Abstract
Multimorbidity significantly impacts health, well-being, and the economy; therefore, exploring notable factors associated with multimorbidity across all age groups is critical. For this investigation, we focused on the relationship between four lifestyle factors and multimorbidity risk. We recruited 11,031 Chinese citizens aged ≥ 12 years from 31 provinces between July 2021 and September 2021 using a quota sampling strategy to ensure that the socioeconomic characteristics (sex, age, rural–urban distribution) of those participating in this research were representative of national demographics. In the first stage, multivariable logistic regression models were utilized as a means of investigating the relationship between lifestyle factors and multimorbidity. Then, a multinomial logistic regression model was used with the aim of examining the Healthy Lifestyle Profile (HLP) related to the number of chronic diseases. Multivariable logistic regression models assessed the interaction effects and joint association among the four lifestyle factors. Overall, 18% of the participants had at least one disease, and 5.9% had multimorbidity. Approximately two-thirds of the participants were physically inactive, 40% had consumed alcohol, 39% were underweight or overweight, and 20% were or had been smokers. Participants who maintained one HLP showed a 34% lower multimorbidity risk (adjusted OR, 0.66; 95% CI, 0.48 to 0.92), while participants who maintained 4 HLP showed a 73% lower multimorbidity risk (adjusted OR, 0.27; 95% CI, 0.17 to 0.43), as compared to those who had 0 HLP. The joint association analysis revealed that participants with all four healthy lifestyle factors had 0.92 times lower odds of multimorbidity (95% CI: 0.90, 0.94) in comparison with the all-unhealthy reference cluster. Notably, individuals with a combination of healthy smoking status and healthy body weight had the highest minimized odds of multimorbidity (OR: [0.92], 95% CI: 0.91, 0.94). Common lifestyle habits, alone or in combination, are associated with multimorbidity risk. This study provides insights for public health programs to promote a healthy lifestyle at a younger age and to alleviate multimorbidity risk in older people.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multimorbidity, when at least two chronic conditions are simultaneously present in an individual, is a major challenge for global public health (Salisbury, 2012). For China, a developing country, the presence of multimorbidity undoubtedly increases the burden on the economy (La et al., 2022) and healthcare systems (H. H. Wang, 2014). The combination of multiple diseases can lead to poorer health (Lujic et al., 2022; Q. Zhang et al., 2022; Y. Zhang et al., 2020), lower life quality (Fortin et al., 2004; Makovski et al., 2019), and higher mortality risk (Emerging Risk Factors Collaboration et al., 2015; Rocca et al., 2021). However, chronic disease presence rises dramatically as people get older (Haug et al., 2020), and diseases tend to cluster (Wikström et al., 2015, pp. 1982–2012). Therefore, most studies on multimorbidity focus on older adults. However, multimorbidity is very common and affects many people < 65 years of age. Some reports suggest that the absolute number of people < 65 years of age with multiple diseases is higher (Barnett et al., 2012) than that of the older population (> 65 years of age). Moreover, the all-cause mortality and hospitalization rates of the middle-aged population are higher than those of the older population (Jani et al., 2019; Lai et al., 2019). Therefore, the prevalence of multimorbidity across different age groups and the associated factors should be characterized. While there is certainly an influence of quantifiable aspects, such as socio-economic status (Pathirana & Jackson, 2018), environmental pollution (Divo et al., 2014), and genetics (Malecki et al., 2020), is key to consider, it is similarly important to acknowledge what role elusive elements have to play, especially when trying to acutely comprehend how multimorbidity risk affects people of different demographics with unique lifestyles so that effective strategies can be formulated (Espeland et al., 2020; Fortin et al., 2014; Wikström et al., 2015).
Focusing more specifically on lifestyle characteristics, the 2013–2020 Global Action Plan for the Prevention and Control of Non-communicable Diseases, also known as NCDs, from the World Health Organization (WHO) can be referenced to determine how impactful behaviors like smoking, drinking alcohol, maintain a healthy diet, and exercising are within this context, as these facets are pinpointed as the four most important (World Health Organization, 2013, pp. 2013–2020). It has been supported by other academics that people who smoke are far more likely to suffer from multiple chronic diseases (Ng et al., 2020; Tommola et al., 2019). In India, middle-aged women who drink alcohol are significantly more likely (18%) to suffer from multimorbidity than their counterparts (Mishra et al., 2021). Moreover, the risk of multimorbidity in people with obesity is five times that in people with a normal body mass index (BMI) (Kivimäki et al., 2022). However, the prevalence of a good lifestyle among Chinese adults is extremely low (Zhu et al., 2019).
In contrast to the unchangeable factors, lifestyle characteristics are subject to change over time. Nearly half of the population has reduced the frequency of their physical activity compared to ten years ago (Picavet et al., 2011). People's lifestyles, in terms of BMI, alcohol consumption, and smoking, have changed over a thirty-year measurement period (Schermer et al., 2022). Individual lifestyles are also associated with societal development (H.-L. Yang et al., 2022). In China, the increase in the rate of urbanization has led to a decrease in activity and a significant increase in the BMI of the population in urban areas (Hou et al., 2019). However, the variability in lifestyle habits gives more people control their lives and health. Adults who change their unhealthy lifestyle are 35% less likely to develop cardiovascular disease and 40% less likely to die (King et al., 2007). In addition, adverse factors due to multimorbidity tend to accumulate with age (de Almeida et al., 2020). Thus, the increasing prevalence of multimorbidity in old age may be managed with healthy habits and early changes in adverse habits earlier in life. The trend of multimorbidity prevalence in sub-Saharan Africa has been proposed to be preventable by early changes in modifiable factors, including BMI (Alkhatib et al., 2021). Furthermore, chronic diseases can be prevented to reduce the incidence of multimorbidity. Prevention-based approaches usually focus on established risk factors, including smoking and alcohol consumption (NHS England, 2014). Thus, a combination of preventive lifestyle changes has also been proposed to be useful in preventing chronic diseases (Fortin et al., 2014; Krokstad et al., 2017). The morbidity of many NCDs, such as cardiovascular diseases (Odegaard et al., 2011), obesity (Matheson et al., 2012), cancer (Sasazuki et al., 2012), and stroke (Chiuve et al., 2008), has been reported to decrease with the accumulation of healthy lifestyles.
However, few studies have evaluated the relationship between the accumulation of multiple lifestyles and the prevalence of comorbidities in various age groups in China. Previous studies conducted in China have focused on middle-aged and elderly populations (Shao et al., 2021; Sun et al., 2021; S. Wang et al., 2017) or limited the scope of multimorbidity to cardiometabolic diseases (W. Chen et al., 2023; Han et al., 2021; Li et al., 2022). In this nationally representative study, we aimed to investigate what relationship there is between four lifestyle aspects (physical activity level, alcohol consumption, smoking history, and BMI) and the multimorbidity risk among 11,031 Chinese individuals aged ≥ 12 years. We hypothesise that there is a negative association between healthy lifestyles and the risk of multimorbidity.
