Abstract
Background
Characterised by feelings of helplessness in the face of clinical, organization and societal demands, medical students are especially prone to moral distress (MD). Despite risks of disillusionment and burnout, efforts to support them have been limited by a dearth of data and understanding of MD in medical students. Yet, new data on how healthcare professionals confront difficult care situations suggest that MD could be better understood through the lens of the Ring Theory of Personhood (RToP). A systematic scoping review (SSR) guided by the RToP is proposed to evaluate the present understanding of MD amongst medical students.
Methods
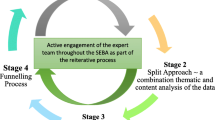
The Systematic Evidence-Based Approach (SEBA) is adopted to map prevailing accounts of MD in medical students. To enhance the transparency and reproducibility, the SEBA methodology employs a structured search approach, concurrent and independent thematic analysis and directed content analysis (Split Approach), the Jigsaw Perspective that combines complementary themes and categories, and the Funnelling Process that compares the results of the Jigsaw Perspective with tabulated summaries to ensure the accountability of these findings. The domains created guide the discussion.
Results
Two thousand six hundred seventy-one abstracts were identified from eight databases, 316 articles were reviewed, and 20 articles were included. The four domains identified include definitions, sources, recognition and, interventions for MD.
Conclusions
MD in medical students may be explained as conflicts between the values, duties, and principles contained within the different aspects of their identity. These conflicts which are characterised as disharmony (within) and dyssynchrony (between) the rings of RToP underline the need for personalised and longitudinal evaluations and support of medical students throughout their training. This longitudinal oversight and support should be supported by the host organization that must also ensure access to trained faculty, a nurturing and safe environment for medical students to facilitate speak-up culture, anonymous reporting, feedback opportunities and supplementing positive role modelling and mentoring within the training program.
Similar content being viewed by others
Background
Moral distress (MD) amongst healthcare professionals (HCP)s is an increasing concern [1,2,3] amidst the COVID-19 pandemic [4,5,6]. Characterised by “a lack of assertiveness or autonomy, socialization pressures to follow others, lack of time, inhibiting power structure, lack of collegial support, and organizational priorities that conflict with care needs” ([7] p. 4), medical students are seen to be especially prone to MD. These concerns are further heightened by data suggesting that poor ethical climes, uncooperative environments, and pressure to carry out or make allowances for unethical acts ([8,9,10,11,12,13,14,15] #95) that predispose to MD have been identified in educational settings involving medical students [16,17,18]. This underscores the need to better understand the effects of MD on medical students and to ensure effective support of ‘at risk’ medical students [19,20,21].
However, a dearth of knowledge on MD amongst medical students and the notion that MD is a personalised sociocultural construct, that is the product of the tension between an individual’s ethical, moral, relational, situational, personal, professional, and societal values, beliefs and principles and regnant sociocultural, institutional and professional expectations, standards and codes of practice, emphasises the need to review how current understanding of MD is mapped [12,13,14, 22].
Drawing upon insights into how HCPs cope with grief and bereavement [15], address complicated care issues [5, 19,20,21, 23, 24] and care for dying patients [23, 25,26,27,28,29,30,31,32,33,34,35,36] that result in similar conflicts between deeply held beliefs, principles, values, and prevailing roles, expectations, and responsibilities and that manifest emotions and reactions akin to that described in MD, we posit that MD may also be better understood through the lens of personhood [37,38,39]. Kuek, Ngiam [25], Ho, Kow [30], Ngiam, Ong [34], Chan, Chia [31] and Huang, Toh [26] review how nurses, doctors and medical students face the deaths of their patients and cope with caring for the dying suggest that the Ring Theory of Personhood (RToP)’s is well equipped to map conflicts between deeply held beliefs, principles, values, and prevailing roles, expectations, and responsibilities that mirror those seen in [5, 23, 24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40] MD [5, 8,9,10,11, 15, 19,20,21, 23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40].
The Ring Theory of Personhood (RToP)
Kuek, Ngiam [29] Kuek, Ngiam [29] Ho, Kow [34] Ngiam, Ong [38]Chan, Chia [35] Ngiam, Ong [38]Chan, Chia [35] Huang, Toh [23, 41,42,43] Kuek, Ngiam [29] Radha Krishna and Alsuwaigh [31]Kuek, Ngiam [25] suggests Radha Krishna and Alsuwaigh [28]’s Ring Theory of Personhood (RToP), [41,42,43]could help identify medical students facing or at risk of MD and direct timely, holistic, personalised, and appropriate support that will attenuate the risk of burnout, attrition in the profession and compromised patient care [12,13,14, 22].
The RToP captures concepts of personhood – or “what makes you, you” [28] and is depicted by 4 rings depicting the (1) Innate, (2) Individual, (3) Relational, and the (4) Societal Rings (Fig. 1).
The Ring Theory of Personhood (RtoP) [28]
At the core of the Ring Theory is the Innate Ring. Krishna and Alsuwaigh defined the Innate Ring as containing the rights and privileges bestowed to all persons by virtue of their being living humans, conceived due to their connections with the Divine or their genetic makeup [23, 28, 29]. Innate Ring also houses the individual’s spiritual, religious and/or theist beliefs and values which are shaped by the individual’s demographical and historical features such as the ethnicity, culture, religion, family unit, gender, society, country, and the social group they were born into [23, 28, 29]. These individualized beliefs, values, moral ideals, and ethical principles influence the individual’s thinking, goals, motivations, and actions, which are expressed through the Individual Ring [23, 28, 29].
The Individual Ring encompasses and builds upon the Innate Ring and represents a conscious function which includes the ability to think, feel, communicate, carry out actions, and interact with the environment [23, 28, 29]. The Individual Ring confers a sense of individuality shaped by the individual’s values, beliefs, principles, biases, preferences, thoughts, emotions, experiences, decision making and personality drawn from the values, beliefs and principles contained in the other three rings [23, 28, 29].
The Relational Ring consists of personal relationships deemed important to the individual, such as family members, loved ones and close friends [23,28, 29]. These ties are determined by the person and can change over time [23, 28, 29].
The Societal Ring is the outermost ring that consists of less intimate relationships such as those shared with colleagues and acquaintances. The Societal Ring also contains societal, religious, professional, and legal expectations set out in the individual’s society to guide and police conduct [23, 28, 29].
