Abstract
Background
Pulmonary hypertension (PH) is a frequent complication in COPD and it is associated with decreased exercise capacity and poor prognosis. We hypothesized that even in COPD patients without significant PH at rest, abnormal pulmonary hemodynamics during exercise affect exercise capacity.
Methods
Consecutive COPD patients with clinically indicated right heart catheterization and resting mean pulmonary arterial pressure (mPAP) < 25 mmHg and age- and sex-matched controls with the same limits of pulmonary hemodynamics but no chronic lung disease who underwent clinical work-up including invasive hemodynamic assessment during exercise, were retrospectively analyzed. Chi-square tests were used to evaluate differences between groups for categorical data and Fisher’s exact test or Mann–Whitney-U-tests for continuous variables. Associations were analyzed with Spearman rank correlation tests.
Results
We included n = 26 COPD patients (female/male: 16/10, 66 ± 11 yr, FEV1: 56 ± 25%predicted) and n = 26 matched controls (FEV1: 96 ± 22%predicted). At rest, COPD patients presented with slightly increased mPAP (21 (18–23) vs. 17 (14–20) mmHg, p = 0.022), and pulmonary vascular resistance (PVR) [2.5 (1.9–3.0) vs. 1.9 (1.5–2.4) WU, p = 0.020] as compared to controls. During exercise, COPD patients reached significantly higher mPAP [47 (40–52) vs. 38 (32–44) mmHg, p = 0.015] and PVR [3.1 (2.2–3.7) vs. 1.7 (1.1–2.9) WU, p = 0.028] values despite lower peak exercise level [50 (50–75) vs. 100 (75–125) Watt, p = 0.002]. The mPAP/cardiac output slope was increased in COPD vs. controls [6.9 (5.5–10.9) vs. 3.7 (2.4–7.4) mmHg/L/min, p = 0.007] and negatively correlated with both peak oxygen uptake (r = − 0.46, p = 0.007) and 6-min walk distance (r = − 0.46, p = 0.001).
Conclusion
Even in the absence of significant PH at rest, COPD patients reveal characteristic abnormalities in pulmonary hemodynamics during exercise, which may represent an important exercise-limiting factor.
Similar content being viewed by others
Introduction
Airway obstruction and loss of functional pulmonary parenchyma are important features of chronic obstructive pulmonary disease (COPD), leading to impaired exercise capacity and survival [1]. In addition, pulmonary hypertension (PH) may complicate the course of COPD and contribute to poor prognosis [2,3,4,5]. The overall prevalence of a mean PAP ≥ 25 mmHg in COPD is estimated to be around 10% [6]. Although severe PH is rare, mild to moderate forms of pulmonary vascular disease (PVD) are quite frequent [7, 8]. Despite normal or mildly elevated pulmonary arterial pressures at rest, hemodynamic response to exercise may be abnormal in these patients, which could substantially contribute to their symptoms and impaired exercise capacity [5, 9, 10]. In recent years, our understanding of pulmonary hemodynamics during exercise improved and prognostically relevant variables have been identified. Out of these, the mPAP/CO-slope may be considered as most robust parameter to characterize abnormal pulmonary hemodynamics during exercise [11,12,13]. However, there are still very limited data available on the characteristic changes in pulmonary hemodynamics during exercise in COPD and on the clinical relevance of these changes.
In this study, we aimed to investigate pulmonary hemodynamics and right ventricular function during exercise in COPD patients with normal or slightly elevated mean pulmonary arterial pressure (mPAP) at rest and to compare them to age- and sex-matched controls. We hypothesized that patients with COPD may show an abnormal pulmonary hemodynamic response to exercise and that this is associated with reduced exercise capacity.
Methods
Study design, patients and ethics
All consecutive COPD subjects who underwent clinically indicated right heart catheterization (RHC) for suspected PH at our clinic between 2005 and 2018 were carefully clinically evaluated and the complete dataset resulting from these investigations was included into a local database, the GRAz Pulmonary Hypertension In COPD (GRAPHIC) registry [2]. For this retrospective analysis, all patients with resting mPAP ≥ 25 mmHg who underwent an exercise test with indwelling catheter, were included. The indication for resting RHC followed international guidelines [14]. Patients who turned out to have resting mPAP < 25 mmHg at RHC underwent exercise-RHC to gain additional information regarding mechanisms of dyspnea and exercise limitation. During their clinical work-up, patients underwent pulmonary function test, transthoracic echocardiography, six-minute-walk distance (6MWD), cardiopulmonary exercise testing (CPET), blood-gas analysis and laboratory testing. The diagnosis of COPD and the severity of airflow limitation were established according to the GOLD recommendations [15] by two independent respiratory physicians. If more than one RHC was performed during the observation period, we included only the first investigation.
