Abstract
Background
To evaluate the flexural strength of digitally milled and printed denture base materials.
Methods
The materials tested were Lucitone 199 denture base disc (Dentsply Sirona), AvaDent denture base puck (AvaDent), KeyMill denture base disc (Keystone), Lucitone digital print denture base resin (Dentsply Sirona), Formlab denture base resin (Formlabs), and Dentca base resin II (Dentca). Sixty bar-shaped specimens of each material were prepared for flexural strength testing and were divided into five groups: control, thermocycled, fatigue cycled, and repair using two different materials. The flexural strength and modulus were tested using a 3-point bend test performed on an Instron Universal Testing Machine with a 1kN load cell. The specimens were centered under a loading apparatus with a perpendicular alignment. The loading rate was a crosshead speed of 0.5 mm/min. Each specimen was loaded with a force until failure occurred. A one-way ANOVA test was used to analyze the data, followed by Tukey’s HSD test (α = 0.05).
Results
The milled materials exhibited higher flexural strength than the printed materials. Thermocycling and fatigue reduce the flexural strengths of printed and milled materials. The repaired groups exhibited flexural strengths of 32.80% and 30.67% of the original flexural strengths of printed and milled materials, respectively. Nevertheless, the type of repair material affected the flexural strength of the printed materials; the composite resin exhibited higher flexural strength values than the acrylic resin.
Conclusions
The milled denture base materials showed higher flexural strength than the printed ones.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
The provision of removable prostheses could enhance oral health-related quality of life. Patients’ satisfaction with dentures is related to using dentures while performing certain functions comfortably [1]. Since removable dentures are still in demand and the conventional technique of complete denture (CDs) fabrication was invented more than 80 years ago, the continuing goal is to overcome all the difficulties related to the fabrication process and enhance the properties of polymethyl methacrylate (PMMA) [2]. Computer-aided design and computer-aided manufacturing (CAD/CAM) technology has led to advancement in designing and manufacturing dental prostheses. This technology has been incorporated into the fabrication of complete dentures. CAD gathers data directly by recording dental structures intraorally or indirectly by scanning impressions or casts orally. The software was used to design the prosthesis. CAM can be performed using rapid prototyping, such as 3D printing (additive method) or computerized numerical control (CNC) machining (subtractive method) [3, 4].
In the field of dentistry, CAD/CAM began with milling technology. The final product file is sent to a milling machine that mills a pre-polymerized denture base acrylic resin block to form the denture base with a designed tooth socket to be received or mills the entire denture in one piece, including the teeth. In addidtive manufacturing the material is selectively deposited in layers, which makes it more conservative and has more design freedom. The advantages of using CAD/CAM technology include high speed, ease of use, high quality, improvement in the mechanical properties of the material, and a reduction in human errors [4, 5]. However, PMMA is not free of problems. PMMA problems are related to fracture strength, color stability, dimensional stability, porosity, processing techniques, and biocompatibility (allergic reactions). The CAD/CAM-milled materials used were prefabricated disc of acrylic resin. The block is manufactured under high heat and pressure, which improves its mechanical properties and reduces the free monomer and porosity compared to processed dentures [6]. 3D printing materials have similar properties to conventional acrylic resins with the convenience of UV (ultraviolet) light curing instead of heat [7]. As the literature began to investigate machinable block properties, a sudden shift occurred to newer technologies in the form of 3D printing materials. Digital dentures were fabricated as described by Goodacre et al. (2012) [5]. The first 3D-printed denture by Dentca was developed in 2015 [8]. Many companies have produced prepolymerized PMMA blocks to which milled or prefabricated denture teeth are subsequently bonded. Recently, a method was established to mill the denture base and teeth from a single denture block AvaDent (AvaDent, USA), Baltic7 denture systems (Merz Dental, Germany), and Ivoclar Vivadent Ivotion (Ivoclar, Vivadent, Liechtenstein). Currently, many factors account for the shift from milling to 3D printing. 3D printing is more economical than milling machines, which involve rotary tool wear replacement and raw material waste. 3D printing enables the simultaneous fabrication of multiple products. While milling depends on the size and number of milling burrs [9]. The main disadvantage of milling is the waste of a large portion of the block that goes to waste, in addition to monochromatic and un-esthetic teeth [9]. The total duration to mill and print a denture is extremely different, favoring the printing process with much higher productivity. The recent popularity and effectiveness of (CAD/CAM) systems have led to the introduction of various denture resin materials. Owing to the lack of literature and independent studies on these materials, it is essential to evaluate their physical and mechanical properties to determine their viability [11]. However, evidence supporting the clinical superiority of CAD/CAM-fabricated dentures and their material-related properties remains limited [12]. Knowledge of the materials used for denture bases and understanding of the underlying properties will provide solid evidence to help clinicians decide on the most appropriate treatment for patients. The fracture resistance of denture base materials can enhance the longevity of the prosthesis, reduce the need for repair, and improve patient satisfaction. Regardless of the mode of fracture (whether it occurs because of an accident or fatigue), the flexural strength of the denture base material is a good indicator of its clinical performance [13]. The breaking load quantifies the resistance of a material to fracture. In a clinical study, bite forces did not exceed 55 N among full-denture wearers [14]. In patients with advanced mandibular bone resorption and users of removable dentures, the maximum biting force decreased to 40 N. A recent study investigated commercially available heat-treated, milled, and printed denture base materials. The breaking loads of all denture base resins were above 40 N [15]. However, CAD/CAM materials may not have better resistance to fracture than conventional materials. The mechanical properties of denture base materials obtained in vitro may not represent reality. The oral environment is subject to constant temperature changes and continuous occlusal loads. Therefore, evaluating the effects of thermocycling and cyclic loading on the mechanical properties of denture base materials is beneficial for clinical applications. The ultimate flexural strength should not be less than 65 MPa for polymer types according to the ISO-20795-1:2013 [16].
