Abstract
Background
Despite being a prognostic predictor, cardiac autonomic dysfunction (AD) has not been well investigated in chronic obstructive pulmonary disease (COPD). We aimed to characterise computed tomography (CT), spirometry, and cardiopulmonary exercise test (CPET) features of COPD patients with cardiac AD and the association of AD with CT-derived vascular and CPET-derived ventilatory efficiency metrics.
Methods
This observational cohort study included stable, non-severe COPD patients. They underwent clinical evaluation, spirometry, CPET, and CT. Cardiac AD was determined based on abnormal heart rate responses to exercise, including chronotropic incompetence (CI) or delayed heart rate recovery (HRR) during CPET.
Results
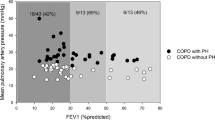
We included 49 patients with FEV1 of 1.2–5.0 L (51.1–129.7%), 24 (49%) had CI, and 15 (31%) had delayed HRR. According to multivariate analyses, CI was independently related to reduced vascular volume (VV; VV ≤ median; OR [95% CI], 7.26 [1.56–33.91]) and low ventilatory efficiency (nadir VE/VCO2 ≥ median; OR [95% CI], 10.67 [2.23–51.05]). Similar results were observed for delayed HRR (VV ≤ median; OR [95% CI], 11.46 [2.03–64.89], nadir VE/VCO2 ≥ median; OR [95% CI], 6.36 [1.18–34.42]).
Conclusions
Cardiac AD is associated with impaired pulmonary vascular volume and ventilatory efficiency. This suggests that lung blood perfusion abnormalities may occur in these patients. Further confirmation is required in a large population-based cohort.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is an inflammatory disease of the airways, alveoli, and microvasculature with systemic effects [1]. Cardiac autonomic dysfunction (AD) predicts long-term mortality, even after adjusting for coronary anatomy and left ventricular function [2, 3]. It is evaluated using a range of variables, among which abnormal heart rate (HR) responses to exercise are particularly attractive owing to their simplicity, availability, and clinical significance. Abnormal HR responses include an inability to use most of the HR reserve during exercise (chronotropic incompetence [CI]) or an inability to immediately slow the HR after exercise (abnormal HR recovery).
Previous studies of AD focused on cardiovascular diseases (CVDs), which worsen cardiac pump function [4,5,6,7]. AD is also highly prevalent in respiratory diseases [8, 9]. However, for COPD, which results in approximately 3 million global deaths annually [1], the factors related to cardiac AD remain unclear [10]. Thus, cardiac AD should be assessed and considered during COPD management [11]. HR responses during incremental exercise to evaluate cardiac autonomic function may be inappropriate in severe COPD patients. Because of ventilatory limitations, they are more likely to stop exercising before they reach their real maximal HR. However, underestimating cardiac function may not occur in mild-moderate COPD, wherein respiratory abnormalities are less pronounced.
Few research studies have explored how COPD-related mechanisms affect cardiac autonomic function [12]. Since enlarged lung volume is associated with impaired cardiac function [13, 14], most studies focused on only the negative effects of airflow obstruction and lung hyperinflation [15, 16]. However, studies have not assessed the impact of pulmonary circulation abnormalities on cardiac AD in COPD, despite the confirmed negative effects of pulmonary vascular loss on cardiac structure and functionRecently, non-invasive methods have provided valuable information reflective of pulmonary blood perfusion. For example, a pulmonary vessel tree segmented using computed tomography (CT) can directly assess pulmonary vascular volume (VV) [17, 18]. Reduced ventilatory efficiency (elevated physiological dead space) shown via a cardiopulmonary exercise test (CPET) reflects vascular pruning and capillary hypoperfusion in COPD [19, 20].
Therefore, this study aimed to characterise the pulmonary structure, lung function, and cardiopulmonary exercise response features in non-severe COPD complicated with cardiac AD and determine associations between cardiac AD and pulmonary VV and ventilatory efficiency parameters.
