Abstract
Introduction
Children may require durable central venous catheters (CVCs) for various reasons. CVC-related integrity complications are common and can often be repaired at the bedside to increase lifetime. Variability in repair techniques can lead to complications, including the need for repeat repair and Central Line Associated Blood Stream Infection (CLABSI).
Methods
The impact of an educational curriculum to standardize tunneled CVC repairs for trainees on a pediatric surgery service was studied, focusing on comfort level with tunneled CVC repair and to determine the impact on complication rates. Rotating trainees studied a dedicated audiovisual educational curriculum comprised of a video, educational slides, and a practical component from November 2020 through January 2022. Experience and comfort level with tunneled CVC repairs were assessed before and after the rotation. CVCs repaired during the duration of the study were evaluated and compared to the period prior.
Results
Forty-nine individuals completed the pre- and post-training survey. Respondents (34.7%, n = 17) most commonly reported one year of surgical experience, and (79.6%, n = 39) had never observed or assisted in a repair previously. Following training, respondents felt more comfortable with all aspects of the CVC repair process (p < 0.001). There were no statistically significant differences in re-repair rates or CLABSI rates following the implementation of the curriculum.
Conclusions
Tunneled CVC procedural repair variability can be standardized with a dedicated educational curriculum for rotating trainees, which improves knowledge and comfort with such procedures.
Similar content being viewed by others
Introduction
Central venous catheters (CVC) are essential for the treatment of several clinical conditions, including in children who require long-term parenteral nutrition, chemotherapy, hydration, additional medications, and frequent blood testing [1]. Though CVCs are widely used, they are not without complications. These include less frequently encountered infections, such as central line-associated bloodstream infection (CLABSI) and exit-site infection, or more commonly, mechanical complications, such as occlusion, dislodgement, and rupture of the line [2, 3]. These complications may result in hospitalization, premature removal of the line, and increased healthcare costs. In the setting of mechanical complications, specifically fracture or rupture of the external portion of the line, repairs can be performed at the bedside to increase its longevity and prevent removal and replacement, and are associated with no increase incidence of infection rate but eliminates the risks of anesthesia associated with CVC replacement in the operating room [4, 5].
Variability in repair techniques can lead to increased complications and there is currently no consensus on the appropriate approach to bedside repairs of tunneled CVC lines. There has been substantial emphasis on quality improvement initiatives to standardize care within medicine, and standardization of practices has been shown to improve outcomes for other pediatric surgery problems [6,7,8]. The pediatric surgery service at Children’s Hospital Colorado (CHCO) is responsible for tunneled CVC troubleshooting and repairs. Similar to many subspecialty surgical disciplines at teaching hospitals, this service is staffed by rotating general surgery residents. Despite experience with clinical care and surgical technique, trainees have varying levels of experience with pediatric surgery-specific problems, such as tunneled CVC repairs. This was seen as an opportunity for standardization and education.
Simulation-based training has become an essential component of surgical training proven to teach skills [9, 10]. Multiple studies have shown that simulation-based training improves procedural knowledge and comfort levels in a variety of surgical contexts [11,12,13]. There is substantial evidence of the impact of simulation in the adult literature, but simulation-based training in pediatric surgery for general surgery residents remains in its infancy [14]. The primary purpose of this study was to assess the impact of a standardized education curriculum for tunneled CVC repairs on procedural comfort level for trainees rotating on a pediatric surgery service. The secondary aim was to determine if this education impacted complication rates.
Methods
Study design
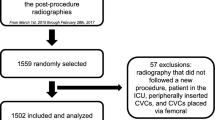
This was a retrospective observational study conducted at CHCO. Children’s Hospital Colorado is a quaternary, freestanding, regional referral children’s hospital. All trainees who participated in the tunneled CVC repair education curriculum between November 2020 and January 2022 were asked to complete pre- and post-curriculum anonymous surveys. Those who completed both were included in this study. Trainees who did not complete both surveys were excluded. This study was reviewed and approved by the Colorado Multiple Institutional Review Board (COMIRB). All methods were carried out in accordance with our COMIRB regulations. Informed consent to participate was waived by Colorado Multiple Institutional Review Board (COMIRB), due to retrospective nature of the study.