Material and Methods
Study design and population
This survey is cross-sectional, seeking to recruit members of the Chinese population from across the country’s 31 provinces, with a multistage, stratified cluster sampling from July 2021 to September 2021. Firstly, in 31 participating provinces, one capital city and two to six non-capital cities were chosen through the random number table method, and 120 cities were chosen. Then, within each city, individuals were selected using a quota sampling strategy to ensure that socioeconomic characteristics (sex, age, and rural–urban distribution) of the study population were comparable to national population characteristics. Finally, a minimum of one trained investigative team was recruited from each city to collect 100–200 questionnaires via direct interaction. Uniform training was provided to the survey teams to ensure methodological uniformity and high-quality data collection. Investigators utilize online survey platforms to distribute questionnaires directly to the public within their designated areas, either through one-on-one sessions or face-to-face interactions. The population included was ≥ 12 years of age at enrollment, without mobility problems or mental abnormalities, resulting in 11,031 valid participants. To ensure the quality of responses, particularly from young adolescents or elderly respondents, investigators ensured informed consent was obtained before participation, and they were also tasked with recording the identifiers of the questionnaires. In scenarios where participants demonstrated the ability for verbal communication but were physically unable to engage with the survey instrument, investigators conducted individual interviews to record the responses on their behalf.
The questionnaire included the following facets: demographic information, a short-form Family Health Scale, and a 10-item Big Five Inventory.
Assessment of lifestyle
Modifiable lifestyle elements were smoking history, alcohol consumption, BMI, and physical activity levels. We asked participants about whether they currently smoke, used to smoke, or have never smoked, falling into categories of current smoker, ex-smoker, and non-smoker. Alcohol consumption was categorized according to frequency, type, and dosage as either light, heavy, or non-drinker. Nondrinkers comprised individuals who had not consumed any alcohol over the last year. Current light drinkers were males who consumed < 25 g of alcohol per day or females who consumed < 15 g of alcohol per day in the past year. Current heavy drinkers were defined as males who consumed > 25 g per day or females who consumed > 15 g per day in the past year. BMI was determined via self-reported weight (kg)/height (m)2 and was categorized into underweight (< 18.5 kg/m2), normal (18.5–24.0 kg/m2), and overweight/obese (≥ 24.0 kg/m2), based on Chinese criteria. Physical activity was determined by utilizing questions obtained from the International Physical Activity Questionnaire (IPAQ) (Craig et al., 2003). More specifically, we investigated physical activity by asking about the hours participants spent each week engaging in moderate-to-vigorous behaviors (such as swimming, cycling, and bodybuilding). The expenditure of metabolic equivalent (MET) hours each week was also added (Supplemental File 1). We grouped total MET (h/week) in tertiles and categorized it as inactivity (< 9.75 MET-h/week), median (9.75–26.25 MET-h/week), and activity (> 26.25 MET-h/week).
These four lifestyle factors were summarized to calculate a Healthy Lifestyle Profile (HLP) ranging from 0 (none) to 4 (all). A higher HLP indicated healthier lifestyle behaviors. Healthy smoking status in this study was coded as 0 if the respondent reported their status as an “ex-smoker” or “current smoker” and 1 if they reported their status as “non-smoker”. Healthy alcohol consumption was coded as “0” if the respondent reported their status as “current light drinker” or “current heavy drinker” (i.e., ever drinker) and 1 if they reported their status as “non-drinker”. Healthy BMI was coded as “0” if the BMI was “ < 18.5 kg/m2” or “ > 24 kg/m2” (i.e., underweight/overweight) and 1 if the BMI was “18.5–24.0 kg/m2” (i.e., normal). Healthy physical activity was categorized as inactivity (coded 0) and activity (coded 1) based on the median MET (< 20.3 MET-h/week [median of total physical activity for every participant]).
Multimorbidity
Multimorbidity was defined as living with two or more chronic conditions. This study collected self-reported medical history based on the physician’s diagnosis. Participants were asked, ‘Have you been diagnosed with any of the following diseases?’ with respect to 20 common conditions in Chinese people, including hypertension, asthma, dyslipidemia, chronic enteritis, thrombus, stroke, chronic gastritis, coronary heart disease, lumbar disc herniation, diabetes, neoplasms, chronic kidney disease, emotional disorders, osteoporosis, Parkinson’s disease, fatty liver disease, Alzheimer’s disease, Chronic Obstructive Pulmonary Disease (COPD), thyroid disease, and viral hepatitis. Individuals with two or more of these 20 diseases were classified as having multimorbidity.
Covariates
Other covariates included in the study were demographic characteristics: age (≤ 30, 31–45, 46–60, ≥ 60 years), sex (female/male), residence (rural/urban areas), and ethnicity (Han/others); socioeconomic factors: educational achievement (no formal school/primary school, middle school, secondary school, college/university, graduate), monthly income (≤ 3000, 3001–4500, 4501–7500, ≥ 7500 Chinese Yuan), and health insurance (no/yes)).
Statistical analysis
We calculated the frequencies and percentages for descriptive analyses. Multimorbidity presence as well as chronic disease number (no disease, 1 disease, 2 diseases, ≥ 3 diseases) for every healthy lifestyle profile (0 to 4 range) were determined through percentages alongside 95% confidence intervals (CIs) with reference to the overall populous. Distinctions in the prevalence of healthy lifestyle profiles between different variables, including multimorbidity, were contrasted via the chi-squared test.
A three-stage regression analysis was conducted. To start, multivariable logistic regression models were used as a means of examining the relationship between single lifestyle aspects and multimorbidity (yes/no). Three logistic models were fitted: (i) unadjusted, (ii) adjusted for age and sex, and (iii) adjusted for age, sex, residence, education, income, insurance, and ethnicity. Second, the correlates of HLP with multimorbidity (yes/no) were analyzed using multivariate logistic regression. Third, a multinomial logit regression model was used with the aim of examining the relationship between HLP and the chronic diseases number (no disease, one disease, two diseases, and ≥ three diseases). The ‘no disease’ category was the reference group.
To demonstrate potential interaction effects among these four lifestyle factors and show which combination generates the best performance in reducing odds of multimorbidity, joint associations of double lifestyle factors and all four lifestyle factors and multimorbidity were assessed using multivariable logistic regression models, adjusted for sex, age, residence, education, income, insurance status, and ethnicity.
To explore the differential association of HLP with multimorbidity in the population groups, we performed subgroup analyses stratified by age and residence using multivariate regression analyses. Findings are reported as odds ratios (OR) and 95% CIs. The estimates could be determined as statistically notable if the P-values were lower than 0.05. All evaluations were conducted through R software (version 4.2.1).
Results
Overall, 11,031 participants aged ≥ 12 years from 31 provinces were included. (Table 1) The demographic, socioeconomic, lifestyle, and morbidity attributes of all participants according to the HLP score categories are presented in Table 1. Most of the participants were < 60 years of age: 42% of the total study population were < 30 years old, 27% were 31–45 years old, 20% were 46–60 years old, and 10% were > 60 years of age. Approximately two-thirds of the participants were physically inactive, 40% had ever consumed alcohol, 39% were underweight or overweight, and 20% were ever smokers. At baseline, 475 (4%) participants had no healthy lifestyle, 1604 (15%) had one HLP, 3553 (32%) had two HLP, 4098 (37%) had three HLP, and 1301 (12%) had four HLP. Overall, 18% of the study population had at least one disease, and 5.9% had multimorbidity. Multimorbid participants had a higher prevalence of unhealthy lifestyles than participants who did not have multimorbidity. Participants with > 2 HLP were more likely to be younger, female, have higher monthly income and have higher education as compared to participants with 0–2 HLP.
