Abstract
Background
Some coronary artery angiography (CAG) scores are associated with the no-reflow phenomenon after percutaneous coronary intervention (PCI) in patients with acute ST-segment elevation myocardial infarction (STEMI). However, quality evidence regarding the association between the CAG scores and microvascular injury is still needed. Our study aimed to validate the ability of the CAG scores in predicting microvascular obstruction (MVO) detected by cardiac magnetic resonance (CMR) imaging.
Methods
From October 2020 to October 2021, 141 consecutive patients with acute STEMI who underwent primary PCI and CMR were retrospectively reviewed. CMR imaging was performed between 3 and 7 days after PCI. The patients were divided into MVO and non-MVO group based on the CMR results. Three CAG scores (SYNTAX score, SYNTAX II score and Gensini score) were used to assess the severity of coronary artery atherosclerotic burden.
Results
A total of 122 patients were included (mean age 60.6 ± 12.8 years). MVO occurred in 51 patients (41.8%). Patients with MVO had higher SYNTAX scores, SYNTAX II scores and Gensini scores than those without MVO (all p < 0.001). The Gensini score (r = 0.567, p < 0.001) showed the strongest correlation with infarction size than SYNTAX score (r = 0.521, p < 0.001) and SYNTAX II score (r = 0.509, p < 0.001). The areas under the receiver operator characteristic curves of SYNTAX score, SYNTAX II score and Gensini score for predicting MVO patients were 0.726, 0.774 and 0.807. In multivariable regression analysis, peak troponin I (odd ratio [OR] = 1.236, p = 0.001) and SYNTAX II score (OR = 11.636, p = 0.010) were identified as independent predictors of MVO.
Conclusions
In patients with acute STEMI undergoing primary PCI treatment, the peak troponin I and SYNTAX II score may be an independent predictor of MVO.
Similar content being viewed by others
Background
Early percutaneous coronary intervention (PCI) has been reported to significantly reduce mortality in patients with acute ST-segment elevation myocardial infarction (STEMI) [1]. However, the consequent improvement in myocardial perfusion post-PCI is not universal. About 50% of patients undergoing primary PCI shows delayed myocardial perfusion [2, 3]. This phenomenon is called as microvascular obstruction (MVO) and is related to structural and functional damage at the microvascular level caused by PCI revascularization [4, 5]. Previous studies have shown a significant increase in the incidence of major adverse cardiovascular events (MACE) in patients with MVO [3].
Cardiac magnetic resonance (CMR) is a non-invasive imaging tool with high spatial resolution, has been widely used to detect and quantify the extent of MVO [6,7,8]. However, the long breath-holding requirements make it difficult for STEMI patients to cooperate, and excessive dosage of gadolinium contrast agent increases the risk of renal failure.
Some coronary artery angiography (CAG) scores, such as the SYNTAX score [9] and Gensini score [10], have been used to assess the coronary artery atherosclerotic burden. SYNTAX score has an excellent performance in predicting the MACE in STEMI patients after PCI [11, 12]. More recently, it has been shown that the SYNTAX score and Gensini score are associated with the no-reflow phenomenon (thrombolysis in myocardial infarction [TIMI] blood flow < 3 or myocardial color grade < 2) after PCI [13, 14]. However, quality evidence regarding the association between the CAG scores and microvascular injury in acute STEMI patients is still needed. In addition, it has been shown that the SYNTAX II score’s sensitivity and specificity are higher than SYNTAX score in predicting in-hospital mortality of high-risk patients with STEMI [15]. The SYNTAX II score connects the characteristics of clinical variables with coronary anatomy, and may also have an important role in predicting microvascular injury. Therefore, our study aimed to validate the ability of three CAG scores in predicting MVO detected by CMR imaging.