Critically each ring also represents an element of the medical student’s identity and the values, beliefs and principles associated with it [23, 28,29,30,31]. This link between personhood and identity affords the RToP a key role in this review. The Innate Identity drawn from the Innate Ring considers religious, gender, cultural, community-based beliefs, moral values and ethical principles. The Individual Identity encompasses personal values, beliefs, and personalities whilst the Relational and Societal Identities drawn from the outermost rings pivot on familial and societal values, beliefs, expectations, and principles, respectively [23, 28, 29, 31] Kuek, Ngiam [29, 31].
Chan, Chia [31] Kuek, Ngiam [25], and Ngiam, Ong [38]Chan, Chia [35] Ngiam, Ong [34] suggest that when the beliefs, moral values, ethical principles, familial mores, cultural norms, attitudes, thoughts, decisional preferences, roles, and responsibilities housed in each of these rings come into conflict in a variety of situations, disharmony and dyssynchrony arise. Disharmony refers to conflicts between values, beliefs, and principles within the rings whilst dyssynchrony refers to conflicts between the rings [28]. It is posited that unresolved disharmony and or dyssynchrony results in MD [25]. These considerations further explain our use of the RToP to guide this review.
Methodology
Krishna’s Systematic Evidence-Based Approach (henceforth SEBA) [40] is employed to structure a systematic scoping review (henceforth SSR in SEBA) of accounts of MD amongst medical students. To enhance accountability and transparency the SSRs in SEBA employ an expert team to guide, oversee and support all stages of SEBA. In this case, the expert team is composed of medical librarians from the Yong Loo Lin School of Medicine (YLLSoM) at the National University of Singapore and the National Cancer Centre Singapore (NCCS), and local education experts and clinicians at NCCS, the Palliative Care Institute Liverpool, YLLSoM and Duke-NUS Medical School, henceforth the expert team. The expert team enhances the reflexivity of the review. The research team also maintained a reflexive diary to highlight their biases, positions, and assumptions.
SSRs in SEBA are built on a constructivist perspective which acknowledges MD as a sociocultural construct informed by prevailing clinical, academic, personal, research, professional, ethical, psychosocial, emotional, legal and educational factors, the individual’s particular circumstances, their self-concept of personhood and the support available to them at the time [41,42,43,44,45]. SEBA’s relativist lens considers various perspectives through data collected from quantitative, qualitative and knowledge synthesis articles.
To operationalise an SSR in SEBA the research team adopted the principles of interpretivist analysis, to enhance reflexivity and discussions [46,47,48,49] in the Systematic Approach, Split Approach, Jigsaw Perspective, Funnelling Process, analysis of data from the grey and black literature and Synthesis of SSR in SEBA which make up SEBA’s 6 stages outlined in Fig. 2.
Stage 1 of SEBA: systematic approach
Theoretical lens
The use of the RToP as a theoretical lens is consistent with the Social Cognitive Theory’s posit of a “triadic reciprocal dynamic relationship between the learner, the environment and the behaviour itself” [50]. The RToP provides a sketch of the conflicts between a medical student’s beliefs, moral values, ethical principles, familial mores, cultural norms, attitudes, thoughts, decisional preferences, roles, and responsibilities (henceforth values, beliefs, and thoughts) within the 4 aspects of the medical student’s identity. The RToP also offers a better understanding of their contextual and environmental factors, enhancing understanding of their motivations, cognition, responses, thoughts, motivations, biases, ideas, choices, actions, and goals providing a holistic appreciation of the conflicts that underpin MD [23, 25,26,27,28,29,30,31, 51]
Determining the title and research question
To ensure a systematic approach, the research and expert teams established the goals of the SSR and the population, context, and concept (PCC) to be evaluated. The primary research question was determined to be: “What is known about MD amongst medical students?” and the secondary questions were: “What are the sources of MD in medical students?” and “What are the interventions employed to help medical students cope with MD?”
Inclusion criteria
A PICOS format was adopted to guide the research process as shown in Table 1 [52, 53].
Searching
The six members of the research team carried out independent searches of seven bibliographic databases (PubMed, Embase, PsycINFO, ERIC, SCOPUS, Web of Science, Google Scholar) for articles published between 1st January 1990 and 31st December 2021. The searches were carried out between 13th February 2021 and 5th May 2021 and between 17th December 2021 and 17th January 2022. The PubMed search strategy may be found in Additional file 1: Appendix A.
Each member of the research team independently sieved through all titles and abstracts from the individual searches of the four databases and created their own lists of titles to be reviewed. Comparing these individual lists via online meetings, the teams used ‘negotiated consensual validation’ to achieve consensus on the final list of titles to be reviewed [54, 55].
The research team then independently reviewed each of the full-text articles from this final list, created individual lists of articles to be included, discussed these online and achieved a consensus on the final list of full-text articles to be included in the SSR. The results of this process are outlined below.
Assessing the quality of included articles
Three research team members individually appraised the quality of the quantitative and qualitative studies using the Medical Education Research Study Quality Instrument (MERSQI) [56] and the Consolidated Criteria for Reporting Qualitative Studies (COREQ) [51, 57]. The MERSQI tool had the following domains: study design, sampling, type of data, validity of evaluation instrument, data analysis and outcomes. The COREQ tool had the following domains: research team and reflexivity, study design, analysis and findings. This allowed the research team to evaluate the methodology employed in the included articles, aid readers and reviewers in appraising the weight afforded the data in the analysis and assist decision-makers in understanding the transferability of the findings. No articles were excluded based on the results of the appraisal.
Stage 2 of SEBA: split approach
Three teams of at least three researchers independently reviewed the included full-text articles. Wong, Greenhalgh [58] Popay, Roberts [59] The first team summarized and tabulated them in keeping with Wong, Greenhalgh [60]’s RAMESES publication standards: meta-narrative reviews and Popay, Roberts [61]’s “Guidance on the conduct of narrative synthesis in systematic reviews”. The tabulated summaries ensure that key points of the articles are not lost (Additional file 2: Appendix B).
Concurrently, the second team independently analysed the included articles using Braun and Clarke [62] Braun and Clarke’s approach to thematic analysis while the third team adopted Hsieh and Shannon’s Hsieh and Shannon [63] approach to directed content analysis. Radha Krishna and Alsuwaigh [31] Concurrent use of thematic and directed content analysis is a key feature of the ‘Split Approach’ and serves to enhance the reproducibility, transparency, and accountability of the analytic process. This concurrent analysis also serves to reduce the omission of new findings or negative reports and enable review of data from different perspectives.