Associations of single lifestyle and HLP with multimorbidity
All four lifestyle factors had independent and statistically significant associations with multimorbidity risk. (Table 2) Current heavy drinkers had a strong positive association with multimorbidity with an adjusted OR of 3.00 (95% CI, 2.10 to 4.27). Current light drinkers also had a positive association with multimorbidity with an adjusted OR of 1.29 (95% CI, 1.06 to 1.57). In comparison to never-smokers, current smokers and ex-smokers both had a 1.5 times higher risk of multimorbidity. Compared to participants with normal BMI, underweight participants were positively associated with multimorbidity with an adjusted OR of 1.42 (95% CI, 1.07 to 1.90).
HLP has a strong inverse association with the risk of multimorbidity. Participants with 1 HLP had a 34% lower multimorbidity risk (adjusted OR, 0.66; 95% CI, 0.48 to 0.92), participants with 2 HLP had a 55% lower multimorbidity risk (adjusted OR, 0.45; 95% CI, 0.32 to 0.62), participants with 3 HLP had a 70% lower multimorbidity risk (adjusted OR, 0.30; 95% CI, 0.21 to 0.43), and those with 4 HLP had a 73% lower multimorbidity risk (adjusted OR, 0.27; 95% CI, 0.17 to 0.43), compared to those with 0 HLP. (Table 3).
Associations of HLP with the number of chronic diseases
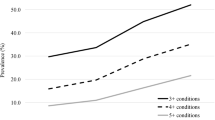
Table 3 reveals an inverse dose–response dynamic between the HLP and chronic disease numbers. The risk of having two diseases was 35% lower for the 1 HLP group (OR 0.65, 95% CI 0.44 to 0.96), 54% lower in the 2 HLP groups (OR 0.44, 95% CI 0.29 to 0.64), 75% lower in the 3 HLP groups (OR 0.25, 95% CI 0.17 to 0.38), and 78% lower in the 4 HLP groups (OR 0.22, 95% CI 0.13 to 0.39), compared to the 0 HLP group in the fully adjusted model. Moreover, the risk of having more than three chronic diseases was 54% lower in the 1 HLP group, 76% lower in the 2 HLP group, 84% lower in the 3 HLP group, and 87% lower for the 4 HLP group, in comparison with the 0 HLP group. Stratified results align with the main findings, indicating an inverse relationship between HLP and multimorbidity risk, most notably in individuals under 60 and urban residents with four HLPs (Figs. 1 and 2).
Joint Associations of Lifestyle Factors
Extending the analysis to encompass all four lifestyle behaviors, a composite of all healthy behaviors was significantly related to reduced multimorbidity risk (OR: 0.92; 95% CI: 0.90, 0.94), as presented in Fig. 3. The most marked protective effect was observed in individuals who maintained healthy drinking habits and physical activity levels despite unhealthy smoking and body weight (U.H.H.U), corresponding to an OR of 0.91 (95% CI: 0.86, 0.96). Furthermore, even in the presence of unhealthy smoking, drinking, and physical activity, healthy body weight alone (U.U.U.H) was related to reduced multimorbidity risk (OR: 0.92; 95% CI: 0.89, 0.94), indicating the considerable impact of maintaining healthy body weight.
Joint association of all healthy lifestyle factors and multimorbidity. Models adjusted for sex, age, residence, education, income, insurance, and ethnicity. Notation: 'H' represents Healthy and 'U' represents Unhealthy across lifestyle factors. In the sequence 'H.H.H.H’ to “U.U.U.U”, each position corresponds to a specific lifestyle factor—1st to Smoking, 2nd to Drinking, 3rd to Physical Activity, and 4th to Body Weight. For instance, 'H.H.H.U' indicates an individual who does not smoke (Healthy), does not drink (Healthy), engages in physical activity (Healthy), but is underweight/overweight (Unhealthy). Color shoud be used for this figure in print
The joint association analysis, examining the interplay between pairs of lifestyle factors, demonstrated that participants adhering to two healthy behaviors had lower odds of multimorbidity when contrasted with those engaging in two unhealthy behaviors. For instance, individuals who neither smoked nor drank had a 4% decrease in multimorbidity risk (OR: 0.96; 95% CI: 0.95, 0.98) relative to their counterparts with both risk factors (Panels A, Fig. 4). Moreover, those who were nonsmokers and maintained a normal weight showed an OR of 0.92 (95% CI: 0.91, 0.94), suggesting a more substantial reduction in odds compared to the reference group. Notably, maintaining a normal body weight appeared to be a significant protective factor across various combinations, as seen in Panels C, E, and F (Fig. 4).
Associations of HLP with multimorbidity, stratified by age and region
Figure 1 represents the age-stratified odds of multimorbidity for individuals with different HLPs. For participants aged < 60 years, a greater number of HLP was related to decreased multimorbidity risk. Participants aged < 30 years with 4 HLP had the lowest risk of multimorbidity (OR 0.09 (95% 0.02, 0.48). For participants aged > 60 years, no statistically notable relationship between lifestyle and multimorbidity could be distinguished.
Figure 2 represents the association between HLP and the risk of multimorbidity when stratified by region. Regardless of region, HLP was inversely associated with multimorbidity. The protective effects of healthier HLP were greater among participants from urban areas compared to those from rural areas. For example, participants living in urban areas with 4 HLP had the smallest multimorbidity risk (OR 0.22, 95% CI 0.12, 0.37). Among participants living in rural areas, those with 4 HLP had a 60% lower multimorbidity risk (odds ratio [OR] 0.40, 95% CI 0.17: 0.97).
Discussion
This study evaluated the relationship between four lifestyle characteristics (physical activity level, alcohol consumption, smoking history, and BMI) and multimorbidity risk. According to research, ours is the initial investigation in China with the aim of analyzing how lifestyle impacts the risk of multimorbidity in age groups ranging from under 18 to over 80 years. The results of this study indicate that common lifestyle habits, either alone or in combination, are associated with the risk of multimorbidity. We found a dose–response association between the number of healthy lifestyles and multimorbidity risk, which persisted significantly after adjusting for demographic factors. Individuals who followed four healthy lifestyles had an 86% lower risk of multimorbidity than those who did not. Within this group, those with four healthy lifestyles had an 87% lower risk of developing three diseases than those with zero. Overall, the risk of multimorbidity was lower for participants with several healthy lifestyles than for those with no healthy lifestyles, and the risk of multimorbidity was reduced with an increasing number of healthy lifestyles, regardless of the number of diseases.
