Abstract
Background
Antibiotic usage and antibiotic resistance (ABR) patterns changed during the COVID-19 pandemic. Inadequate empiric antibiotic therapy (IET) is a significant public health problem and contributes to ABR. We evaluated factors associated with IET before and during the COVID-19 pandemic to determine the impact of the pandemic on antibiotic management.
Methods
This multicenter, retrospective cohort analysis included hospitalized US adults who had a positive bacterial culture (specified gram-positive or gram-negative bacteria) from July 2019 to October 2021 in the BD Insights Research Database. IET was defined as antibacterial therapy within 48 h that was not active against the bacteria. ABR results were based on susceptibility testing and reports from local facilities. Multivariate analysis was used to identify risk factors associated with IET in patients with any positive bacterial culture and ABR-positive cultures, including multidrug-resistant (MDR) bacteria.
Results
Of 278,344 eligible patients in 269 hospitals, 56,733 (20.4%) received IET; rates were higher in patients with ABR-positive (n = 93,252) or MDR-positive (n = 39,000) cultures (34.9% and 45.0%, respectively). Severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2)-positive patients had significantly higher rates of IET (25.9%) compared with SARS-CoV-2-negative (20.3%) or not tested (19.7%) patients overall and in the ABR and MDR subgroups. Patients with ABR- or MDR-positive cultures had more days of therapy and longer lengths of stay. In multivariate analyses, ABR, MDR, SARS-CoV-2-positive status, respiratory source, and prior admissions were identified as key IET risk factors.
Conclusions
IET remained a persistent problem during the COVID-19 pandemic and occurred at higher rates in patients with ABR/MDR bacteria or a co-SARS-CoV-2 infection.
Similar content being viewed by others
Background
Patients with signs and symptoms of bacterial infections are typically treated with empiric antibiotic therapy prior to the availability of information on the specific pathogen and antimicrobial susceptibility. Choosing appropriate empiric therapy thus poses a clinical challenge that can have important consequences. Inadequate empiric therapy (IET), defined as antibacterial therapy not active against the identified bacterial pathogen, is associated with increased mortality, hospitalization, and readmission rates, longer length of stay (LOS), additional antibiotic prescriptions, and higher costs [1,2,3,4,5,6,7]. Antibiotic resistance (ABR), particularly multi-drug resistance (MDR), is a key driver of IET [6, 7], in part because ABR bacteria have fewer available therapeutic options to utilize prior to diagnostic results.
Among hospitalized patients, approximately 8–20% of patients who test positive for severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) have positive cultures for a bacterial co-pathogen, yet 68–76% are treated with antibiotics [8,9,10,11]. These high rates of antibiotic use during the COVID-19 pandemic have been observed in hospitalized patients with influenza as well [12]. There are likely multiple reasons for this pattern, including the desire to prevent bacterial pneumonia and secondary infections, reduced diagnostic and antibiotic susceptibility testing in over-taxed healthcare systems, and uncertainty on how best to manage complex patients with a potentially severe respiratory disease [8, 9, 13]. Increased antibiotic use contributes to ABR, thus potentially compounding challenges involved in patient care [14,15,16]. In one recent study, overall ABR rates per 1000 admissions did not increase in the pandemic compared with pre-pandemic period, but ABR rates were higher in hospitalized SARS-CoV-2-positive patients compared with SARS-CoV-2-negative patients or those not tested for SARS-CoV-2. The largest increase in ABR rates was observed in hospital-onset bacterial cultures [17].
The COVID-19 pandemic has influenced antibiotic usage and ABR, which can lead to changes in IET rates and patient outcomes. We conducted a study of hospitalized US patients prior to and during the COVID-19 pandemic (July 2019 to October 2021) to identify patient and hospital factors associated with IET by ABR status and time period.
Methods
Study design
We conducted a multicenter, retrospective cohort analysis of all hospitalized adults aged ≥ 18 years from 269 US facilities in the BD Insights Research Database (Becton, Dickinson and Company, Franklin Lakes, NJ), which includes both small and large medical care facilities in rural and urban areas throughout the United States. This electronic surveillance system and clinical research database has been previously described and encompasses pharmacy, laboratory, administrative data, patient demographics, and admission, discharge, and transfer data feeds [1, 8, 18, 19]. The retrospective, de-identified data set was approved and informed consent requirements were waived by the New England Institutional Review Board (Wellesley, MA, USA; IRB No. 120,180,023).
