.org/sites/default/files/ctased16.pdf]. Accessed 13 Mar 2021.
Alberta Health Services. Facility peer group development for performance reporting. 2015.
Alberta Health. Alberta health facility and functional centre definitions and facility listing 2020 [Available from: https://open.alberta.ca/dataset/a18c14dc-c816-481a-a8c0-f1cd2496e25d/resource/36cc1a54-0706-4a5f-9bd7-e83a8fc4c57d/download/health-ahcip-facility-listing-2020-01.pdf] Accessed 10 May 2020.
Alberta Health Services. AHS map and zone overview, 2016/17: report to the community 2017 [Available from: https://www.albertahealthservices.ca/assets/about/publications/ahs-ar-2017/zones.html]. Accessed 13 Mar 2021.
Alberta Health Services, Alberta Health. Official standard geographic areas 2018 [Available from: https://open.alberta.ca/dataset/a14b50c9-94b2-4024-8ee5-c13fb70abb4a/resource/70fd0f2c-5a7c-45a3-bdaa-e1b4f4c5d9a4/download/Official-Standard-Geographic-Area-Document.pdf]. Accessed 13 Mar 2021.
Alberta Health Services. Edmonton Zone 2016 [Available from: https://www.albertahealthservices.ca/assets/zone/ahs-zn-edmonton-map-brochure.pdf]. Accessed 13March 2021.
Alberta Health Services. Calgary Zone 2016 [Available from: https://www.albertahealthservices.ca/assets/zone/ahs-zn-calgary-map-brochure.pdf]. Accessed 13 Marc 2021.
Alberta Health Services. North Zone 2016 [Available from: https://www.albertahealthservices.ca/assets/zone/ahs-zn-north-map-brochure.pdf]. Accessed 13 March 2021.
Alberta Health Services. Central Zone 2016 [Available from: https://www.albertahealthservices.ca/assets/zone/ahs-zn-central-map-brochure.pdf]. Accessed 13 Mar 2021.
Alberta Health Services. South Zone 2016 [Available from: https://www.albertahealthservices.ca/assets/zone/ahs-zn-south-map-brochure.pdf]. Accessed 13 Mar 2021.
Alberta Health Services. Rural service access guidelines for emergency department and acute medical inpatient service planning. 2013.
Charlson M, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. https://doi.org/10.1016/0021-9681(87)90171-8.
3M. Health Information Systems. Clinical Risk Grouping Software Definitions Manual. 2013. Update for v1.11 ed.
Stukel T, Glynn RJ, Fisher ES, Sharp SM, Lu-Yao G, Wennberg JE. Standardized rates of recurrent outcomes. Stat Med. 1994;13(17):1781–91. https://doi.org/10.1002/sim.4780131709.
Core Team R. R: a language and environment for statistical computing; 2017.
S. A. S. Institute Inc. Sas/stat. 2012.
Huntley A, Lasserson D, Wye L, Morris R, Checkland K, England H, Salisbury C., Purdy S. Which features of primary care affect unscheduled secondary care use? A systematic review. BMJ Open 2014;4:e004746, 5, doi: https://doi.org/10.1136/bmjopen-2013-004746.
Lowe R, Localio AR, Schwarz DF, Williams S, Tuton LW, Maroney S, et al. Association between primary care practice characteristics and emergency department use in a medicaid managed care organization. Med Care. 2005;43(8):792–800. https://doi.org/10.1097/01.mlr.0000170413.60054.54.
van den Berg M, van Loenen T, Westert GP. Accessible and continuous primary care may help reduce rates of emergency department use. An international survey in 34 countries. Fam Pract. 2016;33(1):42–50.
Turpel-Lafond M. In Plain Sight: Addressing Indigenous-specific Racism and Discrimination in B.C. Health Care. Government of British Columbia. British Columbia; 2020.
Davy C, Harfield S, Mcarthur A, Munn Z, Brown A. Access to primary health care services for Indigenous peoples: a framework synthesis. Int J Equity Health. 2016;15:1–9.
Lavoie J, Forget E, Browne A. Caught at the crossroad: First Nations, health care, and the legacy of the Indian act. J Indig Wellbeing. 2010;8(1):83–100.