Thematic analysis
In the absence of rigorous definitions of MD, three members of the research team adopted Braun and Clarke’s approach to identify key themes across different learning settings and medical student populations. This allowed for the analysis of data derived from quantitative, qualitative, and mixed methodologies. This sub-team independently reviewed the included articles, constructed codes from the surface meaning of the text and collated these into a code book, which was used to code and analyse the rest of the articles in an iterative process. New codes were associated with prior codes and concepts. An inductive approach allowed us to identify codes and themes from the raw data without using existing frameworks or preconceived notions as to how the data should be organized. The sub-team discussed their independent analyses in online and face-to-face meetings and used “negotiated consensual validation” to derive the final themes.
Directed content analysis
Three members of the research team independently employed Hsieh and Shannon’s approach [63] to directed content analysis. This involved “identifying and operationalizing a priori coding categories” by classifying text of similar meaning into categories drawn from prevailing theories. The research team first used deductive category application to extract codes and categories from Radha Krishna and Alsuwaigh [31]’s article, “Understanding the fluid nature of personhood – the Ring Theory of Personhood”. A code book was developed and individual findings were discussed through online and face-to-face meetings. Differences in codes were resolved until consensus was achieved on a final list of categories.
As part of the reiterative process within the SEBA methodology, the initial data was reviewed by the expert and research teams who determined that with current evolutions in concepts of MD extended to various aspects of moral principles and subject to individual, religious, cultural and societal considerations. As a result the expert team advised that the included articles be evaluated using categories drawn from Kuek et alChan, Chia [35]’s article entitled “Extending the Ring Theory of Personhood to the Care of Dying Patients in Intensive Care Units”, to determine the impact of dissonance or conflict between the values, beliefs and principles within individual rings and between the four rings.
Stage 3 of SEBA: jigsaw perspective
The Jigsaw Perspective employs adopted Phases 4 to 6 of France, Uny [64]’s adaptation of Noblit, Hare [65]’s seven phases of meta-ethnography to view themes and categories identified in the Split Approach as pieces of a jigsaw puzzle. Here overlapping/complementary pieces are combined to create a bigger piece of the puzzle to create a wider/holistic view of the overlying data. This process would see themes and subthemes compared with the categories and subcategories identified. Similarities between the subthemes and subcategories are further compared with the codes contained to confirm the similarities and indeed if they are complementary in nature. If this is confirmed, then the subtheme and subcategory are combined to create a bigger piece of the jigsaw puzzle. Guided by the Jigsaw Perspective, these overlaps and similarities were combined to provide a holistic picture of available data on MD in medical students.
Stage 4 of SEBA: funnelling process
A funnelling approach was adopted to streamline results from the three aspects of the Split Approach. It sees data compared and combined to reduce overlap and repetition whilst retaining a holistic perspective of the data.
Results
Two thousand six hundred seventy-one abstracts were identified from eight databases, 316 full text articles were reviewed, and 20 articles were included as shown in Fig. 3.
The themes identified were definitions, causes, impact, influencing factors, assessment, and interventions. The categories identified related to the four rings of the RToP, the Intra-ring conflicts (disharmony) and Inter-ring conflicts (dyssynchrony) (Table 2).
The domains created by combining the themes and the subtheme and the categories and sub-categories are presented in Additional file 3: Appendix C to enhance reproducibility, accountability, and accountability of the Jigsaw Perspective.
The resultant domains were definitions of MD, sources of MD using RToP, recognition of MD and, interventions for MD.
Domain 1: definition of MD
JametonJameton [66] attributes MD to feelings of powerlessness to do what healthcare professionals deemed was morally correct due to organizational restrictions [54]. This definition is widely adopted amongst the included articles [56,57,58,59] and echoed in the definitions in other papers [56, 57, 59, 62]. Recently the concept of MD has been expanded to include cognitive-emotional dissonance between one’s ethical/moral beliefs and actions or behaviour that one is compelled to perform [63,64,65,66,67]. MD can occur immediately or later and at an individual, team or system levels (Table 3).
Domain 2: sources of MD viewed through RToP lens
Innate ring
Female medical students are more likely to report MD than their male counterparts [58, 59, 65, 76, 81]. Aside from gender, religious, spiritual and cultural influences and clinical experience [56, 59, 63, 67, 69, 75, 78] are also sources of MD [62, 69, 81].
Individual ring
The medical students assessment of a situation, their moral standpoint [57,58,59, 62, 66, 67, 70, 81] and concepts of morality [59, 62, 67, 69, 78] can precipitate MD [58, 64,65,66,67, 81].
Relational ring
Social support from family and close friends protects against harmful effects of moral distress [68, 83].
Societal ring
Medical hierarchy also precipitates MD. This revolves around concerns that any dissent and or refusal to abide by the decisions of the senior physicians [56, 64, 66, 67, 69, 76, 81] would prevent the student from ‘fitting in’ [56, 57, 64,65,66]. This desire to ‘fit in’ also underlies resistance to question decisions and actions even when they may run contrary to professional obligations [56, 59, 62,63,64,65,66,67, 69, 76, 78,79,80,81]. MD is compounded by a [67, 68, 76, 79, 80]lack of clarity on the medical student’s role and influence on the team’s decisions and actions [56, 58, 66, 81].
Resource constraints and their implications on quality and access to healthcare also provoke MD [56, 57, 59, 64, 67, 76].
Conflicts
Conflicts are central to the concept of MD and when viewed through the lens of the RToP highlights intra-ring (disharmony) and inter-ring (dyssynchrony) conflict. Though they may occur concurrently, we highlight individual examples of disharmony and dyssynchrony.
Intra-ring conflicts
Dissonance between values and beliefs within a particular ring results in intra-ring conflicts or ‘disharmony’ [77, 84]. For example, ‘disharmony’ within the societal ring, may occur when a patient’s proposed actions run contrary to medical advice [59, 67, 74], or when medical students do not have an opportunity to meet their professional responsibilities such as reporting the abuse of the patient for fear of compromising the patient’s anonymity [76]. MD has also been reported when medical students feel conflicted about giving opioids to opioid dependent patients; witnessing patients undergoing unnecessarily ‘burdensome’ or even ‘futile’ treatment; or witnessing inadequate symptom control because the attending physician was not ‘comfortable’ to do so [56, 57, 59, 62,63,64,65,66,67, 69, 70, 74, 76, 78, 81].