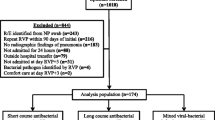
Eligible patients included subjects with 1 to 365 days inpatient stay, a record of discharge or death between July 1, 2019, and October 30, 2021, a positive bacterial culture, and a record of antibiotic therapy. The pre-SARS-CoV-2 period was defined as July 1, 2019 to February 29, 2020. A culture-positive potential bacterial pathogen was defined as a non-contaminant first positive culture for a specified gram-negative or gram-positive bacteria from respiratory, blood, urine, skin/wound, intraabdominal or other source. Microbiology results likely associated with a contaminant or surveillance culture were excluded by a previously described methodology that uses source, time of collection, microorganism type, and number of microorganisms in a culture to flag likely contaminated samples [20].
The major outcome of interest was identification of risk factors contributing to IET, defined as antibiotic therapy prescribed within 48 h from a positive culture collection that did not cover the bacteria or to which the bacteria was subsequently reported as nonsusceptible (NS; laboratory result of intermediate resistance [I] or resistant [R]). For the purposes of this study, the designation of IET was restricted to patients with no adequate antibiotic agent prescribed within 48 h of a positive culture; a patient who received multiple antibiotics with at least one active therapy was NOT categorized as IET. Days of therapy (DOT) included all days of antibiotic therapy (both active or inactive drugs) associated with the index bacteria hospital admission, either before or after the first positive culture.
For the purposes of comparison, patients were categorized into 3 subgroups: (1) patients with any culture positive for a specified gram-negative or gram-positive bacteria; (2) the subset of culture-positive patients with an ABR-positive culture (as defined below); and (3) the subset of ABR-culture positive patients with an MDR-positive culture (as defined below).
Antibiotic susceptibility assessments
Gram-negative bacteria included in these analyses were Enterobacterales (Citrobacter freundii, Escherichia coli, Enterobacter cloacae complex, Klebsiella pneumoniae, Klebsiella oxytoca, Klebsiella aerogenes, Morganella morganii, Proteus mirabilis, Providencia stuartii, Serratia marcescens), Pseudomonas aeruginosa, Acinetobacter complex, and Stenotrophomonas maltophilia. Gram-positive bacteria included in the analyses were Enterococcus spp., Staphylococcus aureus, and Streptococcus pneumoniae.
Antibiotic susceptibility analyses are detailed in Supplementary Section S1. Briefly, ABR in gram-negative bacteria was defined as NS to extended-spectrum cephalosporins (ESC), piperacillin-tazobactam, carbapenems, or fluroquinolones (FQ). MDR in gram-negative bacteria was defined as carbapenem NS, extended-spectrum beta-lactamase producing phenotype, pan-beta-lactam NS, or NS to at least 1 drug in 3 of the following 5 classes: ESC; FQ; carbapenems; aminoglycosides; piperacillin, or piperacillin-tazobactam. For gram-positive bacteria, ABR was defined as Enterococcus resistant to vancomycin (VRE), S. aureus resistant to methicillin (MRSA), and S. pneumoniae NS to penicillin, macrolides, FQ, ESC, or tetracyclines. MDR in gram-positive bacteria was defined as VRE or MRSA. Bacteria defined as MDR were also included in the ABR category.
ABR was identified at the admission level as the first positive culture with any of the ABR bacteria described above. ABR was considered to be community-onset if the first positive ABR event culture was collected ≤ 2 days from admission (with day 1 as day of admission) and was defined as hospital-onset if the culture was collected > 2 days from admission. For patients with an ABR culture, previous susceptible cultures and subsequent ABR or non-ABR cultures with the same or a different pathogen were not evaluated. All results from microbiology testing were obtained from analyses performed by local microbiology labs in the cohort of hospitals included in the BD Insights Research Database. A central laboratory was not used for these analyses.