In a large cohort from seven European nations, a healthy lifestyle, according to the HLP score, was clearly related to the risk of multimorbidity for cancer and cardiometabolic diseases (Freisling et al., 2020). Findings from the Finnish 25–64-year-old cohort revealed that smoking, a lack of physical activity, and a high BMI are unhealthy lifestyles that predispose the intact population to multimorbidity (Wikström et al., 2015, pp. 1982–2012). Similarly, in a Japanese 40–79-year-old population-based large-scale prospective study, the number of healthy lifestyle behaviors had a strong inverse association with death from coronary heart disease, total cardiovascular disease, and stroke (Eguchi et al., 2012). The results from the West of Scotland Twenty-07 Cohort Study demonstrated that five lifestyle factors (diet, BMI, physical activity, alcohol, and smoking) were effective in predicting the development of multimorbidity (Katikireddi et al., 2017). Cross-sectional data from Canada revealed that obesity and sedentary lifestyles increase the risk of multimorbidity (Geda et al., 2021). Similar to the above studies, we focused on the relationship between multiple lifestyles and the prevalence of multimorbidity in China. However, in our study, in addition to the above-mentioned cancers, cardiometabolic diseases, stroke, coronary heart disease, and diabetes, we increased the number of chronic diseases assessed to more than 20, among which also included mental diseases such as emotional disorders besides chronic diseases in the physical level. The age range of the study population was extended from under 18 to over 80 years. Most importantly, our study was stratified based on all age groups to analyze the relationship between lifestyle and the risk of multimorbidity in all age groups. We found that the healthier lifestyle developed at a young age was associated with a lower risk of comorbidity. Thus, the incorporation of a healthy lifestyle earlier in life would have a greater impact on people’s health. For older adults, aging (Fortin et al., 2005), weakness in physical function, and other factors, such as healthcare utilization, have a greater impact on the risk of multimorbidity than lifestyle factors. As compared with other potential factors associated with the risk of multimorbidity, including genetic factors and environment (e.g., socioeconomic status), lifestyle is more feasible to change at an early age. Although this study focuses primarily on the improvement of healthy lifestyles for physical diseases, it has also been shown that there is a positive association between different dimensions of mental health and well-being (Hautekiet et al., 2022). This study revealed that early intervention would have a significant impact on reducing the risk of multimorbidity. This work also characterizes the effect of age- and lifestyle-related factors on multimorbidity and, thus, provides potential direction for future research.
In addition to age stratification, place of residence was also used for stratification. The relationship between a healthy lifestyle and reduced multimorbidity risk was stronger in urban areas than in rural areas. It is well known that an individual's living environment affects their health (Marmot et al., 2008). An Algerian study on urban–rural lifestyle risk factor differences revealed that the lifestyle risk factors are not isolated, and their prevalence varies according to living areas (Kerkadi et al., 2021). First, the difficulty of urban residents in adopting healthy lifestyle habits may have contributed to our findings, which are supported by an Indonesian investigation that portrayed how urban residents are considerably more vulnerable than their rural counterparts in terms of disease (Hussain et al., 2015). Reasons behind this on an international scale can be attributed to how urban areas are typically more polluted, meaning that health outcomes for locals are considerably disrupted (Bridge, 2012). Alongside this, those in rural communities typically engage in physical labor to a greater extent than urban citizens, which is one of the factors that contribute to lower obesity rates for the former demographic as well as lower vulnerability to NCDs (Singh et al., 2011; van Zyl et al., 2020). To focus specifically on China, which is the selected location for our study, it has been proposed that those living in urban areas are more likely to develop multimorbidity in contrast with those in rural areas (Fan et al., 2022; Yi et al., 2019). Meanwhile, the prevalence of diabetes and dyslipidemia in urban areas as compared to rural China was 3.2% (S. H. Yang et al., 2010) and 8.8% (Pan et al., 2016) higher, respectively, and the prevalence of cancers such as breast, thyroid, lip, kidney, oral cavity, colon, prostrate, and pharynx, was also higher in urban areas (Yuan & Xie, 2021). Even so, there is a lack of dedicated investigations in China that have sought to investigate the dynamic between multiple lifestyles and multimorbidity risk with a region of residence for stratification. The mechanisms underlying this difference based on region are not yet clear and require further research. Regardless of the specific relevance, the promotion of a healthy lifestyle for people living in urban areas, especially those with multimorbidity, should be advocated.
The study examined the interplay between the four elements – BMI, alcohol consumption, physical activity, and smoking—and was concerned about their interaction effect on multimorbidity. Compared to the reference group with all four unhealthy factors, either all four or three of these factors are in a healthy state; the results reliably demonstrated a significant decrease in multimorbidity risk, with average odds ratios dropping to as low as 0.92. Regardless of the health status of smoking, alcohol consumption, and physical activity, normal body weight is heavily connected to a reduction in multimorbidity risk. Furthermore, within the six combinations of these four factors, the results indicate that the risk of multimorbidity is significantly reduced for all paired combinations of healthy lifestyles. Similarly, the inclusion of normal body weight, whether in combination with other healthy or unhealthy lifestyle factors, remains a significant protective factor against multimorbidity. In other words, maintaining a healthy body weight offers protection against multimorbidity, and combinations that include a normal body weight have the best performance in enhancing public health.
In the analysis of single factors, individuals with normal BMI also represent the lowest risk of multimorbidity. According to the results of this study, those with a normal BMI are at a 48% lower risk of multimorbidity than people who are overweight or underweight. For reference, normal weight was defined as between 18.5 and 24.9 kg/m2. A study in Canada with participants ≥ 12 years of age living in ten provinces demonstrated that as BMI increased, the likelihood of multimorbidity increased significantly (Geda et al., 2021). Furthermore, the prevalence of multimorbidity increased with each BMI category, peaking in obese category III (Jovic et al., 2016). However, the correlation between BMI and mortality was consistent with the U-shaped relationship between BMI and the risk of multimorbidity in our study. In a large prospective cohort study that lasted 32 years in the United States, the correlation between BMI and mortality was lowest within the BMI range of 18.5–22.4 kg/m2 when adjusted for all four lifestyle factors—dietary habits, physical activity level, smoking habits, and alcohol consumption (Veronese et al., 2016). Few studies have evaluated the relationship between being underweight and multimorbidity. A Swiss study of 12-year BMI trajectories in older adults revealed a significant association between early weight loss and rapid development of multimorbidity later in life (Calderón-Larrañaga et al., 2021). Weight loss is not only a manifestation of several chronic diseases (Vetrano et al., 2018; von Haehling et al., 2017) but may also predict the prodromal phase of forthcoming death (Alley et al., 2010; C. Chen et al., 2019). A longitudinal survey of the Taiwanese ageing population also showed a significant positive association between being underweight and depression (Chang & Yen, 2012). Meanwhile, an unhealthy lifestyle is thought to impair the body's repair function and accelerate aging, thus causing weight loss (Veronese et al., 2016). Therefore, a lower BMI may be a marginal manifestation of the remaining factors that lead to increased multimorbidity, which partly explains our finding that normal weight is a protective factor against multimorbidity.
As expected, people who were currently exercising had a 45% lower risk of developing multimorbidity than those who were not exercising. Previous studies have similarly demonstrated a notable negative relationship between physical activity levels and multimorbidity (Geda et al., 2021). However, physical activity is also negatively correlated with mortality in individuals with multimorbidity (Chudasama et al., 2019). Maintaining a high level of physical activity can help improve free function and thus prevent or improve the symptoms of many age-related chronic diseases (Duggal et al., 2019). Interestingly, individualized aerobic exercise training (Lo et al., 2020) and self-management plans (Khunti et al., 2021) can be used to encourage people who reduce their usual exercise levels due to multimorbidity.
For alcohol consumption and smoking behavior, the risk of comorbidity was reduced by 22% and 61% for non-drinkers and non-smokers, respectively. After adjusting for demographic factors, the positive correlation between these two lifestyle factors and the risk of multimorbidity remained significant. A study conducted in Canada on modifiable lifestyle risk factors and their associations with the first chronic disease revealed that compared to alcohol consumption, BMI, diet, and physical inactivity, heavy cigarette smoking was strongly associated with the risk of at least one of these chronic diseases (Ng et al., 2020). Smoking behavior was also significantly associated with persistent unhealthy psychological states (Menassa et al., 2023). A study from India on women aged 15–49 years revealed that smoking and alcohol consumption increased their multimorbidity risk by 18% as compared to their counterparts (Mishra et al., 2021).