Methods
Study population
This retrospective single-center cohort study enrolled 141 consecutive patients with acute STEMI who underwent primary PCI and CMR at Lianyungang First People’s Hospital between October 2020 and October 2021. STEMI was defined as a combination of chest pain suggested that the duration of myocardial ischemia was > 30 min. The electrocardiography (ECG) indicated ST segment elevation > 2 mm on at least two precordial leads or limb leads, and troponin levels significantly increased beyond double the normal upper limit. The inclusion criteria were as follows: (1) diagnosis of STEMI; (2) PCI performed within 12 h of symptom onset; (3) CAG performed before and immediately after PCI; and (4) CMR performed between 3 and 7 days after PCI. The exclusion criteria were as follows: (1) age < 18 years; (2) previous history of myocardial infarction or revascularization (n = 10); and (3) incomplete CAG image (n = 6) or poor CMR image quality (n = 3). Finally, 122 patients were enrolled (mean age 60.6 ± 12.8 years old; 72.1% was male).
PCI and CAG
PCI treatment was performed using Seldinger's method in all patients with a median time of 4.5 h, using a 5F contrast catheter, 6F guide catheter, and 0.014-inch guide wire. A total of 100 ml nonionic contrast agent (Ultravist 370; Bayer AG, Berlin, Germany) was injected. Heparin was intravenously injected (7.5 ml) and maintained (17.5 ml/h). Drug-eluting stents were used in all the patients. All stents were implanted directly whenever possible, and balloon dilation angioplasty (8–10 atmospheric pressure) was performed in the remaining cases. TIMI blood flow grades were recorded before and after PCI.
CAG score
Based on the results of coronary artery angiography before PCI, three CAG scores (SYNTAX score, SYNTAX II score and Gensini score) were used to assess the severity of coronary artery atherosclerotic burden by two uninformed cardiologists. The SYNTAX score and SYNTAX II score were calculated using the SYNTAX score online calculator (http://www.SYNTAXscore.com). The SYNTAX score evaluated all coronary lesions with diameter stenosis > 50% and vessels with diameter > 1.5 mm [16]. The SYNTAX score for the degree of coronary stenosis were 2 for 50–99%, 5 for 100%. The SYNTAX II score was composed of SYNTAX score and six clinical variables, including age, gender, creatinine clearance, LVEF, chronic obstructive pulmonary disease, and peripheral arterial disease. The Gensini score was calculated based on the product of the degree scoring of coronary stenosis and the location score of the lesion [10]. The Gensini score for the degree of coronary stenosis were 1 for 1–25%, 2 for 26–50%, 4 for 51–75%, 8 for 76–90%, 16 for 91–99%, 32 for 100%. The culprit artery was defined as the target artery treated with PCI.
Cardiac magnetic resonance
CMR examinations were performed in all patients after PCI with a median time of 5.2 days. CMR was performed with a 1.5 T MR scanner (Magnetom Aera XJ, Siemens, Erlangen, Germany) using an 12-element phased-array coil equipped with ECG-gated. The cardiac cine imaging was performed using the steady-state free precession sequence (SSFP) sequence; slice gap, 0 mm; slice thickness, 8 mm; repetition time, 37 ms; echo time, 1.2 ms; field of view, 340 × 340 mm2. T2-weighted imaging was performed using the short time inversion recovery (STIR) sequence with the same prescription of cine images. Late gadolinium enhancement (LGE) imaging was performed using the phase sensitive inversion recovery (PSIR) sequence; slice gap, 0 mm; slice thickness, 8 mm; echo time, 1.3 ms; inversion time, 300–340 ms; field of view, 340 × 340 mm2.
All images were evaluated on the CMR post-processing software (cvi42 v5.13, Circle Cardiovascular Imaging, Calgary, Canada). CMR images were interpreted by two uninformed radiologists, and consensus was reached when opinions were different. Left ventricular ejection fraction (LVEF) were calculated from cine images. The area at risk (AAR) was defined as the high-signal region (> 2 standard deviations [SD] of the normal myocardial signal) on T2-weighted images. T2-weighted images with poor image quality or unrecognizable AAR area were removed. The infarction size (IS) was quantified on LGE images 10 min after gadolinium injection (Gadoteric Acid Meglumine Salt Injection, Hengrui, Lianyungang, China). The signal threshold for IS was set to > 5 SD of the normal myocardial signal. Myocardial salvage index (MSI) was calculated as: MSI = (AAR − IS)/AAR × 100. The MVO was defined as a hypoenhanced region within LGE area. AAR and IS were recorded as percentage of the left ventricular (LV).