Medical students also report MD when they struggle to maintain their professional responsibilities to the patient in the face of contradicting the decisions taken by the physicians [64, 78, 81] or when they feel conflicted when meeting their academic objectives [56, 70, 72, 74, 78] at the cost of what they conceive to be the patient’s choice to refuse [59, 62, 69], or performing tasks that the medical student does not feel confident nor equipped to carry out [62]. Miller et al. [62] describe a student “[beginning] to worry that if she performs the lumbar puncture, she would be putting her own interests as a student before those of her patient, who should always receive the best care possible”(p. 538).
Inter-ring conflicts
Tension between values, principles and beliefs between the rings or Inter-ring conflicts are termed dyssynchrony [77, 84]. Dyssynchrony is exemplified as [67,68,69,70, 72,73,74,75,76,77,78,79,80, 85, 86] medical students struggle with their desire to ‘fit in’ and compromise their ideals and beliefs [56, 65,66,67, 69, 70]. Similarly Dias [66], described medical students experiencing MD when “[participating] in care that [the medical student] does not agree with (abortion appointments)”(p. 6), highlighting the conflict between the Innate Ring with regards to religion and the sanctity of life and the need to meeting clinical obligations which would be part of the societal ring. [67, 69, 70, 73, 75, 84,85,86].
Administrative protocols [65, 76], healthcare inequality and resource constraints also increase the risk of dyssynchrony [56, 57, 59, 64, 65, 67].
Domain 3: recognizing MD
[72] MD often manifests as anxiety, depression [81], a diminished sense of well-being and guilt and burnout and disillusionment and decreased empathy [58, 66, 74, 75]. In some cases, MD may even compromise patient care [56, 62, 67, 70].
MD is also detected through self-reporting via a variety of methods including self-administered surveys [58, 59, 65, 66] and or reflective essays [56, 64]. Yet self-reporting of MD may be compromised by concerns over the impact of such admissions upon career prospects [69, 85] and the lack of clear reporting processes [76].
There were no studies that reported the use of third-party assessment methods completed by tutors or peers that identify MD [67, 75, 78,79,80,81].
Domain 4: interventions
If unaddressed, MD can precipitate disillusionment, self-doubt over a medical career [69] and dissatisfaction with the medical profession [63], burnout [58, 66] and exiting the medical school [56, 65].
Educational interventions to attenuate MD include increasing awareness of MD [57, 62, 65, 81], and ethical issues [65, 66] and enhancing communication skills [62, 64, 72, 81] and professionalism [72, 76, 77, 80].
Education interventions often take the form of case-based ethical discussions [72, 73], case-based small group discussions [68,69,70, 72, 73], large group lectures [72], reflective writing under peer and expert guidance [68, 73, 77, 81] and positive role modelling [68] that run longitudinally throughout the medical school training [81].
Stage 5 of SEBA: analysis of evidence-based and non-data driven literature
Concerns over the quality of the data included from non-data-based articles (grey literature, opinion, perspectives, editorial, letters) and its potential impact upon the analysis of this review saw the themes drawn from evidenced-based publications were compared with those from non-data-based articles. This process found that the themes from both groups to be similar suggesting that information drawn from non-data based articles did not bias the analysis untowardly.
Stage 6 of SEBA: discussion and synthesis of SSR in SEBA
[87, 88]The narrative produced by consolidating the tabulated summaries, themes and categories was guided by the Best Evidence Medical Education (BEME) Collaboration guide [87] and the STORIES (STructured apprOach to the Reporting In healthcare education of Evidence Synthesis) statement [88].
In addressing its primary and secondary research questions on what is known about MD, its causes, and the interventions to address MD in medical students, this SSR in SEBA highlights several key findings.
To begin, MD arises when conflicts that impact deeply held beliefs, values, and principles rooted in the medical student’s identity are not easily resolved. Through the lens of the RToP, such conflicts that underlie MD can be explained by the concepts of disharmony within and/or dyssynchrony between the rings. This process is further influenced by the medical student’s personal, existential, spiritual, familial, societal, cultural, and demographic factors, contextual considerations that influence the severity of these conflicts; their ability to process these conflicts; motivations; and the support structures available to them in addressing these conflicts.
These insights lend themselves to reports of MD amongst other healthcare professionals. For one, [1, 9, 10, 16, 17, 20, 89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108] nurses appear to have more intense episodes of MD due to feelings of powerlessness when faced with the medical hierarchy that belittles their input [1, 20, 97, 100, 103, 105, 108]. Therapists also report MD [108] due to their limited role in diagnosing and influencing care of medical ailments and the subsequent limitations in their roles in care and treatment determinations.
Accounts of MD in medical students and physicians were also largely similar, particularly amongst junior physicians [1, 19, 20, 93, 97, 100, 103, 105, 108]. Junior doctors, like their medical student counterparts, are more prone to MD due to their limited role in treatment decisions within the medical hierarchy [104, 109,110,111,112,113]. For both groups, there is an associated sense of helplessness that appears to recede with progress along the medical hierarchy.
Evidencing the notion that MD is a sociocultural construct informed by psychosocial, individual and contextual considerations, it is clear that assessment requires careful elucidation and a personalised and longitudinal approach. It is here that due consideration of the various values, beliefs and principles of each ring is key and the potential adaptation of the RToP as a tool to evaluate MD comes to light.
Concurrently treating MD requires a holistic and longitudinal perspective of MD and reiterates the need for active involvement of the medical schools in recognising, addressing, and attenuating the effects of MD and supporting medical students facing such distress. Aside from aiding in the diagnosis of MD and identifying medical students ‘at risk’ of MD, medical schools must provide robust and accessible means of support by training faculty to recognise and address MD [71, 85, 114, 115], and ensure the presence of a timely, personalised and ‘safe’ environment where medical students can discuss their concerns without fear of ‘reprisals’ upon their professional reputations and careers. In addition, there is a need to evaluate the hidden curriculum, and the introduction of initiatives such as speak-up culture [70, 79, 81]and anonymous reporting and feedback opportunities [67, 74] and supplementing positive role modelling and mentoring within the training program [68,69,70, 79], would be helpful. These considerations should also be accompanied by a clear delineation of the role and responsibilities of the medical student within the medical teams and the support available to them.