Strengths and limitations
This is the primary nationally representative investigation that has explored the dynamic between a healthy lifestyle profile and multimorbidity in Chinese people from under 18 years to over 80 years. We also provide updated information to facilitate assessment and understanding of the health status of participants from different age groups and regions. This study highlights the importance of healthy lifestyle interventions to prevent multimorbidity as well as treatment programs for people in resource-limited settings.
Our study has some limitations. First, smoking, alcohol consumption, physical activity, BMI, and chronic diseases were measured based on self-reported questionnaires; therefore, measurement errors and recall bias may exist. Second, as this was a cross-sectional and observational study, we could not analyze the causal relationship between lifestyle and multimorbidity; thus, the relationships could be influenced by reverse causation. Further prospective studies in the Chinese population are needed as a means of assessing what impact a healthy lifestyle has on multimorbidity risk. Third, we did not analyze different patterns of multimorbidity, considering only the number of chronic diseases. However, most of our study population was younger than 45 years, and the number of people with multimorbidity was relatively small compared with previous studies. The largest comorbidity number in this study was three; therefore, it was not suitable for cluster analysis. Fourth, we only considered four common lifestyle factors, and other factors, including diet, sleep duration, and other lifestyle factors, can be included in further analysis.
Conclusions
In summary, our results revealed that a healthier smoking status, alcohol consumption, physical activity, and BMI were associated with a reduced multimorbidity risk. We found a dose–response association between the number of healthy lifestyles and multimorbidity risk. Individuals who followed four healthy lifestyle profiles had an 86% lower risk of multimorbidity than those who did not. We also found that the healthier the lifestyle the people develop at a younger age, the lower the risk of multimorbidity. Overall, our findings identify health-related factors that reduce multimorbidity and provide insights for the healthcare system to design health-promoting programs. Future research is needed to determine an effective approach for the whole population to advocate for a healthier lifestyle in public health guidelines.
Data Availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- HLP:
-
Healthy Lifestyle Profile
- NCDs:
-
Non-communicable Diseases
- BMI:
-
Body Mass Index
- IPAQ:
-
International Physical Activity Questionnaire
- MET:
-
Expenditure of metabolic equivalent
- COPD:
-
Chronic Obstructive Pulmonary Disease
- OR:
-
Odds Ratio
- CI:
-
Confidence Intervals
References
Alkhatib, A., Nnyanzi, L. A., Mujuni, B., Amanya, G., & Ibingira, C. (2021). Preventing Multimorbidity with Lifestyle Interventions in Sub-Saharan Africa: A New Challenge for Public Health in Low and Middle-Income Countries. International Journal of Environmental Research and Public Health, 18(23), 12449. https://doi.org/10.3390/ijerph182312449
Alley, D. E., Metter, E. J., Griswold, M. E., Harris, T. B., Simonsick, E. M., Longo, D. L., & Ferrucci, L. (2010). Changes in weight at the end of life: Characterizing weight loss by time to death in a cohort study of older men. American Journal of Epidemiology, 172(5), 558–565. https://doi.org/10.1093/aje/kwq168
Barnett, K., Mercer, S. W., Norbury, M., Watt, G., Wyke, S., & Guthrie, B. (2012). Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet (london, England), 380(9836), 37–43. https://doi.org/10.1016/S0140-6736(12)60240-2
Bridge, C. (2012). Cities, environmental stressors, ageing and chronic disease. Australasian Journal on Ageing, 31(3), 140. https://doi.org/10.1111/j.1741-6612.2012.00628.x
Calderón-Larrañaga, A., Hu, X., Guo, J., Ferrucci, L., Xu, W., & Vetrano, D. L. (2021). Body mass trajectories and multimorbidity in old age: 12-year results from a population-based study. Clinical Nutrition (edinburgh, Scotland), 40(12), 5764–5770. https://doi.org/10.1016/j.clnu.2021.10.012
Chang, H.-H., & Yen, S. T. (2012). Association between obesity and depression: Evidence from a longitudinal sample of the elderly in Taiwan. Aging & Mental Health, 16(2), 173–180. https://doi.org/10.1080/13607863.2011.605053
Chen, C., Ye, Y., Zhang, Y., Pan, X.-F., & Pan, A. (2019). Weight change across adulthood in relation to all cause and cause specific mortality: Prospective cohort study. BMJ (clinical Research Ed.), 367, l5584. https://doi.org/10.1136/bmj.l5584
Chen, W., Wang, X., Chen, J., You, C., Ma, L., Zhang, W., & Li, D. (2023). Household air pollution, adherence to a healthy lifestyle, and risk of cardiometabolic multimorbidity: Results from the China health and retirement longitudinal study. The Science of the Total Environment, 855, 158896. https://doi.org/10.1016/j.scitotenv.2022.158896
Chiuve, S. E., Rexrode, K. M., Spiegelman, D., Logroscino, G., Manson, J. E., & Rimm, E. B. (2008). Primary prevention of stroke by healthy lifestyle. Circulation, 118(9), 947–954. https://doi.org/10.1161/CIRCULATIONAHA.108.781062
Chudasama, Y. V., Khunti, K. K., Zaccardi, F., Rowlands, A. V., Yates, T., Gillies, C. L., Davies, M. J., & Dhalwani, N. N. (2019). Physical activity, multimorbidity, and life expectancy: A UK Biobank longitudinal study. BMC Medicine, 17(1), 108. https://doi.org/10.1186/s12916-019-1339-0
Craig, C. L., Marshall, A. L., Sjöström, M., Bauman, A. E., Booth, M. L., Ainsworth, B. E., Pratt, M., Ekelund, U., Yngve, A., Sallis, J. F., & Oja, P. (2003). International physical activity questionnaire: 12-country reliability and validity. Medicine and Science in Sports and Exercise, 35(8), 1381–1395. https://doi.org/10.1249/01.MSS.0000078924.61453.FB
de Almeida, M. G. N., Nascimento-Souza, M. A., Lima-Costa, M. F., & Peixoto, S. V. (2020). Lifestyle factors and multimorbidity among older adults (ELSI-Brazil). European Journal of Ageing, 17(4), 521–529. https://doi.org/10.1007/s10433-020-00560-z
Divo, M. J., Martinez, C. H., & Mannino, D. M. (2014). Ageing and the epidemiology of multimorbidity. The European Respiratory Journal, 44(4), 1055–1068. https://doi.org/10.1183/09031936.00059814
Duggal, N. A., Niemiro, G., Harridge, S. D. R., Simpson, R. J., & Lord, J. M. (2019). Can physical activity ameliorate immunosenescence and thereby reduce age-related multi-morbidity? Nature Reviews. Immunology, 19(9), 563–572. https://doi.org/10.1038/s41577-019-0177-9
Eguchi, E., Iso, H., Tanabe, N., Wada, Y., Yatsuya, H., Kikuchi, S., Inaba, Y., Tamakoshi, A., & Japan Collaborative Cohort Study Group. (2012). Healthy lifestyle behaviours and cardiovascular mortality among Japanese men and women: The Japan collaborative cohort study. European Heart Journal, 33(4), 467–477. https://doi.org/10.1093/eurheartj/ehr429
Emerging Risk Factors Collaboration, Di Angelantonio, E., Kaptoge, S., Wormser, D., Willeit, P., Butterworth, A. S., Bansal, N., O’Keeffe, L. M., Gao, P., Wood, A. M., Burgess, S., Freitag, D. F., Pennells, L., Peters, S. A., Hart, C. L., Håheim, L. L., Gillum, R. F., Nordestgaard, B. G., Psaty, B. M., … Danesh, J. (2015). Association of Cardiometabolic Multimorbidity With Mortality. JAMA, 314(1), 52–60. https://doi.org/10.1001/jama.2015.7008.
