Abstract
Background
The Tablo Hemodialysis System is a new innovative kidney replacement therapy (KRT) providing a range of options for critically ill patients with acute kidney injury. The use of various effluent rate and treatment durations/frequencies may clear antibiotics differently than traditional KRT. This Monte Carlo Simulation (MCS) study was to develop antibiotic doses likely to attain therapeutic targets for various KRT combinations.
Methods
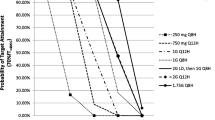
Published body weights and pharmacokinetic parameter estimates were used to predict drug exposure for cefepime, ceftazidime, imipenem, meropenem and piperacillin/tazobactam in virtual critically ill patients receiving five KRT regimens. Standard free β-lactam plasma concentration time above minimum inhibitory concentration targets (40–60%fT> MIC and 40–60%fT> MICx4) were used as efficacy targets. MCS assessed the probability of target attainment (PTA) and likelihood of toxicity for various antibiotic dosing strategies. The smallest doses attaining PTA ≥ 90% during 1-week of therapy were considered optimal.
Results
MCS determined β-lactam doses achieving ∼90% PTA in all KRT options. KRT characteristics influenced antibiotic dosing. Cefepime and piperacillin/tazobactam regimens designed for rigorous efficacy targets were likely to exceed toxicity thresholds.
Conclusion
The flexibility offered by new KRT systems can influence β-lactam antibiotic dosing, but doses can be devised to meet therapeutic targets. Further clinical validations are warranted.
Similar content being viewed by others
Background
Sepsis remains the primary cause of death in critically ill patients requiring kidney replacement therapy (KRT) [1, 2]. KRT affects the pharmacokinetics (PK) and dosing of most antibiotic agents. While many reviews have been published outlining antibiotic dosing adjustments for standard KRTs [3,4,5], new KRT options are being used in practice without supporting dosing guidance. These new KRT regimens utilize different treatment frequencies, durations, and blood/dialysate/ultrafiltrate flow rates, and offer clinicians treatment flexibility to meet critically ill patients’ individual needs [6, 7]. However, some of these new KRT frequency/duration/flow rate combinations are likely to remove antibiotics differently than standard thrice-weekly intermittent hemodialysis or continuous KRT, requiring antibiotic dosage adjustment to attain meet therapeutic targets. It is not feasible to conduct clinical pharmacokinetic trials for all KRT options for all commonly used antibiotics in these patients. Consequently, Monte Carlo Simulations (MCS) that replicate various KRT regimens and that use published demographic and PK data derived from critically ill patients receiving KRT can be conducted to determine which dosing regimens are likely to meet therapeutic targets while minimizing the risk of toxicity [8,9,10,11,12]. This study was to predict optimal doses of five β-lactam antibiotics for various KRT regimens utilized in new innovative KRT systems.
Methods
Development of mathematical pharmacokinetic model
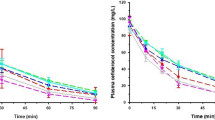
One compartment, first order PK models were developed to predict drug exposure of five β-lactam antibiotics (i.e. cefepime, ceftazidime, imipenem, meropenem and piperacillin/tazobactam) in virtual critically ill patients receiving KRT. Input parameters integrated into PK models were outlined in Table 1. Patient body weights were obtained from a large trial involving critically ill patients undergoing KRT [13] and the PK parameters with variances (i.e. standard deviation) were derived from pertinent PK studies on each study drug conducted in critically ill patients receiving KRT [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41]. Figure 1 depicts five simulated KRT settings: (1) thrice-weekly (Mon-Wed-Fri) 4-hour hemodialysis (HD) at dialysate flow rate (Qd) 300 ml/min, (2) daily 4-hour HD at Qd 300 ml/min, (3) daily sequential therapy consisting of 4-hour HD at Qd 300 ml/min followed by 20-hour ultrafiltration (UF) at ultrafiltrate flow rate (Quf) 5 ml/min, (4) daily 9-hour prolonged intermittent kidney replacement therapy (PIKRT) at Qd 100 ml/min, and (5) daily 24-hour extended PIKRT at Qd 50 ml/min. Transmembrane drug clearance in HD and UF is a function of effluent flow rate (i.e. Qd or Quf) and extraction coefficient. Regression analyses were performed utilizing published transmembrane drug clearance at various effluent flow rates [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28, 31,32,33,34,35,36, 38, 41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63]. The best fitting relationships were modeled to extrapolate extraction coefficient (i.e. saturation or sieving coefficient) at the desired effluent flow rates in KRT settings. Patients were assumed to be anuric adults with no residual renal function. Log-Gaussian distribution was assumed for all input parameters. The equations used in the PK model were as follows:
CLHD = SA x Qd.
CLUF = SC x Quf.
Ke_on = (CLNR + CLHD or UF)/Vd (intra-KRT period).
Ke_off = CLNR /Vd (inter-KRT period).
Where CLHD is the transmembrane clearance during HHD, SA is the saturation coefficient, SC is the sieving coefficient, Qd is the dialysate flow rate, Quf is the ultrafiltrate flow rate, Ke_on is the elimination rate constant during KRT, CLNR is non-renal clearance, Vd is volume of distribution, and Ke_off is the elimination rate constant between KRT treatments.
