Abstract
Background
Excessive use of antibiotics has been reported during the SARS-CoV-2 pandemic. We evaluated trends in antibiotic use and culture positive Gram-negative (GN)/Gram-positive (GP) pathogens in US hospitalized patients before and during the SARS-CoV-2 pandemic.
Methods
This multicenter, retrospective study included patients from 271 US facilities with > 1-day inpatient admission with discharge or death between July 1, 2019, and October 30, 2021, in the BD Insights Research Database. We evaluated microbiological testing data, antibacterial use, defined as antibacterial use ≥ 24 h in admitted patients, and duration of antibacterial therapy.
Results
Of 5,518,744 patients included in the analysis, 3,729,295 (67.6%) patients were hospitalized during the pandemic with 2,087,774 (56.0%) tested for SARS-CoV-2 and 189,115 (9.1%) testing positive for SARS-CoV-2. During the pre-pandemic period, 36.2% were prescribed antibacterial therapy and 9.3% tested positive for select GN/GP pathogens. During the SARS-CoV-2 pandemic, antibacterial therapy (57.8%) and positive GN/GP culture (11.9%) were highest in SARS-CoV-2-positive patients followed by SARS-CoV-2-negative patients (antibacterial therapy, 40.1%; GN/GP, pathogens 11.0%), and SARS-CoV-2 not tested (antibacterial therapy 30.4%; GN/GP pathogens 7.2%). Multivariate results showed significant decreases in antibacterial therapy and positive GN/GP cultures for both SARS-CoV-2-positive and negative patients during the pandemic, but no significant overall changes from the pre-pandemic period to the pandemic period.
Conclusions
There was a decline in both antibacterial use and positive GN/GP pathogens in patients testing positive for SARS-CoV-2. However, overall antibiotic use was similar prior to and during the pandemic. These data may inform future efforts to optimize antimicrobial stewardship and prescribing.
Similar content being viewed by others
Background
The coronavirus disease 2019 (COVID-19) pandemic has had a profound impact on US and global healthcare systems and their efforts to manage bacterial infection and limit antimicrobial resistance. While early reports indicate that approximately 68 to 85% of patients hospitalized with COVID-19 receive antibiotic therapy, only 3.5 to 8.1% of hospitalized patients with COVID-19 show evidence of community-acquired bacterial coinfections and an additional 3 to 14% may develop bacterial infections in the hospital [1,2,3,4]. The widespread use of antibiotics in the absence of documented bacterial infection has significant implications for the development of antibiotic resistance, the incidence of Clostridium difficile infections, and potential adverse events and related toxicities [5,6,7,8].
However, most published data on antimicrobial use and the prevalence of bacterial coinfections in patients with COVID-19 were collected early in the pandemic, when relatively little was known about effective management of COVID-19 or the frequency of coinfections in patients with COVID-19 [3, 9]. These studies also preceded the emergence of clinically relevant COVID-19 variants, including the Delta variant, and do not consider how antibiotic prescribing changed over time. Understanding recent patterns in bacterial coinfections and antibiotic prescribing among inpatients can help identify opportunities to improve patient management and antibiotic stewardship efforts.
In this study, we used data from a large database of US hospitals to evaluate trends in antibacterial use and culture-positive Gram-negative and Gram-positive (GN/GP) pathogens in patients hospitalized before the pandemic (between July 2019 and February 2020) and during various waves within the pandemic (between March 2020 and October 2021).
Methods
Study design
We conducted a multicenter, retrospective cohort study evaluating data from 271 US facilities included in the BD Insights Research Database (Becton, Dickinson and Company, Franklin Lakes, NJ), a database that includes small and large hospitals in both rural and urban areas throughout the United States (Additional file 1: Table S1). Eligible admissions included hospitalized adult (≥ 18 years) patients with > 1-day inpatient admission and a record of discharge or death between July 1, 2019, and October 30, 2021. The study dataset, which has been previously described [2, 10,11,12,13], was approved as a limited, de-identified dataset available for retrospective analysis and was exempted from patient consent by the New England Institutional Review Board in Wellesley, Massachusetts (No. 120180023) and conducted in compliance with Health Insurance Portability and Accountability Act requirements.
