Abstract
Background
SYNTAX score (SS) was shown to positively correlate with postprocedural myocardial injury in patients after elective coronary artery intervention, but evidence about the association of SS with myocardial salvage in ST-segment elevation myocardial infarction (STEMI) patients is still needed. This study aimed to evaluate the prognostic value of SS for myocardial injury and salvage assessed by cardiac magnetic resonance (CMR) after primary percutaneous coronary intervention (PCI) in STEMI patients.
Methods
This single-center retrospective study consecutively enrolled STEMI patients who had undergone primary PCI within 12 h from symptom onset. Both angiography and CMR were performed during hospitalization, and patients were divided into low SS (SS ≤ 22), mediate-high SS (SS > 22) groups. Correlation and multivariable analyses were performed.
Results
A total of 149 STEMI patients (96 low SS, 53 mediate-high SS) were included. In terms of myocardial injury parameters, there was a positive correlation (p < 0.001, Spearman r = 0.292) between SS and infarct size (IS), and a negative correlation (p < 0.001, Spearman r = − 0.314) between SS and myocardial salvage index (MSI). In the multivariable model, SS (> 22 as categorical variable, OR = 2.245, 95% CI [1.002–5.053], p = 0.048; as continuous variable, OR = 1.053, 95% CI [1.014–1.095], p = 0.008) was significantly associated with high IS (≥ mean 35.43). The areas under the receiver operating characteristic (ROC) curves of SS for high IS and low MSI (≤ median 28.01) were 0.664 and 0.610.
Conclusions
In STEMI patients undergoing primary PCI, SYNTAX score positively correlated with infarct size and negatively with myocardial salvage, indicating an independent predictive value of the myocardial injury.
Similar content being viewed by others
Background
Recovery from reperfused myocardial infarction (MI) is burdened by the occurrence of dynamic tissue changes, such as edema, inflammation, microvascular obstruction and hemorrhage [1, 2]. Microvascular obstruction (MVO) is the underlying cause for the no-reflow phenomenon in ST-segment elevation myocardial infarction (STEMI); it is strongly associated with mortality and hospitalization for heart failure (HF) within 1 year; and is considered to be a main secondary endpoint with the independent predictive value of long-term major cardiovascular adverse events (MACE) [2,3,4]. Furthermore, in acute MI patients, a high extent of myocardial loss after STEMI (infarct size, IS) and intramyocardial hemorrhage (IMH) is closely related to all-cause mortality and hospitalization for HF or MACE [5, 6]. Accordingly, myocardial salvage, defined as the amount of myocardium that is jeopardized by a coronary occlusion but spared from infarction, can be used to compare different treatment options so that strategies that benefit salvage could be implemented in clinical practice [7,8,9,10].
Early assessment of myocardial salvage is the most important during the intense care phase. Cardiac magnetic resonance (CMR) is the gold-standard technique for noninvasive myocardial tissue characterization. It is increasingly used for improved long-term risk stratification of post-MI patients or initial evaluation preceding percutaneous coronary intervention (PCI) [2]. Typical indexes of CMR measured 3 to 7 days post-MI are recommended as CMR endpoints in clinical trials [11, 12]. Still, a more integrated approach is often needed to evaluate the complex coronary artery disease (CAD) and the prognosis of STEMI.
The anatomical Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX score, SS) is an important angiographic scoring system that can help clinicians establish the optimum revascularization approach in patients with CAD [13,14,15,16]. Previous studies proved that SS was an independent predictor of MACE and 3 year-mortality after primary PCI [17, 18]. It was also found that SS correlated significantly with cardiac troponin releases after elective PCI and could predict peri-procedural myocardial injury defined as elevated troponin I at 6–24 h post-PCI [19, 20]. However, studies on the association of SS with myocardial injury and salvage as CMR endpoints are rare, and mostly limited to case reports.
Based on the above, the study aimed to evaluate the prognostic value of SS for myocardial injury and salvage assessed by CMR in STEMI patients after primary PCI.