The control group consisted of age- and sex-matched patients who were admitted to our clinic due to suspected PH or unexplained dyspnea during the same time period, but had no chronic lung disease, no obstructive or restrictive changes (FEV1/FVC > 70%, TLC > 80%), a peak oxygen uptake (VO2) ≥ 80% predicted and a mPAP < 25 mmHg and pulmonary arterial wedge pressure (PAWP) ≤ 15 mmHg at RHC at rest. Controls underwent the same diagnostic procedures as the COPD patients. The study protocol conformed to the Declaration of Helsinki and was approved by the Ethics Committee of the Medical University of Graz (EK 32–352 ex 19–20).
Assessment of resting and exercise hemodynamics
Patients underwent routine resting RHC in the supine position using a Swan-Ganz catheter as previously described [16]. The Swan-Ganz catheter was percutaneously inserted via a jugular vein under local anesthesia. The zero reference level was set at the mid-thoracic level [17, 18]. Symptom-limited exercise RHC was performed on a cycle-ergometer with stepwise (25 Watt) increasing workloads every 2 min. Pulmonary pressure readings of systolic, diastolic and mean pulmonary arterial pressure (sPAP, dPAP, mPAP), PAWP and right atrial pressure (RAP) were performed at each exercise level and were averaged over a minimum of three respiratory cycles. Cardiac output (CO) was determined by thermodilution. Blood gas analysis was performed at rest and during peak exercise by an ABL-800-Flex blood gas analyzer (Drott®). Pulmonary vascular resistance (PVR) was calculated as (mPAP-PAWP)/CO, total pulmonary resistance (TPR) was determined as mPAP/CO and transpulmonary pressure gradient (TPG) as mPAP-PAWP. Pressure/flow slopes were calculated from the differences between peak exercise and resting mPAP (or PAWP, RAP or TPG) and the differences between peak exercise and resting CO [12, 19]. Pulmonary vascular compliance (PVC) was calculated by stroke volume (SV)/(sPAP–dPAP) and pulmonary artery (PA) stiffness index by 1/PVC per body surface area (BSA) [20, 21]. Of note, the pulmonary vascular compliance (PVC) represents a measure of pulsatile afterload of the right ventricle. PVC has been shown to be of prognostic relevance in PH and decreased values may help to identify early forms of pulmonary vascular disease [20, 22,23,24,25,26]. Pulmonary artery stiffness is related to PH and COPD severity and correlates with mPAP and PVR during exercise [27, 28].
For assessment of right ventricular function during exercise, we calculated the right ventricular output ratio RVOR = CImax-rest/CIrest, which shows the ability of the subject to increase cardiac output during exercise and is associated with prognosis in pulmonary hypertension patients [29,30,31].
Statistical analysis
Normally distributed variables were represented as mean ± SD and not normally distributed variables as median and interquartile range for continuous data. Categorical data are presented as absolute and relative numbers and between the groups compared using chi-square tests. Differences between the groups in continuous variables were analyzed using Mann–Whitney-U-test for nonparametric variables. Associations were analyzed with Spearman rank correlation coefficient. Significance level was defined as p-value < 0.05. For statistical analysis, IBM SPSS Statistics 26 was used.
Results
Clinical and demographic characteristics
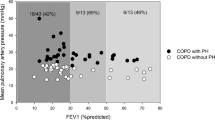
A total of 142 COPD patients who underwent RHC between 2005 and 2018 were identified in our database. Out of these, in n = 115, only resting RHC was performed and in 27 subjects, an additional symptom-limited exercise RHC was performed. One patient was excluded because resting mPAP was ≥ 25 mmHg (29 mmHg) at rest. The remaining 26 patients were matched according to age- and sexto controls (Fig. 1). Table 1 shows the baseline characteristics of the patients. There were no significant clinical differences between the two groups, except for lung function parameters and 6MWD. For comorbidities see Additional file 1: Table S1.