The major shortcomings of conventional PMMA resins include fatigue failure, susceptibility to fracture, and dimensional instability [17]. In a study conducted in 2014, after 18 months of clinical use, the denture fracture rates were 40.8% and 59.2% for maxillary and mandibular dentures, respectively, of which 70.4% had midline fractures during this short period [18].
Theoretically, complete dentures are not prone to fracture in edentulous patients, owing to low masticatory forces. However, the literature has demonstrated various incidences of fractures stemming from fatigue mechanisms, the presence of porosity defects during fabrication, faulty design, and tooth arrangement [17,18,19]. Denture repair procedures usually involve rejoining broken denture base pieces or replacing a tooth (or both). Auto-polymerizing resin is the material of choice for rejoining fractured pieces. Once the repaired material is fully polymerized, it cannot be physically separated from the joined sections. Evaluating the durability of repaired dentures after a fracture is of great clinical importance.
This study evaluated the mechanical properties of milled denture base and 3D-printed denture base materials used to fabricate CAD/CAM dentures. The null hypothesis is that there is no statistically significant difference in the flexural strength of milled and printed denture base materials.
Methods
In this study, the digital CAD/CAM denture base materials investigated were:
-
1.
Lucitone 199 denture base disc original (Dentsply Sirona)- milled.
-
2.
AvaDent denture base puck original (AvaDent) - milled.
-
3.
KeyMillTM denture base disc pink (Keystone) - milled.
-
4.
Lucitone 3D digital print denture base original resin (Dentsply Sirona) − 3D print.
-
5.
Formlabs denture base OP original pink resin (Formlabs) − 3D print.
-
6.
Dentca denture base II original pink resin (Dentca) − 3D print.
Sixty bar-shaped specimens of each of the six denture base materials with dimensions of 4 mm × ´ 4 mm × 25 mm according to the ISO-20795-1:2013 [11], were prepared using the following processes: the CAD/CAM block was sectioned into a grid of rectangular bars by using a 15 LC diamond wafer blade mounted on an Isomet 5000 Precision Saw (Buehler, Lake Bluff, Illinois, USA). Cuts were made at 900 rpm using water irrigation. The dimensions of the sectioned specimens were measured using a micrometer (Model no.293–715; Mitutoyo Corporation, Kanagawa, Japan) [19]. 3D printed materials with the same dimension bars were designed in Autodesk Meshmixer (3.5 macOS) software into bars and exported as a standard tesselation language (STL) file to the printers. Two different printers were used according to the type of material: a Form 2 printer (Model: MELODIOUSSKUNK, Formlabs) and a Carbon3D printer (Model:102750, Carbon3D). Printing layer thickness was 50 μm with 90°angle of orientation of the specimens to the printing platform according to manufacturer recommendation [19]. Specimens were transferred from Formlabs to PreForm software (version 2.19.2), and automatic supports were created. A Form 2 printer was set up, filling the tank with the OP denture base material. The printed specimens were removed from the build platform, and the post-processing treatment was completed. Isopropyl Alcohol (ACS) (IPA) 100% (Lab Chem, Zellenople, PA, USA) was used for primary cleaning for 10 min to dissolve excess or uncured resin. Lastly, the specimens were dried to remove any alcohol on the surface; afterward, the specimens were immersed in glycerin (Vegetable Glycerin, Glycerin supplier, Houston, TX) and then cured in Form Cure at 80 °C for 30 min.
A carbon printer was used to print the Lucitone 3D digital print material and the Dentca denture base material according to the manufacturer’s instructions. After exporting the STL file from the Autodesk Meshmixer to the Carbon 3D software, proper alignment was achieved without support. The Lucitone 3D digital print denture base material was loaded into a printer tank. Once the printing was completed, the specimens were removed from the build platform and washed with 100% isopropyl alcohol (IPA) using a two-bath approach with fresh IPA. Using an ultrasonication bath, the specimens were washed for two minutes (1st cycle), followed by another one minute (2nd cycle). The specimens were dried and cured on one surface of a turntable using an inLab SpeedCure. (Model: JJA2034103) processing unit for 10 min, followed by a 3-minute cooldown. When one side was completely cured, the specimens were flipped, and the other surface was cured for another 10 min, followed by a 3-minute cooldown. The printing procedure for Dentca materials is almost the same as that for Lucitone 3D digital printing. Once the printing was complete, the specimens were washed with 100% isopropyl alcohol in a container over an orbital shaker (Model: S-2.02.20 M) for 5 min at 140 RPM and air-dried for 10–15 min. Finally, the specimens were immersed in a glycerol bath in a Dreve PCU LED box (Model 220000014; DREVE, Germany) for 30 min at 90% intensity. Subsequently, all specimens were polished using a Buehler Grinder-Polisher system (EcoMet 250, Buehler, Lake Bluff, IL, USA). The sequence was as follows: 45 μm and 15 μm diamond grinding disks (Buehler, Lake Bluff, IL) with water were used; further polishing was performed with 1 μm polycrystalline diamond suspension applied onto a cloth polishing pad. The specimen dimensions were measured using a digital micrometer. The specimens had a variation of about ± 0.2 mm in width. Specimens that fell outside of this range were discarded. Finally, the specimens were divided into different groups, and the 12 specimens were divided into control, fatigue, and thermocycle groups. Additionally, another twenty-four specimens were prepared for the repair test group.
