Abstract
Background
A physician’s empathy level substantially impacts clinical competence, patient relationships, and treatment outcomes. Yet, understanding empathy trends from medical students to resident doctors within a single institution is limited. This study delves into empathy trends within a single-center academic setting and identifies factors associated with low empathy.
Methods
This cross-sectional study enrolled the second—to sixth-year medical students of Phramongkutklao College of Medicine and the first—to second-year residents at Phramongkutklao Hospital. It utilized a standardized questionnaire covering demographics, family relationships, the Maudsley Personality Inventory (MPI), and the Jefferson Scale of Empathy (JSE). The relationship between variables and JSE scores was analyzed using independent t-test, one-way ANOVA, and Chi-square tests. Multivariable logistic and linear regression analyses examined associated factors and trends across educational levels. A quadratic term was incorporated to evaluate the presence of a nonlinear trend.
Results
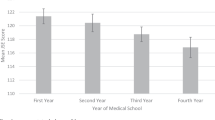
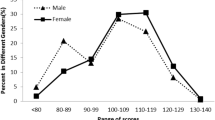
A total of 520 participants, comprising 189 (36.4%) preclinical students, 153 (29.4%) clinical students, and 178 (34.2%) residents, completed the survey. The JSE showed a Cronbach’s alpha of 0.83. The average empathy score was 103.8 ± 15.0, with 27.1% of low empathy levels. Specialty preference and sex-adjusted average empathy scores decreased from 114.5 (95%CI: 112.0–117.0) among second-year medical students to 95.2 (95%CI: 92.2–98.2) among second-year residents (Pnon−linear<0.001). The adjusted proportion of low empathy is highest among sixth-year medical students (54.4%, 95%CI: 34.4–73.2%). Factors associated with low empathy included those preferring procedure-oriented specialties (AOR: 4.16, 95%CI: 1.54–11.18) and a higher parental income (AOR: 2.97, 95%CI: 1.09 to 8.10). Subgroup analysis revealed that residents with a GPAX above 3.5 and those in technology-oriented specialties were also associated with lower empathy (AOR: 3.46, 95%CI: 1.40–8.59 and AOR: 2.93, 95%CI: 1.05–8.12, respectively).
Conclusion
A declining empathy trend was observed among medical students, which then plateaued among residents. Additionally, residents in technology-oriented specialties may require empathy enhancements due to their ongoing patient consultations. Addressing these issues requires collaborative planning between students and teachers to foster empathy throughout the medical curriculum.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Empathy in medical professionals has been critical for clinical competence and enhanced patient satisfaction and cooperation during treatment [1, 2]. These factors collectively contribute to improved treatment outcomes [3, 4]. However, numerous studies indicate a consistent decline in empathy levels among medical students throughout their education and residency. This significant reduction in empathy, observed as students progress through their academic years, is a trend documented in the United States [2, 5] and various countries worldwide, including Thailand [5, 6].
A systematic review of seven studies also highlights a significant decrease in empathy among resident physicians throughout their residency, which may adversely affect patient care quality and medical professionalism [7]. Further findings reveal that residents exhibit lower empathy levels than early-stage medical students and specialists [8, 9]. These might be due to workload and stress being prevalent among resident physicians [10, 11], with studies suggesting that physicians often cope by diminishing their empathy toward patients [12].
Empathy is primarily a cognitive attribute, focusing on understanding—rather than feeling—the patient’s experiences, concerns, and perspectives, along with the ability to communicate this understanding and the intention to assist [13]. Empathy, crucial for interpersonal relationships, likely correlates with personality traits affecting these dynamics. Positive associations are expected between empathy and traits fostering relationships, like sociability, whereas negative correlations might exist with traits hindering them, such as introversion and neuroticism [14, 15].
Preferred specialties are also one of the factors that may influence empathy levels. Personality traits, role models, market forces, societal needs, personal networks and educational experiences influence medical students’ specialty choices. Previous studies categorized specialties as “people-oriented” (e.g., internal medicine and family medicine), which focuses on initial health assessments and preventive care; “technology-oriented” (e.g., surgery and orthopedic), which involves specialized therapeutic techniques and is still oriented to the patient; and “procedure-oriented” (e.g., pathology and radiology), which involves specialized diagnostic procedures or applied basic laboratory which are patient-remote specialties [14,15,16]. Those in “people-oriented” fields are more interpersonally inclined than their counterparts, often resulting in higher empathy levels [14, 15, 17].
In addition, research indicates that empathy is associated with variables such as gender, personality traits, early family dynamics, and later socio-educational encounters [15]. For instance, evidence suggests that female medical students and residents exhibit higher levels of empathy than their male counterparts [6, 14, 18]. Nevertheless, to our knowledge, studies on empathy levels among non-binary physicians are rare despite their personality differences, such as higher positive emotions compared to binary genders. Non-binary individuals may face various forms of social exclusion, discrimination, and stigma across multiple domains in society, possibly affecting their empathy [6, 19, 20]. Additionally, individuals from families with either extremely high or low family function (disengaged or enmeshed) tend to demonstrate greater empathy compared to those from families with moderate dynamics [21, 22], and closer relationships within the family may positively affect psychological well-being, thereby influencing empathy levels [21, 23]. Moreover, a higher socioeconomic status within the family environment is linked to reduced levels of empathy [24].