Espeland, M. A., Gaussoin, S. A., Bahnson, J., Vaughan, E. M., Knowler, W. C., Simpson, F. R., Hazuda, H. P., Johnson, K. C., Munshi, M. N., Coday, M., & Pi-Sunyer, X. (2020). Impact of an 8-Year Intensive Lifestyle Intervention on an Index of Multimorbidity. Journal of the American Geriatrics Society, 68(10), 2249–2256. https://doi.org/10.1111/jgs.16672
Fan, J., Sun, Z., Yu, C., Guo, Y., Pei, P., Yang, L., Chen, Y., Du, H., Sun, D., Pang, Y., Zhang, J., Gilbert, S., Avery, D., Chen, J., Chen, Z., Lyu, J., Li, L., & China Kadoorie Biobank Collaborative Group. (2022). Multimorbidity patterns and association with mortality in 0.5 million Chinese adults. Chinese Medical Journal, 135(6), 648–657. https://doi.org/10.1097/CM9.0000000000001985.
Fortin, M., Lapointe, L., Hudon, C., Vanasse, A., Ntetu, A. L., & Maltais, D. (2004). Multimorbidity and quality of life in primary care: A systematic review. Health and Quality of Life Outcomes, 2, 51. https://doi.org/10.1186/1477-7525-2-51
Fortin, M., Bravo, G., Hudon, C., Vanasse, A., & Lapointe, L. (2005). Prevalence of multimorbidity among adults seen in family practice. Annals of Family Medicine, 3(3), 223–228. https://doi.org/10.1370/afm.272
Fortin, M., Haggerty, J., Almirall, J., Bouhali, T., Sasseville, M., & Lemieux, M. (2014). Lifestyle factors and multimorbidity: A cross sectional study. BMC Public Health, 14, 686. https://doi.org/10.1186/1471-2458-14-686
Freisling, H., Viallon, V., Lennon, H., Bagnardi, V., Ricci, C., Butterworth, A. S., Sweeting, M., Muller, D., Romieu, I., Bazelle, P., Kvaskoff, M., Arveux, P., Severi, G., Bamia, C., Kühn, T., Kaaks, R., Bergmann, M., Boeing, H., Tjønneland, A., … Ferrari, P. (2020). Lifestyle factors and risk of multimorbidity of cancer and cardiometabolic diseases: A multinational cohort study. BMC Medicine, 18(1), 5. https://doi.org/10.1186/s12916-019-1474-7
Geda, N. R., Janzen, B., & Pahwa, P. (2021). Chronic disease multimorbidity among the Canadian population: Prevalence and associated lifestyle factors. Archives of Public Health = Archives Belges De Sante Publique, 79(1), 60. https://doi.org/10.1186/s13690-021-00583-7
Han, Y., Hu, Y., Yu, C., Guo, Y., Pei, P., Yang, L., Chen, Y., Du, H., Sun, D., Pang, Y., Chen, N., Clarke, R., Chen, J., Chen, Z., Li, L., Lv, J., & China Kadoorie Biobank Collaborative Group. (2021). Lifestyle, cardiometabolic disease, and multimorbidity in a prospective Chinese study. European Heart Journal, 42(34), 3374–3384. https://doi.org/10.1093/eurheartj/ehab413
Haug, N., Deischinger, C., Gyimesi, M., Kautzky-Willer, A., Thurner, S., & Klimek, P. (2020). High-risk multimorbidity patterns on the road to cardiovascular mortality. BMC Medicine, 18(1), 44. https://doi.org/10.1186/s12916-020-1508-1
Hautekiet, P., Saenen, N. D., Martens, D. S., Debay, M., Van der Heyden, J., Nawrot, T. S., & De Clercq, E. M. (2022). A healthy lifestyle is positively associated with mental health and well-being and core markers in ageing. BMC Medicine, 20(1), 328. https://doi.org/10.1186/s12916-022-02524-9
Hou, B., Nazroo, J., Banks, J., & Marshall, A. (2019). Are cities good for health? A study of the impacts of planned urbanization in China. International Journal of Epidemiology, 48(4), 1083–1090. https://doi.org/10.1093/ije/dyz031
Hussain, M. A., Huxley, R. R., & Al Mamun, A. (2015). Multimorbidity prevalence and pattern in Indonesian adults: An exploratory study using national survey data. British Medical Journal Open, 5(12), e009810. https://doi.org/10.1136/bmjopen-2015-009810
Jani, B. D., Hanlon, P., Nicholl, B. I., McQueenie, R., Gallacher, K. I., Lee, D., & Mair, F. S. (2019). Relationship between multimorbidity, demographic factors and mortality: Findings from the UK Biobank cohort. BMC Medicine, 17(1), 74. https://doi.org/10.1186/s12916-019-1305-x
Jovic, D., Marinkovic, J., & Vukovic, D. (2016). Association between body mass index and prevalence of multimorbidity: A cross-sectional study. Public Health, 139, 103–111. https://doi.org/10.1016/j.puhe.2016.05.014
Katikireddi, S. V., Skivington, K., Leyland, A. H., Hunt, K., & Mercer, S. W. (2017). The contribution of risk factors to socioeconomic inequalities in multimorbidity across the lifecourse: A longitudinal analysis of the Twenty-07 cohort. BMC Medicine, 15(1), 152. https://doi.org/10.1186/s12916-017-0913-6
Kerkadi, A., Al Mannai, H., Saad, D., Yakti, F. A. Z., Attieh, G., & Bawadi, H. (2021). Clustering of Lifestyle Risk Factors among Algerian Adolescents: Comparison between Urban and Rural Areas: GSHS Data. International Journal of Environmental Research and Public Health, 18(13), 7072. https://doi.org/10.3390/ijerph18137072
Khunti, K., Highton, P. J., Waheed, G., Dallosso, H., Redman, E., Batt, M. E., Davies, M. J., Gray, L. J., Herring, L. Y., Mani, H., Rowlands, A., & Yates, T. (2021). Promoting physical activity with self-management support for those with multimorbidity: A randomised controlled trial. The British Journal of General Practice: The Journal of the Royal College of General Practitioners, 71(713), e921–e930. https://doi.org/10.3399/BJGP.2021.0172
King, D. E., Mainous, A. G., & Geesey, M. E. (2007). Turning back the clock: Adopting a healthy lifestyle in middle age. The American Journal of Medicine, 120(7), 598–603. https://doi.org/10.1016/j.amjmed.2006.09.020
Kivimäki, M., Strandberg, T., Pentti, J., Nyberg, S. T., Frank, P., Jokela, M., Ervasti, J., Suominen, S. B., Vahtera, J., Sipilä, P. N., Lindbohm, J. V., & Ferrie, J. E. (2022). Body-mass index and risk of obesity-related complex multimorbidity: An observational multicohort study. The Lancet. Diabetes & Endocrinology, 10(4), 253–263. https://doi.org/10.1016/S2213-8587(22)00033-X
Krokstad, S., Ding, D., Grunseit, A. C., Sund, E. R., Holmen, T. L., Rangul, V., & Bauman, A. (2017). Multiple lifestyle behaviours and mortality, findings from a large population-based Norwegian cohort study—The HUNT Study. BMC Public Health, 17(1), 58. https://doi.org/10.1186/s12889-016-3993-x
La, D. T. V., Zhao, Y., Arokiasamy, P., Atun, R., Mercer, S., Marthias, T., McPake, B., Pati, S., Palladino, R., & Lee, J. T. (2022). Multimorbidity and out-of-pocket expenditure for medicines in China and India. BMJ Global Health, 7(11), e007724. https://doi.org/10.1136/bmjgh-2021-007724
