Abstract
Background
Resting pulmonary hypertension (PH) is not uncommon in patients with chronic obstructive pulmonary disease (COPD). In the current study, we aimed to identify physiological predictors of resting PH in patients with COPD.
Methods
We retrospectively analyzed data derived from right heart catheterization in sixty-nine stable patients with COPD. Patients were categorized into COPD-PH (n = 33) and COPD-non-PH (n = 36), based on the “6th World Symposium on PH.”
Results
Demographics, forced expiratory volume in 1 s (FEV1), lung volumes, cardiac output, and cardiac index were similar between groups, yet COPD-PH had greater pulmonary vascular resistance (PVR) and lower resting PaO2 (P < 0.05). The proportion of COPD-PH patients did not differ across the range of FEV1 (χ2 = 3.01, P = 0.22). No correlations were found between PVR and the degree of airflow obstruction or resting hyperinflation. Resting PaO2 was the only predictor of both pulmonary artery pressure and PVR.
Conclusions
Increased PVR, in response to arterial hypoxemia or directly induced by tobacco smoking, is likely the key factor that led to resting PH in the current sample of patients with moderate-severe COPD, regardless of the degree of airflow limitation or resting hyperinflation.
Similar content being viewed by others
Background
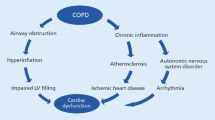
Pulmonary hypertension (PH) is a common, potentially inevitable complication of chronic obstructive pulmonary disease (COPD) [1]. The presence of PH in patients with COPD is linked to poor health-related quality of life, impaired exercise capacity, increased risk of severe acute exacerbation, frequent hospitalization, and increased mortality [2,3,4,5]. The reported prevalence of resting PH in COPD varies considerably from 20 to 91% based on the definition of PH, methods used to determine pulmonary artery pressure (PAP), and the studied population [4, 6, 7]. Precise determination of the prevalence of PH among patients with COPD is also hindered by the methodological and ethical limitations of performing right heart catheterization (RHC) on a large scale, and the potential errors associated with the use of echocardiography alone in these patients [8, 9]. More recently, the 6thWorld Symposium on PH proposed a more accurate hemodynamic classification of PH associated with COPD that incorporated measurements of pulmonary vascular resistance (PVR) and cardiac function [4]. This proposed classification would indeed have an impact on disease prevalence.
COPD-associated PH is usually of mild-moderate severity [10, 11], that is sometimes associated with the degree of airflow obstruction severity [12,13,14,15]. Nevertheless, in a small percentage of patients, PH severity may exceed the severity of airflow obstruction [16, 17]. In this regard, there has been a recent interest in the “pulmonary vascular phenotype” in patients with COPD where the degree of vascular derangements surpasses the degree of airway involvement [16]. Those patients may certainly benefit from referral to specialized centers for individual therapy decisions and early targeted PH therapy.
Pathophysiological changes in COPD including vascular endothelial remodeling, arterial hypoxemia, vasoconstriction of pulmonary arteries, vascular compression from hyperinflation, inflammation, and direct toxic effects of cigarette smoke, solely or in combination, are factors that can lead to PH [10, 18, 19]. In the current study, we aimed to assess hemodynamic characteristics of resting PH across the spectrum of COPD severity using data derived from RHC, the gold standard tool for precise PAP measurement [20]. We also aimed to identify resting physiological parameters that could predict the presence of PH in patients with COPD including measurements of gas exchange, airflow obstruction, and resting hyperinflation.
Methods
Study design
We retrospectively analyzed data from 69 stable patients diagnosed with COPD who underwent spirometry, body plethysmography, and RHC using a Swan-Ganz catheter (Edwards-Laboratories, Santa Ana, CA, USA) over 3 years period. Measurements were performed during different clinical research studies (unpublished data) that were ethically approved by the ethical committee of Alexandria University (Egypt). For the purpose of lung function testing, patients were asked to withdraw from used inhalers before performing lung function tests (short-acting bronchodilators (4 h), and long-acting bronchodilators (8 h)).