Statistical analysis
The potential risk factors for IET considered in the study included: ABR to evaluated antibiotics as described above, MDR, COVID-19 time period (pre-SARS-CoV-2, SARS-CoV-2), SARS-CoV-2 testing status (positive, negative, or not tested), pathogen category (gram-positive, gram-negative, both gram-positive and gram-negative), specific bacteria, clinical factors and characteristics associated with the index bacteria hospital admission including the time before and after culture collection (culture source [respiratory, blood, urine, skin/wound, intraabdominal or other]; onset (community or hospital-onset); DOT; LOS; intensive care unit [ICU] admission; ventilated status; and prior 30- or 90-day admission), underlying clinical condition (sepsis/severe sepsis, renal insufficiency/failure, liver dysfunction, myocardial injury, and cytokine dysregulation syndrome) [1, 21], patient demographics (sex and age), facility characteristics (bed size, urban/rural location, teaching status, and geographic region [US census region]).
In the exploratory phase of the analysis, we performed descriptive analyses of IET for three subgroups based on ABR status (all positive cultures, ABR-positive cultures, and MDR-positive cultures) to explore risk factors that potentially influenced IET and their association with ABR. Chi-square tests were used to evaluate the bivariate association between IET and each potential risk factor. In the multivariate analysis phase, which included all the above-specified variables in all analyses, random intercept logistic regression models were used to identify IET risk factors. Risk was reported as odds ratios (OR). The analyses were stratified by ABR and MDR to examine risk factors that significantly predicted IET for resistant bacteria. All statistical tests were performed using a pre-specified two-tailed alpha level of 0.05. Analyses were conducted using R (R Ver. 4.1.2, R Foundation for Statistical Computing, Vienna, Austria), with RStudio (Boston, MA).
Results
The majority (65.1%) of the 269 hospitals included in the study database were in urban locations and 66.9% were non-teaching hospitals (Table 1). Overall, 278,344 patients with a positive bacterial culture were evaluated. For most patients, positive cultures were due to gram-negative bacteria (n = 226,725; 81.5%) and Enterobacterales was the most common bacterial pathogen (n = 180,450; 64.8%). Gram-positive bacteria were identified in 71,269 patients (25.6%). There were 19,650 patients (7.1%) with both gram-negative and gram-positive bacteria included in the previous case counts. Amongst patient admissions, 93,252 (33.5%) and 39,000 (14.0%) met the criteria for ABR and MDR, respectively. Gram-negative bacteria accounted for 84,398 (90.5%) ABR admissions and 25,360 (65.0%) MDR admissions.
IET by ABR status and clinical characteristics
A total of 56,733 (20.4%) patient admissions with a positive culture received IET. IET occurred in 32,561 (34.9%) and 17,554 (45.0%) of ABR and MDR positive cultures, respectively. Compared with the full cohort, ABR and MDR positive cultures were significantly associated with IET (P < 0.001) (Table 2).
Evaluations of the association between bacterial pathogen source and incidence of IET found that respiratory or intraabdominal sources had the highest rates of IET. This pattern was consistent across ABR and MDR cultures. Hospital-onset bacterial cultures had a significantly higher rate of IET compared with community-onset cultures overall and for ABR isolates (both P < 0.001), but not for MDR isolates, which had high rates of IET for both community-onset (44.8%) and hospital-onset (45.8%) cultures (P = 0.084).
For all bacterial pathogens, IET occurred at higher rates in the ABR and MDR subgroups compared with the overall patient cohort. IET rates were higher for gram-positive versus gram-negative bacteria, and highest in patients with both gram-positive and gram-negative positive cultures (Table 2). Although S. maltophilia/Acinetobacter complex accounted for < 1% of positive cultures, the IET rate for this combined bacterial pathogen group was 65.0% in the overall patient cohort. High IET rates were also observed in patients with multiple bacterial bacteria (44.9%), P. aeruginosa (36.8%), and Enterococcus spp (42.0%). The largest disparities in IET rates based on resistance status were observed for Enterobacterales spp. (14.1% overall, 27.8% for ABR, and 40.0% for MDR) and S. aureus/S. pneumoniae (7.5% overall, 30.3% for ABR, and 29.7% for MDR).
