Abstract
Background
Multimorbidity is defined as two or more chronic health conditions existing in an individual simultaneously. Multimorbidity has been associated with poor conditions, such as higher health care costs and the poor quality of life. Thus, identifying the risk factors of the multimorbidity is required for multimorbidity prevention.
Methods
This study was based on the Comprehensive Demonstration Research Project of Major Chronic Noncommunicable Disease Prevention and Control Technology in Northeast China initiated by China Medical University. The investigation was a cross-sectional study under a multistage stratified cluster random sampling design. Associations between multimorbidity and sociodemographic and behavioral factors in adult residents were investigated using univariate analysis and multivariate logistic regression analysis.
Results
A total of 6706 participants were enrolled in this investigation, and the prevalence of multimorbidity was 21.2% among the adult residents of northeastern China. There existed differences of association between age and multimorbidity risks (65–69 years old: OR = 3.53, 95%CI: 2.04–6.12; 70–74 years old: OR = 5.26, 95%CI: 3.02–9.17). Participants who are overweight had significantly high multimorbidity risk (OR = 2.76, 95%CI: 1.50–5.24). Family history of hypertension and family history of diabetes were significantly associated with high multimorbidity risk (family history of hypertension: OR = 2.34, 95%CI: 1.96–2.79; family history of diabetes: OR = 1.77, 95%CI: 1.38–2.26). Compared with the frequency of fatigue (< 1 time/week or 1–2 times/week), that (≥3 times/week) was associated with high multimorbidity risk (OR = 1.39, 95%CI: 1.07–1.81). For fresh fruit consumption, compared with eating fruits regularly, eating rarely had a higher risk of multimorbidity (OR = 2.33, 95%CI: 1.90–2.85).
Conclusions
Sociodemographic indices (age, BMI, family history of hypertension, and family history of diabetes) and behavioral indices (fatigue status and fresh fruit consumption) increase the risks of multimorbidity. This study provides a necessary route to prevent and control multimorbidity in northeast China.
Similar content being viewed by others
Introduction
Multimorbidity is defined as two or more chronic health conditions existing in an individual simultaneously [1,2,3,4]. Multimorbidity increases with aging [5]. Aging is a risk factor of multimorbidity; moreover, the number and proportion of the elderly are increasing sharply in China. Thus, China has to face a heavy burden of the multimorbidity in future decades [6, 7].
Multimorbidity has been associated with adverse events, including longer hospitalizations, multiple medical treatments, more complications, psychological distress, higher health care costs, and the poorer quality of life [8,9,10,11,12,13,14,15]. A higher number of chronic conditions in an individual is associated with higher mortality [16,17,18]. In addition, multimorbidity is associated with a higher risk of unemployment [19], and multimorbidity leads to a substantial economic burden on health care systems [20,21,22]. Therefore, identifying the risk factors for multimorbidity to further address the major public health problems.
To date, the prevalence and pattern of multimorbidity has been investigated worldwide. The prevalence of multimorbidity are reported as following: 28% in Americans [23], 37.1% in Australia [24], 58.2% in women who are more than 50 years old in Brazil [25], and 6.4–76.5% in the population aged 60 years or more in China [26]. The difference of multimorbidity prevalence may arise from population, data sources, and eating habits from different areas. The major patterns of multimorbidity are identified as cardiovascular and metabolic diseases, mental health problems, and musculoskeletal disorders in the elderly who lived in Europe, the United States (U.S.), and Australia [27]. In contrast, cardiopulmonary-mental-degenerative disorder and cerebrovascular-metabolic disorder are the patterns identified in China [28]. Indeed, different methods, population, and chronic diseases have been used in defining multimorbidity pattern, affording that there exists no consensus on the determination and classification of multimorbidity pattern.
