Abstract
Purpose
Empathy is an important skill for physicians as it can lead to improved patient outcomes and satisfaction. This study assessed self-reported empathy by medical students across all four years of medical school and potential differences in empathy across students interested in different subspecialties.
Method
All medical students enrolled at New York Medical College in August 2020 were invited to participate in this study. Participants completed the student version of the Jefferson Scale of Empathy.
Results
A total of 179 medical students participated. Mean empathy score in fourth-year students was significantly lower than that in first-year students. Mean empathy score was greatest among students interested in Pediatrics and was greater in participants who identified as women.
Conclusions
Self-reported empathy may be lower in upper-year medical students when compared to lower-year students. The potential reasons for lower empathy in the later years of training are discussed. A systematic curriculum for teaching and maintaining empathy should be developed and uniformly implemented across medical schools to combat a potential decline in empathy.
Similar content being viewed by others
Introduction
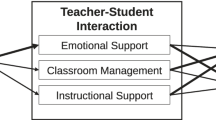
Empathy can be defined as the ability to imagine and understand the thoughts, perspective, and emotions of another person [1]. Some individuals believe empathy to be a cognitive attribute, whereas others assert that empathy is either an emotional characteristic or a combination of cognitive and emotional functions [2, 3]. One thing is widely agreed upon, empathy is a complex multi-dimensional concept that has many components and steps [4, 5]. Clinical empathy, a term used for the practice of empathy by healthcare providers, goes further than the term’s basic definition and incorporates an individual’s ability to communicate an understanding of the patient’s thoughts, perspective, and emotions to the patient and check for accuracy, in addition to acting on this understanding in a therapeutic manner [5].
Empathy is widely recognized to be an important characteristic for healthcare providers to possess and is key to fostering interpersonal relationships between patients and physicians. Empathy has also been shown to improve both patient and physician satisfaction, improve diagnostic accuracy, enhance patient compliance, and have a positive role in clinical outcomes [6,7,8,9]. As a result, clinical empathy is an essential skill that medical students must develop and maintain throughout their training to succeed as a physician. As a skill that likely has a significant cognitive component, empathy can be enhanced through education [10]. Just like any other skill, continuous and deliberate practice is a substantial feature of the training required to cement empathy in trainees [11]. The literature suggests that there are several methods to train students to be empathic healthcare providers, such as having students write a reflective essay on their personal experience with illness, or from the point-of-view of another individual with an illness [10, 12, 13]. Another example of how empathy can be taught is through experiential/simulated learning interventions, such as simulations of auditory hallucinations via headphones and a simulated experience of changes that occur during aging including decreased mobility, loss of vision and hearing, and decreased manual dexterity [14, 15].
Prior studies have shown that self-reported empathy levels tend to decrease during medical school training [16,17,18], which may be explained by several theories. One theory is that increased emotional distress due to high workload and expectations, burnout, and depression are all direct contributors to a decline in empathy during medical training [19, 20]. Another theory is that medical students may be mistreated at some point in their medical school education, leading to cynicism and what has been termed “traumatic de-idealization” [21, 22]. Due to the high educational demands placed by medical schools on their students, formally incorporating empathy training throughout the formal curriculum has posed a challenge for many schools. Thus, knowledge of when empathy is most likely to decline in an individual’s medical school education is crucial in providing a timely intervention to prevent this decline and preferably increase empathy in students.
Based on existing research [16,17,18], as well as observations made by the investigators, we believe that an inverse relationship may exist between duration of medical training and self-reported empathy. Therefore, we sought to investigate this relationship in a population of medical school students utilizing a self-report survey of empathy. We also sought to investigate potential differences in empathy across groups of students based on their specialties of interest, to determine if individuals going into certain fields of medicine report differing levels of self-rated empathy.
Methods
Study Participants
All medical students at New York Medical College (NYMC), a private medical school in the northeast of the USA, were emailed regarding participation in this research study at the beginning of the 2020–2021 academic year. A link to complete the Jefferson Scale of Empathy (JSE) student version was sent to all students matriculated in the M.D. program using Google Forms. Subjects were informed that participation in the study was completely voluntary and responses were anonymous. Variables collected included age group, gender, year of medical school, specialty of interest, and JSE score. The results were accessed by the investigators and data from the survey was entered into a preformatted spreadsheet stored on password-protected computers. Participants gave their informed consent by choosing to complete the JSE and clicking submit after having been informed of the risks, benefits, and details of the study in the initial email. Surveys were open for a total of 4 weeks. There were no exclusion criteria. This study was approved by the Institutional Review Board (IRB) of New York Medical College (IRB Protocol ID: 12,956).