Subjects
In the current analysis, we included sixty-nine stable patients with moderate-severe COPD who underwent resting lung function tests and RHC after written informed consent. Patients who had a history of acute exacerbation related to COPD in the 4 weeks before the procedure date were excluded. We also excluded patients with asthma, congestive heart failure, obstructive sleep apnea, or other known significant comorbid conditions that may contribute to increased PAP.
Patients were categorized based on the "6thWorld Symposium on PH - proposed hemodynamic classification of PH associated with COPD" into those with resting PH (COPD-PH) and those without (COPD-non-PH) [4]. COPD-non-PH was defined as mean pulmonary artery pressure (mPAP) < 21 mmHg or mPAP 21–24 mmHg with PVR < 3 Wood Units (WU); COPD-PH was defined as mPAP 21–24 mmHg with PVR ≥ 3 WU or mPAP 25–34 mmHg including those with severe PH (i.e., mPAP ≥ 35 mmHg or mPAP ≥ 25 mmHg with low cardiac index (CI) < 2.0 L/min/m2) [4, 21].
Procedures
Lung function tests and arterial blood gases
Spirometry and body plethysmography were performed using HypAir, Medisoft, Sorinnes, Belgium. Data were presented as percentages of predicted normal values using the Global Lung Function Initiative (GLI) reference equations [22, 23]. Arterial blood samples were collected from the radial artery at rest while breathing ambient room air just before the RHC procedure, then immediately analyzed.
Right heart catheterization
RHC was conducted in patients with COPD within 24 h of lung function testing at the same time of the day. A triple-lumen Swan-Ganz catheter (model 93A-131-7F, Edwards Laboratories, Santa Ana, CA, USA) was inserted into the pulmonary artery under pressure wave monitoring (Hewlett Packard Viridia CMS monitor; Böblingen, Germany). The pressure transducer was zeroed at the level of the left atrium (i.e., at the mid-thoracic line) [20]. mPAP was calculated as [mPAP = diastolic PAP + (systolic–diastolic PAP)/3] [1]. Pulmonary artery wedge pressure (PAWP) and cardiac output (CO) were measured as per guidelines [4, 24]. CI and PVR were calculated using the following formulae [CI = CO/body surface area] and [PVR = (mPAP–mean PAWP)/CO], respectively [20].
Statistical analysis
The unpaired t-test or Mann–Whitney rank sum test was used to compare differences between COPD-PH and COPD-non-PH patients. Associations between dependent variables (mPAP and PVR) and relevant independent variables (age, forced expiratory volume in 1 s (FEV1), functional residual capacity (FRC), and resting partial pressure of arterial oxygen (PaO2)) were assessed using linear regression models. A comparison of proportions was done using the χ2 test. Statistical significance was set at P < 0.05. Data were analyzed using SPSS-V20 and SigmaPlot-11.
Results
Subjects’ characteristics and resting pulmonary functions are summarized in Table 1. Patients (age: 56 ± 10 years, mean ± SD) had an average FEV1 of 32 ± 17% predicted. Smoking status was as follows: 70% were current smokers, and 30% were ex-smokers. Patients had evidence of resting hyperinflation and pulmonary gas trapping (i.e., FRC of 140 ± 28% predicted and residual volume/total lung capacity (RV/TLC) of 44 ± 11%). Resting PaO2 and partial pressure of arterial carbon dioxide (PaCO2), while breathing ambient room air, were 62 ± 11 and 50 ± 6 mmHg, respectively (Table 2).
Using the above definitions, resting PH was identified in 33/69 (48%) patients with COPD; out of those, 6 patients had severe PH [defined as mPAP ≥ 35 mmHg or mPAP ≥ 25 mmHg with unexplained low CI (< 2.0 L/min/m2)]. A chi-square test showed that the proportion of COPD-PH patients did not differ across the range of severity of airflow obstruction as determined by FEV1 (χ2 = 3.26, P = 0.20), Fig. 1.