Intervention
An education curriculum for bedside repairs of tunneled CVCs was implemented in November 2020 to standardize the process of CVC repairs. All trainees at any level of postgraduate training who rotated on the pediatric surgery service at CHCO as well as advanced practice providers (APPs) covering non-surgical services were asked to complete an anonymous survey detailing their demographic data and experience and comfort levels with CVC repair at the start of the rotation. They subsequently completed an education curriculum, which consisted of audiovisual materials including a video (https://vimeo.com/517348712), educational slides, and a practical training component taught by a senior APP. Following completion of the curriculum, a second anonymous survey was sent to assess for changes in comfort levels with tunneled CVC repair and measure the impact of the education curriculum.
The education curriculum consists of three components: (1) a practical simulation component using a mannequin (Chester Chest, VATA, Canby, OR) and materials used in tunneled CVC repair where the trainee undergoes simulation with a senior APP that walks them through all steps of the repair process. (2) A computer-generated educational video simulating the tunneled CVC repair process. The video includes narrated information on indications for repair, appropriate set-up, the actual repair process (identifying the line defect, transecting proximally, and repairing using a commercially available tunneled CVC repair kit), and information on troubleshooting. (3) Educational slides provided in print and available for the trainees in our secure shared online drive included similar information to the video. Since our number of tunneled CVC repairs in the 2-year period before implementation was relatively low (2.6 average per month), throughout the rotation we ensured participants received continued proctoring for CVC repair procedures by an experienced member of our pediatric surgical team that included APPs, pediatric surgery fellows, and pediatric surgery attendings.
To track the primary outcome of this study (self-reported comfort with aspects of the tunneled CVC repair process), pre- and post-curriculum surveys were used. The set of questions addressed specific components of the repair process and respondents answered on a Likert scale (0–10), with 0 indicating feeling completely unqualified and 10 indicating feeling completely comfortable with performing that aspect of the repair process without supervision.
The secondary outcomes of interest were re-repair rates and CLABSI within 30 days (based on standard surgical complication tracking timeframe) of bedside tunneled CVC repair. An electronic medical record query to assess all central venous catheter repairs by the pediatric surgery service since November 2018 was performed. The pre-education period was defined as November 2018 through October 2020, and the post-education period was defined as November 2020 to January 2022. A retrospective chart review was performed to determine if the repair was performed by an APP or trainee and the subsequent post-graduate level (PGY). Re-repair was defined as any tunneled CVC that required repeat repair within 30 days of the initial re-repair. CLABSI was defined as a CLABSI within 30 days of repair of the CVC.
Statistical analysis
Measures were reported as mean [standard deviation (SD)] for continuous variables and number (%) for categorical variables. We used the Wilcoxon signed-rank test to test for differences between pre- and post-curriculum. We performed the Wilcoxon rank-sum test on the difference between pre- and post-curriculum measures to test if there was a difference by experience (1 year vs. > 1 year). We tested for differences in re-repair and CLABSI rates pre- and post-curriculum by using logistic regression. Statistical Process Control (SPC) chart was generated to evaluate overall CLABSI rates during the study timeframe and the impact of the instituted educational curriculum. An interaction of time (before or after November 2020) by who completed the repair (residents 1–2 yrs, residents > 2 yrs, APP) was included in the model to look for a difference over time in rates.
Results
Overall Population
There were 59 individuals who completed the pre-curriculum survey and 50 individuals who completed the post-curriculum survey. Of these, 49 completed both surveys and were thus included in the analysis. The mean (SD) age was 31.1 (3.9) years and 55.1% [27] were female. Most trainees were from the University of Colorado and 18.4% [9] were from outside institutions. Five (10.2%) were APPs from CHCO rotating from non-surgical services, such as the inpatient medical service. Approximately half (51.0%, n = 25 had 1–2 years of training and 84.1% (37) of residents were categorical general surgery. Six (13.6%) of the residents planned to pursue pediatric surgery following training. The most common post-training plan was general surgery subspecialty (56.8%, n = 25) (Table 1).
Prior experience
Most individuals had no prior pediatric surgery experience (57.1%, n = 28) or had spent 3–4 weeks on a pediatric surgery service (28.6%, n = 14). Only 9 (18.8%) of individuals had previously assisted or observed a tunneled CVC repair and only 4 (8.1%) had performed a repair. Full data on prior experience is provided in Table 2.