Pharmacodynamic & safety targets
The pharmacodynamic (PD) targets for study drugs were free plasma drug concentration time above the minimum inhibitory concentration (fT > MIC) of the pathogen for 40%, 50% and 60% of the dosing interval (40%, 50%, and 60% fT > MIC) for carbapenems (imipenem and meropenem), penicillin (piperacillin) and cephalosporins (cefepime and ceftazidime) respectively [64, 65]. Furthermore, the attainment of the free plasma drug concentrations exceeding four times MIC (fT > MICx4) is associated with maximal bacterial killing effect of β-lactams [66, 67]. Attaining this latter aggressive PD target has been recommended for critically ill patients to optimize clinical efficacy while preventing bacterial resistance [68]. Thus, we used each of these two PD targets (40%, 50% or 60% fT> MIC and 40%, 50% or 60% fT> MICx4) to predict the optimal drug doses in critically ill patients receiving KRT. For tazobactam, the target was to attain 50% free plasma drug concentration above the threshold concentration (50% fT > threshold) [69, 70]. Clinical and Laboratory Standards Institute susceptibility breakpoint MICs reported against the reference microorganism, Pseudomonas aeruginosa, were used to evaluate the probability of target attainment (PTA) of each dosing regimen: 2 mg/L for imipenem and meropenem, 16 mg/L for piperacillin with threshold tazobactam concentrations of 4 mg/L, and 8 mg/L for cefepime and ceftazidime [69].
In general, β-lactam antibiotics are considered safe and the dosing regimens are primarily determined by pharmacokinetic/pharmacodynamic target attainment. However, β-lactam-associated neurotoxicity has been correlated with high plasma concentrations and is more commonly reported in critically ill patients with kidney dysfunction [71,72,73,74,75,76]. Total plasma concentrations of > 64 mg/L and > 20 mg/L have been associated with increased neurotoxicity risk for meropenem and cefepime respectively [73,74,75]. A recent retrospective study suggested that the total piperacillin trough plasma concentrations of 157 mg/L in combination with tazobactam was linked to the incidence of neurologic disorders in critically ill patients [76]. No ceftazidime or imipenem studies have evaluated the relationship between neurotoxicity and plasma concentrations. However, it is suggested that free plasma concentrations should not exceed eight times the MIC for β-lactam antibiotics without validated toxicity threshold concentrations to lower the risk of toxicity [68]. We assessed the potential risk of neurotoxicity associated with each simulated drug dosing regimen by evaluating total plasma concentrations at the end of each day during one week of antibiotic therapy, using these suggested toxicity threshold concentrations (i.e. 20 mg/L, 64 mg/L, 157 mg/L, 16 mg/L, and 64 mg/L for cefepime, ceftazidime, piperacillin, imipenem and meropenem, respectively).
Monte Carlo simulation and optimal dosing regimen
Various dosing regimens of each study drug were simulated using 0.5-hour intermittent infusions. Additionally, 4-hour extended infusions were simulated for cefepime and piperacillin/tazobactam. In KRT settings 1–3, the initial doses were infused immediately after a 4-hour HD. For KRT setting 4 with daily 9-hour PIKRT, each drug dosing regimen was infused in the 2 scenarios representing the possible extreme infusion situations: (1) “Early PIKRT” where the initial dose is infused at the beginning of PIKRT and (2) “Late PIKRT” where the initial dose is given 15 h prior to PIKRT. Monte Carlo simulation (MCS) [Crystal Ball Classroom Edition, Oracle] generated a week of free plasma drug concentration-time profiles of each simulated dosing regimen in 5,000 virtual patients in each of 5 KRT settings. Then, the PTA of each simulated dosing regimen was calculated for the different PD targets. A dosing regimen was considered optimal if PTA was attained in ≥ 90% of 5,000 virtual patients with the smallest daily dose during one week of antibiotic therapy.
Results
MCS determined the optimal dosing regimens for all study antibiotics in all five KRT settings (Table 2). It is predicted that alterations in KRT regimens would influence on the PTA of dosing regimens, necessitating different antibiotic doses to attain desired efficacy targets. It should be noted that the clinical relevance and potential for toxicity were considered when selecting optimal doses for aggressive PD targets (40–60% fT> MICx4). Thus, when antibiotic dose regimens yielded a PTA slightly below 90%, particularly on day 1, but considered clinically acceptable, these regimens were deemed optimal. Furthermore, if achieving PTA of \( \ge \)90% necessitated a dose greater than the maximal conventional dose and/or substantially increased the risk of potential toxicity, antibiotic regimens with a PTA less than 90% were also accepted as optimal following a careful evaluation of benefits vs. risks. Overall, the recommended doses for thrice-weekly HD, daily HD, and sequential therapy (KRT settings 1–3) were consistent for all study antibiotics, while higher doses were needed for daily PIKRT therapy (settings 4 and 5). The PTAs of all simulated antibiotic doses in all five KRT settings were provided in supplementary materials.
Notably, the 9-hour PIKRT setting (KRT setting 4) presented a challenge in that two extreme dosing scenarios could potentially exist contingent upon the timing of antibiotic administration relative to the PIKRT. Antibiotic initial doses given at the initiation of 9-hour PIKRT (early PIKRT) yielded different antibiotic exposures compared to those infusions occurring 15 h before the 9-hour PIKRT (late PIKRT). However, our recommended antibiotic doses for 9-hour PIKRT setting achieved PTA ∼90% independent of when the antibiotic was infused in relation to PIKRT.