Statistical analysis
Statistical analyses were performed using the IBM SPSS software (version 26.0; IBM Corp, Chicago, IL, USA). Continuous variables were expressed as mean ± SD or median (25th to 75th percentile), and were compared using independent sample t-tests or Mann–Whitney U-tests. Categorical data were expressed as n (%) and were compared using Chi-squared tests. Spearman correlation analysis was used to assess the correlation between coronary scores and IS (%LV). The area under the curve (AUC) in the receiver operating characteristic (ROC) analysis was used to assess predictive performance. Binary logistic regression analysis was performed to assess the coronary scores for predicting MVO (results were expressed as odds ratio [OR] and 95% confidence interval [CI]). Coronary scores were converted into categorical variables based on the cutoff value. The variables of p < 0.1 in the univariable analysis were included in the multivariable tests. All tests were two-tailed and p < 0.05 was considered as statistically significant.
Results
Characteristics of patients
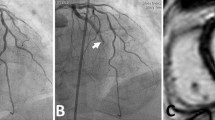
A total of 122 patients with acute STEMI were enrolled, with 51 (41.8%) in the MVO group and 71 (58.2%) in the non-MVO group. Typical examples (with and without MVO) of patients are shown in Fig. 1. In the comparison of data between the two groups, there were no statistically significant differences in age, gender, heart rate, systolic blood pressure, diastolic blood pressure, hypertension, diabetes, current Smoker, dyslipidemia, GRACE score, serum creatinine, serum uric acid, albumin, plasma fibrinogen, D-Dimer, neutrophil, lymphocyte, total cholesterol, triglyceride, low density lipoprotein cholesterol (LDL-C), high density lipoprotein cholesterol (HDL-C), Killip class, time from symptom onset to PCI, time from PCI to CMR, culprit artery left circumflex artery (LCX), number of diseased arteries, and final TIMI flow grade (all p > 0.05). Compared with the non-MVO group, the MVO group had higher peak Troponin I, higher peak creatine kinase (CK), higher peak creatine kinase isoenzyme (CK-MB), higher pro-B-type natriuretic peptide (PRO-BNP), higher C-reaction protein (CPR), more culprit artery left anterior descending artery (LAD), less culprit artery right coronary artery (RCA), more initial TIMI 0/1 flow, lower LVEF, larger AAR (%LV), larger and IS (%LV), lower MSI, higher SYNTAX scores, higher SYNTAX II scores and higher Gensini scores (all p < 0.05) (Table 1).
Two typical examples (with and without MVO) of angiography and cardiac magnetic resonance image. Case one (a–d): A 49-year-old male STEMI patient with MVO was diagnosed to have a total occluded proximal segment of the LAD (SYNTAX score 20.5, SYNTAX II score 39, and Gensini score 80); Case two (e–h): A 68-year-old male STEMI patient without MVO was diagnosed to have a total occluded proximal segment of the RCA (SYNTAX score 10, SYNTAX II score 30.6, and Gensini score 32). STEMI ST-segment elevation myocardial infarction; MVO microvascular obstruction; LAD left anterior descending artery; RCA right coronary artery
Correlations between coronary scores and IS
In the correlation analysis, three coronary scores were positively correlated with IS (%LV). Among them, Gensini score (r = 0.567, p < 0.001) showed the strongest correlation with IS (%LV) than SYNTAX score (r = 0.521, p < 0.001) and SYNTAX II score (r = 0.509, p < 0.001) (Fig. 2).