Assessments and Data Collection
The student version of the JSE was used to measure empathy in study participants. The JSE is a 20-item self-rated questionnaire which queries level of empathy using a 7-point Likert scale (1 = Strongly Disagree, 7 = Strongly Agree) and statements such as “Understanding body language is as important as verbal communication in physician patient relationships,” “Physicians should try to stand in their patients' shoes when providing care to them,” and “Physicians should try to think like their patients in order to render better care” [23]. Half of the survey items are positively worded and directly scored while the other half are negatively worded and thus reverse scored. The maximum score on the JSE is 140 and the minimum score is 20. Other data collected as part of the JSE survey included gender, age (grouped into categories that included < 22, 22–24, 25–27, 28–30, 31–33, 34–36, > 36), year of medical school, and specialty of interest. Of note, the JSE utilizes multiple surgical subspecialty options for participants to choose from, including “Surgery” (incorporating general surgery, transplant surgery, trauma surgery, vascular surgery, colorectal surgery, cardiothoracic surgery, undecided, and other), “Neurosurgery,” “Orthopaedic Surgery,” and “Plastic Surgery.” For the purposes of this study, all subcategories of surgery were combined.
Statistical Analyses
The association between year of medical school and mean JSE score was assessed using Spearman’s rho test, as the year of medical school variable was not normally distributed. Independent samples t tests were performed to assess differences in mean JSE score between academic years, gender, and specific specialties of interest compared to the rest of the study population. Cohen’s d was calculated as a measure of effect size for all independent samples t-tests performed. Cohen’s classification of effect sizes was as follows: small (d = 0.10 to.39), moderate (d = 0.40 to.69), or large (d > 0.70) [24]. If an independent samples t-test comparing mean empathy score across two different years of medical school was found to be significant, an analysis of covariance (ANCOVA) was performed to compare the two means while adjusting for gender as a covariate, a known modifier of empathy score [6, 25]. T-tests were only performed for specialties of interest in which at least ten study participants indicated an interest in pursuing a career in that specialty. For any independent samples t-test comparing specific specialties to the rest of the study population that was statistically significant, an ANCOVA was then performed adjusting for gender and year of medical training as covariates. In the analysis performed assessing the difference in mean JSE score in those intending to pursue a career in a field of surgery compared to the rest of the study population, all surgical subspecialties were combined into one group. All analyses were performed using IBM SPSS Statistics Version 28.0 (IBM Corp, Armonk, NY, USA). Data are presented as mean ± standard deviation (SD) unless otherwise stated.
Results
Study Population Characteristics
A total of 179 medical students across all 4 years of medical school participated in this research, equaling a total response rate of 21.3% (179 of 840 total medical students). Forty-nine participants (27.4%) were in their first year of medical school, 52 (29.1%) were in their second year, 46 (25.7%) were in their third year, and 32 (17.9%) were in their fourth year. One hundred nine study participants (60.9%) identified as a woman, 68 participants (38.0%) identified as a man, and two (1.1%) preferred not to indicate their gender. Based on a chi-square analysis, the proportion of participants who identified as a woman was not significantly different among different years of medical school in our study population (χ2 = 5.99, p = 0.112). The most common age group in this study was 25–27 years old (52%).
The most common specialty preferences among survey respondents were as follows: undecided (n = 49, 27.4%), internal medicine/medicine subspecialties (n = 20, 11.2%), pediatrics (n = 17, 9.5%), emergency medicine (n = 14, 7.8%), and surgery/surgical subspecialties (n = 13, 7.3%) (see Table 1 for a complete list of all specialties).
Mean JSE score in the overall study population was 119.6 ± 8.4 (92–140). JSE scores were normally distributed in this study population based on a non-significant Kolmogorov–Smirnov test (p = 0.20) and Shapiro–Wilk test (p = 0.08).