All microbiology results were derived from local testing performed by individual microbiology labs within the cohort of hospitals in the database. SARS-CoV-2 infection was defined as a positive polymerase chain reaction (PCR) or antigen test ≤ 7 days prior to hospitalization or up to 14 days after hospitalization. In this study, a pathogen was defined as a microorganism with the potential to cause disease; the association between the microorganism and a clinically relevant infection was not evaluated.
Gram-negative (GN) or Gram-positive (GP) bacteria were identified from blood, the upper and lower respiratory tract, intra-abdominal tissues, skin, wounds, urine, and other sources based on standards of the local laboratories. GN pathogens evaluated included Enterobacterales (Citrobacter freundii, Escherichia coli, Enterobacter cloacae, Klebsiella aerogenes, Klebsiella pneumoniae, Klebsiella oxytoca, Proteus mirabilis, Providencia stuartii, Serratia marcescens, Morganella morganii), Acinetobacter baumannii, Pseudomonas aeruginosa, and Stenotrophomonas maltophilia, while GP pathogens evaluated included Enterococcus species, Staphylococcus aureus, and Streptococcus pneumoniae.
Results likely to be associated with environmental or surveillance cultures (e.g., rectal or nasal swabs) were excluded using a previously described algorithmic methodology that considers the source of the specimen, the time of collection, the type of microorganism, and the number of microorganisms in a culture to help exclude non-pathogenic samples [14].
Outcomes
The primary outcomes of our study were the percentage of patients who were prescribed an antimicrobial agent for at least 24 h and the percentage of patients with a GN/GP-positive culture result not due to a contaminant. Secondary outcomes included the type of antimicrobial prescribed and the duration of antibiotic usage. Patients were classified into one of four groups:
-
(1)
those discharged in the pre-pandemic period (July 2019 to February 2020), and the following 3 groups during the pandemic periods (March 2020 to May 2020 [original virus], June 2020 to August 2020, September 2020 to November 2020, December 2020 to February 2021 [predominantly Alpha variant], March 2021 to May 2021, June 2021 to October 2021 [predominantly Delta variant]);
-
(2)
those who tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection;
-
(3)
those who tested negative for SARS-CoV-2; and
-
(4)
those not tested for SARS-CoV-2 (also referred to as “untested” patients).
Antibiotic use was also analyzed by commonly used antibacterial classes (3rd and 4th generation cephalosporins, beta-lactam with beta-lactamase inhibitor combination [BLIC], glycopeptides, and macrolides).
Statistical analysis
Descriptive analyses were used to evaluate trends in antibiotic use, culture-positive results, and pathogen types. Generalized estimating equations (GEE) were used to assess the percentage of patients using antibiotic therapy and with GN/GP-positive pathogens across the study period and during the pandemic by SARS-CoV-2 testing status and to estimate prevalence with 95% confidence intervals. Trends were evaluated by pandemic wave. All GEE models were adjusted by gender, age, length of stay (LOS), ICU stay, use of ventilators, and ≥ 1 comorbid condition as well as by hospital-level factors (urban vs rural status, bed size, teaching status, and geographic region). In bivariate analyses, chi-square tests were used to evaluate the bivariate correlations of SARS-CoV-2 status with the percentages of patients prescribed antibiotics and percentages of patients with GN/GP pathogens. To evaluate the bivariate relationships between LOS (or GN/GP LOS) and SARS-CoV-2 status, T-tests or analyses of variance (ANOVA) were used. All statistical tests were performed using a pre-specified two-tailed alpha level of 0.05. Analyses were conducted using R (R Ver. 4.1.2, R Foundation for Statistical Computing, Vienna, Austria), with RStudio (Boston, MA).