Materials and methods
Study participants
We prospectively recruited outpatients with clinically stable COPD diagnosed at the China-Japan Friendship Hospital according to the global initiative for chronic obstructive lung disease (GOLD) guidelines [1]. All participants underwent medical interviews, pulmonary function tests (PFTs), chest CT, and CPET. Inclusion criteria were as follows: post-bronchodilator ratio between forced expiratory volume in 1 s and forced vital capacity (FEV1/FVC) < 70%, FEV1 > 50%; achieving maximal effort during the CPET recommended by the ATS/ACCP [21]. Exclusion criteria were as follows: (pulmonary hypertension) PH; left ventricular (LV) dysfunction; ischaemic heart disease; atrial fibrillation; valvular heart disease; cardiomyopathy; taking medications affecting HR; previous rehabilitation programmes.
The recruitment period was between July 2022 and July 2023. The study was approved by the institutional review board at the China-Japan Friendship Hospital (2022-KY-141), and written informed consent was obtained from all participants.
Procedures
PFT and CT acquisition
Initially, patients underwent assessments of demographic data, medical history, smoking exposure, and respiratory symptoms. PFTs and chest CTs were then performed. Spirometry, body plethysmography, and diffusing lung capacity for carbon monoxide (DLCO) measurements were performed using automated equipment (Jaeger Masterscreen, Germany). [22] All volumetric CT scan images were obtained at full inspiration in the supine position. CT images were reconstructed with a slice thickness of 1 mm and a 1 mm increment, with a resolution of 512 × 512 mm, using a 320-slice CT (Genesis, Canon Medical System, Japan). Next, quantitative CT image analysis was performed using the FACT-Digital LungTM software (DeXin, Xi’an, China). Each pulmonary vessel tree was segmented, generating a vascular volume relative to the entire lung. Emphysema was quantified on full inspiration using low-attenuation areas of the lung (<-950 Hounsfield units).
CPET
On the second day of assessments, patients were instructed not to take inhaled bronchodilators (β2 agonists and anticholinergics), consume alcohol or stimulant drinks, or engage in vigorous exercise for 24 h. Standardised CPETs were conducted using an electromagnetically braked cycle ergometer (Jaeger Masterscreen, Germany), following the manufacturer’s guidelines [23]. A continuous ramp protocol was applied. After 2 min of unloaded pedalling (rest phase-0 W), a 3-min warm-up phase (20 W) followed. The test phase included 20 W/2 min load increments. Patients were instructed to pedal with 60–65 rotations per minute. Patients’ effort was maximal if two or more of the following criteria emerged: predicted maximal HR is achieved; predicted maximal oxygen uptake and/or a plateau is observed; RER > 1.10.
Measurements included standard gas exchange, breathing pattern parameters, HR (12-lead electrocardiography), and O2 saturation (pulse oximetry, SpO2). V-slope and ventilatory equivalent methods were used to determine the anaerobic threshold (AT). [23] Peak VO2 and RER were reported as the average values determined over the last 30 s of the CPET. O2 pulse during the peak exercise was calculated as VO2/HR. The nadir ventilatory equivalent for carbon dioxide (VE/VCO2) was defined as the lowest 30-second average data point observed during a CPET. The nadir VE/VCO2 has been used as an indicator of ventilatory efficiency because of its prognostic value and clinical utility [19, 20].
Endpoint analysis
Abnormal HR responses are identified by both CI and abnormal heart rate recovery (HRR). Chronotropic response (CR) is defined as [(peak HR–rest HR) / (age-predicted maximal HR–rest HR)]. CI would be diagnosed if CR failed to reach 80%. Abnormal HRR is defined as an HR that declines ≤ 12 beats/min in the first minute after exercise. Age-predicted maximum HR was obtained using an established formula (220-age).
Statistical analysis
The normality of all data was tested using the Shapiro–Wilk test. Continuous variables are presented as mean ± standard deviation (SD) or median and interquartile range. Unpaired Student’s t-tests or Mann–Whitney U tests were performed for between-group (GOLD 1 and 2; CI and no CI; normal and abnormal HRR) comparisons of continuous variables. Categorical variables are presented as proportions. The X2 test was used to compare the frequencies of the categorical variables. Multivariate logistic regression analyses were used to determine the odds ratios between selected PFT, CT, and CPET parameters (independent variables) and CI or abnormal HRR (dependent variables) (online supplement). For multivariate regression, a forward likelihood ratio model was used with stepwise entry and removal criteria of 0.05 and 0.10, respectively. Continuous variables (e.g., PFT, CT, and CPET parameters) were converted to categorical forms, with the cut-off point set at the median of all samples.