MCS also evaluated the safety of each antibiotic dosing regimen utilizing the suggested safety threshold from the literature. Overall, the potential for a substantial increase in neurotoxicity risk were more pronounced with the MCS-recommended cefepime and piperacillin/tazobactam dosing regimens designed to attain aggressive PD targets. Tables 3 and 4 present the probability of increased neurotoxicity risk with MCS-recommended cefepime and piperacillin/tazobactam dosing regimens respectively in all five KRT settings. The recommended ceftazidime dose for aggressive PD target (60% fT> MICx4) also elevated drug concentrations above the safety threshold in 25–52% of simulated patients in thrice-weekly HD (KRT setting 1). Additionally, the recommended imipenem doses for aggressive PD target (40% fT> MICx4) resulted in drug concentrations exceeding the safety threshold in 0.3–8.3% and 9.0-11.9% of the virtual cohort in thrice-weekly HD and Early 9-hour PIKRT settings, respectively. Further information on the potential neurotoxicity risk predicted with MCS-recommended dosing regimens for ceftazidime, imipenem and meropenem are reported in supplementary materials.
Discussion
This is the first study to attempt to develop common antibiotic dosing recommendations using MCS for the breadth of KRT options available for critically ill patients receiving newer KRT. MCS was able to identify plausible antibiotic doses in all five KRT settings that would attain PD targets. As aforementioned, the same antibiotic doses were recommended for KRT settings 1–3 [i.e. thrice-weekly HD, daily HD, and sequential therapy (4-hour HD, followed by 20-hour UF daily)]. However, a higher proportion of simulated patients exhibited an increased risk of drug-induced neurotoxicity in the thrice-weekly HD setting compared to daily HD or sequential therapy, attributed to less frequent HD sessions per week. The recommended antibiotic doses to attain less aggressive PD targets (40–60% fT> MIC) in these KRT settings 1–3 were similar to those recommended for end stage kidney disease patients with HD [77,78,79,80,81], while higher antibiotic doses were necessary to attain aggressive PD targets (40–60% fT> MICx4). For KRT settings 4 and 5 [i.e. 9-hour and extended PIKRT], the recommended antibiotic doses were 50–100% higher than those for KRT settings 1–3, except piperacillin/tazobactam.
The MCS analysis predicted that piperacillin/tazobactam 4.5 g q12h, and 4.5 g q8h or 3.375 g q6h would attain piperacillin PD targets of 50% fT> MIC and 50% fT> MICx4 respectively, while concurrently achieving the tazobactam target of 50% fT > threshold in KRT settings 1–4. It should be noted that these drug dosing regimens should be administered post-HD in KRT settings 1–3 but can be given regardless of the timing of 9-hour PIKRT in setting 4. The consistent piperacillin/tazobactam doses recommended for KRT settings 1–4 are likely due to preserved and robust piperacillin non-renal clearance observed in patients with AKI receiving KRT [38, 40, 41] and similar total piperacillin dialytic clearance during HD and 9-hour PIKRT. Piperacillin non-renal clearance is substantial (45.7 + 38.3 ml/min), and the frequency of KRT did not significantly influence PTA in simulated patients. Moreover, the estimated piperacillin extracorporeal clearances during HD with Qd 300 ml/min and 9-hour PIKRT with Qd 100 ml/min were ∼93 ml/min and ∼46 ml/min respectively. Consequently, total piperacillin removal during a 4-hour HD or a 9-hour PIKRT was comparable, resulting in similar PTA and the selection of the same optimal piperacillin dosing regimen in KRT settings 1–4. It should be also noted that for less aggressive PD target (50% fT> MIC), smaller piperacillin doses (i.e. 2 g q12h and 3 g q12h) than recommended (i.e. 4 g q12h) would attain 90% PTA in these KRT settings but the accompanying tazobactam doses (i.e. 0.25 g q12h and 0.375 g q12h) did not successfully attain the target of 50% fT > threshold. Attainment of acceptable PTA for 50% fT > threshold required tazobactam 0.5 g q12h. Thus, piperacillin/tazobactam 4.5 g q12h was chosen as the optimal regimen to meet both piperacillin and tazobactam targets in these KRT settings.
Extended infusion is a common strategy to maximize the time-dependent bactericidal activity of β-lactam antibiotics. In our MCS study, we evaluated the PTA of cefepime and piperacillin/tazobactam doses with extended infusion in critically ill patients receiving KRT. Administering these antibiotics with a 4-hour extended infusion resulted in a slight increase in PTA by 0–4% for cefepime and by 1–5% for piperacillin, respectively, compared to the same doses given via a 0.5-hour intermittent infusion. However, this PTA increase did not affect the selection of optimal cefepime and piperacillin/tazobactam doses in our analysis. Extended infusion was advantageous in achieving a PTA of ≥ 90% when cefepime and piperacillin doses with intermittent infusion yielded slightly below 90% PTA. For example, in KRT setting 2, piperacillin 4 g q8h with intermittent infusion resulted PTA 88–89%, but when administered with extended infusion, the PTA increased to 91–92%. Nevertheless, these PTA differences between intermittent vs. extended infusion did not appear clinically significant in our simulated patients.