The prevention and control of chronic disease are necessary for multimorbidity management, underscoring the identification of risk factors of the multimorbidity. The risk factors for multimorbidity have been identified in studies, including age, female, and low socioeconomic status [29,30,31]. Moreover, influencing factors of multimorbidity, such as racial and ethnic, remain controversial [32, 33]. Thus, more studies are needed to investigate risk factors for multimorbidity. In this paper, we investigated the prevalence of multimorbidity and further evaluated the sociodemographic and behavioral influences on multimorbidity among adult residents to identify the risk factors for multimorbidity in Changchun, China.
Materials and methods
Ethical statement
The study was approved by the Ethics Committee of China Medical University. The study protocol was performed in accordance with the principles outlined in the Declaration of Helsinki, and informed consent was collected from each of participants.
Study population
The study was affiliated to the Comprehensive Demonstration Research Project of Major Chronic Noncommunicable Disease Prevention and Control Technology in Northeast China initiated by China Medical University. The investigation, which was conducted from January 1, 2019 to November 31, 2019, was a cross-sectional study under a multistage stratified cluster random sampling design. The data were collected from residents of 10 districts in Changchun city, Jilin Province. The adult residents were enrolled according to following inclusion criteria: (1) over the age of 35 years; (2) with registered permanent residence (a record officially identifying area residents); (3) living in Changchun for more than 6 months; (4) with consciousness and no communication barriers; (5) good compliance. The exclusion criteria satisfied the followings: (1) incomplete information; (2) data with outliers. (Supplemental Fig. 1).
Questionnaire and health examination
The questionnaire was designed by the China Medical University and the School of Public Health, Jilin University. Direct face-to-face interview survey was performed by uniformly trained investigators. Questionnaires and data of anthropometric measurements were collected from each participant. Demographic information (sex, age, ethnicity, marital status, occupation, annual income, and level of education), health behaviors (smoking, drinking, diet, sleep status, and physical activity), and history of chronic diseases (hypertension, diabetes, coronary heart disease, and stroke), were collected from the questionnaires. In addition, the information of anthropometric measurements (height, weight, blood pressure, fasting blood glucose, and blood lipids) were obtained from health examination. Every physical measurement was checked by two medical staffs together. Blood samples were collected and transported to a central laboratory via a cold chain transport system.
Statistical analysis
Constituent ratio was used to represent the composition of prevalence of chronic diseases for classified participants according to sociodemographic and behavioral characteristics. Chi-square (χ2) test was used to identify the relationship of multimorbidity with sociodemographic and behavioral characteristics. Multivariate logistic regression was performed to analyze odds ratios (OR) for multimorbidity. The predictive models were built on the basis of risk factors and visualized using nomograms, and the performance of our models was evaluated using the Harrell’s concordance index (c-index). SPSS version 24.0 and R version 4.1.0 were used for statistical analysis, and P-values < 0.05 was considered statistically significant.
Results
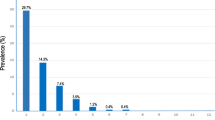
A total of 6706 participants were enrolled in this investigation. The mean age of the participants was 68.79 years old, and the prevalence of multimorbidity was 21.2%. The participants were divided into four groups according to the number of chronic disease (1 disease, 2 diseases, and ≥ 3 diseases), and corresponding data of prevalence are showed in Table 1. Significant differences of prevalence classified by number of chronic diseases existed in age, BMI, marital status, family history of hypertension, family history of diabetes, educational level, occupation, annual income, physical exercise, sleep status, fatigue status, stay up late, salt taste, edible oil taste, carbonated drinks, fresh fruit consumption, meat consumption (red meat and poultry), consumption of fish, and consumption of eggs and beans (P < 0.05).