Impact of Curriculum
When comparing mean comfort levels with components of the CVC repair process, there was a statistically significant increase for all 8 components addressed by the survey (Table 3). The differences in comfort levels prior to and after the curriculum were compared based on years of training. There was no statistically significant difference in comfort levels between individuals with one year of training and those with more than one year of training (Fig. 1), suggesting the curriculum impact of the curriculum may not depend on training level.
Secondary outcomes
There were 113 lines repaired during the study period: 63 prior to the implementation of the education curriculum and 50 after. The rate of 30-day re-repairs was 24.8% (28) overall; it was 25.4% [16] prior to the curriculum and 24.0% [12] after the curriculum was implemented. Rates of re-repair are displayed in Fig. 2A. Differences in re-repair rates based on who performed the repair were minimal, except for trainees with 1–2 years of experience. The rate of re-repair was 50.0% prior to the curriculum and 33.3% after the curriculum. However, these differences were not statistically significant.
The overall rate of CLABSI rate during the study timeframe was 1.11 per 1000 central line days (116 infections in 104,294 central line days during our timeframe). Out of the 113 lines that required repair during the duration of the study, there were three (4.8%) CLABSIs prior to the education curriculum and five (10.0%) after resulting in pre-curriculum and post-curriculum. There were no statistically significant differences in CLABSI rates following the institution of our educational curriculum in November 2020, as noted in our SPC chart (Fig. 2B).
Discussion
This study indicates an educational curriculum dedicated to standardizing the CVC repair process improves comfort levels in all aspects of the repair procedure. This trend was seen with all trainees who participated, regardless of their level of training. This indicates that a practical curriculum to standardize pediatric surgery procedures can benefit not just junior residents, but also senior residents and fellows. However, this curriculum did not statistically impact re-repair or CLABSI rates in our limited series.
Simulation-based education has been extensively studied in graduate medical education for both surgical and non-surgical trainees [15]. Proponents of simulation-based training argue that practicing simulations before performing procedures on patients improves patient safety. This has been confirmed by multiple studies of the impact of simulation on the performance of surgical residents and subspecialty procedures [16,17,18,19,20]. It has been shown to be most impactful for less commonly performed [19]. Within our study cohort, most trainees had never seen nor performed a CVC repair previously, indicating their low rates of exposure. This highlights the importance of practical education curriculums to increase familiarity with procedures prior to performing them on patients.
The implementation of a curriculum to teach trainees rotating on pediatric surgery resulted in increased confidence with all aspects of the repair process, regardless of the level of the trainee. Our findings are consistent with multiple prior studies that report improvements in confidence levels for trainees following simulation-based training [13, 14, 18, 21]. There is, however, mixed data on the impact of such curriculums on year of training. The impact of simulation training on confidence levels based on training status may be dependent upon the procedure addressed, as prior interventions have led to an increased comfort level with procedures even among faculty [22]. We did not perform a sensitivity analysis by discreet year of training, but we did not see any difference between the mean difference in confidence levels when comparing trainees with less than one year of training and those with more. Though not statistically significant, certain domains resulted in greater increases for trainees with more experience, indicating there may also be utility in tailoring education curriculums based on the experience level of the learner.
The Accreditation Council for Graduate Medical Education (ACGME) requires general surgery residents to complete at least 20 pediatric surgery cases during residency [23]. The number of pediatric surgery rotations are often minimal with variable caseloads, which highlights the heterogeneity in exposure to pediatric surgery and associated pathology and cases [14, 24]. The minimal time on pediatric surgery service, diversity of cases, and low case volume can leave trainees ill-prepared when rotating on pediatric surgery services. Simulation-based learning has been shown to be successful in improving the performance of pediatric surgeons [25]. However, most simulation models have been developed for pediatric surgery fellows, leaving a need and opportunity for educational curriculums for general surgery residents. Curriculums, such as ours, provide instruction and training on procedures that are rare for general surgery residents, but a common procedure in pediatric surgery, and can serve as a model for other procedures and education initiatives.