Distribution of mean pulmonary artery pressure (mPAP, mmHg) across the range of FEV1 (%predicted) in patients with COPD (n = 69). Resting pulmonary hypertension (PH) was present in 46% of patients with moderate airflow obstruction (i.e., FEV1: 50–79%predicted), 69% of those with severe airflow obstruction (i.e., FEV1: 30–49%predicted), and in 42% of patients with very severe airflow obstruction (i.e., FEV1 < 30%predicted). The proportion of patients with COPD who had resting PH did not differ across the range of airflow obstruction severity as determined by FEV1 (χ2 = 3.01, P = 0.22). COPD, chronic obstructive pulmonary disease; FEV1, forced expiratory volume in 1 s
Tables 1 and 2 show comparisons between COPD-PH and COPD-non-PH patients. Age, weight, height, body mass index, FEV1, and lung volumes (FRC and TLC) were similar between groups (all P > 0.05). RV (as an absolute value) was greater in COPD-PH vs. COPD-non-PH patients, but RV/TLC was similar between groups, Table 1. Measurements during RHC showed that CO, CI, and PAWP were all similar between groups, yet COPD-PH patients had greater PVR than COPD-non-PH patients (P < 0.001), Table 2. In addition, COPD-PH had lower resting PaO2 compared to COPD-non-PH patients (P = 0.03), but resting PaCO2 was similar between groups, Table 2.
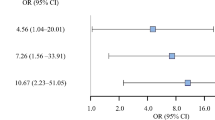
Correlates with mPAP and PVR
Linear regression models predicting mPAP and PVR were significant and among the independent variables (age, FEV1, FRC, and resting PaO2), resting PaO2 was the only predictor of both mPAP and PVR, Table 3. PVR, in turn, correlated well with mPAP (R = 0.70, P < 0.001). Receiver operating characteristic (ROC) curve analysis also showed a statistically significant accuracy of resting PaO2 in diagnosing resting PH in the current sample of patients with COPD (area under the curve = 0.66, P = 0.026); the best cut-off was resting PaO2 < 62.6 mmHg (sensitivity: 58%, specificity 70%).
Discussion
The main findings of the current study are (1) In a single center well-characterized cohort of patients with COPD, the proportion of having resting PH did not differ regardless of the degree of airflow obstruction or resting hyperinflation. (2) COPD patients with and without PH had similar resting CO, CI, and PAWP. (3) Resting PaO2 (and none of the resting physiological lung function parameters) was found to be a good predictor of having resting PH in the current sample of patients with moderate-severe COPD.
The current sample included a group of stable patients with variable severity of COPD as assessed by the GLI reference equations [22, 23]. Patients had moderate to very severe airflow obstruction with an average FEV1 of 32%predicted and evidence of resting hyperinflation and pulmonary gas trapping (Table 1). It has been previously observed that some COPD patients might show a pronounced increase in PAP by as much as 20 mmHg during acute exacerbation (and acute respiratory failure) and returns to its baseline value after the recovery; hypoxic pulmonary vasoconstriction may have a contributory role [25, 26]. Given that, we have carefully confirmed the lack of recent acute exacerbation in our patients within the 4 weeks before the RHC procedure date to avoid potential impacts on PAP measurements.
The wide variability in the reported prevalence of PH in patients with COPD can be due to variable mPAP thresholds used in different studies and/or different methods used to measure PAP [3, 10, 27,28,29]. In this single-center small cohort and using the 6thWorld Symposium proposed hemodynamic classification of PH associated with COPD [4], we have identified resting PH by RHC in 48% of our patients with COPD. Though we have used RHC (the gold standard method to measure PAP), our sample selection is not population-based and cannot indeed be used as an accurate assessment of overall disease prevalence. However, reporting such a high percentage matches with previous reports [30], and further highlights the burden of PH in patients with COPD.