Although numerous studies have investigated factors associated with empathy levels, there is limited information examining empathy across medical students and residency training within a single institution [6]. Previous studies have found that empathy often declines during medical school [25, 26]. Still, these studies are typically restricted to either medical students or residents or compare students and residents from different institutions [5, 6]. Similar to other hospitals here at Phramongkutklao College of Medicine (PCM) and Phramongkutklao Hospital (PMK), residents often serve as educators for medical students, and their ability to model empathy is crucial. Residents ' effective communication and teaching strategies can foster a more empathetic environment for students, enhancing their learning experience and professional attitudes [27]. On the other hand, medical students who are engaged, ask thoughtful questions, and actively participate in patient care help create a stimulating learning environment for residents [28]. Hence, understanding empathy trends within a single institution is essential for fostering a culture of empathy in healthcare.
Herein, the present study explores the level of empathy and associated factors with low empathy levels from the 2nd year medical students to 2nd year residents utilizing the data from PCM and PMK. The PCM curriculum includes two pre-clinical and three clinical years, with students transitioning from basic sciences to clinical rotations at PMK. Residents were trained at PMK, a tertiary care facility, and received training across various specialties, providing similar settings for both groups. Moreover, the present study also included non-binary gender in addition to the binary sexes. The insights from the present study would help design a tailored course to improve and maintain empathy levels across the continuum of professionality. Enabling targeted educational strategies informs curriculum development, ultimately contributing to the training of compassionate and competent healthcare professionals.
Methods
Study design and subjects
A cross-sectional study was carried out at PCM and PMK in Bangkok, Thailand, utilizing a self-administered survey. This survey included medical students from their second to sixth years, comprising 486 students and first—and second-year residents, totaling 285 residents at PMK. Whereas those who did not answer the JSE completely were excluded. The sample size calculation for a finite population of 771 was 254, using a desired precision of 0.05, a confidence interval of 0.95, and an expected prevalence of low empathy of 57% [29]. Figure 1 illustrates the flow of study participants and missing variables.
Phramongkutklao College of Medicine and Phramongkutklao Hospital educational settings
The PCM curriculum, spanning six years, is divided into one pre-medical year, two pre-clinical years focusing on basic sciences and three clinical years aimed at developing clinical experiences. Initially, first-year students, known as pre-medicals, study only basic science on other campuses with different contexts. Therefore, this study included second to sixth-year medical students. From the second to the third year, pre-clinical students begin to integrate basic science with clinical cases, primarily learning in classrooms and occasionally interacting with actual patients. Starting in the fourth year, students transition to clinical medical students, studying at PMK and rotating through various specialties and sub-specialties. In their final year, in addition to their rotation at PMK, students undertake a 4-month externship training at hospitals under the Ministry of Public Health, experiencing first contact with patients under relatively less supervision for the first time.
Regarding the residents at PMK, the hospital enrolls doctors who graduated from PMK and those who did not. As a tertiary care facility, it includes approximately 1,200 beds and offers training across various specialties and sub-specialties. These include major specialties like internal medicine, general surgery, obstetrics and gynecology, pediatrics, and minor specialties such as otolaryngology, radiology, orthopedics, pathology, etc.
Data collection
This study utilized a standardized questionnaire divided into three sections. The first section contained questions to gather demographic data, including gender, age, current year of study, cumulative grade point average (GPAX), current or preferred specialty, maternal and paternal status, education level of parents, monthly household income, and a rating scale out of 10 to assess the participant’s relationship with their current self, family, and past relationships. The second section used the Maudsley Personality Inventory (MPI) to assess introversion and extroversion personality traits. The third section featured the Jefferson Scale of Empathy (JSE), including the medical student version (S-version) for medical students and the health profession (HP-version) for resident doctors.
The survey, conducted on paper, was distributed to medical students after a monthly assembly. For residents, it was handed out after a monthly seminar. An information sheet was accessible through a QR code integrated into the survey, and participants were urged to review it carefully before proceeding. An interpretation of the MPI and JSE scores was provided on the last page of the survey. A basket was provided at the room’s exit for participants to submit the questionnaires to ensure anonymity, and no personal identification data was collected.
Participants were given multiple-choice options for categorical variables. For example, they could specify their gender as male, female, or non-binary. For family relationships, they rated their satisfaction on a scale from 1 (least satisfied) to 10 (most satisfied). Participants filled in boxes with their answers for continuous variables, such as three digits for GPAX and seven for monthly income.