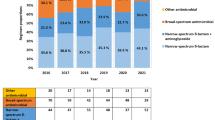
IET by SARS-CoV-2 status and time period
IET rates were slightly, but significantly, higher in the SARS-CoV-2 period (20.5%) compared with the pre-SARS-CoV-2 time period (20.2%; P = 0.044) (Fig. 1). This difference was retained in patients with ABR-positive cultures (35.1% vs. 34.4%; P = 0.034), but did not reach statistical significance in patients with MDR-positive cultures (45.3% vs. 44.3%; P = 0.055). During the SARS-CoV-2 period, significantly higher IET rates compared with the pre-pandemic period were observed in SARS-CoV-2 positive patients, and significantly lower rates were observed in patients not tested for SARS-CoV-2; there was no significant difference in IET rates in SARS-CoV-2-negative patients compared with pre-pandemic rates. For ABR positive cultures, IET rates for all three SARS-CoV-2 testing statuses (positive, negative, and not tested) were significantly higher compared with the pre-pandemic period. For MDR positive cultures, only SARS-CoV-2-positive patients had significantly higher IET rates compared with the pre-pandemic period (Fig. 1).
Inadequate empiric therapy (IET) in patients with positive bacterial cultures by SARS-CoV-2 status. for (A) All positive cultures; (B) Antibiotic-resistant positive cultures; and (C) Multi-drug-resistant positive cultures. Observed data are presented as n IET admissions/N admissions with positive cultures (%). “Positive” and “negative” refer to SARS-COV-2-positive and -negative. P values compare the statistical difference in IET rates vs. the pre-SARS-CoV-2 time period
Impact of IET on DOT and LOS
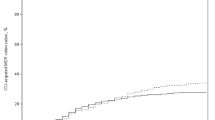
Patients who received IET had a significantly longer duration of therapy (mean DOT of 8.86 [standard deviation (SD) 9.03]) compared with patients who received adequate empiric therapy (6.79 [6.29]; P < 0.001). Duration of therapy was longer for IET patients with positive cultures for ABR (9.95 DOT [10.36]) or MDR (10.49 DOT [10.80]; P < 0.001 for both) compared with overall positive cultures (Table 3). More DOT for IET vs. AET was observed for all drug classes for all positive cultures and ABR-positive cultures. In patients with MDR-positive cultures, more DOT with IET vs. AET were observed for FQ, beta-lactamase inhibitor combinations, and macrolides, but not for ESC, carbapenems, and glycopeptides. Patients who received IET, including those with ABR- or MDR-positive cultures, also had significantly increased hospital LOS and ICU LOS compared with those receiving adequate empiric therapy (Table 3).
Risk factors for IET in multivariate analyses
A multivariate analysis was performed to determine risk factors associated with IET. Significant increases in the risk of IET were observed for ABR-positive cultures vs. all positive cultures (OR 2.59 [95% CI 2.52–2.65]; P < 0.001) and for MDR-positive cultures vs. all positive cultures (OR 1.84 [95% CI 1.78–1.89]; P < 0.001) (Table 4). MDR-positive cultures were also associated with an increased risk of IET relative to ABR-positive cultures (OR 1.86 [95% CI 1.81–1.92]; P < 0.001). Patients positive for SARS-CoV-2 had a significantly increased risk for IET in the overall cohort (OR 1.20 [95% CI 1.15–1.26]; P < 0.001) and in subgroups with an ABR-positive culture (OR 1.07 [95% CI 1.02–1.12]; P = 0.005) or MDR-positive culture (OR 1.13 [95% CI 1.03–1.25]; P = 0.013).
Additional risk factors for increased IET in patients with a positive bacterial culture included respiratory source, hospital onset, gram-positive or combined gram-positive/gram-negative culture, Enterococcus spp., P. aeruginosa or S. maltophilia/Acinetobacter complex, multiple bacterial pathogens, heart failure/myocardial injury, liver dysfunction, renal failure/insufficiency, older age (> 54 years), female sex, more antibiotic DOT, longer hospital LOS, and prior 30-day or 90-day admissions (Table 4). Most of the risk factors for increased IET were retained in subgroup analyses of ABR and MDR (Table 4, Table S1).
Discussion
Our study spanning 8 months prior to the COVID-19 pandemic through October 2021 and encompassing almost 300,000 hospital admissions with positive bacterial cultures found that SARS-CoV-2-positive patients had significantly higher rates of antibiotic IET compared with the overall patient population during the pre-pandemic period and with SARS-CoV-2-negative and not tested patients during the pandemic period. We further observed elevated IET rates in patients with ABR- or MDR-positive cultures; the IET rate for MDR bacteria in this study (45% for evaluated bacteria across all culture sources) was similar to rates recently reported for patients with bloodstream infections caused by carbapenem-resistant Enterobacterales (44.7%) or VRE (39.6%) [7], providing further confirmation of these data. Our finding that IET was associated with additional DOT and longer hospital and ICU stays is consistent with other studies[1,2,3, 5, 6, 22] and documents the substantial burden not only for patients receiving IET, but also for hospital facilities, particularly during surge capacity periods.