Methods
Study design and participants
This single-center retrospective observational study enrolled STEMI patients who underwent primary PCI at Cangzhou central hospital (tertiary care hospital) between October 2018 and September 2020. Inclusion criteria were as follows: (1) electrocardiography (ECG) features consistent with acute STEMI in accordance to Fourth Universal Definition of Myocardial Infarction [1]; (2) time duration within 12 h from typical chest pain to primary PCI; (3) CMR within 3–10 days from symptom onset. In addition, patients were excluded for the following reasons: (1) old myocardial infarction history; (2) poor image quality; (3) declined CMR for personal reasons. The present study was approved by the ethical committee of Cangzhou Central Hospital (2020-286-01). The requirement for informed consent was waived by the ethical committee of Cangzhou Central Hospital due to the retrospective nature of the study.
PCI procedures
Primary PCI was performed based on current guidelines [21]. Patients were administered a loading dosage of aspirin 300 mg (Bayer, 100 mg) and clopidogrel 300 mg (Plavix, 75 mg) or ticagrelor 180 mg (BRILINTA, 90 mg) before coronary angiography and PCI was performed via radial access using a 6-F arterial sheath. After access was established, 2500 U of unfractionated heparin was injected through the sheath. Coronary angiography was performed using a 6-F IL 3.5 multifunctional guiding catheter (Terumo, Tokyo, Japan). ECG and invasive blood pressure monitoring were continuously performed during the surgery. For PCI, additional heparin (total 100 U/kg, including the previous dose) was routinely administered through the arterial sheath. The guiding catheter was deployed at the ostium of the coronary artery for diagnostic angiography. A revascularization strategy (balloon angioplasty only or stenting) was chosen based on the surgeon’s decision. After the procedure, patients were administered a maintenance dosage of aspirin 100 mg daily and ticagrelor 90 mg twice a day or clopidogrel 75 mg once a day. Additional medications, such as statins, β-receptor blockers, angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, glycoprotein IIb/IIIa inhibitors, and low-molecular-weight heparin, were administered based on the recommended guidelines unless contraindicated. Pre- and post-PCI antegrade flow in the infarct-related artery was characterized using the TIMI system.
SYNTAX score
The SS for each patient was calculated retrospectively, based on scoring for all coronary lesions with diameter stenosis > 50%, and vessels with diameter > 1.5 mm, using the SS algorithm, as recommended [14, 16]. The calculation was done using an openly accessible web-based score calculator (http://www.syntaxscore.com). Based on the previous reports [22, 23] SS was categorized as low (≤ 22), intermediate (22 < SYNTAX score ≤ 32), or high (≥ 33), and patients were divided into low SS and mediate-high SS groups. The SYNTAX score was assessed visually by two experienced interventional cardiologists trained to perform SYNTAX score assessments and blinded to the treatment and CMR data. Every significant inter-observer difference required a recalculation.
Laboratory tests, echocardiography and CMR
Blood samples were taken immediately after hospitalization, and echocardiography was performed on 5 (3–7) days from symptom onset. CMR was performed on 7.15 (5.26–8.24) days from symptom onset using a 3.0-T scanner (GE Discovery MR750w; GE Healthcare, Milwaukee, WI, USA) with electrocardiographic-gated image acquisition, as described in previous studies [24, 25]. MRI parameters were measured on short-axis images covering the entire left ventricle (8-/0-mm slice thickness/slice gap) with the following sequences: a steady-state free precession (SSFP) cine sequence to determine the left ventricular (LV) function, mass and volume, and a short-tau inversion recovery T2-weighted (T2-STIR) sequence to determine the area at risk (AAR) of myocardial infarction. Late gadolinium enhancement (LGE) images were acquired approximately 10 ~ 15 min after the intravenous administration of gadolinium-based contrast medium (0.2 mmol/kg, Magnevist, gadopentetate dimeglumine injection, Bayer) to determine the IS.
Analysis was performed using dedicated software (cmr42 version 5.11.3, Circle Cardiovascular Imaging, Calgary, Alberta, Canada). Images were anonymized, batched, and analyzed in a blinded fashion by two experienced operators. The AAR was defined as a high-signal myocardial edema mass/LV mass ratio. The IS was defined as the hyperenhanced myocardium on the LGE images and is expressed as the infarcted LV mass/LV mass ratio. MVO was defined as dark areas surrounded by hyperenhanced myocardium on the LGE images. The presence of IMH was defined as hypointense areas within the brighter edematous zone on T2-STIR images. The papillary muscles were included in the LV cavity volume. The regions of interest for the volumes of AAR, IMH, IS, and MVO were created by manually drawing the lesion contours. In contrast, the LV volume was calculated by the semiautomated drawing of endocardial and epicardial contours on each slice for the whole LV myocardium. Myocardial edema was described as areas with a signal intensity > 5 standard deviations (SD) that of remote normal myocardium. The IS was calculated using the > 5 SD method. Discordant cases were reviewed and reconciled with superior imaging specialists. The myocardial salvage index (MSI) was defined as (AAR − IS)/AAR × 100.
