Abstract
Background
Breast Cancer (BC) is the most common cancer in women worldwide and, although 70% of patients are responsive to selective Estrogen Receptor (ER) modulators such as Tamoxifen (Tam), patients’ survival is comprised by resistance to endocrine therapy. Brazilian flora, especially the Amazon biome, is one of the richest global sources of native species with potentially bioactive compounds. Arrabidaea chica is a plant native to the Amazon that has been used in the treatment of different diseases. However, its action on BC remains unclear.
Methods
Herein the biological effects of the chloroform extract of A. chica (CEAC) were evaluated on BC cells and in in vivo model. After confirmation of CEAC antioxidant capacity, cells were treated with CEAC and Tam, alone and with CEAC+Tam. The cell viability was evaluated by MTT and hormone receptor transcripts levels were assessed (ESR1, ESR2 and AR). Finally, anticarcinogenicity of CEAC was recorded in Drosophila melanogaster through Epithelial Tumor Test (ETT).
Results
The study confirmed the antioxidant activity of CEAC. CEAC was selective for MCF-7, downregulating ESR2 and AR transcripts and upregulating ESR2 expression. The modulatory effects of CEAC on ERs did not differ between cells treated with Tam and with CEAC+Tam. Interestingly, previous treatment with CEAC, followed by treatment with Tam promoted a significant decrease in cell viability. The extract also presented anticarcinogenic effect in in vivo assay.
Conclusion
The bioassays on breast tumor cells demonstrated the antiproliferative activity of the extract, which modulated the expression of hormone receptors and sensitized luminal tumor cells to Tam. These results suggest that CEAC could be a complementary treatment for BC.
Similar content being viewed by others
Background
Epidemiological data on cancer are still alarming with an annual global incidence of over 439.2 new cases per 100,000 men and women per year. In 2020, there were estimated 9.9 million deaths [1, 2]. Breast cancer (BC) remains the most common non cutaneous tumor among women worldwide [3,4,5]. Its occurrence is steadily increasing in developing countries in which between 1 in 8 (about 12%) women will develop invasive BC during her lifetime [6, 7]. Worldwide, 2,088,849 million new BC cases and 626,679 deaths were recorded in 2018, expecting 3 million cases in 2030 [8].
BC is a hormone-related tumor [9, 10]. Therefore, nuclear receptor (NR) family of transcription factors plays essential roles in development and maintenance of malignant breast cells [11]. Estrogen receptor (ER) and Androgen receptor (AR) are frequently co-expressed in BC, although they may behave in different ways in view of the tumor heterogeneity [12]. ER-α and ER-β have similar binding affinities for estrogens; share a high degree of homology in the DNA-binding regions but interact with different other proteins suggesting divergence in transcriptional machinery control [13]. Although distinct genes codify for ER-α and ER-β, they can exist as heterodimer, and ER-β may modulate ER-α activity [14]. AR is structurally similar to ERs and how it drives, promotes or controls breast tumorigenesis remains largely unexplored [15, 16].
In this context, assessment of a breast cancer’s receptor status is essential to classify and define therapeutic strategies [17]. Accordingly, BC is categorized in four main molecular subtypes based on ER-α, progesterone receptor (PgR), and human epidermal growth factor receptor 2 (Her2) expression [11]. The tumors are divided into Luminal type expressing ER and/or PgR, being Luminal A when lack Her2, and Luminal B when express high levels of Ki67. Luminal B may or may not express Her2. Her2 enriched are BC which are negative for hormone receptors and present high levels of Her2. Finally, triple-negative BC do not express any of above markers [18, 19].
Nearly 70% of breast tumors express hormone receptors (ER and/or PgR) with better outcomes [20, 21]. Moreover, a high prevalence of ER-positive BCs express the androgen receptor (AR), and AR expression may be also associated with better outcome [22]. ER-α-positive BCs initially respond to antagonists or antiestrogens and pre- and postmenopausal women have benefited from these therapeutic strategies [23]. These tumors are mainly treated with Tamoxifen (Tam), which has been clinically used for the last 40 years [24]. Tam is a triphenylethylene derivative that functions as selective ER modulator (SERM) [25, 26]. In the breast, Tam acts as an antagonist that binds to ER and impairs estrogenic effects [27, 28]. Tam can reduce the chance of recurrence in 40 to 50% after 5 years and 30% after 10 years of treatment [29]. However, about 30% of women develop de novo or acquire resistance to hormonal therapies progressing to a metastatic disease [30, 31].
Tam resistance has been associated with the expression levels of ER-α and ER-β [32, 33] especially to lower levels of ER-β [34]. The resistance toward Tam treatment has been also related with the expression of the AR [35]. However, ER-α-negative BCs have been have been benefitted from Tam in terms of recurrence, once Tam can bind directly to AR [36]. Park and collaborators demonstrated that that ER-α-positive and AR-positive BCs display a better prognosis compared to ER-α-negative and AR-positive BCs [37].
Natural product-derived compounds are being extensively explored as potential cancer treatments, specially to overcome resistance and side effects, and to prolong patient’s overall survival [38, 39]. Considering ER-positive BC, is desirable to develop new therapeutic agents that modulate ER expression achieving greater effectiveness, with less side effects impairing thrombosis and pulmonary embolism detected in 10 years-treated patients [40, 41].
Brazilian flora, especially the Amazon biome, is one of the richest global sources of native species with potentially bioactive compounds for the treatment of various diseases. The species Arrabidaea chica (Humb. & Bonpl.) B. Verlot, popularly known as “pariri” “crajiru” or “chica”, has been explored and its components (flavonoids, anthocyanins, tannins and phytosterols) isolated for the fight against fungi, bacteria, inflammatory processes, and tumors. The ability of A. chica extracts in reducing Ehrlich tumors without adverse effects has been previously describe [42]. However, the in vitro antitumor activity of A. chica extracts, especially in ER-positive BC, has not been described yet. Furthermore, its potential to induce cancer has not been evaluated.
The Epithelial Tumor test (ETT) has been used to detect epithelial tumor clones (Warts) in Drosophila melanogaster. This test evaluates the carcinogenic, anticarcinogenic, chemopreventive, and modulatory potential of different substances [38, 43, 44]. The test stands outs for its sensibility and reliability as a toxicological test and detects the loss of heterozygosity of the wts tumor suppressor gene, which leads to uncontrolled cell proliferation and the consequent formation of epithelial tumors [45]. The wts homologous gene in humans is the Large Tumor Suppressor Kinase 1 gene (LATS1) [46], and D. melanogaster shows considerable genetic homology with humans when compared to other mammalian models [47, 48] being used in important researchers related to treatment of tumors [49].
Here, we hypothesize that A. chica chloroform extract (CEAC) have selective effect across BC subtypes, modulating hormone receptors and cellular response to Tam treatment. To test this notion, we evaluated the cytotoxic potential of CEAC in four BC cell lines. In ER-positive strains, we compared how the treatment with CEAC alone or with Tam altered the viability, and hormone expression in MCF-7 and T-47D cells. Finally, we evaluated the antitumor potential of CEAC in in vivo model.
Methods
Chemicals
High purity chemicals and reagents were purchased from commercial sources, and all dilutions were prepared immediately before use. For in vitro assays, Dulbecco’s Modified Eagle Medium Nutrient Mixture F-12 (DMEM/F-12), Roswell Parki Memorial Institute (RPMI-1640), Leibovitz’s (L-15), fetal bovine serum (FBS), Epidermal Growth Factor (EGF), insulin and antibiotic gentamicin solution were purchased from (Gibco®). The 3-[4,5-dimethylthiazole-2—yl]2,5-diphenyltetrazolium bromide (MTT), CAS 57360-69-7, dimethylsufoxide (DMSO), CAS 67-68-5 and hydrocortisone were purchased from Sigma-Aldrich®. Tamoxifen Citrate (Sandoz) was gently donated by the Cancer Hospital from Federal University of Uberlandia.
For in vivo assays, Doxorubicin hydrochloride (DOX), commercial name Fauldoxo® (CAS 25316-40-9, batch 19B1091, Laboratório Industrial Brasileiro de Biologia e Síntese - Libbs, São Paulo – Brazil) was used as positive control at 0.4 mM. This concentration was based on previous studies that demonstrated the induction of epithelial tumors in D. melanogaster by DOX [44, 50,51,52,53]. Tween 80 (CAS 9005-65-6) at 1% (v/v) was used as negative control and for dilution of the compounds.
Plant material and preparation of A. chica extracts
Attending the Brazilian legislation (Law number 13.123 / 2015) this study was registered in the National System of Management of Genetic Heritage and Associated Traditional Knowledge under number A5573F8.