Lavoie J, Kaufert J, Browne AJ, Mah S, O'Neil J, Sinclair S, et al. Negotiating barriers, navigating the maze: First Nation peoples’ experience of medical relocation. Can Public Admin. 2015;58(2):295–314. https://doi.org/10.1111/capa.12111.
Lavoie J, O'Neil JD, Sanderson L, Elias B, Mignone J, Bartlett J, et al. The national evaluation of the First Nations and Inuit health transfer policy. Manitoba First Nations Centre for Aboriginal Health Research. Winnipeg; 2005.
Lavoie J, Wong ST, Ibrahim N, O'Neil J, Green M, Ward A. Underutilized and undertheorized: the use of hospitalization for ambulatory care sensitive conditions for assessing the extent to which primary healthcare services are meeting needs in British Columbia first nation communities. BMC Health Serv Res. 2019;19(1):50. https://doi.org/10.1186/s12913-018-3850-y.
Lavoie J, Kornelsen D, Boyer Y, Wylie L. Lost in maps: regionalization and Indigenous health services. Healthc Pap. 2016;16(1):63–73. https://doi.org/10.12927/hcpap.2016.24773.
Zook H, Kharbanda A, Flood A, Harmon B, Puumala S, Payne N. Racial differences in pediatric emergency department triage scores. J Emerg Med. 2016;50(5):720–7. https://doi.org/10.1016/j.jemermed.2015.02.056.
Wallace R, Hughes-Cromwick P, Mull H, Khasnabis S. Access to health care and nonemergency medical transportation: two missing links. Transp Res Rec. 1924;2005:76–84.
McLane P, Bill L, Barnabe C. First Nations members’ emergency department experiences in Alberta: a qualitative study. CJEM. 2021;23(1):63–74. https://doi.org/10.1007/s43678-020-00009-3.
Harrison B, Finkelstein M, Puumala S, Payne NR. The complex association of race and leaving the pediatric emergency department without being seen by a physician. Pediatr Emerg Care. 2012;28(11):1136–45. https://doi.org/10.1097/PEC.0b013e31827134db.
Mataloni F, Colais P, Galassi C, Davoli M, Fusco D. Patients who leave emergency department without being seen or during treatment in the Lazio region (Central Italy): determinants and short term outcomes. PLoS One. 2018;13(12):e0208914. https://doi.org/10.1371/journal.pone.0208914.
Li D, Brennan J, Kreshak A, Castillo E, Vilke G. Patients who leave the emergency department without being seen and their follow-up behavior: a retrospective descriptive analysis. J Emerg Med. 2019;57(1):106–13. https://doi.org/10.1016/j.jemermed.2019.03.051.
Nwankwo C. First Nations and Métis health service: literature review of first nations and Métis’ use of the emergency department: University of Saskatchewan & Saskatoon Health Region; 2014.
Durand A, Gentile S, Devictor B, Palazzolo S, Vignally P, Gerbeaux P, et al. ED patients: how nonurgent are they? Systematic review of the emergency medicine literature. Am J Emerg Med. 2011;29(3):333–45. https://doi.org/10.1016/j.ajem.2010.01.003.
Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19(1):47–59.
Durand A, Palazzolo S, Tanti-Hardouin N, Gerbeaux P, Sambuc R, Gentile S. Nonurgent patients in emergency departments: rational or irresponsible consumers? Perceptions of professionals and patients. BMC Res Notes. 2012;5:525.
Government of Canada. What is the Indian Register 2021 [Available from: https://www.sac-isc.gc.ca/eng/1100100032463/1572459644986#chp3]. Accessed 13 Mar 2021.
