Abstract
Background
Patients’ knowledge of their atrial fibrillation (AF) and anticoagulation therapy are determinants of the efficacy of thromboprophylaxis. Nurses may be well placed to provide counselling and education to patients on all aspects of anticoagulation, including self-management. It is important that nurses are well informed to provide optimal education to patients. Current practice and knowledge of cardiovascular nurses on AF and anticoagulation in the Australian and New Zealand (ANZ) context is not well reported.
This study aimed to; 1) Explore the nurse’s role in clinical decision making in anticoagulation in the setting of AF; 2) Describe perceived barriers and enablers to anticoagulation in AF; 3) Investigate practice patterns in the management of anticoagulation in the ANZ setting; 4) Assess cardiovascular nurses’ knowledge of anticoagulation.
Methods
A paper-based survey on current practices and knowledge of AF and anticoagulation was distributed during the Australian Cardiovascular Nursing College (ACNC) Annual Scientific Meeting, February 2014. This survey was also emailed to Cardiovascular Trials Nurses throughout New South Wales, Australia and nursing members of the Cardiac Society of Australia and New Zealand (CSANZ).
Results
There were 41/73 (56 %) respondents to the paper-based survey. A further 14 surveys were completed online via nurse members of the CSANZ, and via an investigator developed NSW cardiovascular trials nurse email distribution list. A total of 55 surveys were completed and included in analyses. Prior education levels on AF, stroke risk, anticoagulation and health behaviour modification were mixed. The CHA2DS2VASc and HAS-BLED risk stratification tools were reported to be underused by this group of clinicians. Reported key barriers to anticoagulation included; fears of patients falling, fears of poor adherence to medication taking and routine monitoring. Patient self-monitoring and self-management were reported as underutilised. ANZ cardiovascular nurses reported their key role to be counselling and advising patients on therapy regimens. Anticoagulant-drug interaction knowledge was generally poor.
Conclusion
This study identified poor knowledge and practice in the areas of AF and anticoagulation. There is scope for improvement for cardiovascular nurses in ANZ in relation to AF and anticoagulation knowledge and practice.
Similar content being viewed by others
Background
Atrial fibrillation (AF) is the most common cardiac rhythm irregularity and increases stroke risk three to five-fold [1]. The population prevalence is estimated at 2.3–3.4 %. The lifetime risk of AF is approximately 1 in 4 [1]. This incidence increases with age and rises to affect 11 % of the population over 80 years [2]. This primarily cardiogeriatric condition is characterised by chaotic electrical activity in the upper chambers of the heart. Stroke and thromboembolism are major complications of AF. Evidence-based interventions to reduce stroke risk in AF include anticoagulation and the insertion of a left atrial appendage (LAA) device, as well as the rhythm control methods such as cardioversion and catheter ablation [3]. Oral anticoagulation is the most common way to reduce stroke risk in individuals with AF. Whilst the recent advent of new oral anticoagulants (NOACs) such as the thrombin inhibitor dabigatran, and factor Xa inhibitors rivaroxaban and apixaban have held the promise of simplified dosing without the need for frequent blood testing, concerns persist of bleeding risk and the lack of any reversal agent for these agents [3]. To date, warfarin remains the most commonly used oral anticoagulant, and its use is inherently burdensome. This burden is often related to the need for routine monitoring, adaptation of lifestyle habits and more often than not; complex dosing requirements [4]. The quality of overall anticoagulation quality can be assessed by an individual’s time in therapeutic range. An individual with AF should aim to maintain their INR between 2 and 3 [5, 6]. However, many individuals may find this challenging to achieve due to a variety of factors. Unstable INRs are likely to be a consequence of medication, food or lifestyle interactions [7]. Quality anticoagulation is reliant on patients and caregivers’ knowledge of their chronic condition and anticoagulation therapy [8]. The often lifetime duration of treatment increases the complex issues of adherence, and emphasises the need for education refreshment throughout all care settings. Previous studies have highlighted that clinicians including physicians, pharmacists, dieticians and nurses fail to meet adequate knowledge levels to provide accurate and up-to-date information to patients [9, 10]. A recent European study drew attention to the need for improvement in cardiovascular nurses’ knowledge and practice on oral anticoagulant therapy [9]. With an increasing prevalence of AF, there is greater need for innovative strategies to improve patient outcomes. Strategies may include patient self-testing and self-management. The success of these strategies are dependent upon appropriate patient selection [11]. Patients must have good manual dexterity and cognitive abilities [12]. Further, they must be adept in managing the device; interpreting, understanding and taking action based on results. Self-testing and self-management should not be discounted by clinicians, as a method to improve knowledge, self-efficacy, overall quality of anticoagulation, and patient outcomes [11]. Nurses account for greater than 50 % of the health workforce in Australia and often spend the most time with patients providing clinical care. They are experienced in counselling, therefore, may be well-placed to provide patient education on anticoagulation and promote self-management during regular healthcare interactions.