β-lactam antibiotics are generally considered safe; however, in recent years, there has been an increasing recognition of neurological deterioration in critically ill patients receiving a β-lactam [72, 82]. In this MCS analysis, we also assessed the safety of each antibiotic dosing regimen at the end of each day over a 1-week treatment period and found a substantial increase in the risk of neurotoxicity with the recommended cefepime and piperacillin/tazobactam doses, particularly to attain the aggressive PD targets (Tables 3 and 4). Notably, the cefepime safety threshold used in our analysis (i.e., total trough concentration of ≥ 20 mg/L) would be approximately equivalent to a free drug concentration of 16 mg/L, assuming protein binding of 20% [16]. This safety threshold (16 mg/L) closely approaches the PD target threshold concentrations (MIC of 8 mg/L or MICx4 of 32 mg/L). Unavoidably, cefepime doses attaining the aggressive PD target yielded total cefepime concentration exceeding the safety threshold (16 mg/L) at the end of each simulated day in many simulated patients (58–99%). The MCS also indicated that piperacillin/tazobactam doses achieving the aggressive PD target would elevate the risk of neurotoxicity in up to 63% of virtual cohort. For safety reasons, we deemed cefepime and piperacillin/tazobactam doses slight below 90% of the PTA as optimal, if higher doses substantially increased the risk of neurotoxicity. Furthermore, we accepted the doses that resulted in PTAs of less than 80% on day 1, but consistently attained PTAs ∼90% for the remainder of the week. For instance, in early 9-hour PIKRT and extended PIKRT settings, cefepime 3 g LD then 1 g q6h and 2 g q8h yielded PTAs of 77% and 63% respectively on day 1 while maintaining PTA ∼90% for the rest of week. The MCS predicted that PTA ≥ 90% on day 1 to attain aggressive PD target in these KRT settings would require cefepime doses of up to 8 g/day exceeding the maximal conventional daily dose (6 g/day). Thus, we selected these cefepime doses as optimal not to exceed 6 g/day despite the lower PTA on day 1. With similar considerations, we accepted piperacillin/tazobactam doses as optimal for aggressive PD target in KRT settings 2–4, even though they resulted in PTAs of less than 80% on day 1, as they achieved PTA ∼90% for the rest of the week. When a clinician seeks to ensure target attainment on day 1, a higher cefepime or piperacillin/tazobactam LD may be prescribed on day 1, after evaluating the benefits vs. toxicity risk based on the MCS results provided in this report.
Clinicians should be vigilant about the potential risk of neurotoxicity with the recommended cefepime and piperacillin/tazobactam doses in simulated KRT settings. They also should practice careful monitoring to detect any clinical manifestations of neurotoxicity. If available, therapeutic drug monitoring (TDM) should be performed to optimize antibiotic therapy. Currently, β-lactam TDM is more commonly utilized in hospitals in some European countries and Australia but has been limited to research purposes in the U.S. and other regions [83, 84]. In clinical settings where β-lactam TDM is not readily accessible, clinicians should carefully weigh the benefits and risks based on the PTA and the potential neurotoxicity risk predicted in our MCS analyses. For patients at a high risk of neurotoxicity, clinicians should consider using cefepime and piperacillin/tazobactam doses designed to attain less aggressive PD targets or an alternative antibiotic.
This study has several limitations. First, we modelled the virtual patients based on published body weight and pharmacokinetic parameters derived from critically ill patients undergoing KRTs. We assumed that these virtual patients were anuric adults receiving uninterrupted KRT sessions. Additionally, our modeling was limited to only 5 KRT regimens. Therefore, the applicability of our MCS findings is confined to individuals matching to the modeled patient characteristics and receiving one of the modeled KRT settings. All the studied β-lactam antibiotics are primarily eliminated via the kidneys and are readily dialyzable. Consequently, patients with residual or improving kidney function might require higher doses than recommended, while prolonged interruptions in KRT may necessitate lower doses. Secondly, our study assumed a serious infection with P. aeruginosa in determining the initial β-lactam dosing recommendations. The susceptibility MIC breakpoints for P. aeruginosa are typically higher than those for other Enterobacterales [69]. If a different pathogen with lower MICs (e.g. <8 mg/L for cefepime and ceftazidime; <16 mg/L for piperacillin/tazobactam; <2 mg/L for imipenem and meropenem) is identified as the cause of infection, clinicians may consider reducing the initial dosing regimens based on the susceptibility results. Lastly, this study predicts that cefepime and piperacillin/tazobactam doses aimed to attain aggressive PD targets would result in plasma drug concentrations exceeding safety thresholds, thereby increasing the risk of neurotoxicity. It is strongly advisable that clinicians carefully assess the benefits and risks predicted with these regimens when considering treatment for this vulnerable patient population.
Conclusions
Innovative KRT systems allow clinicians wider KRT flexibility than ever before. MCS was able to predict dosing recommendations for five commonly used β-lactam antibiotics for critically ill patients receiving wide variations in KRT applications. Vigilant monitoring for antibiotic adverse effects when attempting to attain aggressive PD targets is essential, especially for cefepime and piperacillin/tazobactam.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AKI:
-
acute kidney injury
- fT > MIC :
-
time of free-serum concentration above the minimum inhibitory concentration
- HD:
-
hemodialysis
- KRT:
-
kidney replacement therapy
- MCS:
-
Monte Carlo Simulations
- PIKRT:
-
prolonged intermittent kidney replacement therapy
- PK:
-
pharmacokinetic
- PD:
-
pharmacodynamic
- PTA:
-
probability of target attainment
- TDM:
-
therapeutic drug monitoring
References
Vaara ST, Pettilä V, Reinikainen M, Kaukonen KM. Finnish Intensive Care Consortium. Population-based incidence, mortality and quality of life in critically ill patients treated with renal replacement therapy: a nationwide retrospective cohort study in Finnish intensive care units. Crit Care. 2012;16(1):R13.
Bagshaw SM, Laupland KB, Doig CJ, Mortis G, Fick GH, Mucenski M, et al. Prognosis for long-term survival and renal recovery in critically ill patients with severe acute renal failure: a population-based study. Crit Care. 2005;9(6):R700–9.
Hoff BM, Maker JH, Dager WE, Heintz BH. Antibiotic dosing for critically ill adult patients receiving intermittent hemodialysis, prolonged intermittent renal replacement therapy, and continuous renal replacement therapy: an update. Ann Pharmacother. 2020;54(1):43–55.