ROC curve analysis
The ROC curve analysis of the three coronary scores predicted MVO is shown in Table 2. Among them, Gensini score showed the largest area under the curve (AUC = 0.807, 95% CI 0.730–0.884, p < 0.001) than SYNTAX score (AUC = 0.726, 95% CI 0.634–0.818, p < 0.001) and SYNTAX II score (AUC = 0.774, 95% CI 0.689–0.859, p < 0.001). At the optimal cutoff value of 61, the Gensini score predicted MVO sensitivity and specificity were 76.5% and 77.5%. At the optimal cutoff value of 17.5, the SYNTAX score predicted MVO sensitivity and specificity were 74.5% and 67.6%. At the optimal cutoff value of 36.4, the SYNTAX II score predicted MVO sensitivity and specificity were 62.7% and 85.9% (Fig. 3).
Univariable and multivariable analysis
In the univariable analysis for predicting MVO, variables including peak troponin I, peak CK, Peak CK-MB, culprit artery LAD, culprit artery RCA, Initial TIMI flow 0/1, LVEF, AAR, IS, MSI, SYNTAX score, SYNTAX II score, and Gensini score had a p-value < 0.1 After adjustment for other potential confounders including PRO-BNP, AAR, IS and MSI, the multivariable analysis showed that the peak troponin I (OR = 1.236, 95% CI 1.095—1.395, p = 0.001) and SYNTAX II score (OR = 11.636, 95% CI 1.816—74.556, p = 0.010) were identified as independent predictors of MVO (Table 2).
Discussion
In the present study, we investigated the association between the CAG scores and MVO in patients with acute STEMI after PCI. We found that (1) patients with MVO had higher SYNTAX score, SYNTAX II score, and Gensini score than those without MVO; (2) Gensini score showed the strongest correlation with IS than SYNTAX score and SYNTAX II score; and (3) the peak troponin I and SYNTAX II score were independent associated with MVO after adjustment for potential confounders.
Coronary artery angiography score is widely used to assess extent and severity of coronary atherosclerotic disease (CAD) burden [17]. Previous studies proved that the SYNTAX score and Gensini score could predict the no-reflow phenomenon defined by TIMI flow or myocardial color grade post-PCI [13, 14]. However, multiple evidences showed that TIMI flow or myocardial color grade underestimated the prevalence of microvascular injury [2, 18]. CMR is an excellent imaging tool for detecting MVO with high sensitivity and specificity, and a recent expert consensus recommends 3–7 days post-PCI as the preferred CMR imaging time point to evaluate MVO [19]. Therefore, evaluating the association between coronary scores and MVO can provide higher quality evidence for early identification of patients with microvascular injury.
The MVO is a severe marker of microvascular blood flow dysfunction. The development of MVO depends on several factors: (1) the shedding of atherosclerotic or thrombotic debris caused by PCI [20], (2) vasospasm caused by the release of vasoconstrictor factors such as endothelin and thromboxane [21], (3) activation of platelets and coagulation factors in microvascular caused by endothelial cell injury [4], and (4) progressive inflammatory cells accumulation in the infarct area [22]. Our study showed that patients with MVO had significantly higher coronary scores than those without MVO. This may be because higher coronary scores indicated that the coronary artery stenosis was more severe and the lesion site was closer to the proximal segment of the LV dominant artery, which also suggested a larger area of LV myocardium with insufficient blood supply [23]. Previous studies also proved that the development of MVO was associated with reduced initial TIMI grade, anterior infarct location, and larger IS [2, 3]. Therefore, these reason may explain the association between MVO and higher coronary scores.
The SYNTAX score [11, 12] and SYNTAX II score [15, 24] have excellent performance in predicting the mortality and MACE during hospitalization and follow-up in high-risk patients after PCI. However, our results showed that the Gensini score had the largest AUC in predicting MVO than the SYNTAX score and SYNTAX II score. Although three scores were grading the severity of CAD, there are many differences between them. In the SYNTAX score algorithm, the percent diameter stenosis was not carefully differentiated, and only non-occlusive (50–99% diameter stenosis) and occlusive (100% diameter stenosis) lesion were considered. In addition, excessive morphological scores may weakened the effect of thrombotic load in patients with acute STEMI. In the Gensini score algorithm, the percent diameter stenosis was carefully differentiated from 25 to 100%, and the severity score of lesion stenosis increased geometrically, which reinforced the effect of thrombotic load in patients with acute STEMI.