Pulmonary hemodynamics at rest
The hemodynamic data derived from resting RHC are provided in Table 2. Compared to the control group, COPD patients had slightly elevated mPAP [21 (18–23) mmHg vs. 17 (14–20) mmHg, p = 0.022], PVR [2.5 (1.9–3.0) WU vs. 1.9 (1.5–2.4) WU, p = 0.035] and TPR [4.3 (3.8–5.7) WU vs. 3.5 (2.7–4.4) WU, p = 0.007], while there were no significant differences in PAWP, RAP and CO as well as in pulmonary arterial compliance and stiffness. Out of the resting hemodynamic parameters only mPAP and TPR were significantly associated with peak VO2 and none of the assessed parameters was associated with 6MWD.
Pulmonary hemodynamics during exercise
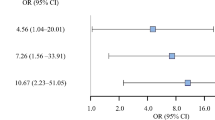
During exercise, COPD patients, as compared to controls, reached significantly lower maximal exercise levels [50 (50–75) Watt vs. 100 (75–125) Watt, p = 0.002], and had impaired peak oxygen uptake [peak VO2 64 (48–80) %predicted vs. 97 (87–102) %predicted, p < 0.001] and 6MWD [360 (289–441) m vs. 449 (329–493) m, p = 0.033)]. Resting hemodynamic differences between COPD and controls became more pronounced during exercise (Table 2). COPD patients had steeper mPAP/CO [6.9 (5.0–10.9) mmHg/L/min vs. 3.7 (2.4–7.4) mmHg/L/min, p = 0.007], RAP/CO [2.3 (1.3–4.2) mmHg/L/min vs. 1.2 (0.5–2.1) mmHg/L/min, p = 0.025], TPG/CO [3.5 (1.6–4.5) mmHg/L/min vs. 1.6 (0.9–3.5) mmHg/L/min, p = 0.048] and PAWP/CO-slopes [COPD: 2.9 (1.9–6.4) vs. controls: 1.8 (1.3–4.2) mmHg, p = 0.051] as compared to controls (Fig. 2). RVOR was significantly decreased in COPD patients as compared to controls [0.9 (0.5–1.2) vs. 1.3 (0.7–1.8), p = 0.020].
Association between exercise capacity and pulmonary hemodynamics
Several parameters of exercise hemodynamics were associated with peak VO2 and 6MWD (Table 3 and Fig. 3). The mPAP/CO slope, PVC at peak exercise, and RVOR showed the strongest correlations with both peak VO2 and 6MWD.
The relationship between cardiopulmonary exercise testing derived peak oxygen uptake (Peak VO2) and 6-min walk test (6MWT) with mean pulmonary arterial pressure/cardiac output slope (mPAP/CO slope (A, B), pulmonary vascular compliance (PVC) (C, D) and right ventricular output reserve (RVOR) (E, F). Red dots represent COPD patients, green dots controls
Discussion
In this study, we show that COPD patients, even without significant pulmonary hypertension at rest, present with characteristic changes in pulmonary hemodynamics and right ventricular function during exercise as compared to age- and sex-matched controls without chronic lung disease. The significant association between these changes and exercise capacity highlights the clinical relevance of these findings.
Pulmonary hemodynamics at rest and exercise in COPD
According to the available studies, elevation of resting mPAP in COPD patients is associated with clinical worsening and progression to PH [32, 33], however, the clinical relevance of exercise hemodynamics, which may help to reveal the pathophysiology of exercise dyspnea, has only rarely been investigated in these patients. A recent study, providing new insights into specific characteristics of exercise pulmonary hemodynamics in COPD, described a strong increase in mPAP on effort [10]. In addition, a small previous study in COPD patients undergoing lung volume reduction surgery, revealed that the wall thickness of pulmonary vessels was not related to mPAP at rest, but was strongly correlated with mPAP during exercise (r = 0.721, p = 0.02) and with the change in mPAP from rest to exercise (r = 0.899, p = 0.0004) [34]. Our results complement these findings, because we provide a characterization of pulmonary hemodynamics during exercise in COPD and show significant associations between changes in exercise hemodynamics and decreased exercise capacity, suggesting potential mechanisms of exercise limitation in these patients.