The Maudsley personality inventory
Developed by Eysenck in 1959, the MPI, also known as the Eysenck Personality Inventory (EPI), is extensively utilized in the United States and the United Kingdom and adapted versions in Germany and France [30]. Its Thai adaptation [31] comprises 48 items, with 24 items each assessing Extraversion-Introversion (scale-E) and Neuroticism-Stability (scale-N) with construct validity between 0.64 and 0.78 and reliability scores of 0.91 and 0.90, respectively. Scoring differentiates positive from negative questions, with “Yes” earning 2 or 0 points, “Not sure” earning 1 point, and “No” 0 or 2 points [31]. This study focuses exclusively on the Extraversion-Introversion scale to examine introversion. Introversion was classified for individuals with MPI scores in the 1st quartile, Ambiversion for those in the 2nd and 3rd quartiles, and Extroversion for those in the 4th quartile.
The Jefferson Scale of Empathy
The Jefferson Scale of Empathy is an assessment tool used to measure empathy levels within the medical field, developed by Dr. Hojat and colleagues in 2001 for medical students [14]. It was later adapted by physicians and medical personnel [9]. The JSE features 20 questions, answered on a 7-point Likert scale, ranging from 1 (strongly disagree) to 7 (strongly agree) [13]. The JSE has been validated and published in research for validity and reliability [32]. Furthermore, the Thai version of the Jefferson Scale of Physician Empathy has been developed, demonstrating its reliability with a score of 0.76 and has undergone appropriate content and construct validity testing [33]. The JSE levels were further classified, establishing low cutoff scores at ≤ 91 for males and ≤ 97 for females [34]. While high are categorized as ≥ 126 and ≥ 128 for males and females, respectively [34].
Specialty subgroups
The participants were asked to provide their preferred specialty or current specialty, and the specialties were categorized as follows: (1) Procedure-oriented specialties involving specialized procedures or laboratory research with primary colleague interaction in hospital settings and are patient-remote (e.g., radiology, pathology). (2) Technology-oriented specialties focus on specialized therapeutic techniques and expert consultancy, mainly hospital-based, with some relatively patient-oriented office work (e.g., orthopedic surgery, neurosurgery, ophthalmology). For the people-oriented groups, including (3) Non-primary care specialties, providing episodic or long-term care for specific medical issues, combining ambulatory and hospital-based practice (e.g., cardiology, nephrology, dermatology). (4) Primary care specialties offer initial health assessments, preventive education, and comprehensive care for various conditions, primarily in office settings (e.g., family medicine, internal medicine, pediatrics) [14,15,16, 35].
Statistical analysis
All analyses were performed using StataCorp, 2021, Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC. The study subjects were described using a frequency distribution of demographic characteristics. Categorical data were presented as percentages. Continuous variables were presented as mean and standard deviation (SD) in the case of a normal distribution and median and interquartile range (IQR) in the case of a non-normal distribution. Family relationship satisfaction was categorized using a median score of 9 as the cutoff, with scores of 9 or 10 indicating above-median satisfaction and 8 or below indicating below-median satisfaction. Cronbach’s alpha was utilized to determine the internal consistency reliability, and the construct validity of relationship satisfaction was explored using exploratory factor analysis.
The relationship between the variables and JSE scores was analyzed using an independent t-test, ANOVA, and Chi-square as appropriate. Binary logistic regression analysis determined the odds ratio (OR) with 95%CI. Multivariable analysis was performed using logistic regression and linear regression analysis, and an adjusted odds ratio (AOR) and adjusted beta coefficient were presented. Linear regression was used to calculate preferred specialty- and sex-adjusted means, while logistic regression was applied to proportions to assess the statistical significance of linear and nonlinear trends. The presence of a nonlinear trend was initially evaluated by incorporating a quadratic term into the regression model. All statistical tests were two-sided; a P-value less than 0.05 was considered statistically significant. Although the final model was adjusted for potential confounders, the risk of residual confounding effects persists. Therefore, a sensitivity analysis was performed to address unmeasured confounding, employing E-values estimated by the e-value package (Supplementary Tables 1 and 2) [36, 37]. The study utilized the ggplot2 package in R software, version 4.3.3, for visualization.
Results
Characteristics of participants
The study involved 342 medical students and 178 residents, achieving response rates of 70.4% and 62.5%, respectively. Of the participants, 56.9% were male, and 2.5% identified as non-binary gender (Table 1). A majority (55.1%) of medical students preferred people-oriented specialties. Among the residents, 56.1% were people-oriented, 30.4% were technology-oriented, and 13.5% were procedure-oriented specialties. Over half of the participants (54.6%) had a GPAX above 3.5. The median monthly household income was 100,000 baht (IQR: 50,000-200,000). The average empathy score was 103.8 ± 15.0, with 27.1% classified in the lower empathy group. Moreover, Cronbach’s alpha of the JSE in the present study was 0.83, revealing good internal consistency reliability.