Leaves of A. chica were collected at the Faculty of Pharmacy’s Medicinal Herb Garden (UFJF), Juiz de Fora city, MG. The plant material was authenticated and stored at the Herbarium of the Botany Department of the Federal University of Juiz de Fora, MG, Brazil. The leaves (20 g) were dried at room temperature, powdered in a knife mill and firstly defatted, by maceration, using n-hexane. Based on previous studies that shown A. chica is rich in flavonoids and deoxyanthocyanidins [50], CHCl3 was chosen as solvent for extraction. Then, the powered material was extracted, by maceration, using CHCl3 as solvent. Following extraction, the solvent was filtered into a round bottom flask and removed under vacuum, at 40 °C, using a rotary evaporator to yield 2 g of the crude chloroform extract of A. chica, which was used in all assays.
Antioxidant activity
The free-radical scavenging activity was measured by the [2,2’-azinobis-(3-ethylbenzothiazoline-6-sulfonate)] (ABTS+) assay according with da Cruz et al. (2020) [54] with some modifications. The ABTS+ radical cation stock solution was prepared by mixing 7 mM ABTS+ with potassium persulfate (140mM), incubated at room temperature in the dark for 16 h. The ABTS+ was then diluted in ethanol until reached OD 0.700 ± 0.020 at 734nm. CEAC (125 μg/mL; 250 μg/mL; 500 μg/mL and 1000 μg/mL) was mixed with ABTS+ in 96-well plates. Absorbance was read at 415 nm using a microplate reader (Robonik®). Trolox was used as reference at concentrations ranging from 0.1 to 2 mM and the results were expressed as Trolox equivalents.
Cell culture
Four established breast cell lines were used throughout this study: (i) MCF 10A, non-tumorigenic, grown in DMEM/F-12 medium supplemented with 10 μg/mL of EGF, 0,25 μg/mL of Hydrocortisone and 10 μg/mL of insulin; (ii) MCF-7, ER-positive BC, maintained in RPMI-1640 medium; (iii) T-47D, ER-positive BC, also kept in RPMI-1640 medium supplemented with 10 μg/mL of insulin, and (iv) MDA-MB-231, triple-negative BC, cultured in L15 medium. The cell lines were obtained from American Type Culture Collection and confirmed to be free of mycoplasma contamination.
Tamoxifen-resistant MCF7 cells (MCF-7/TamR) were obtained after prolonged and continuous exposure of the MCF7 lineage to Tam (ranging from 0.1 μM to 1.0 μM) for a period of three months, as previously described [51,52,53,54].
All strains were supplemented with 10% of FBS, and 50 μg/mL of gentamycin, and kept in culture at 37° C in an atmosphere of 5% CO2 (Thermo Scientific™ Forma Series 3 Water Jacketed CO2 Incubator). For the cell line MDA-MB-231 the flasks were kept closed, free from CO2.The medium was changed on alternate days, until cell reached 80-90% confluence, when they were used in subsequent experiments.
Cell viability assay
The cell viability was evaluated by MTT reduction following previously instructions published by [55], with minor modifications. The four cell lines were cultured and, after confluence and trypsinization, 1x104 cells of each lineage were seeded in 96-well microplates with proper culture conditions for 24 h. Subsequently, cells were treated with 7 μg/mL, 15 μg/mL, 30 μg/mL, 62 μg/mL, 125 μg/mL, 250 μg/mL, 500 μg/mL and 1000 μg/mL of CEAC for 24 and 48 h. MTT solution (5mg/mL) was then added, incubated for 4 h, and the supernatant was carefully discarded. The insoluble formazan crystals produced by intracellular dehydrogenase was solubilized with DMSO, and the absorbance of each well was determined at 570 nm using Automatic Elisa Plate Reader (IndiaMART, DD Bioinfotech / Nathupura, New Delhi).
Each sample was measured in triplicate, and each experiment was repeated three times (n= 3). The mean OD of the treated cells was compared to the mean OD of the control wells (treated with vehicle only-DMSO) [55]. Wells with complete medium, without cells, were considered as blank. Cell viability was reported according to Formula (F1) = [(Absample-Absblank)/(AbsDMSO-Absblank)*100].
The half maximal inhibitory concentration (IC50) was calculated by non-linear regression from a dose-response curve between the compound concentration and percent growth inhibition [56], using the GraphPad Prism 6.0 software (GraphPad Software, San Diego, CA, USA). Selective indexes (SI) were also calculated using the Formula (F2) = SI = IC50-MCF 10A/IC50-BC cells. Values of SI ≥ 2.0 are considered significant [57].
The CEAC was selective to ER-positive BC cells. For this reason, the viability of T-47D and MCF-7 cells was further evaluated, as described above, after treatment, for 48 h, with CEAC at 1000 μg/mL; 1 μM and 2 μM of Tam [58, 59], alone. Cells were also treated with CEAC associated with Tam at 1 μM and 2 μM simultaneously or with one compound followed by the other. Finally, the viability of MCF-7/TamR cells was evaluated under the same conditions mentioned above.
qPCR analysis
Total RNA was isolated from MCF-7, T-47D and MCF-7/TamR cells treated with CEAC (1000 μg/ mL), Tam (1μM), and CEAC associated with Tam for 48 h, using Trizol® reagent (Invitrogen). The protocol was followed according to the supplier’ instructions. Cells treated with DMSO were included as control. q-PCR was carried out to evaluate the capacity of CEAC and Tam to modulate the transcriptional levels of ESR1, ESR2 and AR in ER-positive BC cell lines. The quality of extracted RNA was verified by electrophoresis on 1.5% agarose gel, stained with GelRed 1x (Uniscience), as well as by the reason of the spectrophotometric readings at 260 and 280 nm (Nanodrop 1000-ThermoFischer). First-strand cDNA was synthetized as previously described [60].
q-PCR was carried out on StepOnePlus Systems (Applied Biosystems), using 5.0 μM of specific primers designed for each gene as follows: ESR1 - F: CTAACTTGCTCTTGGACAGGAAC / R: GATTTGAGGCACACAAACTCCTC; ESR2 - F: GGGAATGGTGAAGTGTGGCT / R: TCATGTGTACCAACTCCTTGTCGG; AR: F: CATGTGGAAGCTGCAAGGTCT / R: GTGTAAGTTGCGGAAGCCAGG [38, 60]. Transcripts were quantified by ΔCq method after relative standard curve optimization with 5.0 μL of Power SYBR Green PCR Master Mix (Applied Biosystems, Carlsbad, CA, USA) and 2.0 μL cDNA. All data were normalized by β-2-microglobulin (β2M) gene (F: CCTGCCGTGTGAACCATGT / R: GCGGCATCTTCAAACCTCC) [60].
Epithelial Tumor Test (ETT)
Four concentrations of CEAC were defined (2.5, 5.0, 10.0 and 20.0 μg/μL) to be used in in vivo assay, and ETT was performed according to the methods proposed by Costa and contributors [61]. Heterozygotic larvae wts +/+ mwh were obtained from the cross between virgin females wts/TM3, Sb1 [45] with males mwh/mwh [61]. Third-instar larvae (72 ± 4 h) were submitted to a chronic treatment for about 48h. The D. melanogaster strains were kept under optimal laboratory conditions (25 ± 4 °C and 65% RH) in BOD-type chamber (Model: SL224, SOLAB – Equipamentos para Laboratórios, São Paulo, SP, Brazil).
At first, the toxicity test (TX) was carried out to assess the lethal concentration of CEAC for D. melanogaster. Larvae of third-instar (72 ± 4 h) were counted and placed in separate tubes containing 1.5 g of culture medium (mashed potatoes) [44, 62] for D. melanogaster with 5.0 mL of different concentrations of CEAC, alone (2.5, 5.0, 10.0 e 20.0 μg/μL) or in association with DOX (CEAC at 2.5, 5.0, 10.0 μg/μL, and DOX at 0.4 mM). The number of surviving flies per treatment were counted and provided an indicator of the toxicity of the compound [48].
Based on TX test, we performed ETT in post-treatment format [43, 48, 61]. The larvae were pre-treated with DOX at 0.4 mM to induce tumors and, after 6 h, the third stage larvae (72 ± 4 h) were washed and subjected to chronic treatment with CEAC at 2.5, 5.0, 10.0 μg/μL. Three controls were included: (i) negative control reverse osmosis water; (ii) solvent control with tween 80 1% (v/v) used to dilute CEAC; and (iii) positive control with DOX at 0.4mM. All experiments were conducted in quadruplicate.