Acknowledgements
Alireza Jalaeian Bashirzadeh assisted in statistical analysis. Team members Danika Littlechild, Eunice Louis (Maskwacis Health Services), Anne Bird (Yellowhead Tribal Council), Kris Janvier (Organization of Treaty Eight First Nations of Alberta) and Tessy Big Plume (Stoney Nakoda Tsuut’ina Tribal Council) contributed to interpretation of data. Elders Helen Bull (Maskwacis Health Services), Mary Crawler (Bighorn First Nation), Lena Firth (O’Chiese First Nation), Patsy Tina Jacobs (Stoney Nakoda Tsuut’ina Tribal Council) and Dustin Twin (Organization of Treaty Eight First Nations of Alberta) contributed to interpretation of data. Val Austen-Wiebe and Kienan Williams (Indigenous Wellness Core, Alberta Health Services) have been key supporters of the wider project this manuscript derives from. Leslee Mackey (University of Alberta) provided proof reading, editing and formatting support. An abstract based on this work was accepted to the Canadian Association of Emergency Physicians 2020 conference, which was canceled due to COVID-19. The abstract was published in the Canadian Journal of Emergency Medicine, Volume 22, Supplement 1.
The views expressed in this document are solely those of the authors and do not represent those of their employers. AFNIGC has ensured compliance with the First Nations principles of Ownership, Control, Access to and Possession (OCAP®) of research data, and provides the following disclaimer: “Parts of this publication are based on data and information from the Understanding and Defining Quality of Care in the Emergency Department with First Nations Members in Alberta project. The analyses, conclusions, opinions and statements expressed herein, however, do not necessarily reflect the views of the Alberta First Nations Information Governance Centre (AFNIGC) and are solely those of the author(s). Statistics reproduced from this document must be accompanied by a citation of this document, including a reference to the page on which the statistic in question appears.”
Funding
Funding was provided by the Canadian Institutes for Health Research #156176. The funder had no role in directing research methods, data collection, analysis or interpreting and reporting results.
Author information
Authors and Affiliations
Contributions
PM, BH, CB, BRH, AC, LB, KR, and RR contributed to design of the research. PM, AC, BH and LB contributed to acquisition of data. PM, CB, BRH, AC, KF, LB, KR, CH, BH and RR contributed to analysis or interpretation of data. PM drafted the article. KF assisted in writing the first draft of the discussion. PM, CB, BRH, AC, LB, KF, KR, CH and RR critically revised the text for important intellectual content. All authors approve the final version to be published. All authors agree to act as guarantors of the work.
Authors’ information
PM is a PhD Sociologist, Assistant Scientific Director of the Emergency Strategic Clinical Network and Adjunct Assistant Professor in the University of Alberta Department of Emergency Medicine. CB is a Métis health services researcher, rheumatologist, and expert in Indigenous health. BRH is Professor of Emergency Medicine and Senior Medical Director of the AHS Emergency Strategic Clinical Network. AC is the Manager of Population Health Assessment for Alberta Health and Adjunct Professor in the University of Alberta School of Public Health. LB is a Cree Traditional Practitioner/Knowledge Keeper and Executive Director of Alberta First Nations Information Governance Center with 40 years of experience with Indigenous health program development, delivery, practice and policy and research on community, national and international levels. KF is a Research Associate in the School of Public Health at the University of Alberta with a focus in Indigenous research. KR is Assistant Scientific Director of the Addiction and Mental Health Strategic Clinical Network and leads provincial harm reduction efforts for marginalized populations. CH (Blackfoot, Kainai Nation) is a Project Coordinator with the First Nations Health & Social Secretariat of Manitoba. BH (Aapooyaaki) has training as a Registered Nurse and is from the Kainai Nation. She is former Chair of the First Nations Information Governance Centre and currently the Health Director of the Blackfoot Confederacy. She has 30 plus years of experience working with First Nations, American, Australian and New Zealand Indigenous populations on health policy, health systems equity and Indigenous led research. RR is Professor of Pediatrics at the University of Alberta and a PhD bio-statistician.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval is granted by the University of Alberta Health Research Ethics Board Pro 00082440. Administrative permission to access data was granted through a Data Disclosure Agreement with Alberta Health Services. A formal reserach agreement was signed with AFNIGC.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendices 1-4. 1.
EDC Groupings used in Analysis. Appendix 2. Day of Week by Shift (Night, Day, Evening). Appendix 3. Emergency visit comorbidities. Appendix 4. Unique Patient Variables (based on 1st emergency visit).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
McLane, P., Barnabe, C., Holroyd, B.R. et al. First Nations emergency care in Alberta: descriptive results of a retrospective cohort study. BMC Health Serv Res 21, 423 (2021). https://doi.org/10.1186/s12913-021-06415-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-021-06415-2