Study aim
The aim of this study was to:
-
1)
Explore the nurse’s role in clinical decision-making in anticoagulation in the setting of AF.
-
2)
Describe perceived barriers and enablers to anticoagulation in AF.
-
3)
Investigate practice patterns in the management of anticoagulation.
-
4)
Assess cardiovascular nurses’ knowledge of anticoagulation.
Methods
Design, setting and sample
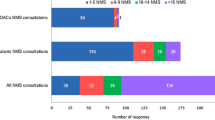
Data were collected by survey methods. The survey was conducted at the 8th Annual Scientific Meeting of the Australian Cardiovascular Nursing College, Gold Coast, Australia on 22nd Feb 2014. All delegates attending on this date were invited to participate in the study. Additional responses were sought via an email distribution list of the Nurses Council of the Cardiac Society of Australia and New Zealand, and a state-wide cardiovascular research nurse email distribution list. Additionally, nurses working in a single site CCU of a metropolitan teaching hospital were invited to participate. (Refer to Table 1 for sampling frame response).
Measurements and item generation
A self-report questionnaire, recently used during a European study of cardiovascular nurses was used to assess variables related to warfarin-drug, warfarin-food interactions and knowledge on novel anticoagulants and self-management [9]. Permission to reproduce these survey items was approved by the corresponding author. The original questionnaire was reported as demonstrating good face validity. Study investigators reviewed the original survey used in Europe, and felt that the variables and items included were applicable to the ANZ setting, given the similarities in westernised healthcare systems and availability of pharmacological agents at the time of the survey. Additional investigator developed questions were included; these were developed following consultation with expert cardiovascular nurses and an extensive review of the literature. Some questions were adapted from other surveys that addressed barriers to anticoagulation or elicited the cardiovascular nurse’s role in decision-making around anticoagulation therapy [13]. The questionnaire was distributed in English.
Data collection
All delegates were provided with a paper-based survey on their chair during the session and invited by the convenor to participate. Attendees were asked to place the completed questionnaires in a designated collection box following the session. Subsequent to the conference, the same survey was electronically distributed to nursing members of the Cardiac Society of Australia and New Zealand and via a state-wide cardiovascular research nurse email distribution list. Additionally, nurses working in the hospital CCU were invited to participate. The hospital site was selected for inclusion, due to the locality of the site in relation to the research team’s clinical practice setting. Online survey methods have previously been used to gain understanding of practice patterns in the ANZ setting [14]. Therefore, the research team believed this would yield worthy response and enhance findings from the paper-based survey. To address the potential for selection bias, a poster and box was placed in the ward setting for clinicians to provide responses. A notification for completion of the electronic survey was sent electronically once, and no reminders were sent. Within the electronic survey information, participants were advised that this survey was previously undertaken at the recent ACNC conference, and asked not to complete if they had already participated.
Data management and data analysis
The online survey was conducted using the web-based SurveyMonkey™ platform ( www.surveymonkey.com ) and remained open until 12/05/2014. Paper based surveys were manually entered into the electronic system; this assisted in accounting for missing values. The survey ascertained the basic demographic and education characteristics of nurses related to highest qualification and length of time working in cardiovascular nursing. Descriptive analyses were used to describe the sample and the responses to study variables.