For echocardiographic evaluation, Xcelera R4.1 (Philips Medical Systems) was used. Echocardiographic morphological and functional parameters were measured according to the definitions and recommendations from the available American Society of Echocardiography guidelines [26].
Statistical analysis
Categorical data are presented as numbers and percentages, and continuous data are presented as the mean (standard deviation) or median (interquartile range). The Shapiro–Wilk test was applied to assess for data normality. Continuous variables with normal distributions were compared using the t-test. Continuous parameters that were not normally distributed were compared using the Mann–Whitney test. Categorical variables were compared using the chi-squared test (Fisher’s exact test when the expected value was < 5). Spearman’s correlation coefficient was used to analyze associations between SS and CMR or echocardiographic parameters. Independent predictors of high IS and low MSI were determined in a multivariable binary logistic regression model using the backward stepwise method adjusted for all baseline variables found significant (p < 0.05) in the univariable logistic regression model. Receiver operating characteristic (ROC) curves were generated to determine the usefulness of SS to discriminate high IS and low MSI. All statistical analyses were performed using SPSS version 20 (IBM, Armonk, NY, USA) and graphs were generated using GraphPad Prism version 8.0 (GraphPad Software, La Jolla, CA, USA). P-value of < 0.05 was regarded as statistically significant.
Results
Baseline characteristics of patients
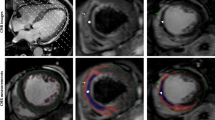
A total of 215 AMI patients who underwent primary PCI within 12 h from symptom onset were retrospectively included. Out of the 39 with no CMR data, 24 with old myocardial infarction, and three with poor image quality were excluded. Finally, 149 patients (mean age 59.89 ± 10.86 years, 72.5% male) were enrolled for analysis (Fig. 1 and Table 1). Examples of obtained arteriographic results are illustrated in Fig. 2. According to SS (17[9–25]), patients were divided into low SS (≤ 22, n = 96) and mediate-high SS (> 22, n = 53) groups. Differences in baseline characteristics between the two groups are shown in Table 1. Compared with the low SS group, patients in the mediate-high SS group were older (58.32 ± 11.47 vs. 62.72 ± 9.09, p = 0.011), and had a lower BMI (26.25 ± 3.62 vs. 24.92 ± 2.86, p = 0.023). The prevalence of multivessel disease (p < 0.001), initial TIMI thrombus grade 4/5 (p = 0.002), initial TIMI flow grade 0/1 (p = 0.008), and APOB (p = 0.038) were higher but creatinine clearance rate (p = 0.016) was lower in the mediate-high SS group. There were no differences between groups concerning medical history, culprit lesion, mode of reperfusion, and medications after surgery (all p > 0.05).
Two case examples of arteriography and cardiac magnetic resonance image. Case one (a–e): A 59 years old man with anterior ST-elevation myocardial infarction was identified to have a single total occluded LAD (SYNTAX score 18.5 and infarct size 22.74); Case two (f–j): A 64 years old man also with anterior ST-elevation myocardial infarction was identified to have total occluded LAD and diffused diseased intermediate branch and RCA (SYNTAX score 32.5 and infarct size 54.91). LAD left anterior descending artery; RCA right coronary artery
Transthoracic echocardiography and CMR parameters
All transthoracic echocardiography (TTE) parameters were comparable between the two groups (Table 2). Whereas CMR showed a lower left ventricular ejection fraction (LVEF, 52.86 ± 13.45 vs. 45.65 ± 12.01%, p = 0.001), MSI (30.30[19.23–45.41] vs. 24.52[13.92–35.69] %, p = 0.016) and higher left ventricular end-systolic volume (LVESV, 51.28[38.23,72.17] vs. 63.96[51.34–80.38] mL, p = 0.029), and IS (33.93 ± 11.94 vs. 38.06 ± 9.40%LV, p = 0.029) in mediate-high SS group patients when compared with those in low SS group. There was no significant difference between the two groups in terms of MVO, IMH and AAR (Table 2 and Fig. 3).