Emerging adult flies from the different treatments were collected and kept in ethanol 70%. Only adult flies without the chromosome balancer TM3, Sb1 were analyzed, which can be differentiated phenotypically by the absence of truncated bristles [43, 45 48]. Tumors can be detected in all segments of the fly and D. melanogaster stands out for being an experimental model useful in genetic toxicology tests, as well as in studies of DNA repair processes.
Statistical analyses
Data were expressed as the mean ± standard deviation (SD) from three independent experiments. For the MTT assay, differences between the viability across cells lines were determined using one-way analysis of variance (ANOVA) and the Tukey HSD post hoc. Gene expression data were compared through Student’s independent t-test. Statistical comparisons of survival rates (TX) of D. melanogaster were performed using the Chi-squared (X2) test for ratios of independent samples. All the above results were analyzed using the GraphPad Prism 7.0 (GraphPad Software Inc., La Jolla, CA, EUA). Statistical significance was considered when p < 0.05.
The A. chica carcinogenic and/or anticarcinogenic potential, evaluated in ETT test, was determined by the Mann, Whitney and Wilcoxon nonparametric U test, with α=0.05 level of significance, using Prophet 5.0 (Phophet Software).
Results
Antioxidant potential and cytotoxicity
The antioxidant potential of CEAC was determined by the radical scavenging activity using the ABTS+ method and the results expressed as % of inhibition relative to Trolox as reference standard. The ABTS+ test showed radical scavenging activities in a dose dependent manner, and, in the highest concentration of CEAC (1000 μg/mL), the ABTS+ radicals were inhibited by 51.92%, showing the antioxidant potential of the extract (Fig. 1).
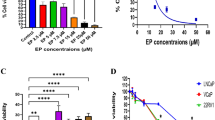
Subsequently, we evaluated the cytotoxic effect of CEAC on human breast cell lines including tumorigenic (T-47D, MCF-7, and MDA-MB-231) and non-tumorigenic (MCF 10A) lineages through MTT assay, performed for 24 (Fig. 2A) and 48 hours (Fig. 2B). The cellular behavior was similar in both treatments in which the viability of the MCF 10A lineage was maintained at around 57% for all tested concentrations. The cytotoxicity of CEAC was significantly higher for MCF-7 cells when compared to control (cells treated with DMSO, only) and to other cell lines, mainly in concentrations above 62 μg/mL. The IC50 of CEAC on MCF-7 cells was estimated at 8 μg/mL, with SI of 180.87.
Cytotoxic effects of chloroform extract of Arrabidaea chica (CEAC) on human luminal breast cancer cells T-47D, MCF-7. The non-tumorigenic cell line MCF 10A and the triple-negative breast cancer cell MDA-MB231 were included in this study. Cells treated with DMSO (diluent) were used as control. Treatments were performed on the four cell lines with different concentrations of CEAC for 24 (A) and 48 hours (B). Cell viability rates of luminal breast cancer cell lines were also recorded after treatment with CEAC and Tamoxifen (Tam) for 48 hours in T-47D (C) and MCF-7 (D) cell lines. Cells were treated with CEAC and Tam in isolation and combined. Data are presented as mean ± S. D of three independent experiments. Significance was calculated by one-way ANOVA, and Tukey’s post hoc test. # treatments with DMSO differed from all treatments with CEAC, p < 0.0001. a: treatment in MCF-7 differed from treatment in MCF 10A. b: treatment in MCF-7 differed from treatment in T-47D. (*p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001)
As the viability of the non-tumorigenic cell MCF 10A did not differ across treatments and CEAC was selective for luminal breast tumor cells, the concentration of 1000 μg /mL was used for further experiments in treatments for 48 hours in T-47D and MCF-7 cell lines, which express ER. Tam is widely used as ER antagonist, and it is the first line therapy for ER-positive BC. However, 40% of women receiving Tam develop resistance, which comprises treatment and patient’s survival [63]. Therefore, we compared the cellular effects of CEAC with Tam (1 μM and 2 μM) in isolated and combined treatments. All treatments differed from the control with diluent and the behavior of both cells was not different according to the Tam concentration. The effects were similar for 1 μM and 2 μM of Tam.
For the T-47D cell line (Fig. 2C), treatment with CEAC alone significantly reduced viability when compared to treatments with Tam alone. However, the cytotoxic effect was even greater when CEAC was combined with Tam. The viability of T-47D cells after treatment with CEAC was 53% and with CEAC + Tam (1 μM) was 34%. Tam also significantly decreases the viability of the MCF-7 cells (Fig. 2D). However, corroborating with our data, the cytotoxicity of CEAC for the MCF-7 was even more expressive and significantly higher when the extract was combined with Tam. Therefore, the viability of MCF-7 cells after treatment with CEAC was 7% and with CEAC+Tam (1 μM) was 4%The lowest concentration of Tam was then defined for further molecular assays.
Modulation of hormone receptors transcriptional levels
The expression of the ESR1, ESR2 and AR genes was quantified in T-47D and MCF-7 cell lines treated with CEAC (1000 μg /mL) and Tam (1μM), alone and with CEAC + Tam (combined treatment) for 48 hours (Fig. 3). As expected, MCF 10A and MDA-MB231 do not express hormone receptors (Fig. 3A-C).
Relative levels of hormone receptors transcripts after treatment with the chloroform extract of Arrabidaea chica (CEAC) and Tamoxifen (Tam). Gene expression levels were recorded without treatment in MCF 10A, T-47D, MCF-7 and MDA-MB231 cell lines (A, B, C). T-47D (D, E, F) and MCF-7 (G, H, I) cell lines were treated with 1000 μg /mL of CEAC, Tam (1 μM) and CEAC + Tam (1000 μg /mL, and 1 μM, respectively) for 48 h. The relative expression levels of the genes encoding for Estrogen Receptor alpha (ESR1), Estrogen Receptor beta (ESR2), and Androgen receptor (AR) were quantified by the comparative Cq method. * p <0,05, ** p <0,01, *** p <0,001 e **** p <0,0001
In the T-47D cells (Fig. 3D) the expression of ESR1 decreased by 5.6-fold (p <0.01) and 4.2-fold (p <0.001) after treatments with CEAC or Tam, respectively, when compared to control (cells treated with diluent). When CEAC was associated with Tam, the expression of ESR1 increased, and differed only from the treatment with the extract alone. Regarding the ESR2 gene (Fig. 3E), although slightly higher, its expression did not differ from the control in T-47D cells treated with CEAC. ESR1 levels decreased significantly when T-47D cells were treated with Tam alone (22.7-fold) and with CEAC + Tam (3.5-fold), compared to control. When treatment with CEAC was compared with Tam, ESR2 transcripts were 27.8-fold higher after treatment with CEAC. For both receptors, the combined treatments did not promote a significant difference in gene expression compared to treatment with Tam alone. Analysis of AR expression (Fig. 3F) revealed that the transcripts were differentially modulated between experiments, with higher AR transcriptional levels in the combined treatment of CEAC + Tam. Interestingly, CEAC + Tam treatment led to an increase in AR expression and a rescue of ESR1 expression that, accordingly to Park and collaborators, would represent a BC with better outcome. Moreover, when Tam was associated to CEAC, there was a partial rescue of ESR2 expression that, accordingly to the above researchers, could avoid the establishment of Tam resistance [37].
For the MCF-7 cells CEAC was responsible for promoting a decrease in ESR1 expression (alone or combined with Tam) (Fig. 3G), and an increase in ESR2 transcripts, which was 6.2-fold higher when compared to control (p <0.01), 105.6-fold higher when compared to treatment with Tam (p <0.01), and 99.4-fold higher when compared to CEAC + Tam treatment (p <0.001) (Fig. 3H). Finally, the AR transcripts were downregulated after treatment of MCF-7 with CEAC, upregulated after treatment with Tam alone and upregulated at higher levels with CEAC + Tam treatment (Fig. 3I).
As CEAC modulated the expression of ESR2 we tested the effect of the extract before or after treatment with Tam at 48 hours intervals (Fig. 4). Interestingly, the viability of the T-47D (Fig. 4A) and MCF-7 (Fig. 4B) cell lines was significantly compromised. Furthermore, the initial treatment with CEAC (1000 μg/mL) followed by Tam (1 μM) showed a greater reduction in viability. For T-47D cells the viability reached 14% and for the MCF-7 lineage 3%.