It is clear from our data that ABR is closely connected with IET. We found a 2.59-fold increased risk of IET with ABR-positive cultures and an MDR-positive culture was associated with an additional 1.86-fold increase in IET compared with ABR-positive cultures. Over one-third (34.9%) of patients with ABR-positive cultures and 45.0% of patients with MDR-positive cultures received IET upon hospital admission, a finding that highlights difficulties in choosing empiric therapy for patients with potentially resistant bacterial pathogens. Of the many factors we assessed in multivariate analyses, including age, comorbidities, isolate source, and ventilator/ICU status, only specific, highly-resistant bacteria (Enterococcus and S. maltophilia/Acinetobacter complex) were associated with a higher risk of IET than ABR. Other factors with significant contributions to high IET rates included respiratory source, hospital-onset infections, and certain underlying conditions (heart failure/myocardial injury, liver dysfunction, and renal failure/insufficiency), older age, and prior admissions. It should be noted that although we identified multiple significant risk factors for IET, the magnitude of their effects varied substantially. IET risk factors identified in our study may serve as predictors of patients in need of aggressive initial antibiotic treatment and as candidates for future studies aimed at optimizing initial therapy choices in high-risk patients.
The SARS-CoV-2 pandemic has further exacerbated challenges with ABR and IET. We previously reported that ABR rates for hospital-onset bacterial infections during the first 20 months of the COVID-19 pandemic were significantly higher than in the preceding pre-pandemic period, particularly in SARS-CoV-2-positive patients, but overall ABR rates were significantly lower in hospitalized patients due to decreased rates in community-onset infections [17]. Although overall IET rates remained similar in the pre-pandemic and pandemic periods, during the SARS-CoV-2 period we observed significant increases in IET over pre-pandemic rates in patients with ABR-positive cultures and those who were SARS-CoV-2 positive; hospital-onset infections were a key contributing factor. Patients with SARS-CoV-2 and bacterial infections are at higher risk for mortality than SARS-CoV-2-negative patients [1, 23] and have more antibiotic usage and longer hospital and ICU LOS [8, 17]. IET, which is associated with increased LOS and mortality [1, 7], likely contributes to these impaired outcomes in SARS-CoV-2-positive patients.
The strong association between ABR and IET was retained during both the pre-pandemic and pandemic periods. A recent report estimated that bacterial ABR was associated with an estimated 4.95 million deaths worldwide in 2019 [24]. There is evidence that the COVID-19 pandemic may have contributed to increases in bacterial ABR in hospitalized patients [17, 25]. During peak capacity periods associated with the COVID-19 pandemic, hospital systems were forced to decrease diagnostic and antibiotic susceptibility testing and reallocate staff from antimicrobial stewardship activities to COVID-related priorities while at the same time increasing antibiotic consumption [13]. The increased ABR rates we have observed in hospitalized SARS-CoV-2-positive patients may reflect these factors, particularly the increased antibiotic exposure and LOS in this patient population [17]. Future longitudinal studies will be needed to explore ongoing changes in IET and ABR in US hospitals. A study of 38 Michigan hospitals found that early increases in antibiotic consumption diminished over time as more experience was gained with managing SARS-CoV-2 infections [26], perhaps augmented by the less severe disease observed later in the pandemic [27]. Lag times of approximately 3 to 6 months have been reported between antibiotic changes and resistance levels in a pre-pandemic study [28], so reductions in ABR may not be immediately apparent.
Irrespective of pandemic-related factors, however, IET remains an important challenge in the treatment of hospitalized patients. Although one option to address this problem is expanded use of broad-spectrum antibiotics, these antibiotics are associated with increased ABR and therefore have the potential to actually compound IET challenges. In addition, broad-spectrum drugs can have negative clinical consequences, including increased risk of Clostridioides difficile infection [29, 30] and higher rates of severe sepsis following hospital discharge [31]. Accordingly, the solution to IET does not appear to be indiscriminate broad-spectrum antibiotic use, but rather a tailored therapy approach based on risk factor assessment, diagnostic testing, and antimicrobial stewardship efforts, including vaccination programs to reduce infectious diseases [32,33,34,35]. Although the study reported here focused on IET in culture-positive patients, it is important to note that a substantial proportion of culture-negative or not tested hospitalized patients receive prolonged antibiotic therapy (> 3 days) [17]. This patient population would benefit from antimicrobial stewardship programs as well.