Cyclic loading (fatigue group)
Twelve-bar specimens per material were subjected to 60% of the measured static fracture load in the control group at a frequency of 1 Hz in a water bath under a pneumatically driven fatigue tester for 50,000 cycles [21, 22]. A powered cylinder and an electronic control device (Pober Industries, Waban MA) were used for fatigue cycling. The load was applied perpendicular to and at the center of the specimen using a three-point bend fixture with a 7/8” diameter piston.
Thermal cycle
Twelve bar specimens for each material were simultaneously exposed to the same thermal temperature changes by repetitive immersion into 5 °C cold water for 30 s and subsequently into 55 °C hot water for another 30 s each cycle for 5,000 cycles. The thermal cycle apparatus (Sabri Dental Enterprises, Downers Grove, IL) consisted of two tanks containing hot and cold water, and a basket-holding specimen was moved between the hot and cold baths at preset times [23, 24].
The repairing materials used were
-
Jet Set-4TM Set; self-polymerized acrylic resin Tooth Shade (Jet, Lang Dental Mfg.).
-
GradiaÒ Gum Shade GC, Modifier GM32 Flowable Composite (GC America Inc) + GradiaÒ Indirect Restoration System-Composite Primer (GC America Inc); light-polymerized.
Repairing procedure
Twenty-four bar specimens were prepared for each specimen. A silicone mold was prepared using a bar specimen to aid in repairing the bars (Exaflex Putty; Vinyl Polysiloxane (GC America). The specimens were sectioned in the middle using a diamond blade with an Isomet 11-1180 low-speed saw (Buehler, LTD). The joint surface was trimmed to ensure an accurate fit between the fragments. Sectioned bars were placed to assist in orienting and holding the specimens during repair. Repairing procedure is illustrated in Fig. 1. Each group was divided into two subgroups, A and B (n = 12 in each group). Group A was repaired with self-polymerized acrylic, and Group B was repaired with flowable direct composite resin following the manufacturer’s instructions. The gap was estimated to be standardized as 0.7–1.0 mm as the thickness of the blade and minimum finishing [17].
Subgroup A
The composite primer was applied with a brush to each side of the joint and then light cured for 1 min (Bluephase 20i, wavelength 385–515 nm). Composite resin was applied to each side and held to join the two parts of the bar under the pressure of the silicone mold. Light curing was performed on all sides for 3 min.
Subgroup B
The liquid of Jet Set-4 was applied with a brush on each side of the joint to wet the area, then adding a brush on each side. The repaired bar was placed in the mold, and the liquid was brushed on top of the bar to ensure coating. The bar was held under the pressure of the silicone mold for 4 min. The repaired bars were polished to remove excess repaired material following the same sequence as previously mentioned.
Flexural strength testing
Specimens were stored in an incubator in distilled water at 37 °C for a week: control, fatigued, thermocycled, and repaired groups. The specimens were air-dried for 10 min before testing. Three-point bending tests were conducted according to the International Organization for Standardization guidelines (ISO 6872:2014(E)). A three-point flexural test of the specimen was performed on an Instron 5566 A Universal Testing Machine (Instron, Norwood, Massachusetts) with a 1kN load cell. The specimens were positioned on a fixture and centered under a loading apparatus with a perpendicular alignment. The loading rate was a crosshead speed of 0.5 mm/min, controlled using Bluehill Universal 4.08 software version (Instron, Norwood, Massachusetts) [21]. Each specimen was loaded with a force until failure occurred.
The flexural strength and flexural modulus calculations were obtained directly by the calculation software through these formulas:
Flexural strength [MPa].
where:
α is the flexural strength [MPa].
P is the maximum load [N].
L is the support span [mm].
b is the width of the specimen at the failure site [mm].
h is the height of the specimens at the failure site [mm].
Flexural modulus [MPa]
Where.
L is the support span [mm].
m is the slope of the linear portion of the load-deflection curve [N/mm].
b is the width of the specimen at the failure site [mm].
h is the height if the specimen at the failure site [mm].
Differences in flexural strength and modulus were analyzed using a one-way analysis of variance (ANOVA). Post-hoc flexural strength testing was accomplished using the Tukey HSD test (a = 0.05) for paired comparisons of the means of the different groups. All statistical analyses were performed using the JMP Pro Statistics software package for Mac (15.1.0 version).
Results
For the control group, the mean of the flexural strength of milled materials was 137.32 ± 14.18 MPa, while printed materials was 119.73 ± 13.00 MPa. AvaDent exhibited the highest flexural strength of 146.00 ± 12.53 MPa, whereas Lucitone 3D print exhibited the lowest of 108.12 ± 2.17 MPa, showing a statistically significant difference between them. As for the flexural modulus, the Dentsply Block exhibited the highest value of 2.09 ± 0.61 GPa, while Dentca displayed the lowest of 1.15 ± 0.27 GPa. Notably, the milled materials exhibited higher flexural strength and modulus than the 3D printed materials, considering a significant difference of (p < 0.0001). For the control group, the flexural strength and flexural modulus of the different denture materials are presented in Tables 1 and 2. In the control group, the flexural strength was significantly highest in AvaDent, while flexural modulus was significantly highest in Dentsply Block.
For the fatigued and thermocycled groups, the flexural strengths and moduli of the specimens were tested after cyclic loading and thermocycling. The flexural strength decreased for materials subjected to post-treatments, such as cyclic loading or thermocycling. In the fatigued group, the flexural strength was significantly highest in Dentsply Block, while in the thermocycled group, the flexural strength was significantly highest in Dentca, Dentsply Block, and Keystone.