Pulmonary pressure-cardiac output slopes
There is growing evidence for the importance of mPAP/CO slope in exercise testing for predicting clinical outcomes [11, 13]. According to recent studies, healthy subjects have mPAP/CO slopes of 1.6 to 3.3 mmHg/L/min, whereas patients with PVD typically show values > 3 mmHg/L/min [11, 13]. A mPAP/CO slope > 3 mmHg/L/min was independently associated with hospitalization and survival in patients with chronic exertional dyspnea and preserved ejection fraction and a mPAP/CO slope ≥ 2.9 mmHg/L/min was significantly correlated with age-adjusted mortality in systemic sclerosis [13, 35]. Moreover, the predictive value of this slope is independent from pulmonary resting hemodynamics [36]. The mPAP/CO slope of our COPD cohort was increased to 6.9 mmHg/L/min, indicating a strongly abnormal pulmonary hemodynamic response to exercise. In addition, peak VO2 was significantly negatively associated with the mPAP/CO-slope, suggesting that pathological exercise hemodynamics may significantly contribute to exercise limitation. This might explain the exercise induced dyspnea of these patients. In order to further explore the underlying reason of mPAP elevation at exercise, we assessed the changes in TPG, PAWP and RAP during exercise. We found that all pressure/CO slopes were steeper in COPD patients as compared to controls, suggesting that both pre- and postcapillary factors and an additional increase in intrathoracic pressure may significantly contribute to abnormal pulmonary hemodynamics during exercise in COPD.
Impact of right ventricular function
Apart from the involvement of pulmonary vessels, also changes in right ventricular function and its adaptation to increased afterload may be of prognostic importance and even early signs of RV failure may be associated with poor outcome [31, 37,38,39,40]. RVOR, among other factors, depends on the ability of the right ventricle to increase cardiac output during exercise. RVOR was significantly reduced in COPD patients as compared to controls (0.9 L/min/m2 vs. 1.3 L/min/m2, p = 0.02), which might suggest a limited right ventricular reserve in COPD patients. In addition, RVOR was significantly associated with peak VO2 and 6MWD, suggesting an important contribution to exercise limitation in COPD. Of note, RV function at rest as characterized by echocardiography (tricuspid annular plane systolic excursion), did not differ between COPD patients and controls.
Limitations
The retrospective nature and the relatively low number of included subjects are obvious limitations of the current study. This limitation may at least partly be compensated by the thorough invasive hemodynamic characterization by an experienced clinical team. The relatively small number of included patients did not allow to perform multivariate analysis and to investigate mortality as an endpoint. Nevertheless, the clear associations with exercise capacity underline the clinical relevance of pulmonary hemodynamics during exercise in COPD. Another limitation is the absence of a truly healthy control group which was not available due to ethical reasons along with the invasive nature of the investigation.
Conclusions
Even in the absence of more than mild pulmonary hypertension, COPD patients show characteristic abnormalities in pulmonary hemodynamics and right ventricular function during exercise, which may significantly contribute to their exercise limitation.
Availability of data and materials
Not applicable.
Abbreviations
- 6MWD:
-
6-Minute walk distance
- BMI:
-
Body mass index
- BSA:
-
Body surface area
- CI:
-
Cardiac index
- CO:
-
Cardiac output
- COPD:
-
Chronic obstructive pulmonary disease
- CPET:
-
Cardiopulmonary exercise testing
- DLCO:
-
Diffusing capacity of lung for carbon monoxide
- DLCOcVA:
-
Diffusing capacity of lung for carbon monoxide for alveolar volume corrected for hemoglobin
- dPAP:
-
Diastolic pulmonary arterial pressure
- FEV1 :
-
Forced expiratory volume in the first record of expiration
- FVC:
-
Forced vital capacity
- Hb:
-
Hemoglobin
- mPAP:
-
Mean pulmonary arterial pressure
- NtproBNP:
-
N-terminal pro-brain natriuretic peptide
- PA:
-
Pulmonary artery
- PAWP:
-
Pulmonary arterial wedge pressure
- PH:
-
Pulmonary hypertension
- PVC:
-
Pulmonary vascular compliance
- PVR:
-
Pulmonary vascular resistance
- RAP:
-
Right atrial pressure
- RHC:
-
Right heart catheterization
- RVOR:
-
Right ventricular output ratio
- sPAP:
-
Systolic pulmonary arterial pressure
- SV:
-
Stroke volume
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TLC:
-
Total lung capacity
- TPG:
-
Transpulmonary pressure gradient
- TPR:
-
Total pulmonary resistance
- VO2:
-
Oxygen uptake
- WHO-FC:
-
World health organization functional class
- WU:
-
Wood units
References
Halpin DMG, Criner GJ, Papi A, Singh D, Anzueto A, Martinez FJ, et al. Global initiative for the diagnosis, management, and prevention of chronic obstructive lung disease. The 2020 GOLD science committee report on COVID-19 and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2021;203:24–36. https://doi.org/10.1164/rccm.202009-3533SO.