Results
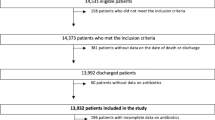
There were 1,789,449 patients hospitalized in the 8-month pre-pandemic period (July 1, 2019, to February 29, 2020) and 3,729,295 patients hospitalized during the pandemic period (March 1, 2020, to October 30, 2021) (Table 1). During the pandemic period, 2,087,774 were tested for SARS-CoV-2 (56.0%) and 189,115 (9.1%) tested positive for SARS-CoV-2 (Table 2). Mean (standard deviation [SD]) age was significantly higher in the SARS-CoV-2-positive group (61.5 [17.9] vs 58.5 [19.7] years for SARS-CoV-2-negative and 57.5 [19.7] years for untested patients, Table 1). Medical facility characteristics and geographic regions by SARS-CoV-2 status are shown in Additional file 1: Table S1. During the pandemic, most patients who were tested for SARS-CoV-2 had specimens collected for microbial testing (89.5%), including 97.1% for patients who tested positive for SARS-CoV-2 and 88.8% for patients who tested negative. Among those not tested for SARS-CoV-2 during the pandemic, 40.0% of patients had specimens collected for microbiologic testing compared to 44.9% during the pre-pandemic period. The proportion of patients with GN/GP pathogens was 11.9% in SARS-CoV-2-positive patients, 11.0% in SARS-CoV-2-negative patients, and 8.3% in patients not tested.
Antibiotic use and GN/GP positivity over time
During the pre-pandemic period (July 2019 through February 2020), 35% (625,994/1,789,449) admissions were prescribed antibacterial therapy for ≥ 24 h and 9.3% (167,045/1,789,449) of admissions were positive for a GN/GP pathogen (Table 2). In the pre-pandemic period, the median duration of antibacterial therapy was 3 days overall and 5 days in patients with a culture-positive GN/GP pathogen (Additional file 2: Table S2). Total admissions prescribed antibacterial therapy and those with a positive bacterial culture for GN/GP pathogens did not significantly change from the pre-pandemic through the pandemic periods over time (Table 3). The median duration of antibiotic therapy in the overall population and among patients with culture-positive GN/GP pathogens also did not change during the pandemic.
Antibiotic use and GN/GP positivity by SARS-CoV-2 testing status
Rates of antibiotic use were substantially higher (P < 0.05) among SARS-CoV-2-positive patients (57.8%) compared to SARS-CoV-2-negative patients (40.1%) or patients not tested (32.8%). Positive GN/GP culture rates were 9.3% among all admissions and were highest (P < 0.05) in SARS-CoV-2-positive patients (11.9%), compared to 11.0% among SARS-CoV-2-negative patients and 8.3% among those not tested.
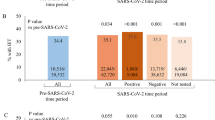
Overall rates of antibacterial use for ≥ 24 h were consistent across time periods in patients not tested. However, antibacterial use significantly decreased by an average of 2.69% each wave in SARS-CoV-2 positive patients (P < 0.001) and 1.69% in SARS-CoV-2 negative patients (P < 0.001) (Table 3, Fig. 1a). For example, among patients who tested positive for SARS-CoV-2, 67.8% received antibiotics between March and May 2020 and 53.5% received antibiotics between June and October 2021.
Overall admissions with a GN/GP-positive culture were consistent across the study period with pre-pandemic rates of 9.4% and 9.2% during the most recent study period. The rate of admissions with a GN/GP-positive culture was highest in SARS-CoV-2 positive patients, peaking at 13.2% during the March 2020 to May 2020 period and decreasing to 11.1% in the most recent period (Table 2; Fig. 1b). During the pandemic period, there was a significant 0.38% decrease in the percent of SARS-CoV-2-positive patients testing positive for GN/GP pathogens by wave (P = 0.023). A significant 0.36% decline in the percentage of SARS-CoV-2-negative patients prescribed antibiotics by wave was also observed, as was a decline of 0.37% (P < 0.001) in antibiotic prescriptions among patients not tested (Table 3).