The secondary aim of this study was to determine if the education curriculum impacts complications associated with CVC repairs. There has been substantial research on rates of CVC complications [1,2,3, 26]. Most prior research does not account for bedside repairs and focuses on initially placed lines, but rates of mechanical complications, such as fracture, and kinking, have been reported to be between 10% and 18% [1, 2, 26]. Our rate of re-repair, which includes mechanical complication as well as any other indication for bedside repair, was 25%. It is possible our rate is higher than previously reported rates given the repair processes and longevity of the line may inherently increase complication rates. CLABSIs are another outcome of interest and occur at a rate of 0.7 to 7.4 per 1000 catheter days [27]. Again, these rates are based on initial placement and do not account for bedside repairs. Consistent with prior data, our reported rate during the study timeframe was 1.11 per 1000 central line days. Although outside of the scope of this study, repaired lines were categorized based on demographics including age at the time of repair, sex, race, ethnicity, weight at the time of repair, and diameter of line. No statistical differences were noted for any of these demographics and our tracked complications, including re-repairs and overall CLABSI rates.
This study is not without limitations. First, the long-term implications of this intervention are unknown. For example, though individuals report increased comfort levels with CVC repairs, it is unclear if this will be retained. Additionally, our sample size is small and represents the experience of residents rotating at a single institution, therefore, our findings may not be generalizable to all populations. Our follow-up period may also have limited our ability to detect any differences in complication rates, and longer-term analysis is warranted. Finally, consistent with any survey-based research is the concern for reporting bias and the Hawthorn effect, which could have impacted results.
Conclusion
In conclusion, an education curriculum that targets the CVC repair process results in increased comfort and confidence with all aspects of the process for surgical trainees rotating on a pediatric surgery service, regardless of training level. However, this limited series failed to statistically affect overall CLABSI or re-repair rates. Such findings support initiatives to incorporate simulation and multi-modal education processes in pediatric surgical training or for dedicated vascular access teams to supplement learning. This curriculum can serve as a model for other low-occurrence procedures to improve trainee comfort levels and performance.
Data Availability
The data generated or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- APP:
-
Advanced practice providers
- CHCO:
-
Children’s Hospital Colorado
- CLABSI:
-
Central line associated blood stream infection
- COMIRB:
-
Colorado Multiple Institutional Review Board
- CVC:
-
Central venous catheter
- SD:
-
Standard deviation
References
Perdikaris P, Petsios K, Vasilatou-Kosmidis H, Matziou V. Complications of Hickman-Broviac catheters in children with malignancies. Pediatr Hematol Oncol. 2008;25(5):375–84.
Cesaro S, Cavaliere M, Pegoraro A, Gamba P, Zadra N, Tridello G. A comprehensive approach to the prevention of central venous catheter Complications: results of 10-year prospective surveillance in pediatric hematology-oncology patients. Ann Hematol. 2016;95(5):817–25.
Pinon M, Bezzio S, Tovo PA, et al. A prospective 7-year survey on central venous catheter-related Complications at a single pediatric hospital. Eur J Pediatr. 2009;168(12):1505–12.
Zens T, Nichol P, Leys C, Haines K, Brinkman A. Fractured pediatric central venous catheters - repair or replace? J Pediatr Surg. 2019;54(1):165–9.
Fletcher J, Woodham D, Cooper SC. Repair of central venous access devices in intestinal failure patients is safe and cost-effective: a retrospective single centre cohort study. Clin Nutr. 2021;40(6):4263–6.
Yousef Y, Youssef F, Homsy M, et al. Standardization of care for pediatric perforated Appendicitis improves outcomes. J Pediatr Surg. 2017;52(12):1916–20.
Willis ZI, Duggan EM, Bucher BT, et al. Effect of a clinical practice Guideline for Pediatric Complicated Appendicitis. JAMA Surg. 2016;151(5):e160194.
Keren R, Luan X, Localio R, et al. Prioritization of comparative effectiveness research topics in hospital pediatrics. Arch Pediatr Adolesc Med. 2012;166(12):1155–64.
Reznick RK, MacRae H. Teaching surgical skills–changes in the wind. N Engl J Med. 2006;355(25):2664–9.
Cook DA, Hamstra SJ, Brydges R, et al. Comparative effectiveness of instructional design features in simulation-based education: systematic review and meta-analysis. Med Teach. 2013;35(1):e867–98.
Robinson WP, Doucet DR, Simons JP et al. An intensive vascular surgical skills and simulation course for vascular trainees improves procedural knowledge and self-rated procedural competence. J Vasc Surg 2017; 65(3): 907 – 15 e3.