Cell viability rates of luminal breast cancer cell lines after alternate treatment with chloroform extract of Arrabidaea chica (CEAC) and Tamoxifen (Tam) for 48 hours. T-47D (A) and MCF-7 (B) cell lines were treated with CEAC followed by Tam (1μM) or with Tam (1μM) followed by CEAC (1000 μg/mL). Data are expressed as means ± SD, n = 3. Significance (*p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001) was calculated by one-way ANOVA, and Tukey’s post hoc test. # treatments with DMSO (control) differed from all treatments with CEAC, p < 0.0001
Cytotoxicity and modulation of hormone receptors in MCF-7/TamR
Treatment with CEAC alone reduced the viability of the MCF-7/TamR lineage by 90% (Fig. 5A), differing significantly from control and treatment with Tam. However, the profile of resistant cells treated with CEAC + Tam did not differ from the cytotoxic effect observed for the extract alone. As for hormone receptors (Fig. 5B), CEAC was responsible for decreasing the expression of ESR1 and AR in these cells and for increasing ESR2 gene transcripts, compared to the control. For CEAC + Tam treatments, only ESR2 transcripts were upregulated and Tam treatments did not differ from control.
Effect of chloroform extract of Arrabidaea chica (CEAC) and Tamoxifen (Tam) on tamoxifen-resistant MCF7 cells (MCF-7/TamR). Cell viability of MCF-7/TamR cells after treatment with CEAC (1000 μg/mL), Tam (1μM) or with CEAC + Tamfor 48 hours (A). Relative levels of hormone receptors transcripts after treatment with CEAC, Tam or CEAC + Tam. Gene expression was recorded through Cq method (B). MCF-7/TamR cell lines were also treated with CEAC followed by Tam (1μM) or with Tam (1μM) followed by CEAC (1000 μg/mL) and the viability evaluated by MTT (C). Data are expressed as means ± SD, n = 3. Significance (*p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001) was calculated by one-way ANOVA, and Tukey’s post hoc test. # treatments with DMSO differed from all treatments, p < 0.0001. ESR1: Estrogen Receptor alpha, ESR2: Estrogen Receptor beta (ESR2), and AR: Androgen receptor
We also investigated the effect of the extract before or after treatment with Tam at 48-hour intervals (Fig. 5C). The viability of the MCF-7/TamR lineage was significantly decreased under all conditions. However, previous treatment with CEAC (1000 μg/ml) followed by Tam (1 μM) promoted a significantly greater reduction in the viability of resistant cells.
Effect of CEAC on D. melanogaster
D. melanogaster has been used for more than 50 years as a model for human diseases related to alterations in replication, DNA repair, translation, drug metabolism and in toxicological research. Among the several advantages of using D. melanogaster stands out its genetic and metabolic similarity with humans and its ability to enzymatically activate promutagens and procarcinogens in vivo [48].
At first, CEAC toxicity was investigated to define the concentrations to be used in ETT assay. The percentage of surviving flies from treatment with tween 80 at 1% (negative control) and with DOX 0.4 mM (positive control) did not differ statistically from treatment with reverse osmosis water (negative control). Regarding treatment of CEAC (2.5, 5.0, 10 and 20 μg /μL) (Fig. 6A), the extract was not significantly toxic to D. melanogaster larvae when compared to the negative control and therefore was used in subsequent experiments.
In vivo assays performed with D. melanogaster treated with the chloroform extract of Arrabidaea chica (CEAC). Percentage of survival of D. melanogaster treated with CEAC (A). Treatments were conducted with CEAC (2.5, 5.0, 10.0 and 20.0 μg/μL). Flies, heterozygous for the Warts tumor suppressor gene, were further treated with different concentrations of CEAC (2.5, 5.0 and 10.0 μg/μL) and total tumors were recorded to demonstrate the carcinogenic (B) effect of CEAC. To demonstrate the anticarcinogenic effect of CEAC (C) flies were pre-treated with Doxorubicin (DOX 0.4 mM) and, subsequently, chronic treated for 48h with different concentrations of the extract. The frequency of tumors was analyzed in different segments, and significance was calculated by the Mann-Whitney Test. **Values considered significant when compared to the positive control (DOX 0.4 mM). *Values considered different from the negative control (P < 0.05). NC, negative control (osmosis reverse water). SC, solvent control (Tween 80 1%). PC, positive control (DOX 0.4mM). NC: Negative control (reverse osmosis water); SC: Solvent control (Tween 80 at 1%); PC: Positive control (DOX 0.4 mM)
CEAC at concentrations of 2.5, 5.0 and 10.0 μg/μL was then assessed by ETT (Fig. 6B-Table 1), and no statistically significant carcinogenic effect of the extract was identified when compared to the negative control. As expected, the solvent control (Tween 80 at 1%) did not differ statistically from the negative control (reverse osmosis water); and DOX 0.4 mM (positive control) generated significantly more tumors than the negative control. This concentration of DOX was based on previous studies that demonstrated the induction of epithelial tumors in D. melanogaster treated with DOX 0.4 mM [38, 43].
Finally, the anticarcinogenic potential of CEAC is represented in Fig. 6C. The individuals were pre-treated with DOX (0.4 mM) for a period of 6 hours and later treated with different concentrations of CEAC (2.5, 5.0 and 10.0 μg/μL). The findings for all three concentrations evaluated differed significantly from the positive control, with a significant reduction in the frequency of total number of tumors in CEAC-treated flies. The inhibition percentages of each concentration (2.5, 5.0 and 10.0 μg/μL) were 92%, 91.4% e 91.8%, respectively (Table 1).
The frequency of tumors was analyzed in different segments, and significance was calculated by the Mann-Whitney Test. aValues considered different from the negative control (p <0.05). ns Values considered not significant when compared to the negative control. bValues considered significant when compared to the positive control (DOX 0.4 mM). Frequency: number of tumors / fly
Discussion
The present study reveals CEAC as an estrogenic and androgenic modulator, potentially promising in the treatment of luminal BC and tamoxifen-resistant cells. Luminal breast tumors express ER and are responsive to endocrine therapy. Estrogen mediates breast cell growth [38, 55] and is associated with etiology of BC being an important target for ER antagonists, such as Tam [59]. However, despite the good prognosis, treatment for ER-positive breast tumors remains challenging, as therapeutic resistance has compromised patients’ survival [57, 58]. Hormonal status has been shown to be decisive in clinical outcome and understanding how different compounds alter the expression of receptors has been crucial for BC management.
Natural products are versatile and perform important antitumor activities, as they act in different pathways, blocking tumorigenesis and controlling the progression of transformed cells [32]. A. chica protective effects involve the reduction of ROS levels and lipid peroxidation supporting the antioxidant potential of CEAC identified in the present study using the ABTS+ method. In addition, this species increases of collagen content during the healing process, with analgesic properties through the inhibition of cyclooxygenases [33, 64,65,66,67] also demonstrated that the plant extract alone, or associated with vincristine, decreased serum transaminases levels, oxidative stress, and hematological toxicity. Our work is pioneer in demonstrating the role of A. chica in the modulation of hormone receptors.
In in vitro assays with breast cell lines, CEAC substantially inhibited the viability of MCF-7 cells, with SI of 180.87. As MCF-7 cells are ER-positive, the results raised the question about the extract's ability to modulate hormone receptors. The ER response is the result of a balance between the signaling pathways of two divergent isoforms ER-α and ER-β [68]. ER-α expression is associated with the development, growth and metastasis of BC [69], and ER-β has been described as tumor suppressor. In addition, ER-β expression independently predicts better disease-free survival in patients treated with Tam [70]. In the present study, ESR1 transcriptional levels were downregulated after treatment of MCF-7 cells with CEAC, and ESR2 gene expression was upregulated. This behavior was also observed in treatments performed in tamoxifen-resistant cells. Therefore, the observed cytotoxicity can be related to the extract's ability to modulate ERs, which led us to the hypothesis about the possibility of the compound being combined with Tam in the treatment of luminal BC cell lines.
When CEAC was combined with Tam, the treatment was slightly more cytotoxic to the T-47D and MCF-7 strains. However, for ERs, there was no difference in the expression of these genes compared to treatments with Tam alone. For AR, also evaluated in the present study, the modulatory effects were more evident, and similar between the T-47D and MCF-7 with lower mRNA levels when cells were treated with CEAC and higher levels when treated with CEAC + Tam. AR stimulates cell proliferation, promotes metastasis and favors resistance to endocrine therapy [71,72,73]. Previous studies indicated that one third of all patients develop resistance to Tam, even though ER-α positivity remains unchanged [74, 75]. In addition, in vitro experiments confirmed a low expression of ER-β in tumors resistant to Tam [53]. Our results demonstrated decreased expression of ESR2 when cells were treated with Tam alone. In the treatment with CEAC + Tam, this profile was maintained in MCF-7 and a partial rescue of ESR2 was obtained in T47-D cells. This partial rescue could indicate a possible effect of CEAC in diminishing the development of Tam resistance in T47D cells. Moreover, Tam + CEAC treatment leads to the maintenance of ERS1 and AR levels which, accordingly to Park and collaborators, would represent a BC with better outcome [37]. Interestingly, the effect of Tam on AR expression was different in MCF-7 cells compared to T47D cells. In T47 D cells, Tam decreased AR expression while in MCF7 cells there was an increase in AR expression. Since T47D are considered a more Tam resistant cell line compared to MCF-7 cells [76], this effect on AR expression could be responsible for the different Tam sensitivity. On the other hand, treatment with CEAC alone achieves one of the main objectives of endocrine therapy by increasing the expression of ESR2 and decreasing that of ESR1 and AR in MCF-7 cells and in MCF-7/TamR.