Trends of empathy across educational years
Figure 2 illustrates the declining trends in the specialty-adjusted and sex-and-specialty-adjusted means from second-year medical students to residents, stratified by sex. The adjusted mean peaks in the second year at 114.5 and stabilizes from the sixth year of medical study into residency, with values ranging between 93.3 and 97.7 (Pnon−linear<0.001). Furthermore, this decreasing trend is consistent across sexes. Figure 3 presents the adjusted proportion of participants with low empathy levels, adjusting specialty and sex or specialty-adjusted. The adjusted prevalence of low empathy progressively increases, peaking in the final year of medical study, and shows a relative decrease among residents compared to six-year medical students (Pnon−linear<0.001).
Relationship between characteristics, family relationships, and empathy
Tables 2 and 3 detail the relationship between participant characteristics, family relationships, and empathy. Cronbach’s alpha of the relationship ratings within the family is 0.88, revealing a good internal consistency reliability. The unidimensionality of the relationship questionnaire was confirmed (Eigenvalue component 1: Eigenvalue component 2 = 4.34:0.98). The Kaiser–Meyer–Olkin measure of sampling adequacy was applied, yielding an overall index of 0.78, indicating sufficient data for factor analysis. Additionally, Bartlett’s test for sphericity confirmed that the intercorrelation matrix was factorable (χ² = 2604.33, p < 0.001). The factor loadings ranged from 0.35 to 0.97, all exceeding the threshold of 0.30. Significant differences in empathy were observed across various factors, including sex, educational level, specialty preference, paternal education level, and perceived family relationships, both past and present.
Logistic regression analysis for the associations factors of low empathy level
Table 4 presents the logistic regression analysis results for factors associated with low empathy levels. The model adjusted for sex, educational level, specialty preference, GPAX, household income, current family relationship, and MPI extroversion-introversion personality scores. Factors associated with lower empathy include being a resident (AOR: 3.01, 95% CI: 1.46 to 6.18), preferring a procedure-oriented specialty (AOR: 4.16, 95% CI: 1.54 to 11.18), having a household income over 200,000 baht (AOR: 2.97, 95% CI: 1.09 to 8.10), and rating the current family relationship as 8 or below (AOR: 1.79, 95% CI: 1.05 to 3.03).
Subgroup analysis was conducted to identify factors associated with lower empathy levels among residents, as shown in Table 5. Both procedure-oriented (AOR: 12.35, 95% CI: 3.08 to 49.57) and technology-oriented specialties (AOR: 2.93, 95% CI: 1.05 to 8.12) were linked to reduced empathy. Additionally, high GPAX scores above 3.5 (AOR: 3.46, 95% CI: 1.40 to 8.59) and rating family relationships as 8 or below (AOR: 3.70, 95% CI: 1.54 to 9.09) were associated with low empathy levels. However, household incomes over 200,000 baht were not significantly associated with low empathy in this analysis.
Linear regression analysis for the association factors with empathy level
Table 6 presents a multivariable linear regression analysis, indicating that being a non-binary gender (adjusted β = − 16.12, 95% CI: − 27.17 to − 5.07), a clinical student (adjusted β = − 4.76, 95% CI: − 8.80 to − 0.73), a resident (adjusted β = − 9.07, 95% CI: − 13.06 to − 5.07), and having a preference for procedure-oriented specialties (adjusted β = − 8.69, 95% CI: − 15.00 to − 2.39) are associated with lower empathy levels, consistent with findings from the logistic regression model. A subgroup analysis by educational level and specialty preference for the association between non-binary gender and empathy level is presented in Supplementary Table 3.
Discussion
This study successfully enrolled medical students and residents from a single-center medical college to investigate empathy trends across the professional continuum. After adjusting for specialty preferences and sex, we found that empathy scores were lowest in the final year of medical education and stabilized during residency. Additionally, factors such as residency status, preference for or current engagement in non-people-oriented specialties, high household income, poorer perception of family relationships, and a high GPAX among residents were associated with lower levels of empathy.
The average empathy score among medical students in this study was notably lower than those reported in other studies involving Thai medical students (110.1 ± 10.9 among pre-clinical students and 108.5 ± 11.5 among clinical students) and dental students (114.3 ± 13.1) [5, 38]. In contrast, a study among nurse students in Thailand revealed that empathy scores are relatively lower (89.8 ± 14.7) than in the present study [39]. This may highlight differences in empathy levels between health professionals responsible for patient management (e.g., physicians and dentists) and nurses involved in basic medical procedures and caregiving. However, further study might be needed, as previous research done in the US showed similar empathy levels between nurses and physicians [40].
To our knowledge, research on empathy among residents in Thailand is limited, making direct comparisons difficult. Among residents in this study, the average empathy score was 99.4 ± 15.0, with 37.1% classified as having low empathy. In contrast, a nationwide survey of 824 residents in Japan found an average JSE score of 103.6, slightly higher than the scores found in our study [17]. This highlights the need to maintain empathy among both medical students and resident groups in the population. Furthermore, a nationwide study among medical students in the United States revealed a relatively high average JSE score of 116.5 ± 10.9. In contrast, a study among medical students in the United Kingdom reported a JSE score of approximately 81, indicating possible differences in empathy levels across cultures [32, 41].