Pistolesi V, Morabito S, Di Mario F, Regolisti G, Cantarelli C, Fiaccadori E. A guide to understanding Antimicrobial Drug Dosing in critically ill patients on renal replacement therapy. Antimicrob Agents Chemother. 2019;63(8):e00583–19.
Jang SM, Lewis SJ, Mueller BA. Harmonizing antibiotic regimens with renal replacement therapy. Expert Rev Anti Infect Ther. 2020;18(9):887–95.
Heung M, Yessayan L. Renal replacement therapy in Acute kidney Injury: controversies and Consensus. Crit Care Clin. 2017;33(2):365–78.
Zaman T, Moore K, Jellerson J, Chahal Y, Schumacher J, Dalessandri-Silva C, et al. Extension of Tablo TrEatmeNt Duration (XTEND) study: successful 24 h prolonged therapy with Tablo in critical patients. BMC Nephrol. 2022;23(1):338.
Carlier M, Taccone FS, Beumier M, Seyler L, Cotton F, Jacobs F, Roberts JA. Population pharmacokinetics and dosing simulations of cefepime in septic shock patients receiving continuous renal replacement therapy. Int J Antimicrob Agents. 2015;46(4):413–9.
Lewis SJ, Kays MB, Mueller BA. Use of Monte Carlo Simulations to Determine Optimal Carbapenem Dosing in critically ill patients receiving prolonged intermittent renal replacement therapy. J Clin Pharmacol. 2016;56(10):1277–87.
Chaijamorn W, Charoensareerat T, Srisawat N, Pattharachayakul S, Boonpeng A. Cefepime dosing regimens in critically ill patients receiving continuous renal replacement therapy: a Monte Carlo simulation study. J Intensive Care. 2018;6:61.
Jang SM, Gharibian KN, Lewis SJ, Fissell WH, Tolwani AJ, Mueller BA. A Monte Carlo simulation approach for β-lactam dosing in critically ill patients receiving prolonged intermittent renal replacement therapy. J Clin Pharmacol. 2018;58:1254–65.
Sember AM, LoFaso ME, Lewis SJ. An optimal extended-infusion dosing of cefepime and ceftazidime in critically ill patients with continuous renal replacement therapy. J Crit Care. 2022;69:154011.
Bagshaw SM, Wald R, Adhikari NKJ, Bellomo R, da Costa BR, Dreyfuss D, et al. Timing of initiation of renal-replacement therapy in acute kidney injury. N Engl J Med. 2020;383(3):240–51.
Allaouchiche B, Breilh D, Jaumain H, Gaillard B, Renard S, Saux MC. Pharmacokinetics of cefepime during continuous venovenous hemodiafiltration. Antimicrob Agents Chemother. 1997;41(11):2424–7.
Malone RS, Fish DN, Abraham E, Teitelbaum I. Pharmacokinetics of cefepime during continuous renal replacement therapy in critically ill patients. Antimicrob Agents Chemother. 2001;45(11):3148–55.
Isla A, Gascón AR, Maynar J, Arzuaga A, Toral D, Pedraz JL. Cefepime and continuous renal replacement therapy (CRRT): in vitro permeability of two CRRT membranes and pharmacokinetics in four critically ill patients. Clin Ther. 2005;27(5):599–608.
Philpott CD, Droege CA, Droege ME, Healy DP, Courter JD, Ernst NE, et al. Pharmacokinetics and pharmacodynamics of extended-infusion cefepime in critically ill patients receiving continuous renal replacement therapy: a prospective, open-label study. Pharmacotherapy. 2019;39(11):1066–76.
Mariat C, Venet C, Jehl F, Mwewa S, Lazarevic V, Diconne E, Fonsale N, Carricajo A, Guyomarc’h S, Vermesch R, Aubert G, Bidault R, Bertrand JC, Zeni F. Continuous infusion of ceftazidime in critically ill patients undergoing continuous venovenous haemodiafiltration: pharmacokinetic evaluation and dose recommendation. Crit Care. 2006;10(1):R26.
König C, Braune S, Roberts JA, Nierhaus A, Steinmetz OM, Baehr M, Frey OR, Langebrake C, Kluge S. Population pharmacokinetics and dosing simulations of ceftazidime in critically ill patients receiving sustained low-efficiency dialysis. J Antimicrob Chemother. 2017;72(5):1433–40.
Isla A, Gascon AR, Maynar J, Arzuaga A, Sanchez-Izquierdo JA, Pedraz JL. In vitro AN69 and polysulphone membrane permeability to ceftazidime and in vivo pharmacokinetics during continuous renal replacement therapies. Chemotherapy. 2007;53(3):194–201.
Kinowski JM, de la Coussaye JE, Bressolle F, Fabre D, Saissi G, Bouvet O, et al. Multiple-dose pharmacokinetics of amikacin and ceftazidime in critically ill patients with septic multiple-organ failure during intermittent hemofiltration. Antimicrob Agents Chemother. 1993;37(3):464–73.
Afshartous D, Bauer SR, Connor MJ, Aduroja OA, Amde M, Salem C, et al. Pharmacokinetics and pharmacodynamics of meropenem and imipenem in critically ill patients treated with continuous venovenous hemodialysis. Am J Kidney Dis. 2014;63(1):170–1.
Boucher BA, Hudson JQ, Hill DM, Swanson JM, Wood GC, Laizure SC, et al. Pharmacokinetics of imipenem/cilastatin burn intensive care unit patients undergoing high-dose continuous venovenous hemofiltration. Pharmacotherapy. 2016;36(12):1229–37.