The median duration of antibiotic use was consistent across study periods but varied by SARS-CoV-2 testing status and by GN/GP-culture status. Among SARS-CoV-2-positive patients, the median duration of antibiotic use was 5 days throughout the study period. The median duration of antibiotic therapy was 4 days in SARS-CoV-2-negative patients and 3 days in patients who were not tested. The duration of antibiotic therapy was greater among patients with positive GN/GP cultures across all SARS-CoV-2 testing groups. For example, among patients with GN/GP culture-positive results, median duration of antibiotic therapy was steady at 5.0 days.
The use of different classes of antibiotic therapy was highest in all groups during the early pandemic period (between March and May 2020) and then declined over time, with the largest declines in SARS-CoV-2 positive patients (Table 4). This was most notable for macrolides and 3rd/4th generation cephalosporins, which both showed a significant (P < 0.001) average decline of 3.78% and 1.61%, respectively, for SARS-CoV-2-positive patients. However, no declines were observed among patients not tested during the pandemic period (Table 3).
Discussion
This is among the first studies to evaluate national changes in inpatient GN/GP positivity and antibiotic use from July 2019, 8 months prior to the onset of the COVID-19 pandemic, through multiple waves of the pandemic. Our data demonstrate that while inpatient antibiotic use temporarily increased early in the pandemic, overall inpatient antibiotic use or GN/GP-positivity rates did not change from July 2019 through October 2021. Total adjusted inpatient GN/GP positivity rates were 9.49% during the pre-pandemic period and 9.35% between June and October 2021, while adjusted rates of antibiotic use during the same time periods were 36.7% and 36.2%, respectively.
Our data suggest that the overall use of antibiotics among inpatients appear to be lower than the results of Centers for Disease Control and Preventions’ (CDC) Emerging Infections Program (EIP) 2015 prevalence surveys, which found that approximately 49.5% of inpatients received antimicrobials [15]. Differences in results may be due to differences in data collection methods, the types of antimicrobials evaluated (antibacterial and selected antimycobacterial and antiviral medications in the CDC EIP study vs antibacterials only in our study), how use was defined, or to recent inpatient antimicrobial stewardship efforts. A more recent study of antibiotic use and presumptive pathogens in Veterans Affairs acute care facilities reported antibiotic use in 41.9% of all hospital stays between October 2017 and September 2018, with 10.2 to 31.4% of antibiotic days of therapy linked to a potential bacterial pathogen [16].
Our results confirmed the findings of other studies that demonstrated an initial increase in antibiotic use during the early pandemic period, particularly among SARS-2-CoV-positive patients [3, 4, 17], followed by a subsequent decrease in later pandemic periods [3]. Rates of GN/GP positivity in SARS-2-CoV-positive patients were 13.3% between March 2020 and May 2020, which decreased to 11.0% between June 2021 and October 2021, while rates of antibacterial antibiotics prescribed during hospitalization decreased from 68.0 to 53.6% over the same period. Similar decreases were observed in SARS-CoV-2-negative patients.
Although increased antibiotic use in the early wave of the pandemic (March 2020 to May 2020) in our study was driven by an increase in use of all 4 evaluated classes of antibiotic (3rd and 4th generation cephalosporins, beta-lactamase inhibitors, glycopeptides, and macrolides), more than half (52.1%) of SARS-CoV-2 + admissions received 3rd or 4th generation cephalosporins. However, the use of all classes of antibiotics decreased in SARS-2-CoV-positive patients in later stages of the pandemic. Similar trends were noted in SARS-CoV-2-negative patients.
A rapid review and meta-analyses of 154 studies evaluating antibiotic prescribing in patients with COVID-19 (N = 35,263) from the onset of the pandemic through June 2020 estimated that overall antibiotic use was 74.6% [3]. However, as noted in our study, a trend towards reduced antibiotic prescribing as the pandemic progressed was reported, from 85.8% in studies conducted before January 2020 to 62.6% for studies ending in April 2020 [3].