Tables 3 and 4 summarize the statistical analysis of the fatigued group, while Tables 5 and 6 summarize those of the thermocycled group.
Summary of flexural test for control compared to post-treatment
These factors were evaluated separately to determine their effect on the flexural strength of the materials. The flexural strength decreased for materials subjected to post-treatments such as cyclic loading or thermocycling. A regression model analysis was used to analyze the factorial interaction between different brands and the interaction with post-treatment factors for the response variable of flexural strength (R2 = 0.52). Tukey’s test determined the significance between groups (p = 0.0001). The flexural strengths of the tested materials decreased with the cycling loading except for Dentsply Block and Lucitone 3D print. Another regression model analysis was used to investigate the factorial interaction between the different brands and the interaction with post-treatment for the flexural modulus response variable (R2 = 0.29). Tukey’s test determined the significance between groups (p = 0.00002).
The flexural strength and flexural modulus of 3D printed groups remained after aging (post-treatment as fatigue or thermocycle). Compared to the milled group, the flexural strength and flexural modulus decreased after post-treatment (fatigue and thermocycling). The results are presented in Tables 7 and 8. However, the flexural strength of the milled and 3D printed groups decreased, whereas that of the 3D printed group with post-treatment (fatigue and thermocycling). Regression model analysis examined the factorial interaction between the different fabrication methods and the interaction with post-treatment variables for flexural strength (R2 = 0.25). Tukey’s test was used to determine the significance of differences between groups (p = 0167). Regression model analysis was used to probe the factorial interaction between different fabrication methods and the interaction with post-treatment for the flexural modulus (R2 = 0.19). Tukey’s test was used to determine the significance of differences between groups (p = 00002).
Fracture graphic analysis - microstructure analysis by 3D microscope
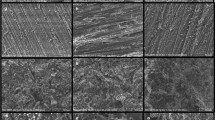
Imaging and scanning electron microscope (SEM)
Fractured specimens from the control group for each material were evaluated using a 3D microscope (VHX-7100 and VHX-S750E; Keyence Corporation, Japan). One specimen from each group was evaluated to characterize its microstructure and fracture mode. For the milled group, the material exhibited deformation on the tensile side before fracturing, as shown in Figs. 2, 3, 4, 5 and 6, and 7. Moreover, the 3D printed group indicated differences between the brands. The Lucitone 3D printer exhibited a high deformation before fracture on the tensile side, whereas Formlabs and Dentca showed a brittle fracture mode. The compression side exhibited shattered pieces, and less deformation was observed on the tensile side before fracture. The results are shown in Figs. 8, 9, 10, 11 and 12, and 13. The load appears to form microcracks when the material deteriorates. Microcracks would lead to complete failure, as fractures occur more rapidly than ductile fractures. These features were observed in 3D printed materials, specifically in Formlabs and Dentca. Lucitone 3D print materials can tolerate increased loads until ultimate fracture but with highly ductile deformation. The keystone material was similar to the load analysis of the Lucitone 3D print material but with less ductile deformation and higher load tolerance. The AvaDent and Dentsply Block materials resisted the maximum load of all tested materials with the least ductile deformation. These characteristics are observed in the SEM and 3D microscope images below and coincide with the load-displacement curve shown in Fig. 14.
3D Microscope images of AvaDent specimen fractured after 3-point bending test 3D Microscope images under x40 Magnification with blue arrows exhibiting the force direction. The approximated fractured joints under x20 magnification exhibited the tension and compression side of the fracture. No obvious deformation was observed at the fracture side
3D Microscope image of Dentsply Block specimen fractured after 3-point bending. 3D Microscope images under x40 Magnification with blue arrows exhibiting the force direction. The approximated fractured joints under x20 magnification exhibited the tension and compression side of the fracture. Minute deformation on the tensile side, with clear sharp fracture at the compression side
3D Microscope images of Keystone specimen fractured after 3-point bending test 3D Microscope images under x40 Magnification with blue arrows exhibiting the force direction. The approximated fractured joints under x20 magnification revealed the tensile and compression side of the fracture. Minute deformation on the tensile side, it is clear at the fracture edges. Clear sharp fracture on the compression side
3D Microscope images of Lucitone 3D print specimen fractured after 3-point bending test. 3D Microscope images under ×40 Magnification with blue arrows exhibiting the force direction. The approximated fractured joints under ×20 magnification indicated the tensile and compression side of the fracture. Clear deformation on the tension side. Clear sharp fracture at the compression side
3D Microscope images of Dentca specimen fractured after 3-point bending test. 3D Microscope images under ×40 Magnification with blue arrows exhibiting the force direction. The approximated fractured joints under ×20 magnification exhibited the tension and compression side of the fracture. Clear deformation on the edges of the fracture on tension side. Compression side exhibited the brittleness of the material and deformation below the outside layer of the specimen
SEM images of Formlabs specimen fractured after 3-point bending test. The SEM images under ×200 magnification showed brittleness of the material under load. It revealed the pattern of the fracture. On the right, image under ×100 magnification reveals the direction of the load from the edges and transfer through the fracture specimen
3D Microscope images of Formlabs specimen fractured after 3-point bending test. 3D Microscope images under ×40 magnification with blue arrows exhibiting the force direction. The approximated fractured joints under ×20 magnification exhibited the tensile and compression side of the fracture. Minute deformation on the edges of the fracture was on tension side. The compression side exhibited brittleness of the material and the corresponding deformation occurred below the outside layer of the specimen. The fractured pieces were observed at this side. These patterns displayed the behavior of brittle materials
Load-Displacement curves of tested denture base materials. The x marks represent the starting point of non-linear curvature, which corresponds to the start of plastic deformation of the materials. In general, the milled group has a higher resistance to deformation than the printed group of materials, except for Keystone. While the printed materials may be able to withstand a larger load by exhibiting limited deformation. Lucitone 3D print had the largest deformation before fracture
Repaired group
The specimens from the repaired group mimicked the fracture and repair of dentures in a dental clinic. The most popular method of repair is using self-polymerized acrylic, although manufacturers of 3D printing materials recommend composite resin because of the nature of the denture base material. The flexural strength of the repaired milled specimens was only approximately 28-31% of the mean original flexural strength in the control group, whereas that of the repaired printed specimens ranged from 13 to 51% of their original flexural strength. These data are presented in Table 9. Figure 15 shows the differences between the control and repair groups using different repair materials. A regression model was used to evaluate the factorial interaction of the repair materials of other brands (R2 = 0.96) (p < 0.0001), and Tukey’s test was performed, and the results were considered statistically significant.