Fish DN, Teitelbaum I, Abraham E. Pharmacokinetics and pharmacodynamics of imipenem during continuous renal replacement therapy in critically ill patients. Antimicrob Agents Chemother. 2005;49(6):2421–8.
Mueller BA, Scarim SK, Macias WL. Comparison of imipenem pharmacokinetics in patients with acute or chronic renal failure treated with continuous hemofiltration. Am J Kidney Dis. 1993;21(2):172–9.
Hashimoto S, Honda M, Yamaguchi M, Sekimoto M, Tanaka Y. Pharmacokinetics of imipenem and cilastatin during continuous venovenous hemodialysis in patients who are critically ill. ASAIO J. 1997;43(1):84–8.
Vos MC, Vincent HH, Yzerman EP. Clearance of imipenem/cilastatin in acute renal failure patients treated by continuous hemodiafiltration (CAVHD). Intensive Care Med. 1992;18(5):282–5.
Kihara M, Ikeda Y, Shibata K, Masumori S, Ebira H, Shiratori K, et al. Pharmacokinetic profiles of intravenous imipenem/cilastatin during slow hemodialysis in critically ill patients. Clin Nephrol. 1994;42(3):193–7.
Primaxin [package insert]. Whitehouse Station. NJ: Merck Sharp & Dohme Corp; 2016.
Tegeder I, Bremer F, Oelkers R, Schobel H, Schüttler J, Brune K, et al. Pharmacokinetics of imipenem-cilastatin in critically ill patients undergoing continuous venovenous hemofiltration. Antimicrob Agents Chemother. 1997;41(12):2640–5.
Isla A, Maynar J, Sánchez-Izquierdo JA, Gascón AR, Arzuaga A, Corral E, et al. Meropenem and continuous renal replacement therapy: in vitro permeability of 2 continuous renal replacement therapy membranes and influence of patient renal function on the pharmacokinetics in critically ill patients. J Clin Pharmacol. 2005;45:1294–304.
Robatel C, Decosterd LA, Biollaz J, Eckert P, Schaller MD, Buclin T. Pharmacokinetics and dosage adaptation of meropenem during continuous venovenous hemodiafiltration in critically ill patients. J Clin Pharmacol. 2003;43:1329–40.
Langgartner J, Vasold A, Glück T, Reng M, Kees F. Pharmacokinetics of meropenem during intermittent and continuous intravenous application in patients treated by continuous renal replacement therapy. Intensive Care Med. 2008;34(6):1091–6.
Giles LJ, Jennings AC, Thompson AH, Creed G, Beale RJ, McLuckie A. Pharmacokinetics of meropenem in intensive care unit patients receiving continuous veno-venous hemofiltration or hemodiafiltration. Crit Care Med. 2000;28:632–7.
Bilgrami I, Roberts JA, Wallis SC, Thomas J, Davis J, Fowler S, et al. Meropenem dosing in critically ill patients with sepsis receiving high-volume continuous venovenous hemofiltration. Antimicrob Agents Chemother. 2010;54(7):2974–8.
Krueger WA, Schroeder TH, Hutchison M, Hoffmann E, Dieterich HJ, Heininger A, et al. Pharmacokinetics of meropenem in critically ill patients with acute renal failure treated by continuous hemodiafiltration. Antimicrob Agents Chemother. 1998;42(9):2421–4.
Merrem. (meropenem) [package insert]. Wilmington, DE: AstraZeneca Pharmaceuticals, LP.; 2014.
Mueller SC, Majcher-Peszynska J, Hickstein H, Francke A, Pertschy A, Schulz M, et al. Pharmacokinetics of piperacillin-tazobactam in anuric intensive care patients during continuous venovenous hemodialysis. Antimicrob Agents Chemother. 2002;46(5):1557–60.
Seyler L, Cotton F, Taccone FS, De Backer D, Macours P, Vincent JL, et al. Recommended β-lactam regimens are inadequate in septic patients treated with continuous renal replacement therapy. Crit Care. 2011;15(3):R137.
Bauer SR, Salem C, Connor MJ Jr, Groszek J, Taylor ME, Wei P, et al. Pharmacokinetics and pharmacodynamics of piperacillin-tazobactam in 42 patients treated with concomitant CRRT. Clin J Am Soc Nephrol. 2012;7(3):452–7.
Keller E, Bohler J, Busse-Grawitz A, Reetze-Bonorden P, Krumme B, Schollmeyer P. Single dose kinetics of piperacillin during continuous arteriovenous hemodialysis in intensive care patients. Clin Nephrol. 1995;43(Suppl 1):20–S23.
Jang SM, Gharibian KN, Lewis SJ, Fissell WH, Tolwani AJ, Mueller BA. A Monte Carlo simulation approach for beta-lactam dosing in critically ill patients receiving prolonged intermittent renal replacement therapy. J Clin Pharmacol. 2018;58(10):1254–65.
Schmaldienst S, Traunmüller F, Burgmann H, Rosenkranz AR, Thalhammer-Scherrer R, Hörl WH, et al. Multiple-dose pharmacokinetics of cefepime in long-term hemodialysis with high-flux membranes. Eur J Clin Pharmacol. 2000;56(1):61–4.
Barbhaiya RH, Knupp CA, Forgue ST, Matzke GR, Guay DR, Pittman KA. Pharmacokinetics of cefepime in subjects with renal insufficiency. Clin Pharmacol Ther. 1990;48(3):268–76.