PAP can be determined by PAWP and the driving pressure within the pulmonary circulation. As such, three main variables that can contribute to an increased PAP: PAWP, CO, and PVR. Resting PAWP was previously reported to be elevated in 19% of a large sample of patients with COPD, but most of these patients had evidence of left heart disease [31]. Also, in the hemodynamic study of the National Emphysema Treatment Trial, 61% of patients had resting PAWP values greater than normal (i.e., > 12 mmHg) [3]. In the current study sample, resting PAWP (and CO) were within the normal range, and they did not differ between COPD-PH and COPD-non-PH patients, matched for airflow obstruction severity (Table 2). However, PVR was significantly higher in COPD-PH compared to COPD-non-PH (P< 0.001). Increased PVR in COPD could be due to vascular endothelial remodeling, arterial hypoxemia, or hypercapnic acidosis both leading to pulmonary vasoconstriction, loss of capillary surface area due to emphysema and/or compression of alveolar vessels from hyperinflation and pressures swings associated with airflow limitation [10, 19, 32].
Chest computed tomography (CT) scans were not available for the current analysis, so we could not assess the role of possible structural emphysema, which can eventually cause compression and destruction of alveolar vessels, perhaps contributing to increased PVR and the occurrence of PH in our patients [3]. Nevertheless, measurements of resting hyperinflation (e.g., FRC and RV/TLC) were not different between COPD-PH and COPD-non-PH patients (Table 1), and additionally they did not correlate with PVR or mPAP in the current analysis, Table 3. It is also expected that with increasing airflow obstruction severity (i.e., decrease in FEV1) with resultant worsening of expiratory flow limitation, the end-expiratory pressures may increase and can be potentially transmitted to the pulmonary vasculature causing a rise in the PAP [7]. However, we did not find any correlation between FEV1 and PVR or PAP in the current analysis. Moreover, the proportion of COPD patients who had resting PH did not differ across a wide range of airflow obstruction severity, Fig. 1.
Alveolar hypoxia is probably the most important factor leading to an increased PVR in COPD, with hypoxic pulmonary vasoconstriction usually coming into action in acute situations (e.g., acute exacerbation and during exercise) [33]. Chronic hypoxia has also been shown to induce structural changes at the level of the pulmonary vessels in animal models resulting in an imbalance between vasodilators and vasoconstrictors, contributing to increased PVR [34, 35]. In this regard, a recent study by Gonzalez-Garcia et al. [5], showed that COPD patients with PH exhibit more ventilatory inefficiency and gas exchange alterations at rest and during exercise compared to those without PH. However, we should acknowledge that in this study [5], COPD patients with PH had more severe airflow obstruction compared with those without PH. In the current study, the significant relationships found between resting PaO2 and both PVR and mPAP may indicate that hypoxic pulmonary vasoconstriction and/or endothelial remodeling is closely related to the pathogenesis of PH in the current sample of patients with COPD. Our results also revealed that, in COPD patients with resting PaO2of ≥ 62.6 mmHg (> 60 mmHg in a previous study) [36], hypoxic pulmonary vasoconstriction might play a minor role in generating resting PH. This notion suggests that vascular inflammation and remodeling, directly induced by tobacco smoking, are possibly the main factors that have led to PH in a substantial number of our patients (30%) who had a resting PaO2 of ≥ 62.6 mmHg while breathing ambient room air. Of note, there was no evidence of hypercapnic acidosis in COPD patients with PH in the current sample (Table 2), so its role in generating pulmonary vasoconstriction seemed negligible.
Collectively, our results suggest that pulmonary vascular abnormalities, in response to arterial hypoxemia or directly induced by tobacco smoking, are perhaps the main mechanisms behind PH in the current sample of patients with COPD.
Limitations
The current analysis included a single-center cohort of patients with moderate-severe COPD, so results may not be generalized. Data from chest CT scans and lung diffusing capacity were not available for the current analysis; this may affect our results on the proportion of resting PH across the severity of COPD. As per standard guidelines, an echocardiogram was done for all patients, but complete data were not available for the current analysis.