Comparison of CMR parameters between the mediate-high SS group and low SS group (a: non-normal distributed parameters; b: normal distributed parameters). MVO microvascular obstruction; IMH intramyocardial hemorrhage; LVEF left ventricular ejection fraction; CMR cardiac magnetic resonance imaging; IS infarct size; LV left ventricular; AAR area at risk; MSI myocardial salvage index
Correlations between baseline variables and CMR parameters
Correlations between baseline variables (SS, CK, initial TIMI flow, GRACE score, CRUSADE score) and CMR parameters by Spearman correlation analysis are presented in Table 3. Among them, SS (r = 0.292, p < 0.001) and CK (r = 0.328, p < 0.001) showed relative stronger correlation with IS (%LV) than other variables. Also, SS (r = -0.314, p < 0.001) and initial TIMI flow (r = 0.216, p = 0.011) were more correlated with MSI. Therefore, SS had a positive correlation with IS (%LV) and a negative correlation with MSI (Fig. 4).
Univariable and multivariable analysis
Univariable analysis revealed that nine variables (all p < 0.05) were significantly associated with an increased risk of high IS (≥ mean 35.43), including initial heart rate, pro-BNP, CK, CKMB, LVEF-TTE, left ventricular end-diastolic diameter (LVEDD), infarct-related artery LAD, SS > 22 (as a categorical variable) and SS (as a continuous variable); LVEF-TTE, baseline TIMI flow 0/1 and SS (not as a categorical variable) were significant predictors for risk of low MSI (≤ median 28.01) (Table 4). After adjustment for other potential confounders including initial heart rate, pro-BNP, CK-MB, LVEDD-TTE, infarct-related artery LAD, multivariable analysis showed that LVEF-TTE (OR = 0.913, 95%CI [0.865–0.962], p = 0.001) and SS > 22 (OR = 2.245, 95%CI [1.002–5.053], p = 0.048) were significant for high IS in model 1; in model 2, LVEF-TTE (OR = 0.914, 95%CI [0.866–0.965], p = 0.001) and SS (as continuous variable) (OR = 1.053, 95%CI [1.014–1.095], p = 0.008) were also the independent predictors of high IS; for low MSI in model 3, only LVEF-TTE (OR = 0.924, 95%CI [0.881–0.970], p = 0.001) was the independent predictor. Among the three models, the SS had higher odd ratio than LVEF-TTE (Fig. 5).
Multivariable logistic regression model for high IS and low MSI. Model1, Model2, Model for low MSI: adjusted for initial heart rate, pro-BNP, CKMB, LVEDD-TTE, IRA = LAD. OR odd ratio; CI confidence interval; IS infarct size; LVEF left ventricular ejection fraction; TTE transthoracic echocardiography; MSI myocardial salvage index; TIMI thrombolysis in myocardial infarction
SYNTAX score in predicting myocardial injury and salvage
The ROC analysis results of SS predicting high IS (≥ mean 35.43) and low MSI (≤ median 28.01) are shown in Fig. 6, with AUC of 0.664 (0.577–0.751, p = 0.001), 0.610 (0.516–0.700, p = 0.026), respectively. At the optimal cutoff point of SS (10.8 for high IS, 10.3 for low MSI), the sensitivity and specificity were similar for high IS diagnosis (81.8%, 45.8%) and for low MSI (81.2%, 40.6%).
Discussion
Although the SYNTAX score was shown to positively correlate with postprocedural myocardial injury in patients after elective coronary artery intervention, quality evidence about the association of SS with myocardial salvage in STEMI patients is still needed. This study evaluated the prognostic value of SS for myocardial injury and salvage assessed by CMR after primary PCI in STEMI patients. To the best of our knowledge, the present study is the first report on the relationship between SS and myocardial injury in STEMI patients undergoing primary PCI within 12 h from symptom onset. We identified three major findings: (1) a significant positive correlation between SS and IS and a negative correlation between SS and MSI. (2) compared to the low SS group, the mediate-high group had lower LVEF as assessed by CMR and higher LVESV, but LVEDV was comparable between groups. (3) according to the univariable and multivariable logistic models, SS (both categorical and continuous variables) was the independent predictor of high IS after adjustment for confounders.