Matzke GR, Frye RF, Joy MS, Palevsky PM. Determinants of ceftazidime clearance by continuous venovenous hemofiltration and continuous venovenous hemodialysis. Antimicrob Agents Chemother. 2000;44(6):1639–44.
Verpooten GA, Verbist L, Buntinx AP, Entwistle LA, Jones KH, De Broe ME. The pharmacokinetics of imipenem (thienamycin-formamidine) and the renal dehydropeptidase inhibitor cilastatin sodium in normal subjects and patients with renal failure. Br J Clin Pharmacol. 1984;18(2):183–93.
Konishi K, Suzuki H, Saruta T, Hayashi M, Deguchi N, Tazaki H, et al. Removal of imipenem and cilastatin by hemodialysis in patients with end-stage renal failure. Antimicrob Agents Chemother. 1991;35(8):1616–20.
Tegeder I, Neumann F, Bremer F, Brune K, Lötsch J, Geisslinger G. Pharmacokinetics of meropenem in critically ill patients with acute renal failure undergoing continuous venovenous hemofiltration. Clin Pharmacol Ther. 1999;65(1):50–7.
Braune S, König C, Roberts JA, Nierhaus A, Steinmetz O, Baehr M, et al. Pharmacokinetics of meropenem in septic patients on sustained low-efficiency dialysis: a population pharmacokinetic study. Crit Care. 2018;22(1):25.
Leroy A, Fillastre JP, Borsa-Lebas F, Etienne I, Humbert G. Pharmacokinetics of meropenem (ICI 194,660) and its metabolite (ICI 213,689) in healthy subjects and in patients with renal impairment. Antimicrob Agents Chemother. 1992;36(12):2794–8.
Christensson BA, Nilsson-Ehle I, Hutchison M, Haworth SJ, Oqvist B, Norrby SR. Pharmacokinetics of meropenem in subjects with various degrees of renal impairment. Antimicrob Agents Chemother. 1992;36(7):1532–7.
Donnellan S, Wright DFB, Roberts JA, Duffull SB, Schollum JBW, Putt TL, Wallis SC, Walker RJ. The pharmacokinetics of meropenem and piperacillin-tazobactam during sustained low efficiency haemodiafiltration (SLED-HDF). Eur J Clin Pharmacol. 2020;76(2):239–47.
Rubino CM, Bhavnani SM, Loutit JS, Lohse B, Dudley MN, Griffith DC. Single-dose pharmacokinetics and safety of Meropenem-Vaborbactam in subjects with chronic renal impairment. Antimicrob Agents Chemother. 2018;62(3):e02103–17.
Arzuaga A, Isla A, Gascón AR, Maynar J, Corral E, Pedraz JL. Elimination of piperacillin and tazobactam by renal replacement therapies with AN69 and polysulfone hemofilters: evaluation of the sieving coefficient. Blood Purif. 2006;24(4):347–54.
Varghese JM, Jarrett P, Boots RJ, Kirkpatrick CM, Lipman J, Roberts JA. Pharmacokinetics of piperacillin and tazobactam in plasma and subcutaneous interstitial fluid in critically ill patients receiving continuous venovenous haemodiafiltration. Int J Antimicrob Agents. 2014;43(4):343–8.
Asín-Prieto E, Rodríguez-Gascón A, Trocóniz IF, Soraluce A, Maynar J, Sánchez-Izquierdo JÁ, et al. Population pharmacokinetics of piperacillin and tazobactam in critically ill patients undergoing continuous renal replacement therapy: application to pharmacokinetic/pharmacodynamic analysis. J Antimicrob Chemother. 2014;69(1):180–9.
Awissi DK, Beauchamp A, Hébert E, Lavigne V, Munoz DL, Lebrun G, et al. Pharmacokinetics of an extended 4-hour infusion of piperacillin-tazobactam in critically ill patients undergoing continuous renal replacement therapy. Pharmacotherapy. 2015;35(6):600–7.
Sinnollareddy MG, Roberts MS, Lipman J, Peake SL, Roberts JA. Pharmacokinetics of piperacillin in critically ill patients with acute kidney injury receiving sustained low-efficiency diafiltration. J Antimicrob Chemother. 2018;73(6):1647–50.
Kanji S, Roberts JA, Xie J, Alobaid A, Zelenitsky S, Hiremath S, et al. Piperacillin population pharmacokinetics in critically ill adults during sustained low-efficiency dialysis. Ann Pharmacother. 2018;52(10):965–73.
Donnellan S, Wright DFB, Roberts JA, Duffull SB, Schollum JBW, Putt TL, et al. The pharmacokinetics of meropenem and piperacillin-tazobactam during sustained low efficiency haemodiafiltration (SLED-HDF). Eur J Clin Pharmacol. 2020;76(2):239–47.
Heim-Duthoy KL, Halstenson CE, Abraham PA, Matzke GR. The effect of hemodialysis on piperacillin harmacokinetics. Int J Clin Pharmacol Ther Toxicol. 1986;24(12):680–4.
Johnson CA, Halstenson CE, Kelloway JS, Shapiro BE, Zimmerman SW, Tonelli A, et al. Single-dose pharmacokinetics of piperacillin and tazobactam in patients with renal disease. Clin Pharmacol Ther. 1992;51(1):32–41.
Wooley M, Miller B, Krishna G, Hershberger E, Chandorkar G. Impact of renal function on the pharmacokinetics and safety of ceftolozane-tazobactam. Antimicrob Agents Chemother. 2014;58(4):2249–55.
Drusano GL. Antimicrobial pharmacodynamics: critical interactions of ‘bug and drug’. Nat Rev Microbiol. 2004;2(4):289–300.