Conclusions
Using the recently proposed RHC-derived hemodynamic classification of PH associated with COPD [4], resting PH was identified in 48% of a single-center cohort of COPD patients with moderate-severe airflow obstruction, and severe PH constituted a respective percentage of these patients. Pulmonary vascular abnormalities, in response to arterial hypoxemia or directly induced by smoking, with resultant increase in PVR are likely the key factors that have led to PH in the current sample, regardless of the degree of airflow obstruction or resting hyperinflation. Resting arterial hypoxemia was found to be a good predictor of having resting PH in patients with moderate-severe COPD.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- CI:
-
Cardiac index
- CO:
-
Cardiac output
- COPD:
-
Chronic obstructive pulmonary disease
- CT:
-
Computed tomography
- FEV1 :
-
Forced expiratory volume in 1 s
- FRC:
-
Functional residual capacity
- FVC:
-
Forced vital capacity
- mPAP:
-
Mean pulmonary artery pressure
- PaCO2 :
-
The partial pressure of arterial carbon dioxide
- PaO2 :
-
The partial pressure of arterial oxygen
- PAP:
-
Pulmonary artery pressure
- PAWP:
-
The pulmonary artery wedge pressure
- PH:
-
Pulmonary hypertension
- PVR:
-
Pulmonary vascular resistance
- RHC:
-
Right heart catheterization
- ROC:
-
Receiver operating characteristic
- RV:
-
Residual volume
- TLC:
-
Total lung capacity
References
Simonneau G, Montani D, Celermajer DS et al (2019) Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur Respir J 53:1. https://doi.org/10.1183/13993003.01913-2018
Kessler R, Faller M, Fourgaut G, Mennecier B, Weitzenblum E (1999) Predictive factors of hospitalization for acute exacerbation in a series of 64 patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 159(1):158–164. https://doi.org/10.1164/ajrccm.159.1.9803117
Scharf SM, Iqbal M, Keller C et al (2002) Hemodynamic characterization of patients with severe emphysema. Am J Respir Crit Care Med 166(3):314–322. https://doi.org/10.1164/rccm.2107027
Nathan SD, Barbera JA, Gaine SP et al (2019) Pulmonary hypertension in chronic lung disease and hypoxia. Eur Respir J 53:1. https://doi.org/10.1183/13993003.01914-2018
Gonzalez-Garcia M, Aguirre-Franco CE, Vargas-Ramirez L, Barrero M, Torres-Duque CA (2022) Effect of pulmonary hypertension on exercise capacity and gas exchange in patients with chronic obstructive pulmonary disease living at high altitude. Chron Respir Dis Jan-Dec 19:14799731221104096. https://doi.org/10.1177/14799731221104095
Gupta KK, Roy B, Chaudhary SC et al (2018) Prevalence of pulmonary artery hypertension in patients of chronic obstructive pulmonary disease and its correlation with stages of chronic obstructive pulmonary disease, exercising capacity, and quality of life. J Family Med Prim Care Jan-Feb 7(1):53–57. https://doi.org/10.4103/jfmpc.jfmpc_18_17
Gologanu D, Stanescu C, Ursica T, Balea MI, Ionita D, Bogdan MA (2013) Prevalence and Characteristics of Pulmonary Hypertension Associated with COPD - A Pilot Study in Patients Referred to a Pulmonary Rehabilitation Program Clinic. Maedica (Bucur) 8(3):243–248
Fisher MR, Criner GJ, Fishman AP et al (2007) Estimating pulmonary artery pressures by echocardiography in patients with emphysema. Eur Respir J 30(5):914–921. https://doi.org/10.1183/09031936.00033007
Arcasoy SM, Christie JD, Ferrari VA et al (2003) Echocardiographic assessment of pulmonary hypertension in patients with advanced lung disease. Am J Respir Crit Care Med 167(5):735–740. https://doi.org/10.1164/rccm.200210-1130OC