Ethical considerations
This study was approved by the St Vincent’s Hospital, Sydney (Ref: LNR/12/SVH/62) and University of Technology Sydney (Ref: 2013000181) human research ethics committees. Approval was provided for both online and paper-based surveys at the conference. The executive committee of the Australian Cardiovascular Nursing College approved survey distribution during the conference event. All conference attendees were informed of the aims of the study. Informed consent was implied by the completion of the survey. No identifying information was collected from the participants to assure confidentiality.
Results
Sample characteristics, demographic information and experience
A total of 55 responses were included in the analyses. The table above identifies most responses were from the ACNC conference, with a response rate of 56 %. Unfortunately, e-survey distributed by CSANZCNC once received two responses, notwithstanding the reach of the email to 320 members. A possible reason for this may be that some of the members of CSANZCNC are also members of ACNC, and had attended the conference, and previously participated in the survey. Most respondents were female 86 % (n = 47), the majority of respondents 91 % (n = 50) came from the three most populated states in Australia (New South Wales, Victoria and Queensland). The remaining respondents were from New Zealand 9 % (n = 5). The majority worked in a metro area 71 % (n = 39), and held a Bachelor degree qualification or above 85 % (n = 47). 33 % (n = 18) identified their current role as Registered Nurse (RN). Though, the seniority of the clinicians was also reflected by the number in expert positions, 36 % (n = 36) identified as Clinical Nurse Consultants or Nurse Practitioners. Three respondents were not clinicians and were employed in the higher education & research sectors. Most 77 % (n = 40) had over 10 years of clinical experience, and 62 % (n = 34) had worked in cardiovascular nursing specialty practice for more than 10 years. Baseline demographic information is summarised in Table 2.
Participation in formal educational programs was reported to be 41–61 % across four associated topics. 48 % had attended a previous education program about AF, 41 % about stroke risk, 57 % about anticoagulation and 61 % about health behaviour modification. Previous education participation is summarised in Table 3.
Adverse outcomes
Fifty percent of respondents had cared for a patient with AF who had experienced an intracranial haemorrhage when receiving anticoagulation. And 74 % of respondents had cared for a patient with AF who had experienced a stroke whilst not receiving anticoagulation. Results are summarised in Table 4.
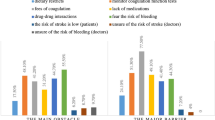
Nurses role in decision making and anticoagulation
Results of the nurses’ role in decision making are summarised in Table 5. More than half of respondents (54 %, n = 29) said they were not involved in multidisciplinary team (MDT) discussions when making treatment decisions on anticoagulation management with patients with AF. Nearly half of respondents agreed (44 %, n = 24) or strongly agreed (7 %, n = 4) that the risk of stroke versus the risk of bleeding was clearly articulated to patients at commencement of anticoagulation for stroke prevention in AF. Most disagreed (41 %, n = 22) or strongly disagreed (13 %, n = 7) that they were unsure to advocate for thromboprophylaxis or not, when involved in team decisions. Most disagreed (50 %, n = 27) or strongly disagreed (6 %, n = 3) that it was difficult to decide where the benefits of thromboprophylaxis outweighed the risks of haemorrhage. Over half disagreed (57 %, n = 30) that they did not feel they knew enough about the risks and benefits of different anticoagulants.
Most respondents (57 %, n = 31) agreed that they took time to understand their patients views on the risks and benefits of anticoagulation, and that they (52 %, n = 28) felt that generally, their patients were well informed about their risks and benefits of anticoagulation at the time of commencement. Just under half (n = 26, 48 %) agreed that their patients received comprehensive education about anticoagulation prior to discharge after hospitalisation. Stroke and bleeding risk stratification tools were reported to be underutilised by this group of clinicians. Specifically, only 25 % (n = 13) agreed that they used a CHADS2 or CHA2DS2-VASc tools, whilst only 18 % (n = 9) agreed they used the HAS-BLED tool, despite the fact that both are recommended in international guidelines for anticoagulation in AF [5]. Over half (n = 28, 52 %) agreed, or strongly agreed that they made use of a shared decision-making model of care to explain the risks and benefits of anticoagulation for stroke prevention in AF.