We used univariate analysis to investigate the influencing factors of multimorbidity on the basis of 26 independent variables listed in the questionnaire, finding that multimorbidity was associated with age, BMI, marital status, family history of hypertension, family history of diabetes, sleep status, fatigue status, salt taste, edible oil taste, carbonated drinks, fresh fruit consumption, meat consumption (poultry), consumption of fish, and consumption of eggs and beans (P < 0.05) (Table 2). The prevalence of multimorbidity increased with aging (P < 0.001). The prevalence of multimorbidity in participants with underweight, normal weight, overweight, or obese was 10.8, 30.0, 24.5, and 20.0%, correspondingly (P < 0.001). There were the significant differences of prevalence in married/cohabitation, unmarried, and divorced/separated (8.6, 21.0, and 24.1%, respectively) (P = 0.027). The prevalence of multimorbidity in participants with family history of hypertension/diabetes was significantly higher than that in participants without the respective/corresponding one (P < 0.001). The prevalence of multimorbidity increased with the deteriorating of sleep status (P < 0.001). The prevalence of multimorbidity increased with the increasing frequency of fatigue (P < 0.001). For salt consumption and edible oil consumption, the prevalence of multimorbidity of appropriate consumption was significantly lower than that of excessive consumption or low consumption (P < 0.001). There also existed significantly differences in the prevalence among current-smokers (45.1%), ex-smokers (46.5%), and non-smokers (35.3%) (P < 0.001). For the consumption of fresh fruit, poultry meat, eggs and beans, and fish, the prevalence of multimorbidity increased with the decreasing frequency of consumption from group (often/always) to group (rarely/never) (all P < 0.05) (Table 2).
We further used a multivariate logistic regression analysis, constructing a prediction model to validate multimorbidity-influencing factors. Data of the multiple logistic regression analysis, shown in Fig. 1, are visualized in the form of a nomogram to provide effective and reliable guides (Fig. 2). We identified that the increasing risks of multimorbidity were associated with independent factors (age, BMI, family history of hypertension, family history of diabetes, fatigue status, and fresh fruit consumption) (all P ≤ 0.01). Multimorbidity risks were related to aging (65–69 years old: OR = 3.53, 95%CI: 2.04–6.12; 70–74 years old: OR = 5.26, 95%CI: 3.02–9.17). Overweight participants had significantly high multimorbidity risks (OR = 2.76, 95%CI: 1.50–5.24). Family history of hypertension and family history of diabetes was significantly associated with high multimorbidity risks (family history of hypertension: OR = 2.34, 95%CI: 1.96–2.79; family history of diabetes: OR = 1.77, 95%CI: 1.38–2.26). Compared with the frequency of fatigue (< 1 time/week or 1–2 times/week), that (≥3 times/week) was associated with high multimorbidity risks (OR = 1.39, 95%CI: 1.07–1.81). For fresh fruit consumption, compared with participants eating fruits regularly, those eating rarely had higher risks of multimorbidity (OR = 2.33, 95%CI: 1.90–2.85). The C-index of the nomogram was 0.650.
Discussions
In this paper, we documented that the prevalence of multimorbidity is 21.2% among the adult residents. In addition, the risks of multimorbidity are associated with age, BMI, family history of hypertension, family history of diabetes, fatigue status, and fresh fruit consumption.
The prevalence of multimorbidity in our study in 2019 is substantially lower than that in the study of Wang et al. in 2012 [34]. The decrease in prevalence of multimorbidity in northeastern China may be due to the implementation of chronic disease prevention and control strategies in decades. Actually, chronic disease prevention and control, supported by series projects focusing on chronic noncommunicable disease prevention and control, have been proceeding in northeastern China. With nationally spreading of 5G networks, healthcare systems conduct precise prevention and control for individuals with multimorbidity.
Aging has been widely considered to be associated with risks of multimorbidity [5, 35]. In agreement with other studies [36,37,38], our study also found that the prevalence of multimorbidity increased dramatically with aging. Moreover, consistent with other studies [25, 39, 40], our study found BMI influenced multimorbidity. Zhang et al. conducted a national investigation, finding that obesity is associated with the risk of multimorbidity in whole China [41]. Surprisingly, we corroborated that obesity was neither protect factor nor risk factor of multimorbidity in Northeastern China.