Statistical significance was set at p < 0.05. All statistical analyses were performed using the Statistical Package for the Social Sciences version 26 (IBM).
Patient and public involvement
Patients and the public were not involved in the design or conduct of this study.
Results
Study population
Out of sixty-five recruited patients, forty-nine were finally included (Fig. S1). Included patients were predominantly men (79.6%) and had a mean (SD) age of 62 (9) years. 26 patients were of GOLD 1 with a mean (SD) FEV1 of 94.9% (14.5%), while 23 were of GOLD 2 with a mean (SD) FEV1 of 67.2% (9.0%). There were no between-group differences in age, sex, body mass index, number of smokers, or presence of diabetes or hypertension between GOLD 1 and GOLD 2. The CT-derived emphysema severity and VV were not different. During CPET, GOLD 2 had lower exercise capacity (VO2peak), breath reserve, and ventilatory efficiency than GOLD 1 (Table 1). GOLD 1 subjects had a mean (SD) VO2peak of 88.7% (18.8%), while GOLD 2 subjects had a mean (SD) VO2peak of 80.5% (13.5%).
Demographic, PFT, CT, CPET parameters, and CI
Table 2 describes demographic, lung function, lung imaging, and cardiopulmonary exercise response variable differences among patients with and without CI. Participants who developed CI had a lower resting DLCO, greater lung hyperinflation, and blood VV abnormalities. Regarding CPET parameters, in addition to a significantly lower VO2peak and VO2 at AT, those with CI had significantly higher nadir VE/VCO2, indicating reduced ventilatory efficiency.
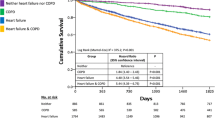
A multivariate logistic regression analysis included variables that exhibited a significant difference in univariate analysis or were consistently related to automatic cardiac function in previous literature [2, 3, 6, 7, 11, 15], with testing for multicollinearity (online supplement). Only IC, VV, and nadir VE/VCO2 independently predicted CI after adjustments (Fig. 1).
The relationship between PFT, CT, CPET parameters and CI. Adjusted OR (with upper and lower 95% CIs) for likelihood of having lung function, imaging and/or cardiopulmonary exercise response impairment in participants with CI compared with those without CI. Abbreviations PFT = pulmonary function test; CT = computed tomography; CPET = cardiopulmonary exercise test; CI = chronotropic incompetence; OR = odds ratio; CI = confidence interval; IC = inspiratory capacity; VV = vascular volume; VE/VCO2 = ventilatory equivalent for carbon dioxide
Demographic, PFT, CT, CPET parameters, and abnormal HRR
Table 3 shows differences between patients with normal and abnormal HRR. Those with delayed HRR had an older age, more severe airflow limitations, gas exchange abnormalities, reduced lung vessel beds, and greater lung emphysema. During CPET, in addition to significantly lower VO2peak and VO2 at AT, patients with delayed HRR had statistically significant lower ventilatory efficiency and breath reserve.
The logistic regression model revealed lung vessel volume and nadir VE/VCO2 as independent predictors for delayed HRR (Fig. 2).
The relationship between PFT, CT, CPET parameters and delayed HRR. Adjusted OR (with upper and lower 95% CIs) for likelihood of having lung function, imaging and/or cardiopulmonary exercise response impairment in participants with delayed HRR compared with those with normal HRR. Abbreviations PFT = pulmonary function test; CT = computed tomography; CPET = cardiopulmonary exercise test; HRR = heart rate recovery; OR = odds ratio; CI = confidence interval; VV = vascular volume; VE/VCO2 = ventilatory equivalent for carbon dioxide;
Discussion
Our main findings were as follows: (1) in COPD, cardiac AD identified by CI and delayed HRR was independently associated with CT indices of pulmonary VV abnormalities; (2) cardiac AD was independently related to high nadir VE/VCO2 during the CPET.
After adjusting for relevant factors in our study, those with CI or delayed HRR had significantly reduced CT-derived VV, a valid index of small vessel loss [17, 18]. A high nadir VE/VCO2 ratio, which indicates increased VD/VT during exercise, was also confirmed as an independent predictor of abnormal HR responses [19, 20, 24]. Thus, our results suggest that patients with cardiac AD are more likely to have reduced pulmonary blood perfusion, which is theoretically in line with the negative effects of pulmonary vascular loss on cardiac structure and function. It is routinely assumed that AD is secondary to chronic sympathetic system overactivation. Pulmonary vascular remodeling could lead to higher left ventricular (LV) mass and LV diastolic dysfunction, then increase sympathetic system overactivation [16, 25,26,27].