Barriers to anticoagulation
Barriers to anticoagulation are summarised in Table 6. Barriers to anticoagulation included fears of the patient falling (75 %, n = 39), fears of poor adherence to: routine monitoring (75 %, n = 39) and medication taking (71 %, n = 36). Other barriers included lack of social support (e.g. patient living alone, or a lack of a caregiver), (41 %, n = 21), and fears of poor literacy (26 %, n = 13). Factors facilitating optimal management of thromboprophylaxis were identified, these are summarised in Tables 7 and 8.
Practice patterns
Results of practice patterns are summarised in Tables 9 and 10. Warfarin remains the most widespread anticoagulant used in daily practice for this cohort of clinicians (100 %, n = 51). Less extensive use of the novel agents was reported. Only 16 % (n = 8) of respondents stated that most patients would be given a choice of anticoagulant, 82 % (n = 41), stated that ‘some’ patients may be offered new anticoagulants. 59 % (n = 29) of respondents stated that patients may modify therapy based on difficulties maintaining INR within therapeutic range (i.e. 2–3). Patient self-testing and self-management were not offered by 60 %, (n = 30) of respondents and 28 %, (n = 14) had never heard of such services. One respondent highlighted a possible rationale for this could be the limited remuneration and funds for the use of point-of-care machines. It was also noted by another that pharmacists had a key role in counselling and education prior to discharge following a hospitalisation. A number of respondents highlighted that the role of decision-making around anticoagulation is usually lead by the physician, cardiologist or GP and often the nurses and patients input were minimal.
Cardiovascular nurses’ knowledge on warfarin interactions
The majority of respondents (n = 34, 69 %) answered correctly that aspirin enhanced the effect of oral warfarin anticoagulation therapy. It is of concern that 48 % (n = 23) of respondents answered incorrectly to interactions related to ibuprofen and 48 % (n = 23) did not know of interactions with topical salicylates. Whilst ibuprofen has no effect on oral anticoagulant therapy, it may impact on overall haemostasis and may increase the risk of gastrointestinal bleeding when used in combination with oral anticoagulants [15]. Only 23 % (n = 11) of respondents answered correctly that topical salicylates enhance oral warfarin anticoagulant therapy. Whilst results of how cardiac agents including propanolol, cholestyramine and atenolol trend towards the correct answers (propanolol enhancing, cholestyramine inhibiting and atenolol having no effect), the rate of respondents who did not know the interactions of these cardiac agents on warfarin therapy was 44–67 %. Only 9–22 % answered the questions on warfarin interactions with gastrointestinal agents correctly. More than two-thirds answered “don’t know” to the question on sucralfate-warfarin interaction. The majority of respondents did not know how any of the vitamin supplements listed affected warfarin therapy (range 42–58 % across the 5 supplements). The questions on the interaction between antibiotics and warfarin were poorly completed; the majority of respondents answered “don’t know”. Results on warfarin interactions are summarised in Table 11.