Study limitations include the use of facility reports rather than a central laboratory for SARS-CoV-2 and antibiotic susceptibility tests. Different laboratories may have used different testing systems and breakpoints for determination of resistance, thereby potentially affecting the ABR and MDR rates reported here. Analyses were based on positive SARS-CoV-2 tests and not on symptomatic infection, so asymptomatic patients admitted for other causes may have been included. Similarly, patients with positive bacterial cultures did not necessarily have a confirmed bacterial infection. Our testing algorithm was designed to remove admissions with contaminating bacteria [20], but it is possible that some bacteria included in our analyses were colonizers. Due to database limitations, information on outpatient antibiotic exposure was not available and antibiotics prescribed in prior admissions were not evaluated, although we did evaluate whether patients were admitted in the prior 30 and 90 days. Selection bias (e.g., a greater likelihood of collecting bacterial culture data on more severely ill patients) may have influenced reported resistance rates. Certain geographic areas and smaller hospitals may have been underrepresented in our database.
Conclusion
Our study documents elevated rates of IET in patients with ABR- or MDR-positive cultures and in patients positive for SARS-CoV-2. IET rates appear to be inextricably linked to ABR, and improvements in both are likely to require expanded use of rapid diagnostic tests, intensified vaccination programs, and a renewed commitment to antimicrobial stewardship programs. The data from our study may be of use in focusing future research efforts aimed at improving the adequacy of empiric therapy and reducing ABR in hospitalized patients.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Puzniak L, Bauer KA, Yu KC, Moise P, Finelli L, Ye G, et al. Effect of inadequate empiric antibacterial therapy on hospital outcomes in SARS-CoV-2-positive bacterial culture: a multicenter evaluation from March to November 2020. Open Forum Infect Dis. 2021;8(6):ofab232.
Dunne MW, Puttagunta S, Aronin SI, Brossette S, Murray J, Gupta V. Impact of empirical antibiotic therapy on outcomes of outpatient urinary tract infection due to nonsusceptible Enterobacterales. Microbiol Spectr. 2022;10(1):e0235921.
Zilberberg MD, Nathanson BH, Sulham K, Fan W, Shorr AF. 30-day readmission, antibiotics costs and costs of delay to adequate treatment of Enterobacteriaceae UTI, pneumonia, and sepsis: a retrospective cohort study. Antimicrob Resist Infect Control. 2017;6:124.
Zilberberg MD, Nathanson BH, Puzniak LA, Zilberberg NWD, Shorr AF. Inappropriate empiric therapy impacts complications and hospital resource utilization differentially among different types of bacterial nosocomial pneumonia: a cohort study, United States, 2014 – 1029. Crit Care Explor. 2022;4(4):e0667.
Raman G, Avendano E, Berger S, Menon V. Appropriate initial antibiotic therapy in hospitalized patients with gram-negative infections: systematic review and meta-analysis. BMC Infect Dis. 2015;15:395.
Kadri SS, Lai YL, Warner S, Strich JR, Babiker A, Ricotta EE, et al. Inappropriate empirical antibiotic therapy for bloodstream infections based on discordant in-vitro susceptibilities: a retrospective cohort analysis of prevalence, predictors, and mortality risk in US hospitals. Lancet Infect Dis. 2021;21(2):241–51.
Ohnuma T, Chihara S, Costin B, Treggiari MM, Bartz RR, Raghunathan K, et al. Association of appropriate empirical antimicrobial therapy with in-hospital mortality in patients with bloodstream infections in the US. JAMA Netw Open. 2023;6(1):e2249353.
Puzniak L, Finelli L, Yu KC, Bauer KA, Moise P, De Anda C, et al. A multicenter analysis of the clinical microbiology and antimicrobial usage in hospitalized patients in the US with or without COVID-19. BMC Infect Dis. 2021;21:227.