In this context, enhanced ER-β signaling can modulate ER-α and AR signaling without complete ablation of hormones [77,78,79,80,81,82]. We suggest that the different effects between isolated and combined treatments may result from competition and / or antagonisms between CEAC and Tam, which needs to be further investigated. We therefore suggest the treatment with CEAC as complementary to Tam, once, the expression and ER-β can sensitize cells to Tam [83,84,85,86]. This effect was proven for T-47D cells and MCF-7/TamR. The initial treatment with CEAC and then with Tam substantially reduced the viability of T-47D cells to 14% and to 11% in MCF-7/TamR. This behavior may be associated with CEAC's ability to modulate ESR2 [87,88,89]. However, further studies are needed to define the therapeutic design and to evaluate the inclusion of CEAC in the treatment of women resistant to Tam. Finally, our results demonstrated a different response profile between the two cell lines of luminal BC. Therefore, we suggest a deeper study of the molecular characterization of luminal breast tumors, as these subtypes may require different therapeutic regimens, which may be limiting for the prognosis of patients.
Regarding the in vivo assays, CEAC (2.5, 5.0, 10.0 and 20.0 μg/μL) did not show significant toxicity for D. melanogaster, validating the safety of these concentrations. In the ETT assay, CEAC did not demonstrate carcinogenic effect at the three concentrations tested (2.5, 5.0 and 10.0 μg/μL). Previous studies have reported that aqueous, butanolic and chloroform extracts of A. chica did not cause mutagenic effect in strains of Salmonella. Even with metabolic activation, the chloroform extract did not show mutagenic effect suggesting the absence of phytochemicals capable of inducing frameshift mutation [43, 62, 90, 91]. Although mutagenicity is an inherent factor in carcinogenicity, both mutagens and non-mutagens compounds can generate transformed cells inducing different cancer hallmarks, including cellular proliferation [43, 62, 92]. Thus, the absence of a mutagenic effect corroborates and reinforces our results on the absence of CEAC carcinogenic potential, supporting the safety of the compound.
Table 1 shows the post treatment model, in which the tumor was induced with DOX (0.4mM) so that the larvae were subjected to chronic treatment with different concentrations of CEAC (2.5, 5.0 and 10.0 μg/μL). The wts gene is maintained in heterozygosity in stock of D. melanogaster in the presence of a chromosomal balancer (TM3). The loss of heterozygosity in the cells of the larval imaginal disc leads to the proliferation of cell clones as tumors in adults [43, 93]. DOX at 0.4 mM has a carcinogenic effect on somatic cells of D. melanogaster [44, 48, 94], which was reversed with CEAC treatment, showing its ability to reduce epithelial tumors. In this context, we suggest that CEAC increases the antioxidant potential of D. melanogaster cells, helping to reduce the damage caused by metabolites generated by DOX, which mimics the genomic damage that cause tumors. The synchronism between DNA replication, with the repair of damage, and the progression of the cell cycle ensure the integrity of the genome avoiding mutations and rearrangements in the DNA [95, 96]. Chromosomal mutations or aberrations affect oncogenes and tumor suppressor genes leading to the malignant transformation [48, 97]. Thus, genomic instability is associated with serious pathological disorders such as cancer [44, 48, 98,99,100,101]. In addition, CEAC induces apoptosis of damaged cells during the embryonic development of the larvae, with consequent reduction of tumors in adults. Therefore, we also suggest that, in the post-treatment, the anticarcinogenic effect of CEAC is due to the increased activity of proteins involved in repair pathways related to the tumor suppressor gene Warts, which promoted the control of cell proliferation and reduction of the formation of epithelial tumors. Importantly, we use the ETT test that assesses the toxicity, mutagenicity and carcinogenicity of different compounds [98, 102,103,104,105], based on phenotypic effects. However, it has been shown that aqueous and ethanolic extracts of A. chica inhibit inflammatory and angiogenic processes [89, 106, 107] and that its ethanolic extract also reduces the lipid oxidative stress marker malondialdehyde [67, 108]. In the present work we also suggest its role in the modulation of hormone receptors.
Conclusion
Our study confirmed the antioxidant activity of CEAC, emphasizing its important role in carcinogenesis. The bioassays on breast tumor cells demonstrated the antiproliferative activity of the extract, being selective to the BC luminal cells. CEAC modulated the expression of ESR1, ESR2 and AR. In in vivo tests, CEAC was not toxic to D. melanogaster, demonstrated anticarcinogenic action, and controlled tumor formation in DOX-treated flies.
As far as we are aware, this is the first study of the hormone modulatory effect of CEAC on BC cells and the anticarcinogenicity effect of CEAC. It will be important to confirm our results in other animal models, as well as further experiments that seek to discover additional mechanisms of this extract in BC.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AR:
-
Androgen receptor
- BC:
-
Breast cancer
- CEAC:
-
Chloroform extract Arrabidaea chica
- DOX:
-
Doxorubicin
- ER:
-
Estrogen receptor
- ESR1:
-
Estrogen receptor alpha
- ESR2:
-
Estrogen receptor beta
- ETT:
-
Epithelial tumor test
- Her2:
-
Human epidermal receptor
- NR:
-
Nuclear receptor
- PgR:
-
Progesterone receptor
- ROS:
-
Reactive oxygen species
- SERM:
-
Selective estrogen receptor modulators
- Tam:
-
Tamoxifen
- TX:
-
Toxicity test
- wts:
-
Tumor suppressor gene
References
Mokbel K, Mokbel K. Chemoprevention of Breast Cancer With Vitamins and Micronutrients: A Concise Review. In vivo (Athens, Greece). 2019;33(4):983–97.
Azamjah N, Soltan-Zadeh Y, Zayeri F. Global Trend of Breast Cancer Mortality Rate: A 25-Year Study. APJCP. 2019;20(7):2015–20.
Coughlin SS, Ekwueme DU. Breast cancer as a global health concern. Cancer Epidemiol. 2009;33(5):315–8.
WHO: Breast cancer: prevention and control. In.; 2018.
Organization WH. Diet, nutrition, and the prevention of chronic diseases: report of a joint WHO/FAO expert consultation, vol. 916: World Health Organization; 2003. http://apps.who.int/iris/bitstream/handle/10665/42665/WHO_TRS_916.pdf;jsessionid=C3A75C0BA1D09CE701CD5F60D8A0641B?sequence=1.
Mathur P, Sathishkumar K, Chaturvedi M, Das P, Sudarshan KL, Santhappan S, et al. Cancer statistics, 2020: report from national cancer registry programme, India. JCO Global Oncology. 2020;6:1063–75.
Basch EM, Thaler HT, Shi W, Yakren S, Schrag D. Use of information resources by patients with cancer and their companions. Cancer. 2004;100(11):2476–83.
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424.
Lee CI, Goodwin A, Wilcken N. Fulvestrant for hormone-sensitive metastatic breast cancer. Cochrane Database Syst Rev. 2017;1(1):Cd011093.
Gompel A. Hormone and breast cancer. Presse Medicale (Paris, France: 1983). 2019;48(10):1085–91.
Gerratana L, Basile D, Buono G, De Placido S, Giuliano M, Minichillo S, et al. Androgen receptor in triple negative breast cancer: A potential target for the targetless subtype. Cancer Treat Rev. 2018;68:102–10.
Rangel N, Fortunati N, Osella-Abate S, Annaratone L, Isella C, Catalano MG, et al. FOXA1 and AR in invasive breast cancer: new findings on their co-expression and impact on prognosis in ER-positive patients. BMC Cancer. 2018;18(1):703.
Gruvberger-Saal SK, Bendahl PO, Saal LH, Laakso M, Hegardt C, Edén P, et al. Estrogen receptor beta expression is associated with tamoxifen response in ERalpha-negative breast carcinoma. Clin Cancer Res. 2007;13(7):1987–94.