Limitations
Even though we had the guidance of an expert team, the use of specific search terms and inclusion of only English language articles compounds the risk of omitting key articles and limiting the findings to North American and European settings. This may lead to the unintended exclusion of articles from other settings. As concepts of MD and personhood are sociocultural constructs, the omission of non-English articles may have significant ramifications on the applicability of these findings in Confucian-inspired societies [31, 116,117,118,119]. [31] Here relational autonomy, filial piety and family-centric associations play a critical role in self-concepts of identity and personhood and thus suggest that concepts of MD [120,121,122,123,124,125] in these settings may be different and not fully reflected by our findings.
Conclusions
MD is a unique phenomenon determined by a medical student’s values, beliefs, goals, principles, perspectives, and contextual and psychoemotional considerations. In evidencing the complexity of this concept, the RToP has shown the potential to be adapted as a tool to evaluate MD holistically and in a socioculturally [119] appropriate manner. Such a tool could guide the support of medical students in need, and help design and oversee a safer learning and working environment for medical students. Concurrently with identity, contextual factors and psycho-emotional considerations constantly changing an RToP tool could also provide longitudinal follow up of medical students who have suffered MD.
Drawing on recent studies on longitudinal support and assessments of medical students the use of a tool to assess MD based on the RToP could be included within a medical student’s [126] to assess progress and direct support. As we look forward to engaging in this growing field, we are especially hopeful for greater understanding of the long-term effects of MD in various cultures and to evaluate the efficacy of support mechanisms for ‘at risk’ and ‘recovering’ medical students.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- MD:
-
Moral Distress
- SSR:
-
Systematic Scoping Review
- SEBA:
-
Systematic Evidence Based Approach
- RToP:
-
Ring Theory of Personhood
- YLLSoM:
-
Yong Loo Lin School of Medicine
- NCCS:
-
National Cancer Centre Singapore
References
Hamric A, Borchers C, Epstein E. Development and Testing of an Instrument to Measure Moral Distress in Healthcare Professionals. Ajob Primary Research. 2012;3:1–9.
Dodek PM, et al. Moral distress and other wellness measures in Canadian critical care physicians. Ann Am Thoracic Soc. 2021;18(8):1343–51.
Vincent H, Jones DJ, Engebretson J. Moral distress perspectives among interprofessional intensive care unit team members. Nurs Ethics. 2020;27(6):1450–60.
Krishna L, et al. The role of palliative medicine in ICU bed allocation in COVID-19: a joint position statement of the Singapore Hospice Council and the Chapter of Palliative Medicine Physicians. Asian Bioeth Rev. 2020;12(2):1–7.
Ho S, Tan YY, Neo SH, Zhuang Q, Chiam M, Zhou JX, Woong NL, Lee G, Krishna LK. COVID-19-a review of the impact it has made on supportive and palliative care services within a tertiary hospital and Cancer Centre in Singapore. Ann Acad Med Singap. 2020;49(7):489–95.
Compton S, Sarraf‐Yazdi S, Rustandy F, Radha Krishna LK. Medical students’ preference for returning to the clinical setting during the COVID‐19 pandemic. Med Educ. 2020;54(10):943–50.
Lamiani G, Setti I, Barlascini L, Vegni E, Argentero P. Measuring moral distress among critical care clinicians: validation and psychometric properties of the Italian moral distress scale-revised. Crit Care Med. 2017;45(3):430–7.
Janvier A, et al. Moral distress in the neonatal intensive care unit: caregiver’s experience. J Perinatol. 2007;27(4):203–8.
Lamiani G, et al. Measuring Moral Distress Among Critical Care Clinicians: Validation and Psychometric Properties of the Italian Moral Distress Scale-Revised. Crit Care Med. 2017;45(3):430–7.
Colville GA, et al. A survey of moral distress in staff working in intensive care in the UK. J Intensive Care Soc. 2019;20(3):196–203.
Lamiani G, et al. Clinicians’ moral distress and family satisfaction in the intensive care unit. J Health Psychol. 2018;25:135910531878193.
Cheong CWS, et al. A systematic scoping review of ethical issues in mentoring in internal medicine, family medicine and academic medicine. Adv Health Sci Educ. 2020;25(2):415–39.
Kow CS, et al. A systematic scoping review of ethical issues in mentoring in medical schools. BMC Med Educ. 2020;20(1):246.
Lee FQH, et al. A Systematic Scoping Review of Ethical Issues in Mentoring in Surgery. J Med Educ Curricul Develop. 2019;6:2382120519888915.
Ong YT, et al. Nurturing professionalism in medical schools. A systematic scoping review of training curricula between 1990–2019. Medical Teacher. 2020;42(6):636–49.
Johnson-Coyle L, et al. Moral distress and burnout among cardiovascular surgery intensive care unit healthcare professionals: A prospective cross-sectional survey. Can J Crit Care Nurs. 2016;27(4):27–36.
Larson CP, et al. Moral Distress in PICU and Neonatal ICU Practitioners: A Cross-Sectional Evaluation. Pediatr Crit Care Med. 2017;18(8):e318–26.
de Boer J, et al. Appropriateness of care and moral distress among neonatal intensive care unit staff: repeated measurements. Nurs Critical Care. 2016;21(3):e19–27.
Henrich NJ, et al. Causes of moral distress in the intensive care unit: A qualitative study. J Crit Care. 2016;35:57–62.
Henrich NJ, et al. Consequences of Moral Distress in the Intensive Care Unit: A Qualitative Study. Am J Crit Care. 2017;26(4):e48–57.
Wocial L, et al. Pediatric Ethics and Communication Excellence (PEACE) Rounds: Decreasing Moral Distress and Patient Length of Stay in the PICU. HEC Forum. 2017;29(1):75–91.
Lamiani G, et al. Caring for Critically Ill Patients: Clinicians’ Empathy Promotes Job Satisfaction and Does Not Predict Moral Distress. Front Psychol. 2020;10:2902–2902.
Huang H, Toh RQE, Chiang CLL, Thenpandiyan AA, Vig PS, Lee RWL, et al. Impact of Dying Neonates on Doctors' and Nurses' Personhood: A Systematic Scoping Review. J Pain Symptom Manage. 2021;63(1):e59–74.