Consistent with prior research, our study observed a declining trend in empathy levels through the years of medical education [6, 7]. A key strength of our study is the inclusion of participants from second-year medical students to second-year residents, facilitating comparison across these groups from a single center. Empathy levels were found to be lowest among sixth-year medical students, stabilizing thereafter in residents. This decline may be attributed to factors such as high workload, mistreatment, unsuitable learning environments, and stress, which are known to reduce empathy levels [7]. Particularly, sixth-year medical students face a challenging 4-month externship in hospitals under the Ministry of Public Health, where they encounter first-hand patient care with minimal supervision by physicians they are not familiar with. The inability to adapt to increased stress and workload, especially in hospitals with a higher patient-to-doctor ratio in different provinces, may contribute to this trend [42].
Overall, procedure-oriented specialties are associated with lower empathy levels. Subgroup analysis further revealed that both procedure- and technology-oriented specialties correlate with lower empathy levels among residents. These findings are consistent with prior research indicating lower empathy levels among individuals in non-people-oriented specialties [14, 15, 17]. Although individuals in procedure-oriented specialties may not frequently interact with patients, those in technology-oriented fields often engage in patient contact. This includes tasks such as delivering bad news, taking histories, and giving treatment, where empathy is crucial in enhancing patient care [1]. Hence, strategies are needed to increase empathy among individuals in technology-oriented specialties. For example, Iramaneerat et al. have reported that dialogue workshops can improve understanding and empathy among the first-year residents of this institute [43]. Nevertheless, the preservation of increased empathy may be a significant challenge.
A good family relationship was also important to a higher empathy level [14, 15]. Parents may significantly influence their children’s empathy development by discussing emotions, rewarding caring behaviors, and modeling empathy [44]. However, higher-income families might exhibit lower empathy levels due to the independence wealth provides [45]. This independence can result in less concern for other’s feelings and a more self-centered outlook [45]. To counteract this, students could engage in empathetic leadership, genuinely connecting with and showing interest in others’ lives. This can be done by initiating a task for the student to ask employees about their lives and show genuine interest in their well-being. This might lead to increased empathy and a stronger emotional connection between students and faculty employees, leading to increased productivity and creativity [46].
A high GPAX was also associated with lower empathy among residents. The relationship between empathy and academic performance in medical students is complex and multifaceted. While some studies have identified a positive correlation between empathy and academic success, others have found no significant link [47]. This discrepancy may stem from the predominant focus on cognitive aspects among medical students, especially those with high grades [48]. In contrast, empathy is more closely aligned with soft skills in the affective domain, which are notably more challenging to assess [49, 50]. Therefore, placing greater emphasis on assessing affective domains may contribute to the long-term maintenance of empathy among medical students.
Enhancing empathy in the medical curriculum can involve several strategies. This includes hands-on learning through workshops and sharing patient stories, along with precise teaching methods like “Invite, listen, and summarize” [51]. Integrating empathy improving class into the curriculum by integrating subjects like Health Systems Science with varied activities and challenges can also be effective [51, 52]. It’s also important to reflect on these sessions afterward to process emotions and learn from them. Working together, students and staff can create relevant and engaging content [53]. Furthermore, emphasizing empathy as an intrinsic value, promoting cultural understanding and diverse interests, and teaching “deep acting” can cultivate authentic empathic connections [52]. Addressing any obstacles to empathy, especially in residency programs, is vital to prevent a decrease in empathy as students progress through their medical training.
Several factors associated with low empathy levels have been identified, but a constructive plan to address these factors is still lacking. Tavakol et al. have further reported that the barriers to empathy among medical students include a lack of role models, a high workload, and an emphasis on cognitive assessment in the medical curriculum [48]. Additionally, any plan to improve empathy should be customized to the specific context of each university. For behavioral change to occur, learners must be motivated and hold positive attitudes toward the desired change, recognizing its significant benefits [54, 55]. Behavioral theories emphasize the importance of a strong sense of belonging and autonomy for learners to adopt sustainable changes. Thus, strategy development should involve learners in co-creation processes [53].
The present study faced several limitations. First, it exclusively targeted medical students and residents from PCM and PMK, potentially limiting the generalizability of its findings to other medical colleges with different curricula. Second, the cross-sectional design precludes the determination of causality, and the paper-based data collection may result in some missing data, leading to the final regression model accounting for 332 (63.85%) participants. This may introduce potential volunteer bias. Nevertheless, the number of participants in the final model still exceeds the calculated sample size of 254. Third, the study did not account for other possible confounding factors, such as stress, anxiety, and burnout. Despite these limitations, a sensitivity analysis for unmeasured confounders demonstrated a relatively high E-value, suggesting a robust association between the variables of interest and empathy levels, as detailed in Supplementary Tables 1 and 2. Fourth, the ratings of family relationships are simplistic and may not fully capture the complexities of family function. Thus, further research might be needed to verify the association between family function and empathy. Fifth, the present questionnaire is subjective and self-perceived, which may lead to potential inaccuracies [56]. However, self-perception and self-awareness could also affect empathy, which is worth exploring [57].