Heldring N, Pike A, Andersson S, Matthews J, Cheng G, Hartman J, et al. Estrogen receptors: how do they signal and what are their targets. Physiol Rev. 2007;87(3):905–31.
Feng J, Li L, Zhang N, Liu J, Zhang L, Gao H, et al. Androgen and AR contribute to breast cancer development and metastasis: an insight of mechanisms. Oncogene. 2017;36(20):2775–90.
Lamb CA, Vanzulli SI, Lanari C. Hormone receptors in breast cancer: more than estrogen receptors. Medicina. 2019;79(Spec 6/1):540–5.
Chun KH, Park JH, Fan S. Predicting and Overcoming Chemotherapeutic Resistance in Breast Cancer. Adv Exp Med Biol. 2017;1026:59–104.
Marotti JD, de Abreu FB, Wells WA, Tsongalis GJ. Triple-Negative Breast Cancer: Next-Generation Sequencing for Target Identification. Am J Pathol. 2017;187(10):2133–8.
Gadi VK, Davidson NE. Practical Approach to Triple-Negative Breast Cancer. J Oncol Pract. 2017;13(5):293–300.
Kunc M, Biernat W, Senkus-Konefka E. Estrogen receptor-negative progesterone receptor-positive breast cancer - "Nobody's land" or just an artifact? Cancer Treat Rev. 2018;67:78–87.
Bak MJ, Furmanski P, Shan NL, Lee HJ, Bao C, Lin Y, et al. Tocopherols inhibit estrogen-induced cancer stemness and OCT4 signaling in breast cancer. Carcinogenesis. 2018;39(8):1045–55.
Kensler KH, Regan MM, Heng YJ, Baker GM, Pyle ME, Schnitt SJ, et al. Prognostic and predictive value of androgen receptor expression in postmenopausal women with estrogen receptor-positive breast cancer: results from the Breast International Group Trial 1-98. Breast Cancer Res. 2019;21(1):30.
Shi Q, Li Y, Li S, Jin L, Lai H, Wu Y, et al. LncRNA DILA1 inhibits Cyclin D1 degradation and contributes to tamoxifen resistance in breast cancer. Nat Commun. 2020;11(1):5513.
Wibowo E, Pollock PA, Hollis N, Wassersug RJ. Tamoxifen in men: a review of adverse events. Andrology. 2016;4(5):776–88.
Cronin-Fenton DP, Damkier P. Tamoxifen and CYP2D6: A Controversy in Pharmacogenetics. Adv Pharmacol (San Diego, Calif). 2018;83:65–91.
Sanchez-Spitman AB, Swen JJ, Dezentje VO, Moes D, Gelderblom H, Guchelaar HJ: Clinical pharmacokinetics and pharmacogenetics of tamoxifen and endoxifen. Expert Rev Clin Pharmacol 2019, 12(6):523-536.
Khosrow-Khavar F, Filion KB, Al-Qurashi S, Torabi N, Bouganim N, Suissa S, et al. Cardiotoxicity of aromatase inhibitors and tamoxifen in postmenopausal women with breast cancer: a systematic review and meta-analysis of randomized controlled trials. Ann Oncol. 2017;28(3):487–96.
Merikhian P, Ghadirian R, Farahmand L, Mansouri S, Majidzadeh AK. MUC1 induces tamoxifen resistance in estrogen receptor-positive breast cancer. Expert Rev Anticancer Ther. 2017;17(7):607–13.
Pan H, Gray R, Braybrooke J, Davies C, Taylor C, McGale P, et al. 20-Year Risks of Breast-Cancer Recurrence after Stopping Endocrine Therapy at 5 Years. N Engl J Med. 2017;377(19):1836–46.
Turner NC, Slamon DJ, Ro J, Bondarenko I, Im SA, Masuda N, et al. Overall Survival with Palbociclib and Fulvestrant in Advanced Breast Cancer. N Engl J Med. 2018;379(20):1926–36.
Cristofanilli M, Turner NC, Bondarenko I, Ro J, Im SA, Masuda N, et al. Fulvestrant plus palbociclib versus fulvestrant plus placebo for treatment of hormone-receptor-positive, HER2-negative metastatic breast cancer that progressed on previous endocrine therapy (PALOMA-3): final analysis of the multicentre, double-blind, phase 3 randomised controlled trial. Lancet Oncol. 2016;17(4):425–39.
Kim C, Kim B. Anti-Cancer Natural Products and Their Bioactive Compounds Inducing ER Stress-Mediated Apoptosis: A Review. Nutrients. 2018;10(8):1021.
Jiang P, Han B, Jiang L, Li Y, Yu Y, Xu H, et al. Simultaneous separation and quantitation of three phytosterols from the sweet potato, and determination of their anti-breast cancer activity. J Pharm Biomed Anal. 2019;174:718–27.
Pancholi S, Lykkesfeldt AE, Hilmi C, Banerjee S, Leary A, Drury S, et al. ERBB2 influences the subcellular localization of the estrogen receptor in tamoxifen-resistant MCF-7 cells leading to the activation of AKT and RPS6KA2. Endocr Relat Cancer. 2008;15(4):985–1002.
De Amicis F, Thirugnansampanthan J, Cui Y, Selever J, Beyer A, Parra I, et al. Androgen receptor overexpression induces tamoxifen resistance in human breast cancer cells. Breast Cancer Res Treat. 2010;121(1):1–11.
Hilborn E, Gacic J, Fornander T, Nordenskjöld B, Stål O, Jansson A. Androgen receptor expression predicts beneficial tamoxifen response in oestrogen receptor-α-negative breast cancer. Br J Cancer. 2016;114(3):248–55.
Park JH, Yoon SM, Yu CS, Kim JH, Kim TW, Kim JC. Randomized phase 3 trial comparing preoperative and postoperative chemoradiotherapy with capecitabine for locally advanced rectal cancer. Cancer. 2011;117(16):3703–12.
Braga DL, Mota STS, Zóia MAP, Lima P, Orsolin PC, Vecchi L, Nepomuceno JC, Fürstenau CR, Maia YCP, Goulart LR et al: Ethanolic Extracts from Azadirachta indica Leaves Modulate Transcriptional Levels of Hormone Receptor Variant in Breast Cancer Cell Lines. International Journal of Molecular Sciences 2018, 19(7).
Alves-Fernandes DK, Oliveira ÉA, Faião-Flores F, Alicea-Rebecca G, Weeraratna AT, Smalley KSM, et al. ER stress promotes antitumor effects in BRAFi/MEKi resistant human melanoma induced by natural compound 4-nerolidylcathecol (4-NC). Pharmacol Res. 2019;141:63–72.
Khamis AAA, Ali EMM, El-Moneim MAA, Abd-Alhaseeb MM, El-Magd MA, Salim EI. Hesperidin, piperine and bee venom synergistically potentiate the anticancer effect of tamoxifen against breast cancer cells. Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. 2018;105:1335–43.
Davies C, Pan H, Godwin J, Gray R, Arriagada R, Raina V, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet (London, England). 2013;381(9869):805–16.
Ribeiro AFC, Telles TC, Ferraz VP, Souza-Fagundes EM, Cassali GD, Carvalho AT, et al. Effect of Arrabidaea chica extracts on the Ehrlich solid tumor development. Rev Bras Farm. 2012;22(2):364–73.
Nepomuceno JC. Using the Drosophila melanogaster to assessment carcinogenic agents through the test for detection of epithelial tumor clones (Warts). Adv Tech Biol Med. 2015;3(3):2–8.
Vasconcelos MA, Orsolin PC, Oliveira VC, Lima PMAP, Naves MPC, de Morais CR, et al. Modulating effect of vitamin D3 on the mutagenicity and carcinogenicity of doxorubicin in Drosophila melanogaster and in silico studies. Food Chem Toxicol. 2020;143:111549.
Eeken JC, Klink I, van Veen BL, Pastink A, Ferro W. Induction of epithelial tumors in Drosophila melanogaster heterozygous for the tumor suppressor gene wts. Environ Mol Mutagen. 2002;40(4):277–82.
Oliveira VC, Constante SAR, Orsolin PC, Nepomuceno JC, de Rezende AAA, Spanó MA. Modulatory effects of metformin on mutagenicity and epithelial tumor incidence in doxorubicin-treated Drosophila melanogaster. Food Chem Toxicol. 2017;106:283–91.
Nishiyama Y, Hirota T, Morisaki T, Hara T, Marumoto T. Iida S-i, Makino K, Yamamoto H, Hiraoka T, Kitamura N: A human homolog of Drosophila warts tumor suppressor, h-warts, localized to mitotic apparatus and specifically phosphorylated during mitosis. FEBS Lett. 1999;459(2):159–65.