Soh TL, Krishna LK, Sim SW, Yee AC. Distancing sedation in end-of-life care from physician-assisted suicide and euthanasia. Singapore Med J. 2016;57(5):220.
Ying PT, Krishna LK, Peng AY. A Palliative Care Model for the Elucidation of Intention within the Multi-Disciplinary Team (MEI). Asian Bioeth Rev. 2015;7(4):359–70.
Wei SS, Krishna LKR. Respecting the wishes of incapacitated patients at the end of life. Ethics & Medicine: An International Journal of Bioethics. 2016;32(1).
Min Kai Chang, M.X.L., Keson Tay, Rachel Jiayu Lee, Dorsett SW Sim, Sumytra Menon, Ravindran Kanesvaran, Rukshini Puvanendran, The Influence of Evolving Confucian Beliefs in the Selection of Proxy Decision-Makers at the End of Life in Singapore. Asian Bioethics Review. 2017;9.
Rachel Jia Yu Lee, D.S.W.S., Keson Tay, Sumytra Menon, Ravindran Kanesvaran, Lalit Kumar Radha Krishna Perceptions of Quality-of-life Advocates in a Southeast Asian Society. Diversity and Equality in Health and Care. 2017.
Kuek JTY, et al. The impact of caring for dying patients in intensive care units on a physician’s personhood: a systematic scoping review. Philosophy, Ethics, and Humanities in Medicine. 2020;15(1):12.
Vig PS, et al. Parental bereavement – impact of death of neonates and children under 12 years on personhood of parents: a systematic scoping review. BMC Palliative Care. 2021;20(1):136.
Radha Krishna LK, Alsuwaigh R. Understanding the fluid nature of personhood - the ring theory of personhood. Bioethics. 2015;29(3):171–81.
Alsuwaigh R, Krishna LK. The compensatory nature of personhood. Asian Bioethics Review. 2014;6(4):332–42.
Alsuwaigh R. How do English-speaking Cancer Patients Conceptualise Personhood? Ann Acad Med Singap. 2015;44(6):207–17.
Ho CY, et al. The impact of death and dying on the personhood of medical students: a systematic scoping review. BMC Med Educ. 2020;20(1):516.
Chan NP, Chia JL, Ho CY, Ngiam LX, Kuek JT, Ahmad Kamal NH, Hanifah Marican Abdurrahman AB, Ong YT, Chiam M, Lee AS, Chin AM. Extending the Ring Theory of Personhood to the Care of Dying Patients in Intensive Care Units. Asian Bioeth Rev. 2022;14(1):71–86.
Hung KC, Lee LW, Liew YX, Krishna L, Chlebicki MP, Chung SJ, Kwa AL. Antibiotic stewardship program (ASP) in palliative care: antibiotics, to give or not to give. Eur J Clin Microbiol Infect Dis. 2022;41(1):29–36.
Heijltjes MT, Morita T, Mori M, Heckel M, Klein C, Stiel S, Miccinesi G, Deliens L, Robijn L, Stone P, Sykes N. Physicians' opinion and practice with the continuous use of sedatives in the last days of life. J Pain Symptom Manage. 2022;63(1):78–87.
Ngiam LXL, et al. Impact of Caring for Terminally Ill Children on Physicians: A Systematic Scoping Review. Am J Hospice Palliative Med. 2020:1049909120950301.
Loh AZ, Tan JS, Jinxuan T, Lyn TY, Krishna LK, Goh CR. Place of care at end of life: what factors are associated with patients’ and their family members’ preferences?. American Journal of Hospice and Palliative Medicine®. 2016;33(7):669–77.
Ong EK, Krishna LK. The sociocultural and ethical issues behind the decision for artificial hydration in a young palliative patient with recurrent intestinal obstruction. Ethics & Medicine: An International Journal of Bioethics. 2015;31(1).
Diehl E, et al. The relationship between workload and burnout among nurses: The buffering role of personal, social and organisational resources. PLoS One. 2021;16(1):e0245798.
Galdikien N, et al. Do nurses feel stressed? A perspective from primary health care. Nurs Health Sci. 2014;16(3):327–34.
White D, Meeker MA. Guiding the Process of Dying: The Personal Impact on Nurses. J Hosp Palliat Nurs. 2019;21(5):390–6.
Ngiam, L.X.L., et al., Impact of Caring for Terminally Ill Children on Physicians: A Systematic Scoping Review. (1938-2715 (Electronic)).
Guba EG, Lincoln YS. Competing paradigms in qualitative research. Handbook of qualitative research. 1994.
Krishna LKR, Renganathan Y, Tay KT, Tan BJ, Chong JY, Ching AH, Prakash K, Quek NW, Peh RH, Chin AM, Taylor D. Educational roles as a continuum of mentoring’s role in medicine–a systematic review and thematic analysis of educational studies from 2000 to 2018. BMC Med Educ. 2019;19(1):1–9.
Mack L. The philosophical underpinnings of educational research; 2010.
Scotland J. Exploring the Philosophical Underpinnings of Research: Relating Ontology and Epistemology to the Methodology and Methods of the Scientific, Interpretive, and Critical Research Paradigms. English. Language Teaching. 2012;5.
Thomas, A., et al., Applications of social constructivist learning theories in knowledge translation for healthcare professionals: a scoping review. (1748-5908 (Electronic)).
Pring R. The ‘false dualism’of educational research. J Philosophy Educ. 2000;34(2):247–60.
Bandura A. Human Agency in Social Cognitive Theory. Am Psychol. 1989;44:1175–84.
Crotty, M., The Foundations of Social Research: Meaning and Perspective in the Research Process. 1998: SAGE.
Ford K. Taking a Narrative Turn: Possibilities. OnCUE Journal: Challenges and Potential Outcomes; 2012.
Sambunjak D, Straus SE, Marusic A. A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med. 2010;25(1):72–8.
Schick-Makaroff K, et al. What Synthesis Methodology Should I Use? A Review and Analysis of Approaches to Research Synthesis. AIMS Public Health. 2016;3:172–215.
Reed DA, et al. Predictive validity evidence for medical education research study quality instrument scores: quality of submissions to JGIM's Medical Education Special Issue. J Gen Intern Med. 2008;23(7):903–7.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Quality Health Care. 2007;19(6):349–57.