Relationship Between Year of Medical Training and Empathy Score
In a non-parametric correlational analysis, a significant negative association was observed between years of medical school education and empathy score (Spearman’s ρ = − 0.217, p = 0.004). In an independent samples t-test, mean empathy score was significantly lower in first semester fourth-year medical students compared to first semester first-year medical students (t = 2.500, p = 0.014, Cohen’s d = 0.568, Table 2). A Cohen’s d of 0.568 indicates a moderate effect size [24]. After correcting for gender as a covariate using an ANCOVA, mean empathy score was still significantly lower in fourth-year students when compared to first-year students (F = 5.45, p = 0.022). Mean empathy score in first-year students was 121.4 ± 7.7 (100–135) and mean empathy score in fourth-year students was 116.8 ± 8.5 (102–140; Fig. 1 and Table 1). There were no other statistically significant differences between mean empathy scores across other years of medical school training (Table 2). The largest difference in mean empathy score in this study population between two consecutive classes was between students beginning their third year of medical school and students beginning their fourth year of medical school.
Relationship Between Specialty of Interest and Empathy Score
In this study population, students interested in pediatrics (n = 17) had a significantly higher mean empathy score compared to the rest of the study population (t = 2.139, p = 0.034, Cohen’s d = 0.545, Table 2 and Fig. 2). This finding remained statistically significant after adjusting for gender and year of medical training (F = 4.15, p = 0.043). Mean empathy score in the pediatrics subgroup was 123.7 ± 9.5 compared to a mean of 119.2 ± 8.2 in the rest of the study population. No other specialty of interest that was assessed was found to have a significantly different mean empathy score when compared to the rest of the study population (Table 2 and Fig. 2). Participants who indicated they were undecided in their choice of career specialty did not have a significantly different mean empathy score compared to the rest of the study population (Table 2 and Fig. 2).
Relationships Between Gender, Age, and Empathy Score
In this study population, identifying as a woman was significantly associated with higher mean empathy score (t = 2.887, p = 0.004, Cohen’s d = 0.446, Table 2). Mean empathy score in those who identified as a woman was 121.1 ± 7.6 compared to a mean empathy score in those who identified as a man of 117.4 ± 9.2. Age group was not significantly associated with differences in mean empathy score (F = 0.954, p = 0.448) in this study population.
Discussion
In this study, we observed a significant negative correlation between years of medical school education and self-rated empathy as measured by the JSE. Mean empathy score was significantly lower among fourth-year medical students when compared to first-year medical students. In addition, mean empathy scores were significantly higher in individuals who identified as a woman and in students who indicated they wished to pursue a career in pediatrics in our study population.
The results of this research study support previous reports that self-reported empathy may decrease during medical school, particularly during the clinical years of training [16, 17]. In a study by Hojat et al., in which the JSE was administered to 125 third-year students at the beginning and end of the academic year, they observed a significant decrease in mean JSE score that occurred after the third year of medical school [26]. In a cross-sectional study by Chen et al., 81% of medical students at Boston University completed the JSE and mean empathy scores were lower in upper-year students compared to lower-year students [27]. In a longitudinal study by Newton et al., in which vicarious empathy (a visceral empathic response) as measured by the Balanced Emotional Empathy Scale was assessed at the beginning of each year of medical school, it was observed that empathy declined significantly over the course of medical school with the greatest decrease occurring after the third and first years [18]. Taken altogether, the result in our current study showing lower self-rated empathy in later years of medical school education is consistent with the existing published body of evidence.
Another finding from our study was the mean JSE score was higher in those who identified as a woman. Higher self-reported empathy among those who identify as a woman is consistent with other published reports [6, 25]. In our study population, there was a higher proportion of those who identified as a woman in the second- and third-year student cohorts. As the differences in these gender proportions were not significantly different in a chi-square analysis, we believe the finding that self-reported empathy was lower in the upper-year classes was not driven by differences in gender proportions among these groups in our study population. Furthermore, when gender was controlled for as a covariate, mean JSE score was still significantly lower in fourth-year students compared to first-year students.
In our study population, those interested in pursuing a career in pediatrics had a higher mean self-rated empathy score than other medical students. Other studies have grouped students into those interested in “people-oriented” specialties, such as pediatrics, versus “technology-oriented” specialties [28, 29]. Many, but not all of these studies, have reported a higher mean empathy score in students interested in pursuing “people-oriented” specialties [28,29,30]. Newton et al. observed that students pursuing what they termed “core” specialties (internal medicine, family medicine, obstetrics and gynecology, pediatrics, and psychiatry) had a higher mean empathy score than students pursuing “noncore” specialties (all other specialties such as surgery and surgical subspecialties, anesthesiology, dermatology, neurology, and radiology) [18].