Baghdadi JD, Coffey KC, Adediran T, Goodman KE, Pineles L, Magder LS, et al. Antibiotic use and bacterial infection among inpatients in the first wave of COVID-19: a retrospective cohort study of 64,691 patients. Antimicrob Agents Chemother. 2021;65:e0134121.
Rawson TM, Moore LSP, Zhu N, Ranganathan N, Skolimowska K, Gilchrist M, et al. Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020;71(9):2459–68.
Langford BJ, So M, Raybardhan S, Leung V, Soucy JR, Westwood D, et al. Antibiotic prescribing in patients with COVID-19: rapid review and meta-analysis. Clin Microbiol Infect. 2021;27(4):520–31.
Ghazi IM, Nicolau DP, Nailor MD, Aslanzadeh J, Ross JW, Kuti JL. Antibiotic utilization and opportunities for stewardship among hospitalized patients with influenza respiratory tract infection. Infect Control Hosp Epidemiol. 2016;37(5):583–9.
Tomczyk S, Taylor A, Brown A, de Kraker MEA, El-Saed A, Alshamrani M, et al. Impact of the COVID-19 pandemic on the surveillance, prevention and control of antimicrobial resistance: a global survey. J Antimicrob Chemother. 2021;76(11):3045–58.
Costelloe C, Metcalfe C, Lovering A, Mant D, Hay AD. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010;340:c2096.
Barnes SL, Rock C, Harris AD, Cosgrove SE, Morgan DJ, Thom KA. The impact of reducing antibiotics on the transmission of multidrug-resistant organisms. Infect Control Hosp Epidemiol. 2017;38(6):663–9.
Tartof SY, Rieg GK, Wei R, Tseng HF, Jacobsen SJ, Yu KC. A comprehensive assessment across the healthcare continuum: risk of hospital-associated Clostridium difficile infection due to outpatient and inpatient antibiotic exposure. Infect Control Hosp Epidemiol. 2015;36(12):1409–16.
Bauer KA, Puzniak LA, Yu KC, Klinker KP, Watts JA, Moise PA, et al. A multicenter comparison of prevalence and predictors of antimicrobial resistance in hospitalized patients before and during the SARS-CoV-2 pandemic. Open Forum Infect Dis. 2022;9(11):ofac537.
McCann E, Srinivasan A, DeRyke CA, Ye G, DePestel DD, Murray J, et al. Carbapenem non-susceptible gram-negative pathogens in ICU and non-ICU settings in US hospitals in 2017: a multicenter study. Open Forum Infect Dis. 2018;5(10):ofy241.
Gupta V, Ye G, Olesky M, Lawrence K, Murray J, Yu K. Trends in resistant Enterobacteriaceae and Acinetobacter species in hospitalized patients in the United States: 2013–2017. BMC Infect Dis. 2019;19(1):742.
Brossette SE, Hacek DM, Gavin PJ, Kamdar MA, Gadbois KD, Fisher AG, et al. A laboratory-based, hospital-wide, electronic marker for nosocomial infection: the future of infection control surveillance? Am J Clin Pathol. 2006;125(1):34–9.
Finelli L, Gupta V, Petigara T, Yu K, Bauer KA, Puzniak LA. Mortality among US patients hospitalized with SARS-CoV-2 infection in 2020. JAMA Netw Open. 2021;4(4):e216556.
Zilberberg MD, Nathanson BH, Sulham K, Fan W, Shorr AF. Carbapenem resistance, inappropriate empiric treatment and outcomes among patients hospitalized with Enterobacteriaceae urinary tract infection, pneumonia and sepsis. BMC Infect Dis. 2017;17(1):279.
Silva DL, Lima CM, Magalhaes VCR, Baltazar LM, Peres NTA, Caligiorne RB, et al. Fungal and bacterial coinfections increase mortality of severely ill COVID-19 patients. J Hosp Infect. 2021;113:145–54.
Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–55.
Centers for Disease Control and Prevention. COVID-19 reverses progress in fight against antimicrobial resistance in U.S [Internet}. July 12., 2022. Available from: https://www.cdc.gov/media/releases/2022/s0712-Antimicrobial-Resistance.html.
Vaughn VM, Gandhi TN, Petty LA, Patel PK, Prescott HC, Malani AN, et al. Empiric antibacterial therapy and community-onset bacterial coinfection in patients hospitalized with coronavirus disease 2019 (COVID-19): a multi-hospital cohort study. Clin Infect Dis. 2021;72(10):e533–41.