In the CvLPRIT study [27], patients treated with a staged complete revascularization (CR) had higher SS (18.3 [15–26] vs. 16 [12–21.5], p = 0.021) than those treated with immediate CR. Interestingly, staged approach patients also had larger IS (%LV) (19.1 [10.2–37.1] vs. 11.6 [6.8–17.6], p = 0.006) and lower MSI (35.1 [5.9–66.4] vs. 61.7 [37.4–75.5], p = 0.008) compared with immediate CR. However, no direct relationship among them was found. In several studies [19, 20, 28, 29], in patients undergone CABG or PCI, SS was not only positively related to peri-procedural myocardial injury (deprived by elevated cardiac troponin and CKMB 6 h after operation) but also an independent predictor of it. The increase in the release of cardiac biomarkers after selective PCI was significantly associated with the extent of atherosclerosis identified by the SS [30]. These findings were consistent with those of our study. Furthermore, in our study, no significant relationship between SS and AAR was found. Thus, the negative correlation between SS and MSI might be interpreted by the positive correlation between SS and IS.
In our study, the LVEF-TTE in the low SS group was comparable with that in the mediate-high SS group (57.63 ± 8.87 vs. 54.77 ± 9.55, p = 0.070), however, LVEF-CMR in the low SS group was significantly higher than that in the mediate-high group (52.86 ± 13.45 vs. 45.65 ± 12.01, p = 0.001). In addition, among our study population, LVEF-CMR was lower than LVEF-TTE, in line with findings reported by another recent multicenter study [31]. Compared with LVEF-TTE, LVEF-CMR significantly improved MACE prediction in patients with echocardiography-LVEF < 50% and had better prognostic meaning.
The SYNTAX score is not only an angiographic tool used to grade the complexity of coronary artery diseases and guide selecting the proper revascularization strategy [32], but also an important score to predict cardiac mortality [33] and major bleeding (defined as BARC types 3 or 5) risk after drug-eluting stent implantation, although the predictive value was lower than CRUSADE score [34]. Because in-hospital hemoglobin drop is common among patients with acute coronary syndrome [35], the predictive value of syntax score might be better in patients who met the well validated high bleeding risk criteria proposed by the academic research consortium [36]. Further research was needed to validate the hypothesis. Thus, in additional to our main findings, SYNTAX score, like PRAISE model [37], should be used as a multifunctional tool for clinical decision-making.
To specify the influence of SS on myocardial injury after STEMI could have important clinical implications. In China, CMR is available only in large hospitals. Therefore, risk stratification for STEMI patients is very important. By evaluating the SS, we might find the patients who have a high risk of myocardial injury. Despite numerous failures to date, the prevention and treatments for STEMI patients with a high risk of myocardial injury should focus on future cardiovascular research.
This study has a few limitations. Firstly, due to the retrospective nature of the study, selection bias might be present. The proportion of patients within a specific SS group (≤ 22, n = 96; 22 < & ≤ 32, n = 36; > 32, n = 17) in our population was too small to allow conclusions in all three groups. Consequently, tests of interaction were underpowered, especially when adjusted for covariables. Secondly, although all patients were enrolled consecutively, part of them declined CMR for personal reasons or unstable clinical station, for example, severe heart failure; on the other hand, only patients presented in hospital undergone primary PCI within 12 h from symptom onset were included in our study population. Thus, we should be very cautious about interpreting the conclusions in specific patients. Thirdly, considering the “shrinkage” of the infarcted region after the acute infarction phase [2], measurement by CMR may lead to IS overestimation in our study. And finally, in this single-center study, the scoring assessment was performed by highly experienced professionals, and a multi-center fully blinded study might be needed to evaluate further the predictive value of SS in everyday clinical practice.
Conclusions
In STEMI patients who had undergone primary PCI, SYNTAX score positively correlated with infarct size and negatively with myocardial salvage. SYNTAX score had an independent predictive value of the myocardial injury.