Wong G, et al. RAMESES publication standards: Meta-narrative reviews. BMC Med. 2013;11:20.
Popay, J., et al., Guidance on the conduct of narrative synthesis in systematic reviews: A product from the ESRC Methods Programme. 2006.
Peters, M., et al. The Joanna Briggs Institute reviewers' manual 2015: methodology for JBI scoping reviews. 2015.
Peters MD, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–6.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101.
Hsieh H-F, Shannon SE. Three Approaches to Qualitative Content Analysis. Qualitative Health Research. 2005;15(9):1277–88.
France EF, et al. A methodological systematic review of meta-ethnography conduct to articulate the complex analytical phases. 2019;19(1):1–18.
Noblit, G.W., R.D. Hare, and R.D. Hare, Meta-ethnography: Synthesizing qualitative studies. Vol. 11. 1988: sage.
Jameton, A., Nursing Practice: The Ethical Issues. 1984.
Camp M, Sadler J. Moral distress in medical student reflective writing. AJOB Empir Bioeth. 2019;10(1):70–8.
Lomis KD, Carpenter RO, Miller BM. Moral distress in the third year of medical school; a descriptive review of student case reflections. Am J Surg. 2009;197(1):107–12.
Wiggleton C, et al. Medical students' experiences of moral distress: development of a web-based survey. Acad Med. 2010;85(1):111–7.
Miller BM. How Should Resident Physicians Respond to Patients' Discomfort and Students' Moral Distress When Learning Procedures in Academic Medical Settings? AMA J Ethics. 2017;19(6):537–43.
Rees CE, Monrouxe LV, McDonald LA. Narrative, emotion and action: analysing 'most memorable' professionalism dilemmas. Med Educ. 2013;47(1):80–96.
Monrouxe L, Shaw M, Rees C. Antecedents and Consequences of Medical Students' Moral Decision Making during Professionalism Dilemmas. AMA J Ethics. 2017;19(6):568–77.
Weber E, Gray S. How Should Integrity Preservation and Professional Growth Be Balanced during Trainees' Professionalization? AMA J Ethics. 2017;19(6):544–9.
Rubashkin N, Minckas N. How Should Trainees Respond in Situations of Obstetric Violence? AMA J Ethics. 2018;20(1):238–46.
Fuks A. Joining the Club. Perspect Biol Med. 2018;61(2):279–93.
Camp ME, et al. Medical student reflections on geriatrics: Moral distress, empathy, ethics and end of life. Gerontol Geriatr Educ. 2018;39(2):235–48.
Schrepel C, et al. Navigating Cognitive Dissonance: A Qualitative Content Analysis Exploring Medical Students' Experiences of Moral Distress in the Emergency Department. AEM Educ Train. 2019;3(4):331–9.
Glick SB, et al. A systematic review of the causes, impact and response to moral distress among medical students. J Gen Internal Med. 2019;34(2):S119–20.
Dias MPS. Medical students' experiences of moral distress-a cross-sectional observational, web-based multicentre study; 2020.
Perni S, et al. Moral distress and burnout in caring for older adults during medical school training. BMC Med Educ. 2020;20(1):84.
Thurn T, Anneser J. Medical Students' Experiences of Moral Distress in End-of-Life Care. J Palliat Med. 2020;23(1):116–20.
Kuhn E, Lunden L, Moysich P, Rogge K, Roscher M, Caning L, Rogge A. Ethik First–extracurricular support for medical students and young physicians facing moral dilemmas in hospital routine. GMS J Med Educ. 2021;38(4).
Alnazly E, Khraisat OM, Al-Bashaireh AM, Bryant CL. Anxiety, depression, stress, fear and social support during COVID-19 pandemic among Jordanian healthcare workers. Plos one. 2021;16(3):e0247679.
Joshua Tze Yin Kuek, L.X.L.N., Nur Haidah Ahmad Kamal, Jeng Long Chia, Natalie Pei Xin Chan, Ahmad Bin Hanifah Marican Abdurrahman, Chong Yao Ho, Lorraine Hui En Tan, and M.S.Q.K. Jun Leng Goh, Yun Ting Ong, Min Chiam, Annelissa Mien Chew Chin, Stephen Mason, Lalit Kumar Radha Krishna, The impact of caring for dying patients in intensive care units on a physician’s personhood: a systematic scoping review. Philosophy, Ethics, and Humanities in Medicine, 2020.
Sanford DE, Fleming DA. We meant no harm, yet we made a mistake; why not apologize for it? A student's view. HEC Forum. 2010;22(2):159–69.
Kopecky KE, et al. Third-Year Medical Students' Reactions to Surgical Patients in Pain: Doubt, Distress, and Depersonalization. J Pain Symptom Manage. 2018;56(5):719–726.e1.
Haig A, Dozier M, Guide BEME, No. 3: Systematic searching for evidence in medical education - Part 2: Constructing searches. Medical Teacher. 2003;25:463–84.
Gordon M, Gibbs T. STORIES statement: Publication standards for healthcare education evidence synthesis. BMC Medicine. 2014;12(1):143.
Brown-Saltzman K. The gift of voice. Narrat Inq Bioeth. 2013;3(2):139–45.
Whitehead PB, et al. Moral distress among healthcare professionals: report of an institution-wide survey. J Nurs Scholarsh. 2015;47(2):117–25.
Abbasi M, et al. Moral distress in physicians practicing in hospitals affiliated to medical sciences universities. Iran Red Crescent Med J. 2014;16(10):e18797.
Green MM, et al. Moral Distress in Rehabilitation. Pm r. 2017;9(7):720–6.
de Boer JC, et al. Appropriateness of care and moral distress among neonatal intensive care unit staff: repeated measurements. Nurs Crit Care. 2016;21(3):e19–27.
Hamric AB. Moral distress and nurse-physician relationships. Virtual Mentor. 2010;12(1):6–11.
Dodek PM, Cheung EO, Burns KE, Martin CM, Archambault PM, Lauzier F, Sarti AJ, Mehta S, Fox-Robichaud AE, Seely AJ, Parshuram C. Moral distress and other wellness measures in Canadian critical care physicians. Ann Am Thorac Soc. 2021;18(8):1343–51.
Dodek P, et al. Moral distress in intensive care unit personnel is not consistently associated with adverse medication events and other adverse events. J Crit Care. 2019;53:258–63.