Finally, the relatively low number of non-binary gender participants may lead to inconclusive findings regarding the relationship between non-binary gender and low empathy levels. To the best of our knowledge, data on this relationship is limited. Additionally, the results of the subgroup analyses may reflect the small sample size rather than the actual effect of an effect modifier. Moreover, the prevalence of non-binary individuals may be underestimated, and interpretations should be made with caution, given that non-binary participants in the present study accounted for only 13 individuals (2.5%), whereas a survey in Thailand suggests that non-binary individuals might comprise up to 9% of the population [58, 59]. This discrepancy highlights the potential for an inconclusive relationship and underestimates the true prevalence. This limitation underscores the necessity for further quantitative and qualitative research to validate the present study’s findings externally.
Conclusion
The present study successfully enrolled medical students and residents from a single institute, providing valuable insights into factors associated with low empathy. These include residency status, preference for non-people-oriented specialties, high household income, poorer family relationships, and a higher GPAX among residents. Despite non-binary individuals showing relatively lower empathy compared to binary genders, the small sample size and possible underestimation render this finding inconclusive, requiring further studies for confirmation. Additionally, empathy scores were lowest among sixth-year medical students. To address these factors, further planning should involve collaboration between students and teachers to maintain a high level of empathy throughout the medical curriculum.
Data availability
The datasets used and/or analyzed during the current study are available from the author upon reasonable request (contact Sethapong Lertsakulbunlue via Sethapong.ler@pcm.ac.th).
Abbreviations
- GPAX:
-
Cumulative grade point average
- JSE:
-
Jefferson Scale of Empathy
- MPI:
-
Maudsley Personality Inventory
- PCM:
-
Phramongkutklao College of Medicine
References
Casas RS, Xuan Z, Jackson AH, Stanfield LE, Harvey NC, Chen DC. Associations of medical student empathy with clinical competence. Patient Educ Couns. 2017;100:742–7.
Hojat M, Gonnella JS, Mangione S, Nasca TJ, Veloski JJ, Erdmann JB, et al. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ. 2002;36:522–7.
Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physiciansʼ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86:359–64.
Canale S, Del, Louis DZ, Maio V, Wang X, Rossi G, Hojat M, et al. The relationship between physician empathy and disease complications. Acad Med. 2012;87:1243–9.
Rojanasaku U, Jumroonrojana K, Saipanish R. Study of changes in medical students’ empathy to patients before and after the first clinical year in Ramathibodi Hospital. J Psychiatrist Association Thail. 2014;59(1):63–72.
Andersen FA, Johansen A-SB, Søndergaard J, Andersen CM, Assing Hvidt E. Revisiting the trajectory of medical students’ empathy, and impact of gender, specialty preferences and nationality: a systematic review. BMC Med Educ. 2020;20:52.
Neumann M, Edelhäuser F, Tauschel D, Fischer MR, Wirtz M, Woopen C, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86:996–1009.
DiLalla LF, Hull SK, Dorsey JK. Effect of gender, age, and relevant course work on attitudes toward empathy, patient spirituality, and physician wellness. Teach Learn Med. 2004;16:165–70.
Ferreira S, Afonso P, Ramos M. do R. Empathy and burnout: a multicentre comparative study between residents and specialists. J Eval Clin Pract. 2020;26:216–22.
Alosaimi FD, Kazim SN, Almufleh AS, Aladwani BS, Alsubaie AS. Prevalence of stress and its determinants among residents in Saudi Arabia. Saudi Med J. 2015;36:605–12.
Soares DS, Chan L. Stress and wellbeing of junior doctors in Australia: a comparison with American doctors and population norms. BMC Med Educ. 2016;16:183.
Sulzer SH, Feinstein NW, Wendland CL. Assessing empathy development in medical education: a systematic review. Med Educ. 2016;50:300–10.
Hojat M. Empathy in health professions education and patient care. Cham: Springer International Publishing; 2016.
Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159:1563–9.
Hojat M, Zuckerman M, Magee M, Mangione S, Nasca T, Vergare M, et al. Empathy in medical students as related to specialty interest, personality, and perceptions of mother and father. Pers Individ Dif. 2005;39:1205–15.
Lieu TA, Schroeder SA, Altman DF. Specialty choices at one medical school: recent trends and analysis of predictive factors. Acad Med. 1989;64:622–9.
Watari T, Houchens N, Nishizaki Y, Kataoka K, Otsuka T, Nakano Y, et al. Empathy competence and future specialty among medical residents in Japan: a nationwide cross-sectional study. Sci Rep. 2023;13:13742.
Toussaint L, Webb JR. Gender differences in the relationship between empathy and forgiveness. J Soc Psychol. 2005;145:673–85.
Newman PA, Reid L, Tepjan S, Akkakanjanasupar P. LGBT + inclusion and human rights in Thailand: a scoping review of the literature. BMC Public Health. 2021;21:1816.