Availability of data and materials
The data set supporting the results of this article are included within the article. The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SS:
-
SYNTAX score
- STEMI:
-
ST-segment elevation myocardial infarction
- PCI:
-
Percutaneous coronary intervention
- IS:
-
Infarct size
- MSI:
-
Myocardial salvage index
- MI:
-
Myocardial infarction
- MVO:
-
Microvascular obstruction
- HF:
-
Heart failure
- MACE:
-
Major cardiovascular adverse events
- IMH:
-
Intramyocardial hemorrhage
- CMR:
-
Cardiac magnetic resonance
- PCI:
-
Percutaneous coronary intervention
- CAD:
-
Coronary artery disease
- ECG:
-
Electrocardiography
- SSFP:
-
Steady-state free precession
- LV:
-
Left ventricular
- AAR:
-
Area at risk
- LGE:
-
Late gadolinium enhancement
- SD:
-
Standard deviations
- ROC:
-
Receiver operating characteristic
- TTE:
-
Transthoracic echocardiography
- LVEDD:
-
Left ventricular end-diastolic diameter
- LAD:
-
Left anterior descending artery
References
Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, Thygesen K, Alpert JS, Jaffe AS et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J 2018.
Ibanez B, Aletras AH, Arai AE, Arheden H, Bax J, Berry C, Bucciarelli-Ducci C, Croisille P, Dall’Armellina E, Dharmakumar R, et al. Cardiac MRI endpoints in myocardial infarction experimental and clinical trials: JACC scientific expert panel. J Am Coll Cardiol. 2019;74(2):238–56.
van Kranenburg M, Magro M, Thiele H, de Waha S, Eitel I, Cochet A, Cottin Y, Atar D, Buser P, Wu E, et al. Prognostic value of microvascular obstruction and infarct size, as measured by CMR in STEMI patients. JACC Cardiovasc Imaging. 2014;7(9):930–9.
de Waha S, Patel MR, Granger CB, Ohman EM, Maehara A, Eitel I, Ben-Yehuda O, Jenkins P, Thiele H, Stone GW. Relationship between microvascular obstruction and adverse events following primary percutaneous coro nary intervention for ST-segment elevation myocardial infarction: an individual patient data pooled analysis from seven randomized trials. Eur Heart J. 2017;38(47):3502–10.
Husser O, Monmeneu JV, Sanchis J, Nunez J, Lopez-Lereu MP, Bonanad C, Chaustre F, Gomez C, Bosch MJ, Hinarejos R, et al. Cardiovascular magnetic resonance-derived intramyocardial hemorrhage after STEMI: Influence on long-term prognosis, adverse left ventricular remodeling and relationship with microvascular obstruction. Int J Cardiol. 2013;167(5):2047–54.
Stone GW, Selker HP, Thiele H, Patel MR, Udelson JE, Ohman EM, Maehara A, Eitel I, Granger CB, Jenkins PL, et al. Relationship between infarct size and outcomes following primary PCI: patient-level analysis from 10 randomized trials. J Am Coll Cardiol. 2016;67(14):1674–83.
Eitel I, Desch S, de Waha S, Fuernau G, Gutberlet M, Schuler G, Thiele H. Long-term prognostic value of myocardial salvage assessed by cardiovascular magnetic resonance in acute reperfused myocardial infarction. Heart (British Cardiac Society). 2011;97(24):2038–45.
Eitel I, Desch S, Fuernau G, Hildebrand L, Gutberlet M, Schuler G, Thiele H. Prognostic significance and determinants of myocardial salvage assessed by cardiovascular magnetic resonance in acute reperfused myocardial infarction. J Am Coll Cardiol. 2010;55(22):2470–9.
Pontone G, Guaricci AI, Andreini D, Ferro G, Guglielmo M, Baggiano A, Fusini L, Muscogiuri G, Lorenzoni V, Mushtaq S et al. Prognostic stratification of patients with ST-segment-elevation myocardial infarction (PROSPECT): a cardiac magnetic resonance study. Circ Cardiovasc Imaging 2017, 10(11).
Ortiz-Perez JT, Lee DC, Meyers SN, Davidson CJ, Bonow RO, Wu E. Determinants of myocardial salvage during acute myocardial infarction: evaluation with a combined angiographic and CMR myocardial salvage index. JACC Cardiovasc Imaging. 2010;3(5):491–500.
Stiermaier T, Jobs A, de Waha S, Fuernau G, Pöss J, Desch S, Thiele H, Eitel I. Optimized prognosis assessment in ST-segment-elevation myocardial infarction using a cardiac magnetic resonance imaging risk score. Circ Cardiovasc Imaging 2017;10(11).