Our study identifies the susceptibility to cardiac AD of one specific subset of patients, the so-called “pulmonary vascular phenotype”. In most COPD patients, loss of the pulmonary vascular bed can be attributed to distal airway damage and alveolar destruction. However, in some patients with mild-to-moderate COPD, vascular pruning and capillary hypoperfusion can exist in both emphysematous and non-emphysematous lung regions, especially in those who are ever-smokers [28,29,30,31,32]. In this subset of individuals, endothelial injury and pulmonary vascular remodelling may occur before developing airflow obstruction or emphysema, the so-called “pulmonary vascular phenotype” [33]. Despite poorer prognosis due to early pulmonary vascular damage [34], this phenotype has been overlooked in most researchand clinical practice. By supplementing cardiac performance for this subset, our finding have stressed that they may be exposed to a higher risk of cardiac dysfunction, appealing more clinical attention and directed research. In addition, pulmonary circulation abnormalities in COPD require better screening tools, with previous studies only focusing on patients with severe pulmonary vascular disease. However, a much larger group with mild disease only exhibited a steep increase in pulmonary arterial pressure during exercise [33, 35]. Based on our findings, abnormal HR responses during exercise tests (e.g., field walking tests and CPET) have the potential to be a non-invasive, accessible, effective screening tool for pulmonary circulation abnormalities. The therapy of the pulmonary vascular phenotype of COPD is challenging. Although optimized treatment of the underlying lung disease is suggested, there are no data to show that this optimized treatment improves PH. On the basis of sentinel studies, long-term oxygen therapy may reduce the progression of PH. As for PAH drugs, we need prospective studies providing evidence that these patients do profit from such therapy before it can be recommended [33].
Cardiac AD exists regardless of the severity of COPD and has predictive value for quality of life and mortality; we suggest physicians pay attention to it during clinical management [36,37,38]. These patients may not experience sufficient symptom relief from typical COPD treatment. Thus, prospective studies should determine whether patients benefit from rehabilitative interventions, such as exercise training, which have been shown to be effective in those with CVDs [33, 35, 39].
The relationship between AD and FEV1 remains controversial. For example, Chicks demonstrated that delayed HRR was independent of FEV1, whereas Hulo reported a higher prevalence of CI as FEV1 decreased [40, 41]. In addition, Cherneva et al. reported a relationship between cardiac AD and lung hyperinflation [16]. Our results showed that these variables could not separate the two groups in multivariate analysis. However, we also observed that delayed HRR was independently associated with a reduced FEF50–75%, which is also closely related to airflow limitation. The controversies regarding the association between AD and different pulmonary function parameters are probably due to different study designs and protocol performances that should be determined in a larger population-based sample.
Limitations
This study had limitations. First, a selection bias may have occurred because our analysis only included mild-moderate patients who were able to achieve their maximal exercise capacity; however, HR responses during or after an incremental maximal exercise test would underestimate the cardiac function of COPD patients who stop tests earlier because of severe ventilatory limitation. HR variability may be a more precise measure of cardiac AD in severe COPD. Nonetheless, for mild-moderate COPD, the literature supports using HR responses to exercise as the biomarker of autonomic function to easily predict clinical outcomes in the clinical setting. Second, the relatively small sample size and multiple tests may have led to false commission or the omission of results (type I/II error). Larger population-based cohorts are needed to confirm the conclusion. Additionally, it would be more precise to include dynamic inspiratory capacity (ICdyn) as an adjusted factor when exploring the correlation between low pulmonary vascular volume and cardiac AD. It is our limitation not to serially measure ICdyn. However, several measures were taken to make our findings more robust: static hyperinflation was assessed by IC at rest and quantified emphysema, which correlates closely to DH; both emphysema and IC were included in the multivariate logistic regression model. Finally, with limited resources, we were unable to evaluate brain natriuretic peptide level and echocardiography for each patient. However, considering that PH and LV dysfunction affect cardiac automatic function, we did taken many other measures to exclude these patients, such as asking medical history, collecting medical records and performing chest CT. To confirm our results, we would also carry out research including essential accessory examinations in the future.