Chaouat A, Naeije R, Weitzenblum E (2008) Pulmonary hypertension in COPD. Eur Respir J 32(5):1371–1385. https://doi.org/10.1183/09031936.00015608
Blanco I, Tura-Ceide O, Peinado VI, Barbera JA (2020) Updated Perspectives on Pulmonary Hypertension in COPD. Int J Chron Obstruct Pulmon Dis 15:1315–1324. https://doi.org/10.2147/COPD.S211841
Cuttica MJ, Kalhan R, Shlobin OA et al (2010) Categorization and impact of pulmonary hypertension in patients with advanced COPD. Respir Med 104(12):1877–1882. https://doi.org/10.1016/j.rmed.2010.05.009
Thabut G, Dauriat G, Stern JB et al (2005) Pulmonary hemodynamics in advanced COPD candidates for lung volume reduction surgery or lung transplantation. Chest 127(5):1531–1536. https://doi.org/10.1378/chest.127.5.1531
Hilde JM, Skjorten I, Hansteen V et al (2013) Haemodynamic responses to exercise in patients with COPD. Eur Respir J 41(5):1031–1041. https://doi.org/10.1183/09031936.00085612
Portillo K, Torralba Y, Blanco I et al (2015) Pulmonary hemodynamic profile in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis 10:1313–1320. https://doi.org/10.2147/COPD.S78180
Kovacs G, Agusti A, Barbera JA et al (2018) Pulmonary Vascular Involvement in Chronic Obstructive Pulmonary Disease. Is There a Pulmonary Vascular Phenotype? Am J Respir Crit Care Med. 1988:1000–1011. https://doi.org/10.1164/rccm.201801-0095PP
Voelkel NF, Cool CD (2003) Pulmonary vascular involvement in chronic obstructive pulmonary disease. Eur Respir J Suppl 46:28s–32s. https://doi.org/10.1183/09031936.03.00000503
Wright JL, Levy RD, Churg A (2005) Pulmonary hypertension in chronic obstructive pulmonary disease: current theories of pathogenesis and their implications for treatment. Thorax 60(7):605–609. https://doi.org/10.1136/thx.2005.042994
Santos S, Peinado VI, Ramirez J et al (2002) Characterization of pulmonary vascular remodelling in smokers and patients with mild COPD. Eur Respir J 19(4):632–638
Rosenkranz S, Preston IR (2015) Right heart catheterisation: best practice and pitfalls in pulmonary hypertension. Eur Respir Rev 24(138):642–652. https://doi.org/10.1183/16000617.0062-2015
Seeger W, Adir Y, Barbera JA et al (2013) Pulmonary hypertension in chronic lung diseases. J Am Coll Cardiol 62(25 Suppl):D109–D116. https://doi.org/10.1016/j.jacc.2013.10.036
Quanjer PH, Stanojevic S, Cole TJ et al (2012) Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J 40(6):1324–1343. https://doi.org/10.1183/09031936.00080312
Hall GL, Filipow N, Ruppel G et al (2021) Official ERS technical standard: Global Lung Function Initiative reference values for static lung volumes in individuals of European ancestry. Eur Respir J. 57:3. https://doi.org/10.1183/13993003.00289-2020
Galie N, Humbert M, Vachiery JL et al (2015) 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Respir J 46(4):903–975. https://doi.org/10.1183/13993003.01032-2015
Weitzenblum E, Apprill M, Oswald M, Chaouat A, Imbs JL (1994) Pulmonary hemodynamics in patients with chronic obstructive pulmonary disease before and during an episode of peripheral edema. Chest 105(5):1377–1382. https://doi.org/10.1378/chest.105.5.1377
Abraham AS, Cole RB, Green ID, Hedworth-Whitty RB, Clarke SW, Bishop JM (1969) Factors contributing to the reversible pulmonary hypertension of patients with acute respiratory failure studies by serial observations during recovery. Circ Res 24(1):51–60. https://doi.org/10.1161/01.res.24.1.51
Weitzenblum E, Sautegeau A, Ehrhart M, Mammosser M, Hirth C, Roegel E (1984) Long-term course of pulmonary arterial pressure in chronic obstructive pulmonary disease. Am Rev Respir Dis 130(6):993–998. https://doi.org/10.1164/arrd.1984.130.6.993