McCartney PJ, Eteiba H, Maznyczka AM, McEntegart M, Greenwood JP, Muir DF, Chowdhary S, Gershlick AH, Appleby C, Cotton JM, et al. Effect of low-dose intracoronary alteplase during primary percutaneous coronary intervention on microvascular obstruction in patients with acute myocardial infarction: a randomized clinical trial. JAMA. 2019;321(1):56–68.
Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, Ståhle E, Feldman TE, van den Brand M, Bass EJ, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. New Engl J Med. 2009;360(10):961–72.
Serruys PW, Onuma Y, Garg S, Sarno G, van den Brand M, Kappetein AP, Van Dyck N, Mack M, Holmes D, Feldman T, et al. Assessment of the SYNTAX score in the syntax study. EuroIntervention. 2009;5(1):50–6.
Morice MC, Serruys PW, Kappetein AP, Feldman TE, Ståhle E, Colombo A, Mack MJ, Holmes DR, Torracca L, van Es GA, et al. Outcomes in patients with de novo left main disease treated with either percutaneous coronary intervention using paclitaxel-eluting stents or coronary artery bypass graft treatment in the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial. Circulation. 2010;121(24):2645–53.
Sianos G, Morel MA, Kappetein AP, Morice MC, Colombo A, Dawkins K, van den Brand M, Van Dyck N, Russell ME, Mohr FW, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1(2):219–27.
Li C, Zhang Q, Wang Q, Zhong J, Wang L, Li K, Yang X. Prognostic values of the SYNTAX score II and the erythrocyte sedimentation rate on long-term clinical outcomes in STEMI patients with multivessel disease: a retrospective cohort study. BMC Cardiovasc Disord. 2020;20(1):213.
Homorodean C, Iancu AC, Leucuţa D, Bãlãnescu Ş, Dregoesc IM, Spînu M, Ober M, Tãtaru D, Olinic M, Bindea D, et al. New predictors of early and late outcomes after primary percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction and unprotected left main coronary artery culprit lesion. J Interv Cardiol. 2019;2019:8238972.
van Gaal WJ, Ponnuthurai FA, Selvanayagam J, Testa L, Porto I, Neubauer S, Banning AP. The Syntax score predicts peri-procedural myocardial necrosis during percutaneous coronary intervention. Int J Cardiol. 2009;135(1):60–5.
Abu Sharar H, Helfert S, Vafaie M, Pleger ST, Chorianopoulos E, Bekeredjian R, Katus HA, Giannitsis E. Identification of patients at higher risk for myocardial injury following elective coronary artery intervention. Catheterization Cardiovasc Interv. 2020;96(3):578–85.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2017.
Neumann F-J, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet J-P, Falk V, Head SJ et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2018.
Thiele H, Desch S, Piek JJ, Stepinska J, Oldroyd K, Serpytis P, Montalescot G, Noc M, Huber K, Fuernau G, et al. Multivessel versus culprit lesion only percutaneous revascularization plus potential staged revascularization in patients with acute myocardial infarction complicated by cardiogenic shock: design and rationale of CULPRIT-SHOCK trial. Am Heart J. 2016;172:160–9.
Ekeloef S, Halladin N, Fonnes S, Jensen SE, Zaremba T, Rosenberg J, Jonsson G, Aarøe J, Gasbjerg LS, Rosenkilde MM, et al. Effect of intracoronary and intravenous melatonin on myocardial salvage index in patients with ST-elevation myocardial infarction: a randomized placebo controlled trial. J Cardiovasc Transl Res. 2017;10(5–6):470–9.
Choudry F, Hamshere S, Saunders N, Veerapen J, Bavnbek K, Knight C, Pellerin D, Locca D, Westwood M, Rakhit R, et al. A randomized double-blind control study of early intra-coronary autologous bone marrow cell infusion in acute myocardial infarction: the REGENERATE-AMI clinical trial†. Eur Heart J. 2016;37(3):256–63.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16(3):233–70.
Khan JN, Nazir SA, Greenwood JP, Dalby M, Curzen N, Hetherington S, Kelly DJ, Blackman D, Ring A, Peebles C, et al. Infarct size following complete revascularization in patients presenting with STEMI: a comparison of immediate and staged in-hospital non-infarct related artery PCI subgroups in the CvLPRIT study. J Cardiovasc Magn Reson. 2016;18(1):85.