Kovacs G, Avian A, Bachmaier G, Troester N, Tornyos A, Douschan P, et al. Severe pulmonary hypertension in COPD—impact on survival and diagnostic approach. Chest. 2022;S0012–3692(22):00192–201. https://doi.org/10.1016/j.chest.2022.01.031.
Nathan SD, Barbera JA, Gaine SP, Harari S, Martinez FJ, Olschewski H, et al. Pulmonary hypertension in chronic lung disease and hypoxia. Eur Respir J. 2019. https://doi.org/10.1183/13993003.01914-2018.
Andersen KH, Iversen M, Kjaergaard J, Mortensen J, Nielsen-Kudsk JE, Bendstrup E, et al. Prevalence, predictors, and survival in pulmonary hypertension related to end-stage chronic obstructive pulmonary disease. J Heart Lung Transplant. 2012;31:373–80. https://doi.org/10.1016/j.healun.2011.11.020.
Portillo K, Torralba Y, Blanco I, Burgos F, Rodriguez-Roisin R, Rios J, et al. Pulmonary hemodynamic profile in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:1313–20. https://doi.org/10.2147/COPD.S78180.
Hoeper MM, Humbert M, Souza R, Idrees M, Kawut SM, Sliwa-Hahnle K, et al. A global view of pulmonary hypertension. Lancet Respir Med. 2016;4:306–22. https://doi.org/10.1016/S2213-2600(15)00543-3.
Kovacs G, Agusti A, Barberà JA, Celli B, Criner G, Humbert M, et al. Pulmonary vascular involvement in chronic obstructive. Pulmonary disease is there a pulmonary vascular phenotype? Am J Respir Crit Care Med. 2018;198:1000–11. https://doi.org/10.1164/rccm.201801-0095PP.
Nathan SD, Barbera JA, Gaine SP, Harari S, Martinez FJ, Olschewski H, et al. Pulmonary hypertension in chronic lung disease and hypoxia. Eur Respir J. 2019;53:1801914. https://doi.org/10.1183/13993003.01914-2018.
Burrows B, Kettel LJ, Niden AH, Rabinowitz M, Diener CF. Patterns of cardiovascular dysfunction in chronic obstructive lung disease. N Engl J Med. 1972;286:912–8. https://doi.org/10.1056/NEJM197204272861703.
Hilde JM, Skjørten I, Hansteen V, Melsom MN, Hisdal J, Humerfelt S, et al. Haemodynamic responses to exercise in patients with COPD. Eur Respir J. 2013;41:1031–41. https://doi.org/10.1183/09031936.00085612.
Zeder K, Banfi C, Steinrisser-Allex G, Maron BA, Humbert M, Lewis GD, et al. Diagnostic, prognostic and differential-diagnostic relevance of pulmonary hemodynamics during exercise—a systematic review. Eur Respir J. 2022. https://doi.org/10.1183/13993003.03181-2021.
Kovacs G, Herve P, Barbera JA, Chaouat A, Chemla D, Condliffe R, et al. An official European Respiratory Society statement: pulmonary haemodynamics during exercise. Eur Respir J. 2017. https://doi.org/10.1183/13993003.00578-2017.
Ho JE, Zern EK, Lau ES, Wooster L, Bailey CS, Cunningham T, et al. Exercise pulmonary hypertension predicts clinical outcomes in patients with dyspnea on effort. J Am Coll Cardiol. 2020;75:17–26. https://doi.org/10.1016/j.jacc.2019.10.048.
Galiè N, Humbert M, Vachiery J-L, Gibbs S, Lang I, Torbicki A, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS)Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J. 2015;46:903–75. https://doi.org/10.1183/13993003.01032-2015.
Singh D, Agusti A, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease: the GOLD science committee report 2019. Eur Respir J. 2019;53:1900164. https://doi.org/10.1183/13993003.00164-2019.
Kovacs G, Maier R, Aberer E, Brodmann M, Scheidl S, Hesse C, et al. Assessment of pulmonary arterial pressure during exercise in collagen vascular disease: echocardiography vs right-sided heart catheterization. Chest. 2010;138:270–8. https://doi.org/10.1378/chest.09-2099.