Oswald-Mammosser M, Apprill M, Bachez P, Ehrhart M, Weitzenblum E (1991) Pulmonary hemodynamics in chronic obstructive pulmonary disease of the emphysematous type. Respiration 58(5–6):304–310. https://doi.org/10.1159/000195950
Falk JA, Kadiev S, Criner GJ, Scharf SM, Minai OA, Diaz P (2008) Cardiac disease in chronic obstructive pulmonary disease. Proc Am Thorac Soc 5(4):543–548. https://doi.org/10.1513/pats.200708-142ET
Weitzenblum E, Hirth C, Ducolone A, Mirhom R, Rasaholinjanahary J, Ehrhart M (1981) Prognostic value of pulmonary artery pressure in chronic obstructive pulmonary disease. Thorax 36(10):752–758. https://doi.org/10.1136/thx.36.10.752
Chabot F, Schrijen F, Poincelot F, Polu JM (2001) Interpretation of high wedge pressure on exercise in patients with chronic obstructive pulmonary disease. Cardiology 95(3):139–145. https://doi.org/10.1159/000047360
Nagaraj C, Tabeling C, Nagy BM et al (2017) Hypoxic vascular response and ventilation/perfusion matching in end-stage COPD may depend on p22phox. Eur Respir J. 50:1. https://doi.org/10.1183/13993003.01651-2016
Fishman AP, Mc CJ, Himmelstein A, Cournand A (1952) Effects of acute anoxia on the circulation and respiration in patients with chronic pulmonary disease studied during the steady state. J Clin Invest 31(8):770–781. https://doi.org/10.1172/JCI102662
Stenmark KR, Fagan KA, Frid MG (2006) Hypoxia-induced pulmonary vascular remodeling: cellular and molecular mechanisms. Circ Res 99(7):675–691. https://doi.org/10.1161/01.RES.0000243584.45145.3f
Faller DV (1999) Endothelial cell responses to hypoxic stress. Clin Exp Pharmacol Physiol 26(1):74–84. https://doi.org/10.1046/j.1440-1681.1999.02992.x
Kessler R, Faller M, Weitzenblum E et al (2001) “Natural history” of pulmonary hypertension in a series of 131 patients with chronic obstructive lung disease. Am J Respir Crit Care Med 164(2):219–224. https://doi.org/10.1164/ajrccm.164.2.2006129
Acknowledgements
The authors would like to thank study participants, nurses, and respiratory physiologists in the Department of Chest Diseases, Alexandria Faculty of Medicine.
Notification of prior abstract presentation
Parts of the data presented herein were presented as an abstract at the European Respiratory Society meeting 2021. https://doi.org/10.1183/13993003.congress-2021.PA3596.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors meet the criteria for authorship as recommended by the International Committee of Medical Journal Editors. All authors played a role in the content and writing of the manuscript. In addition, M.E.A., Y.M.K., T.S.M., and A.F.E. provided the original idea for the study; A.F.E. and A.A. performed data analysis and prepared it for presentation. A.F.E. wrote the first draft of the manuscript and all authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This is a retrospective study and measurements were performed during different clinical research studies (unpublished data) that were ethically approved by the ethical committee of Alexandria University (Egypt). Written informed consent was obtained from all patients prior to their initial study participation.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
^Tamer S. Morsi is deceased.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Atta, M.E., Khalil, Y.M., Abd-Elhameed, A. et al. Physiological predictors of resting pulmonary hypertension associated with COPD: a retrospective analysis. Egypt J Bronchol 17, 11 (2023). https://doi.org/10.1186/s43168-023-00179-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43168-023-00179-5