Conclusion
We are the first to report that cardiac AD is linked to reduced pulmonary VV and low ventilatory efficiency in COPD based on chest CT, spirometry, and CPET characterization. Impaired VV and ventilatory efficiency pointed to reduced pulmonary blood perfusion, possibly affecting cardiac fulfilment.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to patients’ personal information but are available from the corresponding author upon reasonable request.
References
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for Prevention, Diagnosis and Management of COPD: 2023 Report
Vivekananthan DP, et al. Heart rate recovery after exercise is a predictor of mortality, independent of the angiographic severity of coronary disease. J Am Coll Cardiol. 2003;42(5):831–8.
Elhendy A, et al. Prognostic significance of impairment of heart rate response to exercise: impact of left ventricular function and myocardial ischemia. J Am Coll Cardiol. 2003;42(5):823–30.
Lahiri MK, Kannankeril PJ, Goldberger JJ. Assessment of autonomic function in cardiovascular disease: physiological basis and prognostic implications. J Am Coll Cardiol. 2008;51(18):1725–33.
Chaudhry S, et al. Abnormal heart-rate response during cardiopulmonary exercise testing identifies cardiac dysfunction in symptomatic patients with non-obstructive coronary artery disease. Int J Cardiol. 2017;228:114–21.
Laforgia P, et al. Exercise chronotropic incompetence phenotypes the level of cardiovascular risk and exercise gas exchange impairment in the general population. An analysis of the Euro-EX prevention trial. Eur J Prev Cardiol. 2020;27(5):526–35.
Lauer MS, et al. Association of cigarette smoking with chronotropic incompetence and prognosis in the Framingham Heart Study. Circulation. 1997;96(3):897–903.
Wang H, et al. Attenuated heart rate recovery in children and adolescents with obstructive sleep apnea syndrome. Pediatr Res. 2021;89(4):900–4.
Ramos RP, et al. Heart rate recovery in pulmonary arterial hypertension: relationship with exercise capacity and prognosis. Am Heart J. 2012;163(4):580–8.
Spiesshoefer J, et al. Sympathetic and vagal nerve activity in COPD: pathophysiology, presumed determinants and underappreciated therapeutic potential. Front Physiol. 2022;13:919422.
Mohammed J, et al. Evidence for autonomic function and its influencing factors in subjects with COPD: a systematic review. Respir Care. 2015;60(12):1841–51.
Andreas S, et al. Neurohumoral activation as a link to systemic manifestations of chronic lung disease. Chest. 2005;128(5):3618–24.
Washko GR, et al. Arterial vascular pruning, right ventricular size, and clinical outcomes in Chronic Obstructive Pulmonary Disease. A longitudinal observational study. Am J Respir Crit Care Med. 2019;200(4):454–61.
Pelà G, et al. Left ventricular structure and remodeling in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2016;11:1015–22.
Mayr AK, et al. Impaired spontaneous Baroreceptor Reflex sensitivity in patients with COPD compared to healthy controls: the role of lung hyperinflation. Front Med (Lausanne). 2021;8:791410.
Cherneva RV, Youroukova VM, Cherneva ZV. Dynamic hyperinflation, chronotropic intolerance and abnormal heart rate recovery in non-severe chronic obstructive pulmonary disease patients-reflections in the mirror. Pulmonology. 2022;28(6):440–8.
Koo MC et al. Quantitative computed tomography and visual emphysema scores: association with lung function decline. ERJ Open Res, 2023. 9(2).
Rahaghi FN et al. Pulmonary vascular density: comparison of findings on computed tomography imaging with histology. Eur Respir J, 2019. 54(2).
Phillips DB, et al. Impaired ventilatory efficiency, Dyspnea, and Exercise Intolerance in Chronic Obstructive Pulmonary Disease: results from the CanCOLD Study. Am J Respir Crit Care Med. 2022;205(12):1391–402.
Elbehairy AF, et al. Pulmonary Gas Exchange abnormalities in mild chronic obstructive Pulmonary Disease. Implications for Dyspnea and Exercise Intolerance. Am J Respir Crit Care Med. 2015;191(12):1384–94.
American Thoracic S. American College of Chest, ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2003;167(2):211–77.
Graham BL, et al. Standardization of Spirometry 2019 Update. An official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med. 2019;200(8):e70–88.