Kovacs G, Avian A, Pienn M, Naeije R, Olschewski H. Reading pulmonary vascular pressure tracings. How to handle the problems of zero leveling and respiratory swings. Am J Respir Crit Care Med. 2014;190:252–7. https://doi.org/10.1164/rccm.201402-0269PP.
Kovacs G, Avian A, Olschewski A, Olschewski H. Zero reference level for right heart catheterisation. Eur Respir J. 2013;42:1586–94. https://doi.org/10.1183/09031936.00050713.
Godinas L, Lau EM, Chemla D, Lador F, Savale L, Montani D, et al. Diagnostic concordance of different criteria for exercise pulmonary hypertension in subjects with normal resting pulmonary artery pressure. Eur Respir J. 2016;48:254–7. https://doi.org/10.1183/13993003.01678-2015.
Jain P, Rao S, Macdonald P, Kotlyar E, Jabbour A, Hayward C, et al. Diagnostic performance of pulmonary capacitance at rest and during exercise in idiopathic pulmonary arterial hypertension. Heart Lung Circ. 2019;28:289–94. https://doi.org/10.1016/j.hlc.2017.10.019.
Thenappan T, Prins KW, Pritzker MR, Scandurra J, Volmers K, Weir EK. The critical role of pulmonary arterial compliance in pulmonary hypertension. Ann Am Thorac Soc. 2016;13:276–84. https://doi.org/10.1513/AnnalsATS.201509-599FR.
Al-Naamani N, Preston IR, Paulus JK, Hill NS, Roberts KE. Pulmonary arterial capacitance is an important predictor of mortality in heart failure with a preserved ejection fraction. JACC Heart Fail. 2015;3:467–74. https://doi.org/10.1016/j.jchf.2015.01.013.
Pellegrini P, Rossi A, Pasotti M, Raineri C, Cicoira M, Bonapace S, et al. Prognostic relevance of pulmonary arterial compliance in patients with chronic heart failure. Chest. 2014;145:1064–70. https://doi.org/10.1378/chest.13-1510.
Nagel C, Marra AM, Benjamin N, Blank N, Cittadini A, Coghlan G, et al. Reduced right ventricular output reserve in patients with systemic sclerosis and mildly elevated pulmonary artery pressure. Arthritis Rheumatol. 2019;71:805–16. https://doi.org/10.1002/art.40814.
Kovacs G, Avian A, Tscherner M, Foris V, Bachmaier G, Olschewski A, et al. Characterization of patients with borderline pulmonary arterial pressure. Chest. 2014;146:1486–93. https://doi.org/10.1378/chest.14-0194.
Medrek SK, Kloefkorn C, Nguyen DTM, Graviss EA, Frost AE, Safdar Z. Longitudinal change in pulmonary arterial capacitance as an indicator of prognosis and response to therapy and in pulmonary arterial hypertension. Pulm Circ. 2017;7:399–408. https://doi.org/10.1177/2045893217698715.
Sanz J, Kariisa M, Dellegrottaglie S, Prat-González S, Garcia MJ, Fuster V, et al. Evaluation of pulmonary artery stiffness in pulmonary hypertension with cardiac magnetic resonance. JACC Cardiovasc Imaging. 2009;2:286–95. https://doi.org/10.1016/j.jcmg.2008.08.007.
Weir-McCall JR, Struthers AD, Lipworth BJ, Houston JG. The role of pulmonary arterial stiffness in COPD. Respir Med. 2015;109:1381–90. https://doi.org/10.1016/j.rmed.2015.06.005.
Blumberg FC, Arzt M, Lange T, Schroll S, Pfeifer M, Wensel R. Impact of right ventricular reserve on exercise capacity and survival in patients with pulmonary hypertension. Eur J Heart Fail. 2013;15:771–5. https://doi.org/10.1093/eurjhf/hft044.
Chaouat A, Sitbon O, Mercy M, Ponçot-Mongars R, Provencher S, Guillaumot A, et al. Prognostic value of exercise pulmonary haemodynamics in pulmonary arterial hypertension. Eur Respir J. 2014;44:704–13. https://doi.org/10.1183/09031936.00153613.