In a study of 213,338 inpatients diagnosed with COVID-19 in 716 hospitals between March and October 2020 in the Premier Healthcare Database, 77.3% were billed for antibiotic therapy for at least 1 day [18]. However, overall hospital-wide antibiotic use was significantly lower between March and October 2020 compared with March and October 2019, particularly among hospitals with the lowest burden of COVID-19. Hospitals with a higher burden of COVID-19 reported increased use of ceftriaxone, cefepime, and azithromycin, as we observed in SARS-2-CoV-positive patients in our study. The use of vancomycin, piperacillin-tazobactam, and levofloxacin was consistently lower in 2020 vs 2019, regardless of COVID-19 burden, suggesting a possible decline in empiric prescribing on admission and throughout hospitalization.
Our study also confirms the results of numerous previous studies that describe the mismatch between the high levels of antimicrobial use and low levels of confirmed bacterial infections in patients SARS-CoV-2-positive patients [1,2,3,4, 9, 18,19,20,21]. Our results also may provide insights on the frequency of antibiotic use and GN/GP-positive infections among SARS-CoV-2-negative patients and patients not tested for SARS-CoV-2, which appear to be similar to those observed prior to the pandemic and may help inform future inpatient antimicrobial and diagnostic stewardship efforts.
While our study was not designed to evaluate the appropriateness of antibiotic therapy, we suspect that the increased use of antibiotic therapy among SARS-2-CoV-positive patients early in the pandemic was driven by previous experience with coinfections during influenza outbreaks and potentially by an uncertainty about how to manage severe COVID-19 [1, 4, 19]. However, rates of antibiotic prescription in the absence of a documented infection remained high even during the summer and early fall of 2021, when clinicians were more familiar with how to manage COVID-19 and immunosuppressive strategies for managing COVID-19 were more widely available.
High rates of antibiotic use, particularly in the absence of a documented bacterial infection, can increase rates of antimicrobial resistant (AMR) infections. In a previous analysis of the same dataset, we demonstrated that hospitalized patients tested for SARS-CoV-2 infection exhibited a significantly higher rate of antimicrobial resistant (AMR) infections compared to pre-pandemic rates, although overall AMR rates in hospitalized adults did not substantially increase from pre-pandemic levels [11]. Factors associated with increased AMR included increases in overall antibiotic use, rates of positive cultures, duration of antibiotic therapy, and use of inadequate empiric therapy. We also demonstrated that use of inadequate empiric therapy among patients hospitalized during the pandemic was associated with a 21% increase in mortality and longer lengths of stay compared with patients who received adequate empiric therapy, both in the overall population tested for SARS-CoV-2 and among patients who tested positive and negative for SARS-CoV-2 [13].
Given that 41.1% of SARS-CoV-2-positive patients without a positive culture in the analysis received antibacterial therapy for ≥ 72 h, timely review of antimicrobial prescribing as part of antimicrobial stewardship programs that is coupled with enhanced diagnostic stewardship can reduce the selective pressures for antimicrobial resistance. Further study of recent trends and outcomes in antibiotic use among inpatients is warranted given changes in the severity and transmissibility of SARS-CoV-2 infection since emergence of the Omicron variant, the widespread adoption of SARS-CoV-2 vaccination and boosters, and a greater number of therapeutic options for SARS-CoV-2 infections.
This study has several advantages. First, the study includes data from later stages of the pandemic, data derived from a period in which vaccination was widely accessible and when clinicians became increasingly knowledgeable about managing COVID-19. The study also includes data from the period in which clinically relevant variants became increasingly dominant in the United States, including Delta, and patients from a variety of hospitals in geographically diverse regions, which may provide a more complete view of and clinical practice nationwide.
Our study also has several limitations. First, SARS-CoV-2 and pathogen status were based on reports from individual facilities, there was no standard testing method, and no central laboratory was used. No case definition for COVID-19 disease was applied, so it is possible that some SARS-CoV-2-positive patients were asymptomatic and admitted for other reasons. While our algorithm was designed to exclude patients admitted with colonizing microbes [14], some patients without clinically significant infections may have been included. Finally, because influenza was uncommon during our observation period, our pre-pandemic data may not be representative of other time periods.