We identified the risk factors of multimorbidity (the family history of hypertension, family history of diabetes, and fatigue status [≥3 times/week]) in northeast China. These factors confer perception to connections implicated in multimorbidity. Thus, people with these three characteristics should pay more attention to their health and strengthen their awareness of prevention and control. In addition, for fresh fruit consumption, similar to the results of Ruel et al. [42], our results also showed that greater consumption of fruits appears to lower risks of multimorbidity.
Multimorbidity increases the risk of disability and mortality [43,44,45], necessitating the identification of influencing factors of multimorbidity. Moreover, our nomogram also provides effective and reliable guides for the risk-prediction, prevention, and control of multimorbidity. Overall, the adult residents with three characteristics (family history of hypertension, family history of diabetes, and fatigue status) are the population with high risk of multimorbidity. The three characteristics provide theoretical and precisely practical guidelines to prevent and control multimorbidity, such as controlling weight and increasing consumption of fruits.
There are strengths in this study, including the large sample size, comprehensive sociodemographic and behavioral characteristics, and region representativeness of northeast China. However, some limitations also exist. First, the causality between multimorbidity and risk factors could not be reflected in our cross-sectional design. Second, the data in this study were based on self-reported questionnaires; therefore, the accuracy of the reported results cannot be determined.
Conclusion
In conclusion, the prevalence of multimorbidity is 21.2% among the adult residents of northeastern China. Sociodemographic indices (age, BMI, family history of hypertension, and family history of diabetes) and behavioral indices (fatigue status and fresh fruit consumption) increase the risks of multimorbidity. This study provides a necessary route to prevent and control multimorbidity in northeast China.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- CI:
-
Confidence Intervals
- OR:
-
Odds Ratios
References
Organization WH. The world health report 2008 : primary health care now more than ever. The World Health Report 2008: primary health care - now more than ever. 2008;25(7):617.
Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet (London, England). 2012;380(9836):37–43.
Ng SK, Tawiah R, Sawyer M, Scuffham P. Patterns of multimorbid health conditions: a systematic review of analytical methods and comparison analysis. Int J Epidemiol. 2018;47(5):1687–704.
van den Akker M, et al. Comorbidity or multimorbidity: comorbidity or multimorbidity: European journal of general practice. Eur J Gen Pract. 1996;2(2):65–70.
Salive ME. Multimorbidity in older adults. Epidemiol Rev. 2013;35:75–83.
Prince MJ, Wu F, Guo Y, Gutierrez Robledo LM, O'Donnell M, Sullivan R, et al. The burden of disease in older people and implications for health policy and practice. Lancet (London, England). 2015;385(9967):549–62.
Wang HH, Wang JJ, Wong SY, Wong MC, Li FJ, Wang PX, et al. Epidemiology of multimorbidity in China and implications for the healthcare system: cross-sectional survey among 162,464 community household residents in southern China. BMC Med. 2014;12:188.
Condelius A, Edberg AK, Jakobsson U, Hallberg IR. Hospital admissions among people 65+ related to multimorbidity, municipal and outpatient care. Arch Gerontol Geriatr. 2008;46(1):41–55.
Wehling M. Multimorbidity and polypharmacy: how to reduce the harmful drug load and yet add needed drugs in the elderly? Proposal of a new drug classification: fit for the aged. J Am Geriatr Soc. 2009;57(3):560–1.
Marengoni A, von Strauss E, Rizzuto D, Winblad B, Fratiglioni L. The impact of chronic multimorbidity and disability on functional decline and survival in elderly persons. A community-based, longitudinal study. J Intern Med. 2009;265(2):288–95.
Fortin M, Lapointe L, Hudon C, Vanasse A, Ntetu AL, Maltais D. Multimorbidity and quality of life in primary care: a systematic review. Health Qual Life Outcomes. 2004;2:51.
Fortin M, Bravo G, Hudon C, Lapointe L, Almirall J, Dubois MF, et al. Relationship between multimorbidity and health-related quality of life of patients in primary care. Qual Life Res Int J Qual Life Asp Treat Care Rehab. 2006;15(1):83–91.