Cardiovascular nurses’ knowledge on warfarin related advice
There were eight questions that assessed cardiovascular nurse’s knowledge on warfarin advice. Responses are summarised in Table 11. Most questions were answered correctly with the exception of advice around warfarin use and pregnancy. 70 % (n = 34) of respondents knew that patients who are taking warfarin can consume spinach, however that they need to eat the same amount regularly every week. Over half (55 %, n = 26) correctly answered that consuming three glasses of wine will cause an increased in INR. Yet, 21 % (n = 10) of respondents did not know the answer to this question. 88 % (n = 44) of cardiovascular nurses knew that the best time of day to take warfarin was the evening, and 90 % (n = 45) were aware that patients with a stable INR should have it checked every 4 weeks. Only 58 % (n = 29) of nurses would have given correct advice to patients on the action to take if a patient remembered missing a last dose. Over three quarters (76 %, n = 38) of respondents correctly answered that once warfarin is ceased, it takes 5 days to be cleared from the patient’s body. Most (84 %, n = 43) nurses correctly identified that the length of time a patient is expected to be taking warfarin is patient centric, and dependant on individual needs. Only 12 % (n = 6) of respondents correctly answered that women who are pregnant can safely take warfarin during the second and third trimester. Less than half, 48 % (n = 24) of respondents incorrectly answered this question, wrongly identifying that pregnant women should not take warfarin, which is concerning around the correct information provision to this patient population.
Discussion
This study demonstrates that cardiovascular nurses in Australia and New Zealand have insufficient knowledge on oral anticoagulant therapy, warfarin-diet, and warfarin-medication interactions. Our findings are consistent with recent international research [7, 9]. The less extensive reported use of novel agents may be due to their gradual introduction to the Pharmaceutical Benefit Scheme (PBS). The PBS is the national pharmaceutical rebate scheme providing medicines at a government-subsidised price. It is of concern that such a small percentage stated that most patients would be given a choice of anticoagulant. There remains considerable scope for improvement in this area of shared decision-making.
The lack of knowledge of warfarin-medication interactions is alarming. It is of concern at the lack of knowledge on warfarin related advice, particularly pertaining to pregnancy and how alcohol affects INR. Our findings represent a typically older and more experienced cardiovascular nursing population, working in specialised positions with advanced qualifications. And as such, are likely to be more knowledgeable on anticoagulation than other nurses. Given the overall poor results, it is feared that knowledge is likely to be even poorer in the broader nursing population.
Practice patterns
The cardiovascular nurses surveyed stated that warfarin remains the most widespread oral anticoagulant for stroke prevention in AF, whilst NOACs are reported to have lesser usage. It is concerning that only 16 % of respondents stated that most patients would be given a choice. It appears that there is scope for improvement in the practice of shared decision-making and patient-centred care. It is important that nurses maintain an active role in the decision-making processes and act as an advocate for patients and caregivers. This may be particularly problematic when patients are presented with complex risk calculators and benefit statistics of various treatments. Patient self-testing and self-management strategies have been not yet been embraced as innovative practices that support able patients. Barriers to patient self-management and self-testing include frailty, poor manual dexterity and cognitive dysfunction [12]; however these practices should not be discounted by clinicians. Additionally, a poor rebate for self-testing devices may also impede uptake in Australia and New Zealand. The nurse’s role in education and counselling on anticoagulation was highlighted. Some respondents expressed that they often delegate this to the pharmacist for education. This practice appears commonplace, and is worrisome. A respondent expressed “most times, little education is given”. This has immense implication for the quality of thromboprophylaxis.
Knowledge
Cardiovascular nurses must ensure that they are up-to-date with current evidence-based information on AF and anticoagulation therapy to inform the education and care they provide to patients. Incorrect and inaccurate knowledge on drug-drug, drug-food interactions and monitoring requirements was prevalent among the respondents to our survey. This may lead to inappropriate patient counselling and education. This would adversely impact patient outcomes. It is therefore vital that cardiovascular nurses are knowledgeable and keep abreast with new information related to AF and anticoagulation practices. Support for self-testing and self-management practices must be preferred over teaching alone. Nurses are best-placed to provide ongoing counselling throughout the spectrum of care; from hospitalisation to discharge and within primary care settings. However, the quality of this counselling is dependent on a strong contemporary knowledge base. Cardiovascular nurses must refrain from simple task delegation of anticoagulation education to pharmacists or other clinicians, it is important to adopt a combined and comprehensive approach. This may assist in optimising therapy, improving issues of adherence and ultimately patient outcomes. Clinicians must engage further with this topic to ensure safe care. Results from this study highlight the need for cardiovascular nurses to maintain a contemporary knowledge base. The Australian Health Practitioner Regulation Agency (AHPRA) mandates that all registered nurses must participate in at least 20 h of continuing nursing professional development per year that is relevant to the context of practice [16]. Education modules specific to AF and anticoagulation, including stroke and bleeding risk and lifestyle modification may be of assistance in maintaining minimum standards for continuing professional development for cardiovascular nurses.