The flexural strengths of the repaired milled specimens were not significantly affected by the repair material (P = 0.0001). There was no significant difference between the groups treated with the acrylic and composite resins (p = 0.0001). However, the flexural strength of the printed group of the composite resin repair material was significantly higher than that of the acrylic repair group (P = 0.0001). The data are presented in Table 10. *Levels not connected with the same letter are significantly different.
Summary of flexural test results in repaired specimens
The primary purpose of the flexural test was to determine whether the repaired specimens maintained denture durability. For both the milled and 3D printed materials repaired with acrylic and/or composite resins, the flexural strength decreased by more than 50% of its original strength. The flexural strengths of these repaired specimens did not meet the polymer requirements of at least 60 −65 MPa, according to the ISO 20795-1:2013 standard [12]. All specimens broke at the same fracture joint, which is considered the stress-breaking point. The clinical implications of these results indicate that remaking dentures is more favorable than repairing them. This repair procedure serves as a temporary solution. One specimen from each group was analyzed under a 3D microscope. The bonding properties of the repair materials to the base are shown in Figs. 16, 17, 18, 19 and 20, and 21.
3D Microscope images of repaired AvaDent specimens under ×40 magnification. A, B, and C images represents the denture base bar repaired with composite resin. There was no composite resin residue found on the fracture side. D, E, and F images represents the denture base bar repaired with acrylic. There was a tiny amount of acrylic residue (indexed by blue arrow) found on the fracture side
3D Microscope of repaired Dentsply Block specimen under 40× magnification A, B and C images were the denture base bar repaired with composite resin. Composite resin residue (indexed by blue arrow) found on one fractured side only. D, E and F images were the denture base bar repaired with acrylic. Acrylic residue found on one fractured side only (F)
3D Microscope of repaired Keystone specimen under 40× magnification A, B and C images were the denture base bar repaired with composite resin. There was no composite resin residue found on the fracture side. D, E and F images were the denture base bar repaired with acrylic. Acrylic residue found on one fracture side only (F)
3D Microscope of Formlabs repaired specimen under 40× magnification A, B and C images were the denture base bar repaired with composite resin. Partial composite resin residue (indexed by blue arrow) found on both sides. D, E and F images were the denture base bar repaired with acrylic. Acrylic residue found on one fracture side only (E)
3D Microscope of Dentca repaired specimen under 40× magnification A, B and C images were the denture base bar repaired with composite resin. Partial composite resin residue (indexed by blue arrow) found on both sides of the fracture. D, E and F images were the denture base bar repaired with acrylic. Acrylic residue found on one fracture side only (F)
3D Microscope of Lucitone 3D print repaired specimen under 40× magnification A, B and C images were the denture base bar repaired with composite resin. Composite resin residue found on both fractured sides. D, E, and F images were the denture base bar repaired with acrylic. Acrylic residue found on one fracture side only (F)
Discussion
The evaluation of the clinical efficacy of denture base materials used in in vitro testing is based on various mechanical and optical properties. According to ISO standards, the mechanical requirements of denture base polymers must have an ultimate flexural strength of not less than 65 MPa [16]. Three-point or four-point loadings are acceptable tests for denture base materials [16]. The null hypothesis that there is no significant difference in the flexural strength of milled against printed denture base materials, was rejected.
The differences between the ISO (3-point bending test) and ASTM (4-point bending test) methods are the specimen size, shape, thickness, load nose radius, bending momentum, maximum allowable strain, and axial stress. Flexural strength is a material property defined as the maximum stress in a material immediately before it yields. The flexural modulus is the ratio of stress to strain in a flexural deformation. Denture durability may, in part, be measured by flexural strength. Because a denture base may fracture clinically for various reasons, the material must have a high flexural strength due to mastication fatigue or extra orally due to unexpected accidents. The literature related to milled denture base materials was evaluated and compared with that of conventional denture base materials. However, the literature on 3D printed denture base materials has focused on evaluating dimensional accuracy [20]. There are only a few studies available in the literature that have examined the denture base properties tested in this study. A study tested five different types of milled materials: AvaDent, Baltic Denture System, Vita Vionic, Weida digital dentures, and Whole You denture base materials compared to two different conventional materials: Candulor Aesthetic Red (heat cure) and Candulor Aesthetic Blue (self-cure). The mean breaking load was highest for the Weiland Digital Denture block at 82.5 N, while the lowest was 40.3 N for Vita Vionic respective block [15]. In comparison, the breaking load was lower than that in this study because the previous study created pre-cracks in each material in tension sites before placing the bars under a load. Another study reported a mean flexural strength as high as 125.9 MPa in the AvaDent group, which is consistent with the results of this study [22].