Devlin HC, Zaki J, Ong DC, Gruber J. Not as good as you think? Trait positive emotion is Associated with increased self-reported Empathy but decreased empathic performance. PLoS ONE. 2014;9:e110470.
Dávila Pontón Y, Díaz-Narváez VP, Vélez Calvo X, Celleri Gomezcoello A, Aguilera Muñoz J, Calzadilla Núñez A, et al. Empatía Y funcionamiento familiar en estudiantes de medicina de la Universidad De Azuay, Cuenca, Ecuador. Salud Uninorte. 2022;36:571–86.
OLSON DH, RUSSELL CS. Circumplex model of marital and family systems: Vl. Theoretical update. Fam Process. 1983;22:69–83.
Shaffer JW, Duszynski KR, Thomas CB. Family attitudes in youth as a possible precursor of cancer among physicians: a search for explanatory mechanisms. J Behav Med. 1982;5:143–63.
Saarinen AI, Keltner D, Dobewall H, Lehtimäki T, Keltikangas-Järvinen L, Hintsanen M. The relationship of socioeconomic status in childhood and adulthood with compassion: a study with a prospective 32-year follow-up. PLoS ONE. 2021;16:e0248226.
Bhatia G, Shetty JV. Trends of change in empathy among indian medical students: a two-year follow-up study. 2022;45:162–7. https://doi.org/10.1177/02537176221104688
Baig KS, Hayat MK, Khan MAA, Humayun U, Ahmad Z, Khan MA. Empathy levels in medical students: a single center study. Cureus. 2023;15.
Aomatsu M, Otani T, Tanaka A, Ban N, Dalen J. Medical students′ and residents′ conceptual structure of empathy: a qualitative study. Educ Health. 2013;26:4.
Huynh A, Savitski J, Kirven M, Godwin J, Gil KM. Effect of medical students’ experiences with residents as teachers on clerkship assessment. J Grad Med Educ. 2011;3:345–9.
Sathaporn K, Pitanupong J. Factors associated with the improvement of the empathy levels among clinical-year medical students in Southern Thailand: a university-based cross-sectional study. BMC Psychol. 2022;10:128.
Jensen AR. The Maudsley personality inventory. Acta Psychol (Amst). 1958;14:314–25.
Suwanlert S. Some personality characteristics of Thai students. In: Youth, socialization, and mental health. University of Hawaii; 1974. pp. 75–84.
Hojat M, DeSantis J, Shannon SC, Mortensen LH, Speicher MR, Bragan L, et al. The Jefferson scale of empathy: a nationwide study of measurement properties, underlying components, latent variable structure, and national norms in medical students. Adv Health Sci Educ. 2018;23:899–920.
Jumroonrojana K, Zartrungpak S. Development of the Jefferson Scale of physician empathy-student version (Thai version). J Psychiatric Association Thail. 2012;57(2):213–24.
Kataoka HU, Tokinobu A, Fujii C, Watanabe M, Obika M. Eleven years of data on the Jefferson scale of empathy – medical student version: Japanese norm data and tentative cutoff scores. BMC Med Educ. 2023;23:81.
Hojat M, Louis DZ, Maxwell K, Markham F, Wender R, Gonnella JS. Patient perceptions of physician empathy, satisfaction with physician, interpersonal trust, and compliance. Int J Med Educ. 2010;1:83–7.
Linden A, Mathur MB, VanderWeele TJ. Conducting sensitivity analysis for unmeasured confounding in observational studies using E-values: the evalue package. Stata Journal: Promoting Commun Stat Stata. 2020;20:162–75.
Lertsakulbunlue S, Sangkool T, Bhuriveth V, Mungthin M, Rangsin R, Kantiwong A, et al. Associations of triglyceride-glucose index with hyperuricemia among Royal Thai Army personnel. BMC Endocr Disord. 2024;24:1–13.
Detsomboonrat P, Theppanich S, Banyen S, Hongviphat S, Khamnil Y, Lapauthaya K, et al. Empathy level towards patients among Thai dental students: a cross-sectional study. BMC Oral Health. 2023;23:184.
Sirisophon A, Wongupparaj P. Factor analysis of empathy inventory for nursing students. J NAT North. 2024;30(1):115–33.
Fields SK, Hojat M, Gonnella JS, Mangione S, Kane G, Magee M. Comparisons of nurses and physicians on an operational measure of empathy. Eval Health Prof. 2004;27:80–94.
Austin EJ, Evans P, Magnus B, O’Hanlon K. A preliminary study of empathy, emotional intelligence and examination performance in MBChB students. Med Educ. 2007;41:684–9.
Lertsakulbunlue S, Suebtuam R, Eamchotchawalit T, Chantkran W, Chaisakul J. Clinical profile and pharmacological management of snakebites in community care units: a retrospective study using two military hospital databases in South Thailand. Trop Med Infect Dis. 2023;8.