Conclusion
Although antibiotics may have been overused among hospitalized SARS-CoV-2-positive patients during the early wave of the pandemic, decreases in the frequency of antibiotic prescriptions were observed in later waves. Overall antimicrobial use and incidence of culture-positive GN/GP did not change from the pre-pandemic through the pandemic period evaluated. These results, combined with results from previous analyses, may inform opportunities for stewardship programs to refine antibiotic prescribing in the current pandemic and to help inform antibiotic use in future viral outbreaks.
Availability of data and materials
The datasets used and/or analyzed during the current study are included in the tables in the main manuscript and additional information.
References
Russell CD, Fairfield CJ, Drake TM, Turtle L, Seaton RA, Wootton DG, et al. Co-infections, secondary infections, and antimicrobial use in patients hospitalised with COVID-19 during the first pandemic wave from the ISARIC WHO CCP-UK study: a multicentre, prospective cohort study. Lancet Microbe. 2021;2:e354–65.
Puzniak L, Finelli L, Yu KC, Bauer KA, Moise P, De Anda C, et al. A multicenter analysis of the clinical microbiology and antimicrobial usage in hospitalized patients in the US with or without COVID-19. BMC Infect Dis. 2021;21:227.
Langford BJ, So M, Raybardhan S, Leung V, Soucy JR, Westwood D, et al. Antibiotic prescribing in patients with COVID-19: rapid review and meta-analysis. Clin Microbiol Infect. 2021;27:520–31.
Baghdadi JD, Coffey KC, Adediran T, Goodman KE, Pineles L, et al. Antibiotic use and bacterial infection among inpatients in the first wave of COVID-19: a retrospective cohort study of 64,691 patients. Antimicrob Agents Chemother. 2021;65: e0134121.
Tartof SY, Rieg GK, Wei R, Tseng HF, Jacobsen SJ, Yu KC. A comprehensive assessment across the healthcare continuum: risk of hospital-associated clostridium difficile infection due to outpatient and inpatient antibiotic exposure. Infect Control Hosp Epidemiol. 2015;36:1409–16.
Tamma PD, Avdic E, Li DX, Dzintars K, Cosgrove SE. Association of adverse events with antibiotic use in hospitalized patients. JAMA Intern Med. 2017;177:1308–15.
Pierce J, Stevens MP. COVID-19 and antimicrobial stewardship: lessons learned, best practices, and future implications. Int J Infect Dis. 2021;113:103–8.
Nieuwlaat R, Mbuagbaw L, Mertz D, Burrows LL, Bowdish DME, Moja L, et al. Coronavirus disease 2019 and antimicrobial resistance: parallel and interacting health emergencies. Clin Infect Dis. 2021;72:1657–9.
O’Kelly B, Cronin C, Connellan D, Griffin S, Conolly SP, McGrath J, et al. Antibiotic prescribing patterns in patients hospitalized with COVID-19: lessons from the first wave. JAC Antimicrob Resist. 2021;3:dlab085.
Bauer KA, Puzniak LA, Yu KC, Finelli L, Moise P, Ai C, et al. Epidemiology and outcomes of culture-positive bloodstream pathogens prior to and during the SARS-CoV-2 pandemic: a multicenter evaluation. BMC Infect Dis. 2022;22(1):841.
Bauer KA, Puzniak LA, Yu KC, Klinker KP, Watts JA, Moise PA, et al. A multicenter comparison of prevalence and predictors of antimicrobial resistance in hospitalized patients before and during the severe acute respiratory syndrome coronavirus 2 pandemic. Open Forum Infect Dis. 2022;9(11):ofac537.
Finelli L, Gupta V, Petigara T, Yu K, Bauer KA, Puzniak LA. Mortality among US patients hospitalized with SARS-CoV-2 infection in 2020. JAMA Netw Open. 2021;4(4): e216556.
Puzniak L, Bauer KA, Yu KC, Moise P, Finelli L, Ye G, De Anda C, et al. Effect of inadequate empiric antibacterial therapy on hospital outcomes in SARS-CoV-2-positive and -negative US patients with a positive bacterial culture: a multicenter evaluation from March to November 2020. Open Forum Infect Dis. 2021;8(6):ofab232.