There are more studies on milled materials in the literature owing to the increased employment of the subtractive method in fabricating complete dentures [2]. As mentioned previously, literature regarding the mechanical properties of CAD/CAM materials is sparse. The varying AM results of additive manufacturing could be due to multiple factors affecting the output. The printing layer thickness, laser intensity, laser speed, printing angle, and printing orientation were the key variables affecting the outcomes [9]. The difference in the mechanical property values between the milled brands can be explained in terms of the different densities and compositions of each material [21]. A Study compared two milled groups: AvaDent and Tizian Blank PMMA with one conventional heat-polymerized Meliodent. The highest flexural strength was observed in the Tizian group at 130.7 MPa, with the AvaDent at 123.1 MPa, the lowest in the conventional group. The flexural modulus was highest for the AvaDent group at 2519.6 MPa, followed by the Tizian group at 2474.7 MPa and then conventional [2]. A recent study evaluated the flexural strength of three milled materials: L-Temp, Temp Basic Tissue, and IvoBase in comparison to conventional auto-polymerized palapress and conventional heat-polymerized Paladon 65. The highest flexural strength was recorded for the heat-polymerized materials, followed by the L-Temp milled materials, and the lowest flexural strength was recorded in the TemporBasic Tissue-milled group [19]. It can be concluded that there is a comparable flexural strength between milled and conventional denture base materials; however, the easier fabrication process and lower susceptibility to errors could favor the production of milled materials. The printing of materials is technique-sensitive because the printing procedure can affect the output [9]. The literature demonstrates that the orientation of a specimen affects its flexural and tensile strengths. It differs depending on the printing orientation in fused deposition modeling (FDM) with polylactic acid (PLA) and acrylonitrile butadiene styrene (ABS) [24]. The authors suggested that the observed phenomena depended on differential monomer exposure to light with different orientations [20]. A previous study reported that the flexural strength ranged from 120 to 160 MPa for 3D printed PMMA (NextDent Base) according to orientation. The flexural strength was the highest in the 0-degree orientation compared to the 45- and 90-degree orientation [9]. The present study followed the manufacturer’s recommendations to orient the specimens, finding the lowest flexural strength for 3D printed materials as compared to milled materials at 119.7 MPa (printed) and 137.2 MPa (milled), respectively. In contrast to the flexural modulus, higher values in the milled group than printed as 1.9 GPa and 1.4 GPa, respectively.
This means 3D printed materials can withstand more deformation before the breaking point than the milled materials. Milled materials generally can withstand higher loads and exhibit less deformation than 3D-printed materials. However, all the materials had flexural strength values higher than the ISO requirements. A high proportionality limit is required for the base material to resist plastic deformation and withstand repeated masticatory loads [25]. The flexural modulus mainly represents the elastic modulus and, to some extent, the plastic deformation in the material. Although the printed materials exhibited high flexural strength, their clinical efficacy could be better if plastic deformation exceeds the proportional limit. The elastic modulus of 3D printed restorative materials was evaluated in a study that concluded that the high elasticity exhibited by printed materials was due to the lack of filler particles [26]. However, a denture base resistant to deformation provides stable occlusion and appropriate positioning of the mandible. The deformation of the materials is presented in the load-displacement curves shown in Fig. 14.
To evaluate the long-term durability, the flexural strength of the materials was tested under conditions similar to those in the oral environment. Denture materials are subject to unpreventable aging factors. These materials are used in an intraoral environment and are exposed to different levels of occlusal loading and thermocycling owing to food and drink consumption. In a previous study, it was determined that aging affected the mechanical properties of the materials tested. Fatigue and thermocycling treatments decrease the flexural strength and increase the elastic modulus of conventional materials, as reported in the literature [28]. The longer the materials were immersed in water, the more the ultimate flexural strength decreased and the elastic modulus increased [28]. As the number of thermocycling treatments increased, the flexural strength of conventional materials decreased [25]. Regardless of the difference in the PMMA composition or light- or heat-polymerized materials, thermocycling significantly decreased the flexural strength of the materials [29]. Resistance to cyclic loading is a vital characteristic of denture base resins; however, relatively little information has been published concerning it. This study evaluated the effects of cyclic loading in a water bath to simulate clinical conditions. Cyclic loading exposed the specimens to a few load cycles lower than the static flexural strength failure load to stimulate clinical, functional stress. Under cyclic loading, cracks may develop and grow slowly, reducing the plastic deformation and ultimate failure load of the material [30].
In this study, the milled materials were more prone to aging and exhibited decreased flexural strength. However, the flexural modulus increased in the 3D printed group while and decreased in the milled group. This can be explained by the water sorption of the material when placed in a water bath. Water molecules enter the vacancies between the PMMA chains and expand the chains. Water may act as a plasticizer and facilitate the relaxation and movement of polymeric chains, which can degrade mechanical properties. With more extended periods of denture polymer immersion in water, more unreacted monomers and initiators may leach. The formed microvoids are filled with water molecules via inward diffusion. Therefore, the amount of residual free monomers can affect the change in properties over time [28, 29]. A paper that tested 3D-printed provisional restorative materials under artificial aging by immersing them in water for 21 days showed an overall decrease in the fracture load of all materials. These materials included a printed group: (1) Experimental (GC Europe), NextDent C&B, Freeprint Temp, 3Delta Temp, and a milled group; and (2) Teliocad and Luxatemp. The milled Teliocad exhibited a significantly lower fracture load than 3D-printed materials [30].