Ritter KA, Horne C, Nassar A, French JC, Prabhu AS, Lipman JM. Multidisciplinary Simulation Training improves Surgical Resident Comfort with Airway Management. J Surg Res. 2020;252:57–62.
Weingarten N, Byskosh A, Stocker B, et al. Simulation-based course improves Resident Comfort, Knowledge, and ability to Manage Surgical Intensive Care Unit patients. J Surg Res. 2020;256:355–63.
Skertich NJ, Schimpke SW, Lee T, et al. Pediatric Surgery Simulation-based training for the general Surgery Resident. J Surg Res. 2021;258:339–44.
Willis RE, Van Sickle KR. Current status of Simulation-based training in Graduate Medical Education. Surg Clin North Am. 2015;95(4):767–79.
Seymour NE, Gallagher AG, Roman SA, et al. Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg. 2002;236(4):458–63. discussion 63 – 4.
McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. 2011;86(6):706–11.
Zendejas B, Cook DA, Bingener J, et al. Simulation-based mastery learning improves patient outcomes in laparoscopic inguinal hernia repair: a randomized controlled trial. Ann Surg. 2011;254(3):502–9. discussion 9–11.
Augustine EM, Kahana M. Effect of procedure simulation workshops on resident procedural confidence and competence. J Grad Med Educ. 2012;4(4):479–85.
Wang C, Karl R, Sharan L et al. Surgical training of minimally invasive mitral valve repair on a patient-specific Simulator improves Surgical skills. Eur J Cardiothorac Surg 2023.
Admire JR, Pounds LL, Adams AJ, Gomez PP, Willis RE. Development and construct validity of a low-fidelity training platform for driving large and small suture needles. J Surg Educ. 2015;72(3):387–93.
Gomez PP, Willis RE, Van Sickle KR. Development of a virtual reality robotic surgical curriculum using the Da Vinci Si surgical system. Surg Endosc. 2015;29(8):2171–9.
ACGME. Defined Category Minimum numbers for general surgery residents and Credit role. 2019. https://www.acgme.org/globalassets/definedcategoryminimumnumbersforgeneralsurgeryresidentsandcreditrole.pdf (accessed April 24, 2023.
Patel EA, Aydin A, Desai A, Dasgupta P, Ahmed K. Current status of simulation-based training in pediatric Surgery: a systematic review. J Pediatr Surg. 2019;54(9):1884–93.
Barsness K. Simulation-based education and performance assessments for pediatric surgeons. Eur J Pediatr Surg. 2014;24(4):303–7.
Fratino G, Castagnola E, Carlini C, et al. A single institution observational study of early mechanical Complications in central venous catheters (valved and open-ended) in children with cancer. Pediatr Surg Int. 2004;20(9):704–7.
Rinke ML, Chen AR, Bundy DG, et al. Implementation of a central line maintenance care bundle in hospitalized pediatric oncology patients. Pediatrics. 2012;130(4):e996–e1004.
Acknowledgements
These data were presented as an oral presentation at the American College of Surgeons Clinical Congress 2022 in San Diego, California on October 14, 2022.
Funding
This work was supported by the Children’s Hospital Colorado Clinical and Operational Effectiveness and Patient Safety Small Grants Program (Aurora, Colorado).
Author information
Authors and Affiliations
Contributions
Study conception and design: JDM, KF, CD. Data acquisition: MR, CP, KF Analysis and data interpretation: SS, JDM, MR. Drafting of the manuscript: JDM, MR. Critical revision: JDM, MR, CP, KF, SS, CD.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and approved by the Colorado Multiple Institutional Review Board (COMIRB). All methods were carried out in accordance with our COMIRB regulations. Informed consent to participate was waived by Colorado Multiple Institutional Review Board (COMIRB), due to retrospective nature of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1:
Central line repair follow-up survey
Supplementary Material 2:
Central line repair survey
Supplementary Material 3:
Central venous catheter (CVC) repair policy
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Reppucci, M., Prendergast, C., Flynn, K. et al. Trainee educational curriculum to standardize central venous catheter repair. BMC Med Educ 23, 978 (2023). https://doi.org/10.1186/s12909-023-04977-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-023-04977-9