Brossette SE, Hacek DM, Gavin PJ, Kamdar MA, Gadbois KD, Fisher AG, et al. A laboratory-based, hospital-wide, electronic marker for nosocomial infection: the future of infection control surveillance? Am J Clin Pathol. 2006;125:34–9.
Magill SS, O’Leary E, Ray SM, Kainer MA, Evans C, Bamberg WM, et al. Antimicrobial use in US hospitals: comparison of results From Emerging Infections Program prevalence surveys, 2015 and 2011. Clin Infect Dis. 2021;72:1784–92.
Tedijanto C, Nevers M, Samore MH, Lipsitch M. Antibiotic use and presumptive pathogens in the veterans affairs healthcare system. Clin Infect Dis. 2022;74:105–12.
Winders HR, Bailey P, Kohn J, Faulkner-Fennell CM, Utley S, Lantz E, et al. Change in antimicrobial use during COVID-19 pandemic in South Carolina hospitals: a multicenter observational cohort study. Int J Antimicrob Agents. 2021;58: 106453.
Rose AN, Baggs J, Wolford H, Neuhauser MM, Srinivasan A, Gundlapalli AV, et al. Trends in antibiotic use in United States hospitals during the coronavirus disease 2019 pandemic. Open Forum Infect Dis. 2021;8:ofab236.
Bendala Estrada AD, Calderón Parra J, Fernández Carracedo E, Muiñi Míguez A, Ramos Martínez A, Muñez Rubio E, et al. Inadequate use of antibiotics in the covid-19 era: effectiveness of antibiotic therapy. BMC Infect Dis. 2021;21:1144.
Zhu N, Rawson TM, Mookerjee S, Price JR, Davies F, Otter J, et al. Changing patterns of bloodstream infections in the community and acute care across two COVID-19 epidemic waves: a retrospective analysis using data linkage. Clin Infect Dis. 2021. https://doi.org/10.1093/cid/ciab869.
Vaughn VM, Gandhi TN, Petty LA, Patel PK, Prescott HC, Malani AN, et al. Empiric antibacterial therapy and community-onset bacterial coinfection in patients hospitalized with coronavirus disease 2019 (COVID-19): a multi-hospital cohort study. Clin Infect Dis. 2021;72:e533–41.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7.
Acknowledgements
We thank Nicole Cooper and the HealthCare Alliance Group, LLC, for providing manuscript support with funding from Becton, Dickinson and Company.
Funding
This work was supported by a grant from Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, to Becton, Dickinson, and Company, Franklin Lakes, NJ, USA. Medical writing was supported by Becton, Dickinson and Company.
Author information
Authors and Affiliations
Contributions
LAP, KAB, KCY, and VG were involved in study design and in data analysis and interpretation. LPA, KAB, KCY, and VG drafted the manuscript. JAW and CA provided analytic and statistical support. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This electronic surveillance system and clinical research database, which has been previously described, is exempted from patient consent requirements because it uses deidentified data. This retrospective, deidentified data set was approved, and informed consent requirements were waived by the New England Institutional Review Board (Wellesley, MA, USA; IRB No. 120180023). This report follows the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for cohort studies [22]. The study was performed in accordance with all relevant guidelines and regulations, including the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
LAP was an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, and a shareholder in Merck & Co., Inc., Kenilworth, NJ, USA, at the time of the study. KAB is an employee of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA, and a shareholder in Merck & Co., Inc., Kenilworth, NJ, USA. KCY, JAW, CA, and VG are employees of Becton, Dickinson and Company, which was contracted by Merck to conduct the study. KCY and VG also own stock in Becton, Dickinson and Company.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Hospital demographics.
Additional file 2: Table S2.
Duration of antibacterial therapy overall and in admissions with a GN/GP-positive pathogen from July 2019–October 2021 by SARS-CoV-2 testing status.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Puzniak, L.A., Bauer, K.A., Yu, K.C. et al. A multicenter evaluation of antibacterial use in hospitalized patients through the SARS-Cov-2 pandemic waves. BMC Infect Dis 23, 117 (2023). https://doi.org/10.1186/s12879-023-08042-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08042-0