Vogelman B, Gudmundsson S, Leggett J, Turnidge J, Ebert S. CraigWA. Correlation of antimicrobial pharmacokinetic parameters with therapeutic efficacy in an animal model. J Infect Dis. 1988;158(4):831–47.
Tam VH, McKinnon PS, Akins RL, Rybak MJ, Drusano GL. Pharmacodynamics of cefepime in patients with gram-negative infections. J Antimicrob Chemother. 2002;50(3):425–8.
McKinnon PS, Paladino JA, Schentag JJ. Evaluation of area under the inhibitory curve (AUIC) and time above the minimum inhibitory concentration (T > MIC) as predictors of outcome for cefepime and ceftazidime in serious bacterial infections. Int J Antimicrob Agents. 2008;31(4):345–51.
Guilhaumou R, Benaboud S, Bennis Y, Dahyot-Fizelier C, Dailly E, Gandia P, et al. Optimization of the treatment with beta-lactam antibiotics in critically ill patients-guidelines from the French Society of Pharmacology and Therapeutics (Societe Francaise De Pharmacologie et Therapeutique-SFPT) and the French Society of Anaesthesia and Intensive Care Medicine (Societe Francaise d’Anesthesie et Reanimation-SFAR). Crit Care. 2019;23(1):104.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; M100S. 32th Edition ed. Wayne; 2022.
Nicasio AM, VanScoy BD, Mendes RE, Castanheira M, Bulik CC, Okusanya OO, et al. Pharmacokinetics-pharmacodynamics of tazobactam in combination with piperacillin in an in vitro infection model. Antimicrob Agents Chemother. 2016;60(4):2075–80.
Deshayes S, Coquerel A, Verdon R. Neurological adverse effects attributable to beta-lactam antibiotics: a Literature Review. Drug Saf. 2017;40(12):1171–98.
Fugate JE, Kalimullah EA, Hocker SE, Clark SL, Wijdicks EF, Rabinstein AA. Cefepime neurotoxicity in the intensive care unit: a cause of severe, underappreciated encephalopathy. Crit Care. 2013;17(6):R264.
Imani S, Buscher H, Marriott D, Gentili S, Sandaradura I. Too much of a good thing: a retrospective study of beta-lactam concentration-toxicity relationships. J Antimicrob Chemother. 2017;72(10):2891–7.
Lamoth F, Buclin T, Pascual A, Vora S, Bolay S, Decosterd LA, et al. High cefepime plasma concentrations and neurological toxicity in febrile neutropenic patients with mild impairment of renal function. Antimicrob Agents Chemother. 2010;54(10):4360–7.
Huwyler T, Lenggenhager L, Abbas M, Ing Lorenzini K, Hughes S, Huttner B, et al. Cefepime plasma concentrations and clinical toxicity: a retrospective cohort study. Clin Microbiol Infect. 2017;23(7):454–9.
Quinton MC, Bodeau S, Kontar L, Zerbib Y, Maizel J, Slama M et al. Neurotoxic concentration of Piperacillin during continuous infusion in critically ill patients. Antimicrob Agents Chemother 2017;61(9).
Cefepime. Lexi-Drugs. Hudson, OH: Lexicomp. 2023. http://online.lexi.com/. Updated September 19, 2023. Accessed October 6, 2023.
Ceftazidime. Lexi-Drugs. Hudson, OH: Lexicomp. 2023. http://online.lexi.com/. Updated September 30, 2023. Accessed October 6, 2023.
Imipenem. Lexi-Drugs. Hudson, OH: Lexicomp. 2023. http://online.lexi.com/. Updated September 23, 2023. Accessed October 6, 2023.
Meropenem. Lexi-Drugs. Hudson, OH: Lexicomp. 2023. http://online.lexi.com/. Updated September 28, 2023. Accessed October 6, 2023.
Piperacillin/tazobactam. Lexi-Drugs. Hudson, OH: Lexicomp. 2023. http://online.lexi.com/. Updated October 3, 2023. Accessed October 6, 2023.
Beumier M, Casu GS, Hites M, Wolff F, Cotton F, Vincent JL, et al. Elevated β-lactam concentrations associated with neurological deterioration in ICU septic patients. Minerva Anestesiol. 2015;81(5):497–506.
Fratoni AJ, Nicolau DP, Kuti JL. A guide to therapeutic drug monitoring of β-lactam antibiotics. Pharmacotherapy. 2021;41(2):220–33.
Venugopalan V, Hamza M, Santevecchi B, DeSear K, Cherabuddi K, Peloquin CA, et al. Implementation of a β-lactam therapeutic drug monitoring program: experience from a large academic medical center. Am J Health Syst Pharm. 2022;79(18):1586–91.
Acknowledgements
Not applicable.
Funding
This work was supported by Outset Medical Inc.
Author information
Authors and Affiliations
Contributions
SJL and BAM have contributed to the conception or design of the work, the execution, analysis and interpretation for the work and writing the manuscript; approved the final version; and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in compliance with relevant guidelines and regulations. Since the study exclusively used published data from the literature and did not involve human subjects, there was no necessity for Institutional Review Board review.
Consent for publication
Not applicable.
Competing interests
Dr. Mueller received grant funding from Outset Medical Inc. and is consulting for Wolters Kluwer. Dr. Lewis declares no potential conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lewis, S.J., Mueller, B.A. Antibiotic dosing recommendations in critically ill patients receiving new innovative kidney replacement therapy. BMC Nephrol 25, 73 (2024). https://doi.org/10.1186/s12882-024-03469-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-024-03469-2