In the univariable analysis, three coronary scores were predictors of MVO. Interestingly, when the SYNTAX II score was added to the multivariable analysis, the Gensini score and SYNTAX score lost their predictive value. This is most likely related to the role of some clinical variables in the present study. SYNTAX II Score is a comprehensive score that connects coronary anatomy with clinical variables such as age, gender, creatinine clearance, LVEF, etc. Previous studies proved that apart from haemodynamic deterioration, some clinical parameters such as chronic renal failure, lactate, and LVEF had an impact on in-hospital mortality in high-risk patients after PCI [25, 26]. Moreover, the occurrence of MVO is closely related to the decreased LVEF and the increased inflammatory markers [2, 27], as our results demonstrated. Therefore, the SYNTAX II score including LVEF and others clinical variables performed better in predicting MVO.
The CAG scores has also been associated with the magnitude of myocardial injury. Several studies have shown that the SYNTAX score correlated signifcantly with biomarkers of cardiac injury [28, 29]. In a CMR study, Gao et al. [23] observed SYNTAX score was signifcant positive correlation with IS and was the independent predictor of high IS (≥ mean 35.43%LV). These findings were consistent with those of our study. Furthermore, in our study, Gensini score showed the strongest correlation with IS (%LV) than other scores. Previous studies showed that Gensini score was correlated with atherosclerotic plaque burden assessed by intracoronary ultrasound [30]. Therefore, the Gensini score could be a more simple and effective tool for infarct severity assessment post-STEMI.
The study had several limiations. First, this was a single-center study with a small sample size. A multi-center studies with larger sample size would be required reconfirm our results. Second, The observational retrospective design of this study may have resulted in bias in information selection. Finally, this study used angiography-based visual scoring to predict MVO and the results may be affected by observer subjective factors.
Conclusion
In patients with acute STEMI undergoing primary PCI treatment, the peak troponin I and SYNTAX II score may be an independent predictor of MVO.
Availability of data and materials
The data set supporting the results of this article are included within the article. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- STEMI:
-
ST-segment elevation myocardial infarction
- PCI:
-
Percutaneous coronary intervention
- MVO:
-
Microvascular obstruction
- CMR:
-
Cardiac magnetic resonance
- CAG:
-
Coronary artery angiography
- ECG:
-
Electrocardiography
- TIMI:
-
Thrombolysis in myocardial infarction
- SSFP:
-
Steady-state free precession
- STIR:
-
Short time inversion recovery
- LGE:
-
Late gadolinium enhancement
- PSIR:
-
Phase sensitive inversion recovery
- LVEF:
-
Left ventricular ejection fraction
- AAR:
-
Area at risk
- SD:
-
Standard deviations
- IS:
-
Infarct size
- MSI:
-
Myocardial salvage index
- LV:
-
Left ventricular
- AUC:
-
Area under the curve
- ROC:
-
Receiver operating characteristic
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- CK:
-
Creatine kinase
- CK-MB:
-
Creatine kinase isoenzyme
- PRO-BNP:
-
Pro-B-type natriuretic peptide
- CRP:
-
C-reaction protein
- LDL-C:
-
Low density lipoprotein cholesterol
- HDL-C:
-
High density lipoprotein cholesterol
- LCX:
-
Left circumflex coronary artery
- LAD:
-
Left anterior descending artery
- RCA:
-
Right coronary artery
- CAD:
-
Coronary artery disease
References
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. ESC Scientific Document Group. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–177.
Carrick D, Haig C, Ahmed N, McEntegart M, Petrie MC, Eteiba H, et al. Myocardial hemorrhage after acute reperfused ST-segment-elevation myocardial infarction: relation to microvascular obstruction and prognostic significance. Circ Cardiovasc Imaging. 2016;9(1): e004148.
de Waha S, Patel MR, Granger CB, Ohman EM, Maehara A, Eitel I, et al. Relationship between microvascular obstruction and adverse events following primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: an individual patient data pooled analysis from seven randomized trials. Eur Heart J. 2017;38(47):3502–10.