Lai, F. T. T., Wong, S. Y. S., Yip, B. H. K., Guthrie, B., Mercer, S. W., Chung, R. Y., Chung, G. K. K., Chau, P. Y. K., Wong, E. L. Y., Woo, J., & Yeoh, E.-K. (2019). Multimorbidity in middle age predicts more subsequent hospital admissions than in older age: A nine-year retrospective cohort study of 121,188 discharged in-patients. European Journal of Internal Medicine, 61, 103–111. https://doi.org/10.1016/j.ejim.2018.12.001
Li, D., Wang, L., Zhou, Z., Song, L., Chen, S., Yang, Y., Hu, Y., Wang, Y., Wu, S., & Tian, Y. (2022). Role of socioeconomic, lifestyle, and clinical factors in the progression of cardiometabolic multimorbidity in China: A 10-year prospective cohort study. Nutrition, Metabolism, and Cardiovascular Diseases: NMCD, 32(10), 2383–2391. https://doi.org/10.1016/j.numecd.2022.06.016
Lo, Y.-P., Chiang, S.-L., Lin, C.-H., Liu, H.-C., & Chiang, L.-C. (2020). Effects of Individualized Aerobic Exercise Training on Physical Activity and Health-Related Physical Fitness among Middle-Aged and Older Adults with Multimorbidity: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 18(1), 101. https://doi.org/10.3390/ijerph18010101
Lujic, S., Randall, D. A., Simpson, J. M., Falster, M. O., & Jorm, L. R. (2022). Interaction effects of multimorbidity and frailty on adverse health outcomes in elderly hospitalised patients. Scientific Reports, 12(1), 14139. https://doi.org/10.1038/s41598-022-18346-x
Makovski, T. T., Schmitz, S., Zeegers, M. P., Stranges, S., & van den Akker, M. (2019). Multimorbidity and quality of life: Systematic literature review and meta-analysis. Ageing Research Reviews, 53, 100903. https://doi.org/10.1016/j.arr.2019.04.005
Malecki, S. L., Van Mil, S., Graffi, J., Breetvelt, E., Corral, M., Boot, E., Chow, E. W. C., Sanches, M., Verma, A. A., & Bassett, A. S. (2020). A genetic model for multimorbidity in young adults. Genetics in Medicine: Official Journal of the American College of Medical Genetics, 22(1), 132–141. https://doi.org/10.1038/s41436-019-0603-1
Marmot, M., Friel, S., Bell, R., Houweling, T. A. J., Taylor, S., Commission on Social Determinants of Health. (2008). Closing the gap in a generation: Health equity through action on the social determinants of health. Lancet (London, England), 372(9650), 1661–1669. https://doi.org/10.1016/S0140-6736(08)61690-6
Matheson, E. M., King, D. E., & Everett, C. J. (2012). Healthy lifestyle habits and mortality in overweight and obese individuals. Journal of the American Board of Family Medicine: JABFM, 25(1), 9–15. https://doi.org/10.3122/jabfm.2012.01.110164
Menassa, M., Wesenhagen, K., Stronks, K., Franco, O. H., Verschuren, W., & Picavet, H. (2023). Individual mental health patterns and the role of lifestyle among ageing adults over 20 years—The Doetinchem Cohort Study. Archives of Gerontology and Geriatrics, 115, 105222. https://doi.org/10.1016/j.archger.2023.105222
Mishra, V. K., Srivastava, S., & Murthy, P. V. (2021). Population attributable risk for multimorbidity among adult women in India: Do smoking tobacco, chewing tobacco and consuming alcohol make a difference? PLoS ONE, 16(11), e0259578. https://doi.org/10.1371/journal.pone.0259578
Ng, R., Sutradhar, R., Yao, Z., Wodchis, W. P., & Rosella, L. C. (2020). Smoking, drinking, diet and physical activity-modifiable lifestyle risk factors and their associations with age to first chronic disease. International Journal of Epidemiology, 49(1), 113–130. https://doi.org/10.1093/ije/dyz078
NHS England. (2014). Five Year Forward View. https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf
Odegaard, A. O., Koh, W.-P., Gross, M. D., Yuan, J.-M., & Pereira, M. A. (2011). Combined lifestyle factors and cardiovascular disease mortality in Chinese men and women: The Singapore Chinese health study. Circulation, 124(25), 2847–2854. https://doi.org/10.1161/CIRCULATIONAHA.111.048843
Pan, L., Yang, Z., Wu, Y., Yin, R.-X., Liao, Y., Wang, J., Gao, B., Zhang, L., & China National Survey of Chronic Kidney Disease Working Group. (2016). The prevalence, awareness, treatment and control of dyslipidemia among adults in China. Atherosclerosis, 248, 2–9. https://doi.org/10.1016/j.atherosclerosis.2016.02.006
Pathirana, T. I., & Jackson, C. A. (2018). Socioeconomic status and multimorbidity: A systematic review and meta-analysis. Australian and New Zealand Journal of Public Health, 42(2), 186–194. https://doi.org/10.1111/1753-6405.12762
Picavet, H. S. J., Wendel-vos, G. C. W., Vreeken, H. L., Schuit, A. J., & Verschuren, W. M. M. (2011). How stable are physical activity habits among adults? The Doetinchem Cohort Study. Medicine and Science in Sports and Exercise, 43(1), 74–79. https://doi.org/10.1249/MSS.0b013e3181e57a6a
Rocca, W. A., Grossardt, B. R., Boyd, C. M., Chamberlain, A. M., Bobo, W. V., & St Sauver, J. L. (2021). Multimorbidity, ageing and mortality: Normative data and cohort study in an American population. British Medical Journal Open, 11(3), e042633. https://doi.org/10.1136/bmjopen-2020-042633
Salisbury, C. (2012). Multimorbidity: Redesigning health care for people who use it. The Lancet, 380(9836), 7–9. https://doi.org/10.1016/S0140-6736(12)60482-6
Sasazuki, S., Inoue, M., Iwasaki, M., Sawada, N., Shimazu, T., Yamaji, T., Tsugane, S., & JPHC Study Group. (2012). Combined impact of five lifestyle factors and subsequent risk of cancer: The Japan Public Health Center Study. Preventive Medicine, 54(2), 112–116. https://doi.org/10.1016/j.ypmed.2011.11.003
Schermer, E. E., Engelfriet, P. M., Blokstra, A., Verschuren, W. M. M., & Picavet, H. S. J. (2022). Healthy lifestyle over the life course: Population trends and individual changes over 30 years of the Doetinchem Cohort Study. Frontiers in Public Health, 10, 966155. https://doi.org/10.3389/fpubh.2022.966155
Shao, J., Wang, X., Zou, P., Song, P., Chen, D., Zhang, H., Tang, L., Huang, Q., & Ye, Z. (2021). Associating modifiable lifestyle factors with multimorbidity in community dwelling individuals from mainland China. European Journal of Cardiovascular Nursing, 20(6), 556–564. https://doi.org/10.1093/eurjcn/zvaa038
Singh, G. K., Siahpush, M., Hiatt, R. A., & Timsina, L. R. (2011). Dramatic increases in obesity and overweight prevalence and body mass index among ethnic-immigrant and social class groups in the United States, 1976–2008. Journal of Community Health, 36(1), 94–110. https://doi.org/10.1007/s10900-010-9287-9
Sun, Z. J., Fan, J. N., Yu, C. Q., Guo, Y., Bian, Z., Pei, P., Du, H. D., Chen, J. S., Chen, Z. M., Lyu, J., & Li, L. M. (2021). [Prevalence, patterns and long-term changes of multimorbidity in adults from 10 regions of China]. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi, 42(5), 755–762. https://doi.org/10.3760/cma.j.cn112338-20200305-00259