Orsolin P, Silva-Oliveira R, Nepomuceno J. Modulating effect of simvastatin on the DNA damage induced by doxorubicin in somatic cells of Drosophila melanogaster. Food Chem Toxicol. 2016;90:10–7.
Villegas SN. One hundred years of Drosophila cancer research: no longer in solitude. Dis Model Mech. 2019;12(4):dmm039032.
Silva-Silva JV, Moragas-Tellis CJ, Chagas MSS, Souza PRV, Souza CSF, Hardoim DJ, Taniwaki NN, Moreira DL, Dutra Behrens M, Calabrese KS. Antileishmanial Activity of Flavones-Rich Fraction From Arrabidaea chica Verlot (Bignoniaceae). Front Pharmacol 2021, 12:1843.
Das CK, Parekh A, Parida PK, Bhutia SK, Mandal M. Lactate dehydrogenase A regulates autophagy and tamoxifen resistance in breast cancer. Biochimica et biophysica acta Molecular cell research. 2019;1866(6):1004–18.
Zhou Q, Zeng H, Ye P, Shi Y, Guo J, Long X. Differential microRNA profiles between fulvestrant-resistant and tamoxifen-resistant human breast cancer cells. Anticancer Drugs. 2018;29(6):539–48.
Lee MH, Koh D, Na H, Ka NL, Kim S, Kim HJ, et al. MTA1 is a novel regulator of autophagy that induces tamoxifen resistance in breast cancer cells. Autophagy. 2018;14(5):812–24.
Barkovskaya A, Seip K, Prasmickaite L, Mills IG, Moestue SA, Itkonen HM. Inhibition of O-GlcNAc transferase activates tumor-suppressor gene expression in tamoxifen-resistant breast cancer cells. Sci Rep. 2020;10(1):16992.
Gerlier D, Thomasset N. Use of MTT colorimetric assay to measure cell activation. J Immunol Methods. 1986;94(1-2):57–63.
Vichai V, Kirtikara K. Sulforhodamine B colorimetric assay for cytotoxicity screening. Nat Protoc. 2006;1(3):1112–6.
Dashek WV. Methods in plant biochemistry and molecular biology: CRC Press; 2018. https://www.taylorfrancis.com/books/mono/10.1201/9781351074483/methods-plant-biochemistry-molecular-biology-william-dashek, https://doi.org/10.1201/9781351074483.
Post AE, Smid M, Nagelkerke A, Martens JW, Bussink J, Sweep FC, et al. Interferon-stimulated genes are involved in cross-resistance to radiotherapy in tamoxifen-resistant breast cancer. Clin Cancer Res. 2018;24(14):3397–408.
Lillo MA, Nichols C, Perry C, Runke S, Krutilina R, Seagroves TN, et al. Methylparaben stimulates tumor initiating cells in ER+ breast cancer models. J Appl Toxicol. 2017;37(4):417–25.
Araujo TG, Marangoni K, Rocha RM, Maia YC, Araujo GR, Alcântar TM, et al. Dynamic dialog between cytokeratin 18 and annexin A1 in breast cancer: a transcriptional disequilibrium. Acta Histochem. 2014;116(7):1178–84.
Costa W, Oliveira A, Nepomuceno J. Lapachol as an epithelial tumor inhibitor agent in Drosophila melanogaster heterozygote for tumor suppressor gene wts. Genet Mol Res. 2011;10(4):3236–45.
Spanó MA, Frei H, Würgler FE, Graf U. Recombinagenic activity of four compounds in the standard and high bioactivation crosses of Drosophila melanogaster in the wing spot test. Mutagenesis. 2001;16(5):385–94.
Hultsch S, Kankainen M, Paavolainen L, Kovanen R-M, Ikonen E, Kangaspeska S, et al. Association of tamoxifen resistance and lipid reprogramming in breast cancer. BMC Cancer. 2018;18(1):850.
Peña E, Roa FJ, Inostroza E, Sotomayor K, González M, Gutierrez-Castro FA, et al. Increased expression of mitochondrial sodium-coupled ascorbic acid transporter-2 (mitSVCT2) as a central feature in breast cancer. Free Radic Biol Med. 2019;135:283–92.
Vasconcelos CC, Lopes AJO, Sousa ELF, Camelo DS, Lima FCVM. Rocha CQd, Silva GEB, Garcia JBS, Cartágenes MdSdS: Effects of extract of arrabidaea chica verlot on an experimental model of osteoarthritis. Int J Mol Sci. 2019;20(19):4717.
Miranda N, Gerola AP, Novello CR, Ueda-Nakamura T, de Oliveira SS, Dias-Filho BP, et al. Pheophorbide a, a compound isolated from the leaves of Arrabidaea chica, induces photodynamic inactivation of Trypanosoma cruzi. Photodiagnosis Photodyn Ther. 2017;19:256–65.
Vasconcelos CC, Lopes AJO, Sousa ELF, Camelo DS, Lima F, Rocha CQD, et al. Effects of Extract of Arrabidaea chica Verlot on an Experimental Model of Osteoarthritis. Int J Mol Sci. 2019;20(19).
Nayar U, Cohen O, Kapstad C, Cuoco MS, Waks AG, Wander SA, et al. Acquired HER2 mutations in ER+ metastatic breast cancer confer resistance to estrogen receptor–directed therapies. Nat Genet. 2019;51(2):207–16.
Flaherty RL, Intabli H, Falcinelli M, Bucca G, Hesketh A, Patel BA, et al. Stress hormone-mediated acceleration of breast cancer metastasis is halted by inhibition of nitric oxide synthase. Cancer Lett. 2019;459:59–71.
Fernö M, Baldetorp B, Bendahl P-O, Borg Å, Ewers S-B, Olsson H, et al. Recurrence-free survival in breast cancer improved by adjuvant tamoxifen-especially for progesterone receptor positive tumors with a high proliferation. Breast Cancer Res Treat. 1995;36(1):23–34.
Wu Y, Zhang Z, Cenciarini ME, Proietti CJ, Amasino M, Hong T, et al. Tamoxifen resistance in breast cancer is regulated by the EZH2–ERα–GREB1 transcriptional axis. Cancer Res. 2018;78(3):671–84.
Ye L, Lin C, Wang X, Li Q, Li Y, Wang M, et al. Epigenetic silencing of SALL 2 confers tamoxifen resistance in breast cancer. EMBO Mol Med. 2019;11(12):e10638.
Neven P, Jongen L, Lintermans A, Van Asten K, Blomme C, Lambrechts D, et al. Tamoxifen metabolism and efficacy in breast cancer: a prospective multicenter trial. Clin Cancer Res. 2018;24(10):2312–8.
De Santo I, McCartney A, Migliaccio I, Di Leo A, Malorni L. The emerging role of ESR1 mutations in luminal breast cancer as a prognostic and predictive biomarker of response to endocrine therapy. Cancers. 2019;11(12):1894.
Schairer C, Lubin J, Troisi R, Sturgeon S, Brinton L, Hoover R. Menopausal estrogen and estrogen-progestin replacement therapy and breast cancer risk. JAMA. 2000;283(4):485–91.
Karey KP, Sirbasku DA. Differential responsiveness of human breast cancer cell lines MCF-7 and T47D to growth factors and 17 beta-estradiol. Cancer Res. 1988;48(14):4083–92.
Kono M, Fujii T, Lim B, Karuturi MS, Tripathy D, Ueno NT. Androgen receptor function and androgen receptor–targeted therapies in breast cancer: a review. JAMA Oncol. 2017;3(9):1266–73.
Giovannelli P, Di Donato M, Galasso G, Di Zazzo E, Bilancio A, Migliaccio A. The androgen receptor in breast cancer. Front Endocrinol. 2018;9:492.
Cochrane DR, Bernales S, Jacobsen BM, Cittelly DM, Howe EN, D’Amato NC, et al. Role of the androgen receptor in breast cancer and preclinical analysis of enzalutamide. Breast Cancer Res. 2014;16(1):1–19.
Niemeier LA, Dabbs DJ, Beriwal S, Striebel JM, Bhargava R. Androgen receptor in breast cancer: expression in estrogen receptor-positive tumors and in estrogen receptor-negative tumors with apocrine differentiation. Mod Pathol. 2010;23(2):205–12.
Sommer S, Fuqua SA. Estrogen receptor and breast cancer. In: Seminars in cancer biology: 2001: Elsevier; 2001. p. 339–52.