Limitations
This study has some limitations. Firstly, whilst the response rate of 58 % to the paper-based survey distributed during the conference is encouraging, the generalizability of these findings is difficult. These findings represent a typically older and more experienced cardiovascular nursing population, working in specialised positions with higher qualifications. Therefore this may not be representative of the general Australian and New Zealand cardiovascular nursing population whom provide bedside patient education on anticoagulation. Secondly, the majority of respondents (80 %) were attending a cardiovascular nursing conference, for many of the workforce this remains a privilege to secure funding and time to attend such professional development events. The seniority of respondents may reflect the demographic that normally attends conferences, hold a professional society membership or has access to a workplace email account. Again, this limits the generalizability of findings.
Conclusions
The results of our study demonstrate that of the cardiovascular nurses surveyed in Australia and New Zealand most had inadequate knowledge on oral anticoagulant therapy. There is need for improvement, to ensure quality of care for patients with AF receiving anticoagulation. Cardiovascular nurses need to be able to provide accurate, robust and timely advice to patients to topics including lifestyle, medication and food interactions to anticoagulation. A lack of knowledge on these topics may contribute to inappropriate counselling and education. Further, the communication of inaccurate information may implicitly reinforce myths and misconceptions around anticoagulation. The education of patients on anticoagulation is not a role of a single health professional. A team approach must be taken and nurses have a key role in providing answers to questions and sound clinical advice across all care settings. Future research should address modes of delivery of AF and anticoagulation education for clinicians, individuals and their caregivers.
Implications for Clinical Practice |
|---|
• ANZ cardiovascular nurses need to improve their knowledge on oral anticoagulant therapy. |
• Lack of clinician knowledge may lead to inaccurate patient advice and impact adherence to therapy. |
• Including a comprehensive education program pre-discharge may help to improve the quality and safety of anticoagulation |
• Cardiovascular nurses need to be more actively involved in anticoagulation decision making in the clinical setting. |
• Due to the duration of therapy for this chronic condition, there is need for education refreshment and re-assessment of patients and clinicians knowledge, across all care settings. |
• There is need to explore the scope for professional organisations to credential nurses on AF and anticoagulation. |
References
Ball J, Carrington M, McMurray JJV, Stewart S. Atrial fibrillation: Profile and burden of an evolving epidemic in the 21st century. Int J Cardiol. 2013;167(5):1807–24.
Shea JB, Sears SF. A patient’s guide to living with atrial fibrillation. Circulation. 2008;117(20):e340–3.
Ferguson C, Inglis SC, Newton PJ, Middleton S, Macdonald PS, Davidson PM. Atrial fibrillation: Stroke prevention in focus. Australian Critical Care. 2013;27(2):92–98.
Ferguson C, Inglis SC, Newton PJ, Middleton S, Macdonald PS, Davidson PM. Atrial fibrillation and thromboprophylaxis in heart failure: The need for patient-centered approaches to address adherence. Vasc Health Risk Manag. 2013;9(1):3–11.
Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation. Eur Heart J. 2012;33:2719–47.
Wann LS, Curtis AB, January CT, Ellenbogen KA, Lowe JE, Estes M, et al. 2011 ACCF/ AHA/ HRS focused update on the management of patients with atrial fibrillation: a report of the american college of cardiology foundation/ american heart association task force on practice guidelines. Circulation. 2011;1234:104–23.
Couris R, Tataronis G, McCloskey W, Oertel L, Dallal G, Dwyer J, et al. Dietary vitamin K variability affects International Normalized Ratio (INR) coagulation indices. International journal for vitamin and nutrition research. Internationale Zeitschrift fur Vitamin- und Ernahrungsforschung. Int J Vitam Nutr Res. 2006;76(2):65–74.