Dodek PM, et al. Moral distress in intensive care unit professionals is associated with profession, age, and years of experience. J Crit Care. 2016;31(1):178–82.
Dodek PM, et al. Moral distress is associated with general workplace distress in intensive care unit personnel. J Crit Care. 2019;50:122–5.
Fujii T, Katayama S, Nashiki H, Niitsu T, Takei T, Utsunomiya A, Miyazaki K, Dodek P, Hamric A, Nakayama T. Moral distress, burnout, and coping among intensive care professionals in Japanese ICUs [videorecording]: European Society of Intensive Care Medicine; 2018.
Hamric AB, Blackhall LJ. Nurse-physician perspectives on the care of dying patients in intensive care units: collaboration, moral distress, and ethical climate. Critical care medicine. 2007;35(2):422–9.
Dombrecht L, Cohen J, Cools F, Deliens L, Goossens L, Naulaers G, Beernaert K, Chambaere K. Psychological support in end-of-life decision-making in neonatal intensive care units: full population survey among neonatologists and neonatal nurses. Palliat Med. 2020;34(3):430–4.
Dodek PM, Norena M, Ayas N, Wong H. The Relationship Between Moral Distress And Adverse Safety Events In Intensive Care Units. D23 QUALITY IMPROVEMENT IN CRITICAL CARE: American Thoracic Society; 2013. p. A5330–A.
Dzeng E, et al. Moral Distress Amongst American Physician Trainees Regarding Futile Treatments at the End of Life: A Qualitative Study. J Gen Intern Med. 2016;31(1):93–9.
Neumann JL, et al. Burnout, Moral Distress, Work-Life Balance, and Career Satisfaction among Hematopoietic Cell Transplantation Professionals. Biol Blood Marrow Transplant. 2018;24(4):849–60.
Epstein EG, et al. Enhancing Understanding of Moral Distress: The Measure of Moral Distress for Health Care Professionals. AJOB Empir Bioeth. 2019;10(2):113–24.
Trotochaud K, et al. Moral Distress in Pediatric Healthcare Providers. J Pediatr Nurs. 2015;30(6):908–14.
Lamiani G, et al. Clinicians' moral distress and family satisfaction in the intensive care unit. J Health Psychol. 2020;25(12):1894–904.
Prentice T, et al. Moral distress within neonatal and paediatric intensive care units: a systematic review. Arch Dis Childhood. 2016;101(8):701–8.
Jones GAL, et al. Psychological impact of working in paediatric intensive care. A UK-wide prevalence study. Arch Dis Child. 2020;105(5):470–5.
Abbasi M, et al. Moral distress in physicians practicing in hospitals affiliated to medical sciences universities. Iran Red Crescent Med J. 2014;16(10).
Nejadsarvari N, et al. Relationship of Moral Sensitivity and Distress Among Physicians. Trauma Mon. 2015;20(2):e26075.
Førde R, Aasland OG. Moral distress among Norwegian doctors. J Med Ethics. 2008;34(7):521–5.
Aguilera D, et al. Moral distress in pediatric hematology/oncology physicians. Pediatr Blood Cancer. 2014;61:S32.
Zaidi D, et al. Clerkship Ethics: Unique Ethical Challenges for Physicians-in-Training. HEC Forum. 2020;32(2):99–109.
Franco RS, et al. To participate or not participate in unprofessional behavior-Is that the question? Medical Teacher. 2017;39(2):212–9.
Chai HZ, Krishna LKR, Wong VHM. Feeding: What It Means to Patients and Caregivers and How These Views Influence Singaporean Chinese Caregivers’ Decisions to Continue Feeding at the End of Life. Am J Hospice Palliative Med. 2014;31(2):166-171.
Chong JA, et al. Patient and family involvement in decision making for management of cancer patients at a centre in Singapore. BMJ Support Palliat Care. 2015;5(4):420–6.
Ho ZJM, Radha Krishna LK, Yee CPA. Chinese familial tradition and Western influence: a case study in Singapore on decision making at the end of life. Journal of pain and symptom management. 2010;40(6):932–7.
Marc Ho ZJ, et al. The physician–patient relationship in treatment decision making at the end of life: A pilot study of cancer patients in a Southeast Asian society. Palliative and Supportive Care. 2013;11(1):13–9.
Krishna L. Nasogastric feeding at the end of life: A virtue ethics approach. Nursing Ethics. 2011;18(4):485–94.
Krishna LK. Decision-making at the end of life: A Singaporean perspective. Asian Bioethics Review. 2011;3(2):118–26.
Krishna LK, Watkinson DS, Beng NL. Limits to relational autonomy--the Singaporean experience. Nurs Ethics. 2015;22(3):331-340.
Lalit Krishna M. The position of the family of palliative care patients within the decision-making process at the end of life in Singapore. Ethics Med. 2011;27(3):183.
Radha Krishna LK. Personhood within the context of sedation at the end of life in Singapore. BMJ Case Reports. 2013;2013:bcr2013009264.
Radha Krishna LK. Accounting for personhood in palliative sedation: the Ring Theory of Personhood. Med Humanit. 2014;40(1):17–21.
Tan R, et al. Medical Student Portfolios: A Systematic Scoping Review. J Med Educ Curricular Develop. 2022;9:23821205221076024.
Acknowledgements
The authors would like to thank the anonymous reviewers whose advice and feedback greatly improved this manuscript.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
RSRO, RSMW, RCHC, CWNQ, NB, CYLL, YAW, AKLC, AYTT, AP, SWKC, GSS, NT, AMCC, LKRK were involved in data curation, formal analysis, investigation, preparing the original draft of the manuscript as well as reviewing and editing the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
NA.
Consent for publication
NA.
Competing interests
None of the authors have competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix A.
Pubmed Search Strategy. Search strategy employed as part of the systematic scoping review (SSR) process, Stage 1.
Additional file 2: Appendix B.
Summary of included articles. Summaries of key points of articles included with MERSQI and COREQ.
Additional file 3: Appendix C.
Summary of Direct-Content Analysis (DCA) Themes. Impact of Moral Distress according to the Innate, Individual, Relational and Societal Rings of Personhood.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ong, R.S.R., Wong, R.S.M., Chee, R.C.H. et al. A systematic scoping review moral distress amongst medical students. BMC Med Educ 22, 466 (2022). https://doi.org/10.1186/s12909-022-03515-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-022-03515-3