Iramaneerat C, Imjaijitt w, Pongpakatien J, Kitthaweesin T, Mahagita C. Dialogue workshop helps improve residents’ understanding of others. RTAMedJ. 2019;72(3):201–8.
Lam CB, Solmeyer AR, McHale SM. Sibling relationships and empathy across the transition to adolescence. J Youth Adolesc. 2012;41:1657–70.
Jiménez-Moya G, Luengo Kanacri BP, Cumsille P, Martínez ML, Berger C. You may have my help but not necessarily my care: the effect of social class and empathy on prosociality. Front Psychol. 2021;12.
Kahneman D, Deaton A. High income improves evaluation of life but not emotional well-being. Proc Natl Acad Sci. 2010;107:16489–93.
Javaeed A, Abdul Rasheed A, Manzoor A, Ain Q-T, Raphael D, Costa P, Ghauri SK. Empathy scores amongst undergraduate medical students and its correlation to their academic performance. J Adv Med Educ Prof. 2022;10:99–104.
Tavakol S, Dennick R, Tavakol M. Medical students’ understanding of empathy: a phenomenological study. Med Educ. 2012;46:306–16.
Malau-Aduli BS, Hays RB, D’Souza K, Saad SL, Rienits H, Celenza A, et al. Twelve tips for improving the quality of assessor judgements in senior medical student clinical assessments. Med Teach. 2023;45:1228–32.
Pangaro L, ten Cate O. Frameworks for learner assessment in medicine: AMEE guide 78. Med Teach. 2013;35:e1197–210.
McNally G, Haque E, Sharp S, Thampy H. Teaching empathy to medical students. Clin Teach. 2023;20.
Costa-Drolon E, Verneuil L, Manolios E, Revah-Levy A, Sibeoni J. Medical students’ perspectives on empathy: a systematic review and metasynthesis. Acad Med. 2021;96:142–54.
Könings KD, Mordang S, Smeenk F, Stassen L, Ramani S. Learner involvement in the co-creation of teaching and learning: AMEE guide 138. Med Teach. 2021;43:924–36.
Lertsakulbunlue S, Kittisarapong P, Pikulkaew S, Pusayapaibul P, Tangtongsoonthorn A, Wichaiboon C et al. What sustains mask-wearing behavior among elders in a rural community in the post-COVID-19 era: an exploratory mixed-methods study. Behav Sci. 2023;13.
Lertsakulbunlue S, Thammasoon K, Jongcherdchootrakul K, Sakboonyarat B, Kantiwong A. Practices, perceptions, attitudes, barriers and motivation and its impacts on research publication. Asia Pac Scholar. 2023;8:23–35.
Hojat M, Mangione S, Nasca TJ, Cohen MJM, Gonnella JS, Erdmann JB, et al. The Jefferson scale of physician empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61:349–65.
Hamaideh SH, Abuhammad S, Khait AA, Al-Modallal H, Hamdan-Mansour AM, Masa’deh R, et al. Levels and predictors of empathy, self-awareness, and perceived stress among nursing students: a cross sectional study. BMC Nurs. 2024;23:131.
Why Thailand is an Attractive Country for LGBTQIA + Expats. - Pacific Prime Thailand’s Blog. https://www.pacificprime.co.th/blog/why-thailand-is-an-attractive-country-for-lgbtqia-expats/. Accessed 6 Aug 2024.
Pride month 2023: 9% of adults identify as LGBT+ | Ipsos. https://www.ipsos.com/en/pride-month-2023-9-of-adults-identify-as-lgbt. Accessed 6 Aug 2024.
Acknowledgements
We express our gratitude to the Phramongkutklao College of Medicine and its esteemed academic leaders, whose active support was vital for completing this work. Their names are too numerous to mention individually, but their involvement was instrumental in making this project possible. We express our gratitude to Asst. Prof. Somsong Suwanlert and Ms. Supavadee Nuanmanee, President of The Thai Clinical Psychologist Association, thank you for allowing us to use the Thai version of the Maudsley Personality Inventory.
Funding
The author(s) reported funding from the Phramongkutklao College of Medicine.
Author information
Authors and Affiliations
Contributions
The concept for the study was developed by SL, CK, PK, KT, SP, VB, VT, AK and CM. SL, CK, PK, KT, VB, VT and CM collected the data, SL and AK analyzed the data, and SL, CK and PK wrote the first draft. All authors contributed and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Medical Department Ethics Review Committee for Research in Human Subjects, Institutional Review Board, Royal Thai Army (RTA) (Approval no. S024q/66), following international guidelines such as the Declaration of Helsinki, the Belmont Report, CIOMS Guidelines, and the International Conference on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use - Good Clinical Practice. Informed consent was obtained from all subjects with permission from the Institutional Review Board, RTA Medical Department.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lertsakulbunlue, S., Kiatsrithanakorn, C., Kittisarapong, P. et al. Declining empathy trends throughout medical curriculum and association factors of low empathy among medical students and residents: a single center study. BMC Med Educ 24, 951 (2024). https://doi.org/10.1186/s12909-024-05962-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-024-05962-6