Bähler C, Huber CA, Brüngger B, Reich O. Multimorbidity, health care utilization and costs in an elderly community-dwelling population: a claims data based observational study. BMC Health Serv Res. 2015;15:23.
Fortin M, Dubois MF, Hudon C, Soubhi H, Almirall J. Multimorbidity and quality of life: a closer look. Health Qual Life Outcomes. 2007;5:52.
Gu J, Chao J, Chen W, Xu H, Zhang R, He T, et al. Multimorbidity and health-related quality of life among the community-dwelling elderly: a longitudinal study. Arch Gerontol Geriatr. 2018;74:133–40.
Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel JP, et al. The world report on ageing and health: a policy framework for healthy ageing. Lancet (London, England). 2016;387(10033):2145–54.
DuGoff EH, Canudas-Romo V, Buttorff C, Leff B, Anderson GF. Multiple chronic conditions and life expectancy: a life table analysis. Med Care. 2014;52(8):688–94.
Singh K, Patel SA, Biswas S, Shivashankar R, Kondal D, Ajay VS, et al. Multimorbidity in south Asian adults: prevalence, risk factors and mortality. J Public Health (Oxford, England). 2019;41(1):80–9.
Frith E, Ramulu PY, Ashar B, Loprinzi PD. Association of single and multiple medical conditions with work status among adults in the United States. J Lifestyle Med. 2019;9(1):15–26.
Violán C, Foguet-Boreu Q, Roso-Llorach A, Rodriguez-Blanco T, Pons-Vigués M, Pujol-Ribera E, et al. Burden of multimorbidity, socioeconomic status and use of health services across stages of life in urban areas: a cross-sectional study. BMC Public Health. 2014;14:530.
Pefoyo AJ, Bronskill SE, Gruneir A, Calzavara A, Thavorn K, Petrosyan Y, et al. The increasing burden and complexity of multimorbidity. BMC Public Health. 2015;15:415.
Laires PA, Perelman J. The current and projected burden of multimorbidity: a cross-sectional study in a southern Europe population. Eur J Ageing. 2019;16(2):181–92.
Foundation R. Chronic care: making the case for ongoing care: Robert Wood Johnson Foundation; 2010.
Britt HC, Harrison CM, Miller GC, Knox SA. Prevalence and patterns of multimorbidity in Australia. Med J Aust. 2008;189(2):72–7.
de Santos Machado V, Valadares AL, Costa-Paiva LH, Osis MJ, Sousa MH, Pinto-Neto AM. Aging, obesity, and multimorbidity in women 50 years or older: a population-based study. Menopause (New York, NY). 2013;20(8):818–24.
Hu X, Huang J, Lv Y, Li G, Peng X. Status of prevalence study on multimorbidity of chronic disease in China: systematic review. Geriatr Gerontol Int. 2015;15(1):1–10.
Prados-Torres A, Calderón-Larrañaga A, Hancco-Saavedra J, Poblador-Plou B, van den Akker M. Multimorbidity patterns: a systematic review. J Clin Epidemiol. 2014;67(3):254–66.
Wang R, Yan Z, Liang Y, Tan EC, Cai C, Jiang H, et al. Prevalence and patterns of chronic disease pairs and multimorbidity among older Chinese adults living in a rural area. PLoS One. 2015;10(9):e0138521.
Fabbri E, An Y, Zoli M, et al. Aging and the burden of multimorbidity: associations with inflammatory and anabolic hormonal biomarkers. J Gerontol. 2015;70(1):63.
Nagel G, Peter R, Braig S, et al. The impact of education on risk factors and the occurrence of multimorbidity in the EPIC-Heidelberg cohort. BMC Public Health. 2008;8:384.
Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43.
Fabbri E, Zoli M, Gonzalez-Freire M, Salive ME, Studenski SA, Ferrucci L. Aging and multimorbidity: new tasks, priorities, and Frontiers for integrated Gerontological and clinical research. J Am Med Dir Assoc. 2015;16(8):640–7.