Namat RA, Burlacu A, Tinica G, Covic A, Mitu F. Using the SYNTAX score to predict myocardial injury early after on-pump coronary artery bypass surgery: a single-centre experience analysis. Kardiochir Torakochirurgia Pol. 2020;17(2):76–82.
Chen ZW, Yang HB, Chen YH, Ma JY, Qian JY, Ge JB. Impact of multi-vessel therapy to the risk of periprocedural myocardial injury after elective coronary intervention: exploratory study. BMC Cardiovasc Disord. 2017;17(1):69.
de Azevedo DFC, Hueb W, Lima EG, Rezende PC, Linhares Filho JPP, de Carvalho GF, Martins EB, Nomura CH, Strunz CMC, Serrano Junior CV et al. Significant association of SYNTAX score on release of cardiac biomarkers in uncomplicated post-revascularization procedures among patients with stable multivessel disease: MASS-V Study group. Medicine (Baltimore) 2020, 99(8):e18973.
Marcos-Garces V, Gavara J, Lopez-Lereu MP, Monmeneu JV, Rios-Navarro C, de Dios E, Perez N, Cànoves J, Gonzalez J, Minana G et al. Ejection fraction by echocardiography for a selective use of magnetic resonance after infarction. Circ Cardiovasc Imaging 2020, 13(12):e011491.
Yoon YH, Ahn JM, Kang DY, Park H, Cho SC, Lee PH, Lee SW, Park SW, Park DW, Park SJ. Impact of syntax score on 10-year outcomes after revascularization for left main coronary artery disease. JACC Cardiovasc Interv. 2020;13(3):361–71.
Yang CH, Hsieh MJ, Chen CC, Chang SH, Wang CY, Lee CH, Hsieh IC. SYNTAX score: an independent predictor of long-term cardiac mortality in patients with acute ST-elevation myocardial infarction. Coron Artery Dis. 2012;23(7):445–9.
Iijima R, Nagashima Y, Sato K, Tokue M, Araki T, Yamazaki K, Shiba M, Hara H, Sugi K, Nakamura M. SYNTAX score predicts major bleeding following drug-eluting stent implantation in an all-comers population. Rev Esp Cardiol (Engl Ed). 2015;68(1):54–62.
Leonardi S, Gragnano F, Carrara G, Gargiulo G, Frigoli E, Vranckx P, Di Maio D, Spedicato V, Monda E, Fimiani L, et al. Prognostic implications of declining hemoglobin content in patients hospitalized with acute coronary syndromes. J Am Coll Cardiol. 2021;77(4):375–88.
Corpataux N, Spirito A, Gragnano F, Vaisnora L, Galea R, Svab S, Gargiulo G, Zanchin T, Zanchin C, Siontis GCM, et al. Validation of high bleeding risk criteria and definition as proposed by the academic research consortium for high bleeding risk. Eur Heart J. 2020;41(38):3743–9.
D’Ascenzo F, De Filippo O, Gallone G, Mittone G, Deriu MA, Iannaccone M, Ariza-Solé A, Liebetrau C, Manzano-Fernández S, Quadri G, et al. Machine learning-based prediction of adverse events following an acute coronary syndrome (PRAISE): a modelling study of pooled datasets. Lancet. 2021;397(10270):199–207.
Acknowledgements
We want to thank Mr. Jinwei Tian, Dr Ruishuang Zheng and Mr. Dongliang Yang for the statistical advice.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
GG and JZ conceived and supervised the study; GG and LF designed experiments; GG, JF, LW, HN, ZH, LZ and LK performed experiments; GG and YL analyzed data; GG wrote the manuscript; YL and JZ made manuscript revisions. All authors reviewed the results and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was approved by the ethical committee of Cangzhou Central Hospital (2020–286-01). The requirement for informed consent was waived by the ethical committee of Cangzhou Central Hospital due to the retrospective nature of the study. Patient data were completely anonymized. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gao, G., Feng, L., Fu, J. et al. Prognostic value of the SYNTAX score on myocardial injury and salvage in STEMI patients after primary percutaneous coronary intervention: a single-center retrospective observational study. BMC Cardiovasc Disord 21, 591 (2021). https://doi.org/10.1186/s12872-021-02395-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-021-02395-7