Grünig E, Tiede H, Enyimayew EO, Ehlken N, Seyfarth H-J, Bossone E, et al. Assessment and prognostic relevance of right ventricular contractile reserve in patients with severe pulmonary hypertension. Circulation. 2013;128:2005–15. https://doi.org/10.1161/CIRCULATIONAHA.113.001573.
Kessler R, Faller M, Fourgaut G, Mennecier B, Weitzenblum E. Predictive factors of hospitalization for acute exacerbation in a series of 64 patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;159:158–64. https://doi.org/10.1164/ajrccm.159.1.9803117.
Kessler R, Faller M, Weitzenblum E, Chaouat A, Aykut A, Ducoloné A, et al. “Natural history” of pulmonary hypertension in a series of 131 patients with chronic obstructive lung disease. Am J Respir Crit Care Med. 2001;164:219–24. https://doi.org/10.1164/ajrccm.164.2.2006129.
Kubo K, Ge RL, Koizumi T, Fujimoto K, Yamanda T, Haniuda M, et al. Pulmonary artery remodeling modifies pulmonary hypertension during exercise in severe emphysema. Respir Physiol. 2000;120:71–9. https://doi.org/10.1016/s0034-5687(00)00090-6.
Zeder K, Avian A, Bachmaier G, Douschan P, Foris V, Sassmann T, et al. Exercise pulmonary resistances predict long-term survival in systemic sclerosis. Chest. 2020. https://doi.org/10.1016/j.chest.2020.08.2110.
Douschan P, Avian A, Foris V, Sassmann T, Bachmaier G, Rosenstock P, et al. Prognostic value of exercise—as compared to resting pulmonary hemodynamics in patients with normal or mildly elevated pulmonary arterial pressure. Am J Respir Crit Care Med. 2022. https://doi.org/10.1164/rccm.202112-2856LE.
Ghio S, Klersy C, Magrini G, D’Armini AM, Scelsi L, Raineri C, et al. Prognostic relevance of the echocardiographic assessment of right ventricular function in patients with idiopathic pulmonary arterial hypertension. Int J Cardiol. 2010;140:272–8. https://doi.org/10.1016/j.ijcard.2008.11.051.
Spruijt OA, de Man FS, Groepenhoff H, Oosterveer F, Westerhof N, Vonk-Noordegraaf A, et al. The effects of exercise on right ventricular contractility and right ventricular–arterial coupling in pulmonary hypertension. Am J Respir Crit Care Med. 2015;191:1050–7. https://doi.org/10.1164/rccm.201412-2271OC.
Gorcsan J, Murali S, Counihan PJ, Mandarino WA, Kormos RL. Right ventricular performance and contractile reserve in patients with severe heart failure. Assessment by pressure-area relations and association with outcome. Circulation. 1996;94:3190–7. https://doi.org/10.1161/01.cir.94.12.3190.
Haddad F, Vrtovec B, Ashley EA, Deschamps A, Haddad H, Denault AY. The concept of ventricular reserve in heart failure and pulmonary hypertension: an old metric that brings us one step closer in our quest for prediction. Curr Opin Cardiol. 2011;26:123–31. https://doi.org/10.1097/HCO.0b013e3283437485.
Acknowledgements
The authors would like to thank Dr. Daniela Kleinschek (Ludwig Boltzmann Institute for Lung Vascular Research) for data management and the whole team of the outpatient pulmonary department (Medical University of Graz).
Funding
None.
Author information
Authors and Affiliations
Contributions
TS conceived the project and performed data abstraction and data analysis. GK and HO conceived the project and were responsible for final manuscript approval. PD performed data abstraction and manuscript editing. PD, VF, GK, NT and GB had huge impact on data collection and management of the database. All authors contributed to the writing and editing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol conformed to the Declaration of Helsinki and was approved by the Ethics Committee of the Medical University of Graz (EK 32–352 ex 19–20). Due to its retrospective nature, there was no informed consent necessary in order to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
relevant cardiac, pulmonary, hepatic and renal comorbidities from both groups are listed. “Minor intracardiac shunt” was one atrial septum defect without indication for intervention (COPD), one status post occlusion of a foramen ovale 10 years before (control). Table S2. Follow-up right heart catheterization (RHC) and all-cause mortality in COPD patients and controls.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sassmann, T., Douschan, P., Foris, V. et al. Abnormal pulmonary hemodynamics during exercise is associated with exercise capacity in COPD. Respir Res 23, 331 (2022). https://doi.org/10.1186/s12931-022-02238-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-022-02238-9