Marengoni A, Angleman S, Melis R, Mangialasche F, Karp A, Garmen A, et al. Aging with multimorbidity: a systematic review of the literature. Ageing Res Rev. 2011;10(4):430–9.
Wang SB, D'Arcy C, Yu YQ, Li B, Liu YW, Tao YC, et al. Prevalence and patterns of multimorbidity in northeastern China: a cross-sectional study. Public Health. 2015;129(11):1539–46.
Fortin M, Stewart M, Poitras ME, Almirall J, Maddocks H. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Ann Fam Med. 2012;10(2):142–51.
Uijen AA, van de Lisdonk EH. Multimorbidity in primary care: prevalence and trend over the last 20 years. Eur J Gen Pract. 2008;14(Suppl 1):28–32.
Schäfer I, Hansen H, Schön G, Höfels S, Altiner A, Dahlhaus A, et al. The influence of age, gender and socio-economic status on multimorbidity patterns in primary care. First results from the multicare cohort study. BMC Health Serv Res. 2012;12:89.
van Oostrom SH, Picavet HS, van Gelder BM, Lemmens LC, Hoeymans N, van Dijk CE, et al. Multimorbidity and comorbidity in the Dutch population - data from general practices. BMC Public Health. 2012;12:715.
Agborsangaya CB, Lau D, Lahtinen M, Cooke T, Johnson JA. Multimorbidity prevalence and patterns across socioeconomic determinants: a cross-sectional survey. BMC Public Health. 2012;12:201.
Booth HP, Prevost AT, Gulliford MC. Impact of body mass index on prevalence of multimorbidity in primary care: cohort study. Fam Pract. 2014;31(1):38–43.
Zhang Y, Zhou L, Liu S, Qiao Y, Wu Y, Ke C, et al. Prevalence, correlates and outcomes of multimorbidity among the middle-aged and elderly: findings from the China health and retirement longitudinal study. Arch Gerontol Geriatr. 2020;90:104135.
Ruel G, Shi Z, Zhen S, Zuo H, Kröger E, Sirois C, et al. Association between nutrition and the evolution of multimorbidity: the importance of fruits and vegetables and whole grain products. Clin Nutr (Edinburgh, Scotland). 2014;33(3):513–20.
Nunes BP, Flores TR, Mielke GI, Thumé E, Facchini LA. Multimorbidity and mortality in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2016;67:130–8.
Rizzuto D, Melis RJF, Angleman S, Qiu C, Marengoni A. Effect of chronic diseases and multimorbidity on survival and functioning in elderly adults. J Am Geriatr Soc. 2017;65(5):1056–60.
Ryan A, Wallace E, O'Hara P, Smith SM. Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes. 2015;13:168.
Acknowledgements
We thank all the participants of the study.
Funding
Our study was supported by the funds from the National Key R&D Program of China (Grant #2018YFC1311600), National Natural Science Foundation of China (Grant 81973120), and Graduate Innovation Fund of Jilin University (101832020CX267).
Author information
Authors and Affiliations
Contributions
Yawen Liu, Yi Cheng, and Siyu Liu designed the study. Jikang Shi, Yanbo Guo, Zhuoshuai Liang, Lingfeng Pan, and Yang Yu performed the study. Jikang Shi, Yanbo Guo, Weifei Zhu, Aiyu Shao, and Zhen Li analyzed the data, Jikang Shi drafted the manuscript. Wenjun Chen and Chao Gao participated in revising the manuscript. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of China Medical University. The study protocol is performed in accordance with the principles outlined in the Declaration of Helsinki and informed consent was obtained from all the subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no competing interests regarding the publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Figure 1.
Inclusion and exclusion criteria and selection process of participants.
Additional file 2: Supplemental Table 1.
Definition of variables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shi, J., Guo, Y., Li, Z. et al. Sociodemographic and behavioral influences on multimorbidity among adult residents of northeastern China. BMC Public Health 22, 342 (2022). https://doi.org/10.1186/s12889-022-12722-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-022-12722-y