A previous study supports the results of the present study, which found that thermocycling decreased flexural strength in all groups, with a larger effect on milled materials. Although denture base materials are fabricated for long-term use, the literature needs more information on the effects of aging on the properties of CAD/CAM denture base materials. Significant shortcomings of PMMA resins include fatigue failure and susceptibility to fracture. There needs to be clear guidelines for preparing gaps or repair materials [30]. A study intended to establish an ideal material for denture repair using different techniques found that most of the repaired materials currently in use lose 45–65% of the original material strength, except for heat-polymerized materials aided by polyethylene fibers, which have approximately 34% loss of the base material’s original strength [17]. Consequently, developing cost-effective denture repair techniques and materials is considered necessary. A paper evaluated three different repair resins: heat-polymerized, auto-polymerized, and light-polymerized (repairing heat processed: Major Base 20, Major Prodotti Dentari S.p.A.Einaudi Moncalieri) and results showed that heat-polymerized resin had the highest flexural strength but performed at 51% of its original strength [31]. However, this technique (heat polymerized resin) requires custom-made gypsum investment and is time-consuming. One study evaluated three milled materials, LTemp, Temp Basic Tissue, and IvoBase CAD, and two conventional materials, Palapress and Paladon 65, repaired using auto-polymerized acrylic resin (Palapress). The repaired milled group exhibited a flexural strength of approximately 63% of its original strength. The repaired heat-polymerized paladon had comparable results to the repaired milled L-Temp of 60 and 70 MPa. However, the conventional paladon maintained only 40% of its original strength [19]. One research study evaluated the repair gap width and its effect on the strength of repaired specimens. A previous study recommended using up to a 1 mm space to overcome the drawbacks of stress from polymerization shrinkage at the repair interface and aging as thermal cycling, the lower strength of the repair material, possible excess of residual monomer, and a color mismatch [32]. Although the gap size recommendations were followed in the present study, the repaired specimens reached no more than 30.7% of the original strength in the milled group and 32.8% in the printed group. For the milled specimens, there was no difference in the type of repaired material between the auto-polymerized acrylic and composite resin, reaching 30.2% and 31.1% of the original strength, respectively. In contrast to the printed group, the composite resin repair achieved 46.8% of the original strength compared to 18.8% using acrylic. All repaired specimens fractured at the junction between the original base and repair materials. This indicates that the bond strength between the repair material and denture base material is poor.
Limitations of the study includes that additional surface modification to improve the bond between composite material to denture base wasn’t examined. Also, color change of the junction between composite resin layer and denture base must be evaluated.
Conclusions
-
1.
The flexural strength and flexural modulus were higher in milled groups than printed groups.
-
2.
The milled materials were more prone to artificial aging and cyclic loading than the printed materials, as indicated by the decrease in the flexural strength and modulus.
-
3.
In the control group, the flexural strength was significantly highest in AvaDent, while flexural modulus was significantly highest in Dentsply Block.
-
4.
In the fatigued group, the flexural strength was significantly highest in Dentsply Block.
-
5.
In the thermocycled group, the flexural strength was significantly highest in Dentca, Dentsply Block, and Keystone.
-
6.
In the repaired group, Lucitone 3D had the highest flexural strength when repaired with composite.
Data availability
Data is provided in a supplementary file.
Abbreviations
- CD:
-
Complete Denture
- PMMA:
-
PolyMethyle MethAcrylate
- CAD/CAM:
-
Computer-Aided Design and Computed Aided Manufacturing
- ISO:
-
International Standards Organization
- 3D:
-
Three Dimentional
- STL:
-
Standard Tessellation Language
- SEM:
-
Scanning Electron Microscope
References
Awad MA, Lund JP, Shapiro SH, Locker D, Klemetti E, Chehade A, et al. Oral health status and treatment satisfaction with mandibular implant overdentures and conventional dentures: a randomized clinical trial in a senior population. Int J Prosthodont. 2003;16:390–6.
Janeva NM, Kovacevska G, Elencevski S, Panchevska S, Mijoska A, Lazarevska B. Advantages of CAD/CAM versus Conventional Complete dentures - A Review. Open Access Maced J Med Sci. 2018;6:1498–502.
Bidra AS, Taylor TD, Agar JR. Computer-aided technology for fabricating complete dentures: systematic review of historical background, current status, and future perspectives. J Prosthet Dent. 2013;109:361–6.
Davidowitz G, Kotick PG. The Use of CAD/CAM in Dentistry. Den Clin North Am. 2011;55:559–70.
Goodacre CJ, Garbacea A, Naylor WP, Daher T, Marchack CB, Lowry J. CAD/CAM fabricated complete dentures: concepts and clinical methods of obtaining required morphological data. J Prosthet Dent. 2012;107:34–46.
Infante L, Yilmaz B, McGlumphy E, Finger I. Fabricating complete dentures with CAD/CAM technology. J Prosthet Dent. 2014;111:351–5.
Andreescu C, Ghergic D, Botoaca O, Hancu V, Banateanu AM, Patroi D. Evaluation of different materials used for fabrication of Complete Digital Denture. MATERIALE PLASTICE. 2018;55:124–8.
Anadioti E, Musharbash L, Blatz MB, Papavasiliou G, Kamposiora P. 3D printed complete removable dental prostheses: a narrative review. BMC Oral Health. 2020;20:343.
Shim JS, Kim J-E, Jeong SH, Choi YJ, Ryu JJ. Printing accuracy, mechanical properties, surface characteristics, and microbial adhesion of 3D-printed resins with various printing orientations. J Prosthet Dent. 2020;124:468–75.