Niccoli G, Scalone G, Lerman A, Crea F. Coronary microvascular obstruction in acute myocardial infarction. Eur Heart J. 2016;37(13):1024–33.
Becker LC, Ambrosio G. Myocardial consequences of reperfusion. Prog Cardiovasc Dis. 1987;30:23–44.
Zhang L, Yang ZG, Xu H, Yang MX, Xu R, Chen L, et al. Histological validation of cardiovascular magnetic resonance T1 mapping for assessing the evolution of myocardial injury in myocardial infarction: an experimental study. Korean J Radiol. 2020;21(12):1294–304.
Zhang M, Lu Y, Li Z, Shao Y, Chen L, Yang Y, et al. Value of fast MVO identification from contrast-enhanced cine (CE-SSFP) combined with myocardial strain in predicting adverse events in patients after ST-elevation myocardial infarction. Front Cardiovasc Med. 2022;21(8): 804020.
Robbers LF, Eerenberg ES, Teunissen PF, Jansen MF, Hollander MR, Horrevoets AJ, et al. Magnetic resonance imaging-defined areas of microvascular obstruction after acute myocardial infarction represent microvascular destruction and haemorrhage. Eur Heart J. 2013;34(30):2346–53.
Ong AT, Serruys PW, Mohr FW, Morice MC, Kappetein AP, Holmes DR Jr, et al. The SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) study: design, rationale and run-in phase. Am Heart J. 2006;151(6):1194–204.
Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51(3):606.
Bundhun PK, Sookharee Y, Bholee A, Huang F. Application of the SYNTAX score in interventional cardiology: a systematic review and meta-analysis. Medicine (Baltimore). 2017;96(28): e7410.
Yoon YH, Ahn JM, Kang DY, Park H, Cho SC, Lee PH, Lee SW, Park SW, Park DW, Park SJ. Impact of syntax score on 10-year outcomes after revascularization for left main coronary artery disease. JACC Cardiovasc Interv. 2020;13(3):361–71.
Tasar O, Karabay AK, Oduncu V, Kirma C. Predictors and outcomes of no-reflow phenomenon in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Coron Artery Dis. 2019;30(4):270–6.
Matos LCV, Carvalho LS, Modolo R, Santos S, Silva JCQE, Almeida OLR, et al. Gensini score and thrombus burden add predictive value to the SYNTAX score in detecting no-reflow after myocardial infarction. Arq Bras Cardiol. 2021;116(3):466–72 (English, Portuguese).
Hayıroğlu Mİ, Keskin M, Uzun AO, Bozbeyoğlu E, Yıldırımtürk Ö, Kozan Ö, et al. Predictive value of SYNTAX score II for clinical outcomes in cardiogenic shock underwent primary percutaneous coronary intervention; a pilot study. Int J Cardiovasc Imaging. 2018;34(3):329–36.
Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, Van Dyck N, Mack M, Holmes D, Feldman T, et al. Assessment of the SYNTAX score in the syntax study. EuroIntervention. 2009;5(1):50–6.
Doll JA, O’Donnell CI, Plomondon ME, Waldo SW. Contemporary clinical and coronary anatomic risk model for 30-day mortality after percutaneous coronary intervention. Circ Cardiovasc Interv. 2021;14(12): e010863.
Carrick D, Haig C, Carberry J, May VTY, McCartney P, Welsh P, et al. Microvascular resistance of the culprit coronary artery in acute ST-elevation myocardial infarction. JCI Insight. 2016;1: e85768.
Ibanez B, Aletras AH, Arai AE, Arheden H, Bax J, Berry C, et al. Cardiac MRI endpoints in myocardial infarction experimental and clinical trials: JACC scientifific expert panel. J Am Coll Cardiol. 2019;74(2):238–56.