In our study population, the majority of participants were between 22 and 27 years of age. We did not observe a significant difference in mean JSE score among different age groups in our study population; however, there was not a lot of variation in age in this study sample. In other published research, cognitive empathy, the capacity to take the mental perspective of others and to understand their thoughts and feelings, tends to be higher in younger adults in their 20 s when compared to middle-aged and older adults [31]. Emotional empathy, the capacity to feel compassion or similar emotions to what another person is feeling, may not be different across age groups [31]. Thus, as most participants in this study are young adults, they likely tended to start their medical school education with higher self-reported empathy than the general population. Having started at relatively high levels of self-reported empathy, perhaps this allowed for more room for change in a negative direction over the course of their medical education.
Clinical empathy is an important skill for physicians to develop and maintain to provide better patient-centered care and improve clinical and patient-centered outcomes [7, 8]. It is concerning that the current body of evidence suggests that empathy tends to be lower in more advanced students compared to less advanced students. Multiple theories have been postulated for why this phenomenon occurs, especially during the clinical years. Increased exposure to real-life morbidity and mortality during the clinical years can lead to a de-sensitization effect in which students have decreased emotional response to pain and suffering over time [32]. Indeed, downregulation of sensory processing elicited by perceiving pain in others has been shown to occur in physicians with many years of clinical experience [32, 33]. Another theory that may explain the lower empathy observed in more advanced medical students is that students’ expectations about medical practice may be unrealistic going into their clinical training years [34]. Students may enter the immersive learning environment of clinical training with unrealistic expectations that most illnesses can be cured, that there is always a clear “right thing to do,” that all physicians and healthcare providers act in the best interest of their patients and have no other influences, and that once a treatment plan is in place it is easy for the patient to follow it [34]. It is postulated that once a student enters clerkship training and realizes that the reality of practice is different from what they envisioned, this incongruence can lead to significant stress and the utilization of defense mechanisms such as detached concern and decreased empathy [35]. Another potential cause may be increased emotional distress experienced during medical school due to factors such as high workload and expectations, reduced perceived quality of life, financial burden due to student loans, burnout, and depression [19, 20, 36]. Research has shown that medical student debt levels are associated with decreased overall well-being and poorer academic outcomes [36]. As higher self-reported empathy has been associated with positive well-being, it is logical that medical students who experience diminished well-being have lower levels of self-rated empathy [37]. Furthermore, practicing clinical empathy is an effortful skill that requires a high level of cognitive capacity and takes significant time and cognitive resources to practice which can be hard to commit to and maintain with the high workload of medical school [38].
This all begs the question, “what can be done to enhance empathy in medical school?” Perhaps there are certain strategies for teaching empathy and specific time points within an individual’s medical education that can be targeted to increase or at least prevent a decline in empathy in medical students before they begin their careers as physicians. As the largest decline in empathy may occur during the first clinical year of training, the most successful targeted approach may be to focus on enhancing empathy in students immediately prior to and during their first clinical year. Multiple methods for teaching and enhancing empathy in medical school have been proposed and shown to be effective in increasing self-rated empathy levels in students, many of which are well-received by students [10]. Some examples include exercises focusing on understanding patient narratives such as writing exercises, drama exercises, and experiential learning/simulation exercises. In a review on empathy and how it can be sustained during medical school clerkships, Benbassat and Baumal propose two changes they believe can significantly enhance empathy [4]. First, they emphasize the importance of teaching and reinforcing the patient-centered interview technique, as opposed to use of the disease-centered interview. This includes promoting strategies such as letting the patient talk without interruption, use of mostly open-ended questions at the beginning of the interview, and directly asking the patient questions such as “What is bothering you the most?” or “How does this make you feel?” The authors argue that an effective patient-centered interview encourages the patient to share their concerns and sources of distress, which is necessary for the physician to achieve clinical empathy. Second, the authors propose a reimagining of core clinical training from a primarily hospital-based setting to one that includes more primary care, home care, and hospice care settings. They assert that these settings are more conducive to promoting empathy as there are more opportunities for students to build longer-term relationships with patients and directly observe how illness can impact patients’ everyday lives.