Baba N. Materials and processes for CAD/CAM Complete Denture Fabrication. Curr Oral Health Rep. 2016;3.
International Organization for Standardization. Dentistry: ISO 20795-1:2013. ISO. [cited 2021. https://www.iso.org/cms/render/live/en/sites/isoorg/contents/data/standard/06/22/62277.html
Steinmassl P-A, Klaunzer F, Steinmassl O, Dumfahrt H, Grunert I. Evaluation of currently available CAD/CAM denture systems. Int J Prosthodont. 2017;30:116–22.
Murakami N, Wakabayashi N, Matsushima R, Kishida A, Igarashi Y. Effect of high-pressure polymerization on mechanical properties of PMMA denture base resin. J Mech Behav Biomed Mater. 2013;20:98–104.
Steinmassl O, Offermanns V, Stöckl W, Dumfahrt H, Grunert I, Steinmassl P-A. In Vitro Analysis of the fracture resistance of CAD/CAM denture base resins. Materials. 2018;11:401.
Venkat R, Gopichander N, Vasantakumar M. Comprehensive analysis of repair/reinforcement materials for polymethyl methacrylate denture bases: mechanical and dimensional stability characteristics. J Indian Prosthodont Soc. 2013;13:439–49.
Bhattacharya S, Ray P, Makhal M, Sen S, Incidence, And Causes Of Fracture Of Acrylic Resin Complete Denture. J Evol Med Dent Sci. 2014;3:14787–93.
Perea-Lowery L, Minja IK, Lassila L, Ramakrishnaiah R, Vallittu PK. Assessment of CAD-CAM polymers for digitally fabricated complete dentures. J Prosthet Dent. 2021;125:175–81.
Della Bona A, Cantelli V, Britto VT, Collares KF, Stansbury JW. 3D printing restorative materials using a stereolithographic technique: a systematic review. Dent Mater. 2021;37:336–50.
Prpić V, Schauperl Z, Ćatić A, Dulčić N, Čimić S. Comparison of Mechanical properties of 3D-Printed, CAD/CAM, and Conventional denture base materials. J Prosthodont. 2020;29:524–8.
Bedrossian EA, Chung K-H, Ramos V. Effect of layering gingiva-shade composite resin on the strength of denture base polymers. J Prosthet Dent. 2019;122:153.e1-153.e8.
Aguirre BC, Chen J-H, Kontogiorgos ED, Murchison DF, Nagy WW. Flexural strength of denture base acrylic resins processed by conventional and CAD-CAM methods. J Prosthet Dent. 2020;123:641–6.
Al-Dwairi ZN, Tahboub KY, Baba NZ, Goodacre CJ. A comparison of the Flexural and Impact strengths and Flexural Modulus of CAD/CAM and Conventional Heat-cured polymethyl methacrylate (PMMA). J Prosthodont. 2020;29:341–9.
Letcher T, Waytashek M. Material Property Testing of 3D-Printed Specimen in PLA on an Entry-Level 3D Printer. Vol. 2, ASME International Mechanical Engineering Congress and Exposition, Proceedings (IMECE). 2014.
Polychronakis N, Sarafianou A, Zissis A, Papadopoulos T. The influence of Thermocycling on the Flexural Strength of a Polyamide Denture Base Material. Acta Stomatol Croat. 2017;51:309–15.
Tahayeri A, Morgan M, Fugolin AP, Bompolaki D, Athirasala A, Pfeifer CS, et al. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent Mater. 2018;34:192–200.
Takahashi Y, Hamanaka I, Shimizu H. Effect of thermal shock on mechanical properties of injection-molded thermoplastic denture base resins. Acta Odontol Scand. 2012;70:297–302.
Takahashi Y, Hamanaka I, Shimizu H. Flexural properties of denture base resins subjected to long-term water immersion. Acta Odontol Scand. 2013;71:716–20.
Machado AL, Puckett AD, Breeding LC, Wady AF, Vergani CE. Effect of thermocycling on the flexural and impact strength of urethane-based and high-impact denture base resins. Gerodontology. 2012;29:e318–23.
dos Santos Nunes Reis JM, Vergani CE, Pavarina AC, Giampaolo ET, Machado AL. Effect of relining, water storage and cyclic loading on the flexural strength of a denture base acrylic resin. J Dent. 2006;34:420–6.
Reymus M, Fabritius R, Keßler A, Hickel R, Edelhoff D, Stawarczyk B. Fracture load of 3D-printed fixed dental prostheses compared with milled and conventionally fabricated ones: the impact of resin material, build direction, post-curing, and artificial aging—an in vitro study. Clin Oral Investig. 2020;24:701–10.
AlQahtani M, Haralur SB. Influence of different repair Acrylic Resin and Thermocycling on the Flexural Strength of Denture Base Resin. Med (Kaunas). 2020;56:50.
Gad MM, Rahoma A, Abualsaud R, Al-Thobity AM, Fouda SM. Effect of Repair Gap Width on the strength of denture repair: an in Vitro comparative study. J Prosthodont. 2019;28:684–91.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Shatha alshali- reviewed the manuscript , publication process. Ghadeer Basunbul- wrote the manuscript. Anhar Basunbul- prepared the specimens, did the experiment. Russell Giordano- statistical analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
For this type of study formal consent is not required. This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Alshali, S., Basunbul, G., Basunbul, A. et al. Comparison of the flexural strength of printed and milled denture base materials. BMC Oral Health 24, 929 (2024). https://doi.org/10.1186/s12903-024-04695-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-024-04695-8