Tommola, M., Ilmarinen, P., Tuomisto, L. E., Lehtimäki, L., Niemelä, O., Nieminen, P., & Kankaanranta, H. (2019). Cumulative effect of smoking on disease burden and multimorbidity in adult-onset asthma. The European Respiratory Journal, 54(3), 1801580. https://doi.org/10.1183/13993003.01580-2018
van Zyl, S., van Rooyen, F. C., Joubert, G., Kruger, W. H., & Walsh, C. M. (2020). A Comparison of the Socio-Behavioral-Metabolic Risk Profiles and Associated Factors for Chronic Diseases of Lifestyle in Urban and Rural Communities in Central South Africa. Frontiers in Public Health, 8, 570676. https://doi.org/10.3389/fpubh.2020.570676
Veronese, N., Li, Y., Manson, J. E., Willett, W. C., Fontana, L., & Hu, F. B. (2016). Combined associations of body weight and lifestyle factors with all cause and cause specific mortality in men and women: Prospective cohort study. BMJ (clinical Research Ed.), 355, i5855. https://doi.org/10.1136/bmj.i5855
Vetrano, D. L., Pisciotta, M. S., Laudisio, A., Lo Monaco, M. R., Onder, G., Brandi, V., Fusco, D., Di Capua, B., Ricciardi, D., Bernabei, R., & Zuccalà, G. (2018). Sarcopenia in Parkinson Disease: Comparison of Different Criteria and Association With Disease Severity. Journal of the American Medical Directors Association, 19(6), 523–527. https://doi.org/10.1016/j.jamda.2017.12.005
von Haehling, S., Ebner, N., Dos Santos, M. R., Springer, J., & Anker, S. D. (2017). Muscle wasting and cachexia in heart failure: Mechanisms and therapies. Nature Reviews. Cardiology, 14(6), 323–341. https://doi.org/10.1038/nrcardio.2017.51
Wang, H. H. (2014). Epidemiology of multimorbidity in China and implications for the healthcare system: Cross-sectional survey among 162,464 community household residents in southern China. 12. https://doi.org/10.1186/s12916-014-0188-0.
Wang, S., Wu, Y., Ungvari, G. S., Ng, C. H., Forester, B. P., Gatchel, J. R., Chiu, H. F. K., Kou, C., Fu, Y., Qi, Y., Yu, Y., Li, B., & Xiang, Y.-T. (2017). Sleep duration and its association with demographics, lifestyle factors, poor mental health and chronic diseases in older Chinese adults. Psychiatry Research, 257, 212–218. https://doi.org/10.1016/j.psychres.2017.07.036
Wikström, K., Lindström, J., Harald, K., Peltonen, M., & Laatikainen, T. (2015). Clinical and lifestyle-related risk factors for incident multimorbidity: 10-year follow-up of Finnish population-based cohorts 1982–2012. European Journal of Internal Medicine, 26(3), 211–216. https://doi.org/10.1016/j.ejim.2015.02.012
World Health Organization. (2013). Global action plan for the prevention and control of noncommunicable diseases 2013–2020. World Health Organization. https://apps.who.int/iris/handle/10665/94384. Accessed 3 Feb 2023.
Yang, S. H., Dou, K. F., & Song, W. J. (2010). Prevalence of diabetes among men and women in China. The New England Journal of Medicine, 362(25), 2425–2426; author reply 2426. https://doi.org/10.1056/NEJMoa0908292.
Yang, H.-L., Mo, B.-R., Molassiotis, A., Wang, M., He, G.-L., & Xie, Y. J. (2022). Relationship between multimorbidity and composite lifestyle status in Shenzhen. China. Journal of Multimorbidity and Comorbidity, 12, 26335565221123990. https://doi.org/10.1177/26335565221123990
Yi, J. Y., Kim, H., & Chi, I. (2019). Urban-rural differences in multimorbidity and associated factors in China and Korea: A population-based survey study. Geriatrics & Gerontology International, 19(11), 1157–1164. https://doi.org/10.1111/ggi.13771
Yuan, S., & Xie, S.-H. (2021). Urban-rural disparity in cancer incidence in China, 2008–2012: A cross-sectional analysis of data from 36 cancer registers. British Medical Journal Open, 11(4), e042762. https://doi.org/10.1136/bmjopen-2020-042762
Zhang, Y., Zhou, L., Liu, S., Qiao, Y., Wu, Y., Ke, C., & Shen, Y. (2020). Prevalence, correlates and outcomes of multimorbidity among the middle-aged and elderly: Findings from the China Health and Retirement Longitudinal Study. Archives of Gerontology and Geriatrics, 90, 104135. https://doi.org/10.1016/j.archger.2020.104135
Zhang, Q., Han, X., Zhao, X., & Wang, Y. (2022). Multimorbidity patterns and associated factors in older Chinese: Results from the China health and retirement longitudinal study. BMC Geriatrics, 22(1), 470. https://doi.org/10.1186/s12877-022-03154-9
Zhu, N. B., Zhou, M., Yu, C. Q., Guo, Y., Bian, Z., Tan, Y. L., Pei, P., Chen, J. S., Chen, Z. M., Lyu, J., Li, L. M., & China Kadoorie Biobank Collaborative Group. (2019). [Prevalence of “healthy lifestyle” in Chinese adults]. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi, 40(2), 136–141. https://doi.org/10.3760/cma.j.issn.0254-6450.2019.02.003
Acknowledgements
We thank all the investigator’s effort in the questionnaire collecting process and the participants for their contributions to the study.
Funding
This research received no specific grant from any funding agency in the public, commercial or not for profit sectors.
Author information
Authors and Affiliations
Contributions
XZ: conceived the study with support from SZ and RZ. XZ, SZ, and RZ: conducted main literature review. SZ: conducted the data analysis. XZ, SZ, and RZ: did the data interpretation. YW: contributed to the administration of the project. XZ, SZ, RZ, KX, YG, and HM wrote the first draft of the paper. KX, YG and HM reviewed and revised the manuscript. All authors discussed and agreed on the implications of the study findings and approved the final version to be published. All authors have materially participated in the research and article preparation. All authors have approved the final article.
Corresponding author
Ethics declarations
Competing interests
There is no competing interests to declare.
Ethics approval and consent to participate
Ethical approval was granted by the Ethics Committee of Jinan University and informed consent was required from all participants. The ethical approval number is JNUKY-2021–018. The study was conducted in accordance with the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zou, X., Zou, S., Zhang, R. et al. Association of Lifestyle Factors with Multimorbidity Risk in China: A National Representative Study. Applied Research Quality Life 19, 1411–1435 (2024). https://doi.org/10.1007/s11482-024-10291-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11482-024-10291-3