Yager JD, Davidson NE. Estrogen carcinogenesis in breast cancer. N Engl J Med. 2006;354(3):270–82.
Maguire P, Margolin S, Skoglund J, Sun X-F, Gustafsson J-Å, Børresen-Dale A-L, et al. Estrogen receptor beta (ESR2) polymorphisms in familial and sporadic breast cancer. Breast Cancer Res Treat. 2005;94(2):145–52.
Yu K-D, Rao N-Y, Chen A-X, Fan L, Yang C, Shao Z-M. A systematic review of the relationship between polymorphic sites in the estrogen receptor-beta (ESR2) gene and breast cancer risk. Breast Cancer Res Treat. 2011;126(1):37–45. https://pubmed.ncbi.nlm.nih.gov/20390341/, https://doi.org/10.1007/s10549-010-0891-2.
Ghali RM, Al-Mutawa MA, Al-Ansari AK, Zaied S, Bhiri H, Mahjoub T, et al. Differential association of ESR1 and ESR2 gene variants with the risk of breast cancer and associated features: A case-control study. Gene. 2018;651:194–9.
Treeck O, Elemenler E, Kriener C, Horn F, Springwald A, Hartmann A, et al. Polymorphisms in the promoter region of ESR2 gene and breast cancer susceptibility. J Steroid Biochem Mol Biol. 2009;114(3-5):207–11.
Al-Eitan LN, Rababa’h DM, Alghamdi MA, Khasawneh RH: Association between ESR1, ESR2, HER2, UGT1A4, and UGT2B7 polymorphisms and breast Cancer in Jordan: a case-control study. BMC Cancer 2019, 19(1):1-10.
Zheng Y, Huo D, Zhang J, Yoshimatsu TF, Niu Q, Olopade OI. Microsatellites in the estrogen receptor (ESR1, ESR2) and androgen receptor (AR) genes and breast cancer risk in African American and Nigerian women. PLoS One. 2012;7(7):e40494.
Michel AFRM, Melo MM, Campos PP, Oliveira MS, Oliveira FAS, Cassali GD, et al. Evaluation of anti-inflammatory, antiangiogenic and antiproliferative activities of Arrabidaea chica crude extracts. J Ethnopharmacol. 2015;165:29–38.
dos Santos VC, Longo TB, Garcia ALH, Richter MF, Guecheva TN, Henriques JAP. Ferraz AdBF, Picada JN: Evaluation of the mutagenicity and genotoxicity of Arrabidaea chica Verlot (Bignoneaceae), an Amazon plant with medicinal properties. J Toxicol Environ Health A. 2013;76(6):381–90.
Gemelli TF. Prado LdS, Santos FS, de Souza AP, Guecheva TN, Henriques JAP, Ferraz AdBF, Corrêa DS, Dihl RR, Picada JN: Evaluation of safety of Arrabidaea chica verlot (Bignoniaceae), a plant with healing properties. J Toxicol Environ Health A. 2015;78(18):1170–80.
Benigni R, Bossa C. Structure alerts for carcinogenicity, and the Salmonella assay system: a novel insight through the chemical relational databases technology. Mutation Res/Rev Mutation Res. 2008;659(3):248–61.
Berry C, Brusick D, Cohen SM, Hardisty JF, Grotz VL, Williams GM. Sucralose non-carcinogenicity: a review of the scientific and regulatory rationale. Nutr Cancer. 2016.
Benjanuwattra J, Siri-Angkul N, Chattipakorn SC, Chattipakorn N. Doxorubicin and its proarrhythmic effects: A comprehensive review of the evidence from experimental and clinical studies. Pharmacol Res. 2020;151:104542.
Broustas CG, Lieberman HB. DNA damage response genes and the development of cancer metastasis. Radiat Res. 2014;181(2):111–30.
Tacar O, Sriamornsak P, Dass CR. Doxorubicin: an update on anticancer molecular action, toxicity and novel drug delivery systems. J Pharm Pharmacol. 2013;65(2):157–70.
Sidorov R, Ugnivenko E, Khovanova E, Belitsky G. Induction of tumor clones in D. melanogaster wts/+ heterozygotes with chemical carcinogens. Mutation Research/Genetic Toxicology and Environmental. Mutagenesis. 2001;498(1-2):181–91.
Teixeira da Silva T, Braga Martins J, Socorro D, de Brito LM, de Almeida PM, Silva Sá JL, et al. Modulating effect of DL-kavain on the mutagenicity and carcinogenicity induced by doxorubicin in Drosophila melanogaster. J Toxicol Environ Health A. 2021;84(19):769–82.
Graf U, Abraham SK, Guzmán-Rincón J, Würgler FE. Antigenotoxicity studies in Drosophila melanogaster. Mutation Research/Fundamental and Molecular Mechanisms of Mutagenesis. 1998;402(1-2):203–9.
Graf U, Würgler F, Katz A, Frei H, Juon H, Hall C, et al. Somatic mutation and recombination test in Drosophila melanogaster. Environ Mutagen. 1984;6(2):153–88.
de Morais CR, Bonetti AM, Mota AA, Campos CF, Souto HN, Naves MPC, et al. Evaluation of toxicity, mutagenicity and carcinogenicity of samples from domestic and industrial sewage. Chemosphere. 2018;201:342–50.
Naves MPC, de Morais CR, Spanó MA, de Rezende AAA. Mutagenicity and recombinogenicity evaluation of bupropion hydrochloride and trazodone hydrochloride in somatic cells of Drosophila melanogaster. Food Chem Toxicol. 2019;131:110557.
Hernando J, Alvarez L, Ferreiro JA, Sancho I, Comendador MA, Sierra LM. Female germ cell mutagenicity of model chemicals in Drosophila melanogaster: mechanistic information and analysis of repair systems. Mutat Res. 2004;545(1-2):59–72.
Ertuğrul H, Yalçın B, Güneş M, Kaya B. Ameliorative effects of melatonin against nano and ionic cobalt induced genotoxicity in two in vivo Drosophila assays. Drug Chem Toxicol. 2020;43(3):279–86.
Carvajal-Garcia J, Gales ER, Ramsden DA, Sekelsky J: The Drosophila melanogaster Ortholog of RFWD3 Functions Independently of RAD51 During DNA Repair. G3 (Bethesda, Md) 2020, 10(3):999-1004.
Queiroz NCA, Jorge MP, Sousa IMO, Lima CSP, Matias MCM, Dal Rio AC, et al. Arrabidaea chica for oral mucositis in patients with head and neck cancer: a protocol of a randomised clinical trial. BMJ Open. 2018;8(10):e019505.
Costa Salles TH, Volpe-Zanutto F, de Oliveira Sousa IM, Machado D, Zanatta AC, Vilegas W, et al. Electrospun PCL-based nanofibers Arrabidaea chica Verlot - Pterodon pubescens Benth loaded: synergic effect in fibroblast formation. Biomedical Materials (Bristol, England). 2020;15(6):065001.
Campos de Siqueira F, Teixeira Costa Leitão DDS, Zerlotti Mercadante A, Campos Chisté R, Santos Lopes A. Profile of phenolic compounds and carotenoids of Arrabidaea chica leaves and the in vitro singlet oxygen quenching capacity of their hydrophilic extract. Food Res Int (Ottawa, Ont). 2019;126(108597).
Acknowledgements
This work is dedicated to Luiz Ricardo Goulart Filho (in memoriam), PhD, a brilliant Brazilian scientist who have deceased due to covid-19. We are grateful that we have worked with a brilliant scientist and an incomparable person.
Funding
This research was funded by Fundação de Amparo à Pesquisa de Minas Gerais (FAPEMIG), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenadoria de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), and National Institute of Science & Technology in Theranostics and Nanobiotechnology (NIST-TeraNano).
Author information
Authors and Affiliations
Contributions
Conceptualization, T.G.A. and A.A.S.F.; methodology, D.C.B., P.M.A.P.L, I.C.M., C.S.C., A.O.C., J.F.C.G., M.C.G. and D.S.C.; validation, D.C.B. and P.C.O.; formal analysis, T.G.A., D.C.B. P.M.A.P.L. and P.C.O.; writing - original draft preparation, D.C.B. and P.M.A.P.L.; writing - review and editing T.G.A.; A.A.S.F. and L.V.; project administration, T.G.A.; funding acquisition, T.G.A. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Brandão, D.C., Lima, P.M.A.P., Martins, I.C. et al. Arrabidaea chica chloroform extract modulates estrogen and androgen receptors on luminal breast cancer cells. BMC Complement Med Ther 22, 18 (2022). https://doi.org/10.1186/s12906-022-03506-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-022-03506-3