Balady GJ, et al. Clinician’s guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(2):191–225.
Teopompi E, et al. Ventilatory response to carbon dioxide output in subjects with congestive heart failure and in patients with COPD with comparable exercise capacity. Respir Care. 2014;59(7):1034–41.
Aaron CP, et al. Pulmonary vascular volume, impaired left ventricular filling and dyspnea: the MESA Lung Study. PLoS ONE. 2017;12(4):e0176180.
Zweerink A, et al. Chronotropic incompetence in Chronic Heart failure. Circ Heart Fail. 2018;11(8):e004969.
Duus LS et al. COPD: pulmonary vascular volume associated with cardiac structure and function. Int J Cardiovasc Imaging, 2023.
Hueper K, et al. Pulmonary Microvascular Blood Flow in mild chronic obstructive Pulmonary Disease and Emphysema. The MESA COPD Study. Am J Respir Crit Care Med. 2015;192(5):570–80.
Santos S, et al. Characterization of pulmonary vascular remodelling in smokers and patients with mild COPD. Eur Respir J. 2002;19(4):632–8.
Pistenmaa CL, et al. Pulmonary arterial pruning and longitudinal change in percent emphysema and lung function: the genetic epidemiology of COPD Study. Chest. 2021;160(2):470–80.
Estépar RS, et al. Computed tomographic measures of pulmonary vascular morphology in smokers and their clinical implications. Am J Respir Crit Care Med. 2013;188(2):231–9.
Elbehairy AF, et al. Pulmonary vascular volume by Quantitative CT in dyspneic smokers with minor Emphysema. Copd. 2023;20(1):135–43.
Kovacs G, et al. Pulmonary vascular involvement in Chronic Obstructive Pulmonary Disease. Is there a pulmonary vascular phenotype? Am J Respir Crit Care Med. 2018;198(8):1000–11.
Hermann EA, et al. Pulmonary blood volume among older adults in the community: the MESA Lung Study. Circ Cardiovasc Imaging. 2022;15(8):e014380.
Kessler R, et al. Natural history of pulmonary hypertension in a series of 131 patients with chronic obstructive lung disease. Am J Respir Crit Care Med. 2001;164(2):219–24.
Delgado-Ortiz L, et al. Physical activity and cardiac autonomic dysfunction in patients with chronic obstructive pulmonary disease: a cross-sectional analysis. Ann Phys Rehabil Med. 2022;65(3):101501.
Leite MR, et al. Correlation between heart rate variability indexes and aerobic physiological variables in patients with COPD. Respirology. 2015;20(2):273–8.
Mazzuco A, et al. Are heart rate dynamics in the transition from rest to submaximal exercise related to maximal cardiorespiratory responses in COPD? Braz J Phys Ther. 2017;21(4):251–8.
Besnier F, et al. Exercise training-induced modification in autonomic nervous system: an update for cardiac patients. Ann Phys Rehabil Med. 2017;60(1):27–35.
Chick TW, et al. Recovery of gas exchange variables and heart rate after maximal exercise in COPD. Chest. 1990;97(2):276–9.
Hulo S, et al. Chronotropic incompetence can limit exercise tolerance in COPD patients with lung hyperinflation. Int J Chron Obstruct Pulmon Dis. 2016;11:2553–61.
Acknowledgements
Not applicable.
Funding
This research was funded by the Chinese Academy of Medical Sciences Innovation Fund for Medical Sciences (CIFMS) (2021-I2M-1-049).
Author information
Authors and Affiliations
Contributions
M. Shi and S. Qumu conceived and designed the study, drafted and made critical revisions to the manuscript. S. Wang, Y.Peng, L. Yang, K. Huang assisted in development of the protocol and revision of the manuscript. R. He, F. Dong, H. Niu, were involved in implementation and management of the programme. T. Yang and C. Wang designed the program and supervised the work. All authors have read and approved the final manuscript to be published.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the institutional review board at the China-Japan Friendship Hospital (2022-KY-141). Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shi, M., Qumu, S., Wang, S. et al. Abnormal heart rate responses to exercise in non-severe COPD: relationship with pulmonary vascular volume and ventilatory efficiency. BMC Pulm Med 24, 183 (2024). https://doi.org/10.1186/s12890-024-03003-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03003-y