Ferguson C, Inglis SC, Newton PJ, Middleton S, Macdonald PS, Davidson PM. The caregiver role in thromboprophylaxis management in atrial fibrillation: A literature review. Eur J Cardiovasc Nurs. 2015;14(2):98–107.
Oterhals K, Deaton C, De Geest S, Jaarsma T, Lenzen M, Moons P, et al. European cardiac nurses’ current practice and knowledge on anticoagulation therapy. Eur J Cardiovasc Nurs. 2014;13(3):261–9.
Couris RR, Tataronis GR, Dallal GE, Blumberg JB, Dwyer JT. Assessment of healthcare professionals’ knowledge about warfarin-vitamin K drug-nutrient interactions. J Am Coll Nutr. 2000;19(4):439–45.
Heneghan C, Alonso-Coello P, Garcia-Alamino JM, Perera R, Meats E, Glasziou P. Self-monitoring of oral anticoagulation: a systematic review and meta-analysis. Lancet. 2006;367(9508):404–11.
Dolor RJ, Ruybalid RL, Uyeda L, Edson RG, Phibbs C, Vertees JE, et al. An evaluation of patient self-testing competency of prothrombin time for managing anticoagulation: pre-randomization results of VA Cooperative Study #481--The Home INR Study (THINRS). J Thromb Thrombolysis. 2010;30(3):263–75.
Gattellari M, Worthington J, Zwar N, Middleton S. Barriers to the use of anticoagulation for nonvalvular atrial fibrillation. Stroke. 2008;39:227–30.
Newton P, Davidson P, Sanderson C. On behalf of the improving palliative care through clinical trials group. An online survey of Australian physicians reported practice with the off-label use of nebulised frusemide. BMC Palliat Care. 2012;11(1):6.
Ansell J, Hirsh J, Hylek E, Jacobson A, Crowther M, Palareti G. Pharmacology and management of the vitamin K antagonists. Chest. 2008;133(6 suppl):160S–98S.
Australian Health Practitioner Regulation Agency (AHPRA). Nursing and Midwifery Continuing Professional Development Registration Standard. 2010. Accessed 4th August 2014, 2014.
Acknowledgements
The authors would like to express thanks to; Kjersti Oterhals et al. for granting permission to reproduce the survey items previously published in the European Journal of Cardiovascular Nursing 2014 Vol. 13(3) 261–269; the executive committee, members and delegates of the Australian Cardiovascular Nursing College; the nursing council executive committee and nurse members of the Cardiac Society of Australia and New Zealand; and all other participants for their support and contribution to the survey.
This research received funding from the Australian College of Nursing, through a grant of $5,000 awarded in 2013 to support the ‘Atrial Fibrillation and Stroke Thromboprophylaxis in hEart Failure’ (AFASTER) Study. Dr. Caleb Ferguson is currently supported by a UTS Doctoral Scholarship (2012–2015).
Associate Professor Sally C Inglis is currently supported by a Cardiovascular Research Network Life Science Research Fellowship supported by the Heart Foundation and the NSW Office for Medical Research (CR 11S 6226).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors have no conflicts of interest to declare.
Authors’ contributions
CF: Study design, data collection, data analysis and interpretation, manuscript preparation. SCI: Study design, data collection, data analysis and interpretation, manuscript preparation. PJN: Study design, data collection, data analysis and interpretation, manuscript preparation. SM: data analysis and interpretation, interpretation, manuscript preparation. PSM: Study design, data analysis and interpretation, manuscript preparation. PMD: Study design, data analysis and interpretation, manuscript preparation. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ferguson, C., Inglis, S.C., Newton, P.J. et al. Education and practice gaps on atrial fibrillation and anticoagulation: a survey of cardiovascular nurses. BMC Med Educ 16, 9 (2016). https://doi.org/10.1186/s12909-015-0504-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12909-015-0504-1