One limitation of this current study is that students from only a single medical school were sampled, thus limiting the generalizability of these results to other schools in different regions, countries, and continents. Furthermore, only 21% of students at this medical school agreed to participate in this research study by completing the JSE. Our response rate of 21% and sample size of 179 participants is smaller than many other studies on this topic. Participation bias in our sample must be considered, in which individuals who agree to participate in research are likely to disproportionately possess certain characteristic traits, which may include traits related to empathy. In addition, data collection occurred during the COVID-19 pandemic, which limited some clinical exposure in that third- and fourth-year students were removed from the clinical setting from March 2020 until June 2020. Decreased face-to-face time with patients, peers, and supervisors may have contributed to reduced self-reported empathy; however, we do not suspect that the observed findings from this study were largely COVID-related as the majority of clinical rotations in the 2019–2020 academic year were not affected by the pandemic as it began late in the academic year. Additionally, survey responses were collected after resuming in-person clinical rotations.
Response bias must also be kept in mind, as study participants may tend to respond inaccurately or falsely to questions on self-reported questionnaires. However, a strength of this current study is the use of a well-validated tool for measuring empathy, the Jefferson Scale of Empathy (student version). Despite being a self-rated questionnaire, this measurement tool has been used in many research studies across a wide range of populations and is considered to be an accurate measurement tool for empathy [25, 39]. The cross-sectional design of this current research study restricts the ability to infer causation from correlations observed in this study. However, as data were sampled from students in all four years of medical school, it offers an aspect of multiple time points in medical school education to this research. Finally, the analyses of differences in empathy across specialties were limited by relatively small subgroups sizes, as there were twenty different options for specialties to choose from which significantly spread out the total sample. For example, the subgroup of students in this study who indicated an interest in pursuing psychiatry comprised of only ten students.
Conclusion
Empathy among medical students tends to be lower in upper-year medical students compared to lower-year students. This is concerning as clinical empathy is considered a core component of medical professionalism and can lead to improved patient outcomes and patient satisfaction with the healthcare system as well as improved physician job satisfaction. Creation of a standardized empathy curriculum for medical schools, targeted immediately before and during the clinical years, may be the most effective intervention to prevent a decline in empathy among medical students during their training. Multiple methods for teaching and enhancing clinical empathy in medical students have been shown to be effective and are well-received by students. However, more research is needed to determine which methods are the most effective and produce the longest-lasting effects on enhancing empathy. Therefore, the authors believe that medical schools must place a greater effort on teaching and enhancing clinical empathy in students to benefit future patients as well as the well-being of the students throughout their professional careers.
Data Availability
The data that support the findings of this study are available from the corresponding author, SL, upon reasonable request.
References
Decety J. Empathy in Medicine: What It Is, and How Much We Really Need It. Am J Med. 2020;133(5):561–6.
Basch MF. Empathic understanding: a review of the concept and some theoretical considerations. J Am Psychoanal Assoc. 1983;31(1):101–26.
Davis MH. Measuring individual differences in empathy: Evidence for a multidimensional approach. J Pers Soc Psychol. 1983;44(1):113–26.
Benbassat J, Baumal R. What is empathy, and how can it be promoted during clinical clerkships? Acad Med. 2004;79(9):832–9.
Mercer SW, Reynolds WJ. Empathy and quality of care. Br J Gen Pract. 2002;52(Suppl):S9-12.
Gleichgerrcht E, Decety J. Empathy in clinical practice: how individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PLoS ONE. 2013;8(4): e61526.
Kim SS, Kaplowitz S, Johnston MV. The effects of physician empathy on patient satisfaction and compliance. Eval Health Prof. 2004;27(3):237–51.
Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63(606):e76-84.
Hojat M, et al. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359–64.
Batt-Rawden SA, et al. Teaching empathy to medical students: an updated, systematic review. Acad Med. 2013;88(8):1171–7.
Wündrich M, et al. Empathy training in medical students - a randomized controlled trial. Med Teach. 2017;39(10):1096–8.
DasGupta S, Charon R. Personal illness narratives: using reflective writing to teach empathy. Acad Med. 2004;79(4):351–6.
Shapiro J, et al. Point-of-view writing: A method for increasing medical students’ empathy, identification and expression of emotion, and insight. Educ Health (Abingdon). 2006;19(1):96–105.
Bunn W, Terpstra J. Cultivating empathy for the mentally ill using simulated auditory hallucinations. Acad Psychiatry. 2009;33(6):457–60.