Kotani J, Nanto S, Mintz GS, Kitakaze M, Ohara T, Morozumi T, et al. Plaque gruel of atheromatous coronary lesion may contribute to the no-reflow phenomenon in patients with acute coronary syndrome. Circulation. 2002;106:1672–7.
Kleinbongard P, Böse D, Baars T, Möhlenkamp S, Konorza T, Schöner S, et al. Vasoconstrictor potential of coronary aspirate from patients undergoing stenting of saphenous vein aortocoronary bypass grafts and its pharmacological attenuation. Circ Res. 2011;108(3):344–52.
Shi K, Ma M, Yang MX, Xia CC, Peng WL, He Y, et al. Increased oxygenation is associated with myocardial inflammation and adverse regional remodeling after acute ST-segment elevation myocardial infarction. Eur Radiol. 2021;31(12):8956–66.
Gao G, Feng L, Fu J, Li Y, Huo Z, Zhang L, et al. Prognostic value of the SYNTAX score on myocardial injury and salvage in STEMI patients after primary percutaneous coronary intervention: a single-center retrospective observational study. BMC Cardiovasc Disord. 2021;21(1):591.
Kurniawan E, Ding FH, Zhang Q, Yang ZK, Hu J, Shen WF, Zhang RY. Predictive value of SYNTAX score II for clinical outcomes in octogenarian undergoing percutaneous coronary intervention. J Geriatr Cardiol. 2016;13(9):733–9.
Hayıroğlu Mİ, Keskin M, Uzun AO, Yıldırım Dİ, Kaya A, Çinier G, et al. Predictors of In-hospital mortality in patients with ST-segment elevation myocardial infarction complicated With cardiogenic shock. Heart Lung Circ. 2019;28(2):237–44.
Çinar T, Hayiroğlu Mİ, Şeker M, Doğan S, Çiçek V, Öz A, et al. The predictive value of age, creatinine, ejection fraction score for in-hospital mortality in patients with cardiogenic shock. Coron Artery Dis. 2019;30(8):569–74.
Mayr A, Klug G, Schocke M, Trieb T, Mair J, Pedarnig K, et al. Late microvascular obstruction after acute myocardial infarction: relation with cardiac and inflammatory markers. Int J Cardiol. 2012;157:391–6.
Namat RA, Burlacu A, Tinica G, Covic A, Mitu F. Using the SYNTAX score to predict myocardial injury early after on-pump coronary artery bypass surgery: a single-centre experience analysis. Kardiochir Torakochirurgia Pol. 2020;17(2):76–82.
Abu Sharar H, Helfert S, Vafaie M, Pleger ST, Chorianopoulos E, Bekeredjian R, et al. Identifcation of patients at higher risk for myocardial injury following elective coronary artery intervention. Catheter Cardiovasc Interv. 2020;96(3):578–85.
Neeland IJ, Patel RS, Eshtehardi P, Dhawan S, McDaniel MC, Rab ST, et al. Coronary angiographic scoring systems: an evaluation of their equivalence and validity. Am Heart J. 2012;164(4):547–52.
Acknowledgements
Not applicable.
Funding
This study has received funding by the SKY Imaging Research Fund of China Foundation for International Medical Exchange (ID:Z-2014-07-2101).
Author information
Authors and Affiliations
Contributions
ZL and HY conceived and supervised the study; ZL and DW designed experiments; ZL, HY, DW, YZ, YF, YZ and YZ performed experiments; YZ and YF analyzed data; ZL wrote the manuscript; YZ and YZ made manuscript revisions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was approved by the ethical committee of Lianyungang First People's Hospital (KY-20211030001–01) and received informed consent from the patients. Patient data were completely anonymized. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Z., Yin, H., Wang, D. et al. Prediction of microvascular obstruction by coronary artery angiography score after acute ST-segment elevation myocardial infarction: a single-center retrospective observational study. BMC Cardiovasc Disord 22, 410 (2022). https://doi.org/10.1186/s12872-022-02836-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-02836-x