Iuliano AD, Brunkard JM, Boehmer TK, Peterson E, Adjei S, Binder AM, et al. Trends in disease severity and health care utilization during the early omicron variant period compared with previous SARS-CoV-2 high transmission periods — United States, December 2020–January 2022. MMWR Morb Mortal Wkly Rep. 2022;71(4):146–52.
Martinez EP, van Rosmalen J, Bustillos R, Natsch S, Mouton JW, Verbon A. Trends seasonality and the association between outpatient antibiotic use and antimicrobial resistance among urinary bacteria in the Netherlands. J Antimicrob Chemother. 2020;75(8):2314–25.
Webb BJ, Subramanian A, Lopansri B, Goodman B, Jones PB, Ferraro J, et al. Antibiotic exposure and risk for hospital-associated Clostridioides difficile infection. Antimicrob Agents Chemother. 2020;64(4):e02169–19.
Schönherr SG, Ranft D, Lippmann N, Lübbert C. Changes in antibiotic consumption, AMR and Clostridioides difficile infections in a large tertiary-care center following the implementation of institution-specific guidelines for antimicrobial therapy: a nine-year interrupted time series study. PLoS ONE. 2021;16(10):e0258690.
Baggs J, Jernigan JA, Halpin AL, Epstein L, Hatfield KM, McDonald LC. Risk of subsequent sepsis within 90 days after a hospital stay by type of antibiotic exposure. Clin Infect Dis. 2018;66(7):1004–12.
Trevas D, Caliendo AM, Hanson K, Levy J, Ginocchio CG. Diagnostic tests can stem the threat of antimicrobial resistance: infectious disease professionals can help. Clin Infect Dis. 2021;72(11):e893–900.
Verroken A, Scohy A, Gerard L, Wittebole X, Collienne C, Laterre PF. Co-infection in COVID-19 critically ill and antibiotic management: a prospective cohort analysis. Crit Care. 2020;24(1):410.
Bloom DE, Black S, Salisbury D, Rappuoli R. Antimicrobial resistance and the role of vaccines. Proc Natl Acad Sci U S A. 2018;115(51):12868–71.
Klugman KP, Black S. Impact of existing vaccines in reducing antibiotic resistance: primary and secondary effects. Proc Natl Acad Sci U S A. 2018;115(51):12896–901.
Acknowledgements
Part of this research was presented at the World Vaccine Congress, April 18–21, 2022, Washington, DC. We thank Sharon L. Cross, PhD, Fusion MD Medical Science Network, Inc., for providing manuscript support with funding from BD.
Funding
This work was supported by a grant from Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA to BD, Franklin Lakes, NJ, US. Medical writing was supported by BD.
Author information
Authors and Affiliations
Contributions
KAB, LAP, KCY, KPK, PAM, LF, and VG designed the study. JAW conducted statistical analyses. KAB, LAP, JAW, and VG drafted the manuscript. All authors were involved in data interpretation and critical review of the manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki. The retrospective, de-identified data set was approved and informed consent requirements were waived by the New England Institutional Review Board (Wellesley, MA, USA; IRB No. 120180023).
Consent for publication
Not applicable.
Competing interests
KAB, KPK, PAM, and LF are employees of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, USA and shareholders in Merck & Co., Inc., Kenilworth, NJ, USA. LAP was an employee of Merck and Co, Inc. at the time of the analysis and may own stock and/or hold stock options in Merck and Co, Inc. KCY and VG are employees of Becton, Dickinson and Company (BD), which was contracted by Merck to conduct the study, and JAW is a former employee. KCY and VG also own stock in BD.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12879_2023_8453_MOESM1_ESM.docx
Supplementary Material 1: Section S1: Antibiotic susceptibility analyses. Table S1: Hospital and geographic multivariate results for risk factors for inadequate therapy by ABR status. Data are presented as odds ratio (OR) (confidence interval [CI]).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bauer, K.A., Puzniak, L.A., Yu, K.C. et al. Association of SARS-CoV-2 status and antibiotic-resistant bacteria with inadequate empiric therapy in hospitalized patients: a US multicenter cohort evaluation (July 2019 - October 2021). BMC Infect Dis 23, 490 (2023). https://doi.org/10.1186/s12879-023-08453-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08453-z