Varkey P, Chutka DS, Lesnick TG. The Aging Game: improving medical students’ attitudes toward caring for the elderly. J Am Med Dir Assoc. 2006;7(4):224–9.
Hojat M, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–91.
Neumann M, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86(8):996–1009.
Newton BW, et al. Is there hardening of the heart during medical school? Acad Med. 2008;83(3):244–9.
Brazeau CM, et al. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85(10 Suppl):S33–6.
Thomas MR, et al. How do distress and well-being relate to medical student empathy? A multicenter study. J Gen Intern Med. 2007;22(2):177–83.
Kay J. Traumatic deidealization and the future of medicine. JAMA. 1990;263(4):572–3.
Chisholm LP, et al. Evaluation of Racial Microaggressions Experienced During Medical School Training and the Effect on Medical Student Education and Burnout: A Validation Study. J Natl Med Assoc. 2021;113(3):310–4.
Hojat M, et al. The Jefferson Scale of Physician Empathy: Development and Preliminary Psychometric Data. Educ Pscyhol Meas. 2001;61(2):349–65.
Cohen J. Statistical Power Analysis. Curr Dir Psychol Scie. 1992;1(3):98–101.
Hojat M, et al. The Jefferson Scale of Empathy: a nationwide study of measurement properties, underlying components, latent variable structure, and national norms in medical students. Adv Health Sci Educ Theory Pract. 2018;23(5):899–920.
Hojat M, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004;38(9):934–41.
Chen D, et al. A cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007;22(10):1434–8.
Guilera T, et al. Empathy and big five personality model in medical students and its relationship to gender and specialty preference: a cross-sectional study. BMC Med Educ. 2019;19(1):57.
Santos MA, et al. Empathy differences by gender and specialty preference in medical students: a study in Brazil. Int J Med Educ. 2016;7:149–53.
Mostafa A, et al. Empathy in undergraduate medical students of bangladesh: psychometric analysis and differences by gender, academic year, and specialty preferences. ISRN Psychiatry. 2014;2014: 375439.
Beadle JN, de la Vega CE. Impact of Aging on Empathy: Review of Psychological and Neural Mechanisms. Front Psychiatry. 2019;10:331.
Decety J, Yang CY, Cheng Y. Physicians down-regulate their pain empathy response: an event-related brain potential study. Neuroimage. 2010;50(4):1676–82.
Cheng Y, et al. Expertise modulates the perception of pain in others. Curr Biol. 2007;17(19):1708–13.
Schrauth M, et al. Self-image, real physician’s and ideal physician’s image: a comparison of medical students 1981 and 2006. Psychother Psychosom Med Psychol. 2009;59(12):446–53.
Werner ER, Korsch BM. The vulnerability of the medical student: posthumous presentation of L.L. Stephens’ ideas. Pediatrics. 1976;57(3):321–8.
Pisaniello MS, et al. Effect of medical student debt on mental health, academic performance and specialty choice: a systematic review. BMJ Open. 2019;9(7): e029980.
Grühn D, et al. Empathy across the adult lifespan: Longitudinal and experience-sampling findings. Emotion. 2008;8(6):753–65.
Decety J, Jackson PL. The functional architecture of human empathy. Behav Cogn Neurosci Rev. 2004;3(2):71–100.
Williams B, Beovich B. A systematic review of psychometric assessment of the Jefferson Scale of Empathy using the COSMIN Risk of Bias checklist. J Eval Clin Pract. 2020;26(4):1302–15.
Acknowledgements
The authors would like to express their gratitude to Thomas Jefferson University, Center for Research in Medical Education & Health Care, for allowing use of the Jefferson Scale of Empathy.
Funding
No funding was used or obtained to conduct this study. The authors were granted permission for use of the Jefferson Empathy Scale by Thomas Jefferson University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
This study was approved by the Institutional Review Board of New York Medical College (IRB Protocol ID: 12956).
Informed Consent
Study participants were informed that they were participating in a research study by completing a survey measuring empathy, that the process is anonymous, and that they were not required to complete the survey and were able to opt out at any time.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dinoff, A., Lynch, S., Hameed, A.S. et al. When Did the Empathy Die?. Med.Sci.Educ. 33, 489–497 (2023). https://doi.org/10.1007/s40670-023-01768-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40670-023-01768-1