Abstract
Background
Complete and simplified Selvester QRS score have been proposed as valuable clinical tool for estimating myocardial damage in patients with ST-elevation myocardial infarction (STEMI). We sought to comprehensively compare both scoring systems for the prediction of myocardial and microvascular injury assessed by cardiac magnetic resonance (CMR) imaging in patients with acute STEMI.
Methods
In this prospective observational study, 201 revascularized STEMI patients were included. Electrocardiography was conducted at a median of 2 (interquartile range 1–4) days after the index event to evaluate the complete and simplified QRS scores. CMR was performed within 1 week and 4 months thereafter to determine acute and chronic infarct size (IS) as well as microvascular obstruction (MVO).
Results
Complete and simplified QRS score showed comparable predictive value for acute (area under the curve (AUC) = 0.64 vs. 0.67) and chronic IS (AUC = 0.63 vs. 0.68) as well as for MVO (AUC = 0.64 vs. 0.66). Peak high sensitivity cardiac troponin T (hs-cTnT) showed an AUC of 0.88 for acute IS and 0.91 for chronic IS, respectively. For the prediction of MVO, peak hs-cTnT represented an AUC of 0.81.
Conclusions
In reperfused STEMI, complete and simplified QRS score displayed comparable value for the prediction of acute and chronic myocardial as well as microvascular damage. However, both QRS scoring systems provided inferior predictive validity, compared to peak hs-cTnT, the clinical reference method for IS estimation.
Similar content being viewed by others
Background
In survivors of acute ST-elevation myocardial infarction (STEMI), the severity of myocardial damage is of major prognostic relevance [1]. Cardiac magnetic resonance (CMR) imaging enables a precise and comprehensive assessment of infarct severity after STEMI [2], but is still limited due to restricted availability in daily routine.
Previous studies have documented the capability of different electrocardiographic (ECG) markers for prognosis assessment after STEMI [3]. The Selvester QRS Score has been proposed as indicator of infarct size [4]. However, the original Selvester QRS score (=“complete QRS score”) is very complex compromising 54 individual criteria. Accordingly, a simplified version (=“simplified QRS score”) has been formed including only 37 criteria [5].
Both QRS scoring systems have been shown to correlate with the extent of myocardial damage [6, 7]. However, to date no study has directly compared the value of complete versus simplified QRS scoring system for the estimation of myocardial and microvascular damage.
The present investigation aimed to evaluate a direct comparison of complete and simplified QRS score as well as in comparison with the clinical reference method peak hs-cTnT for the prediction of CMR-derived myocardial damage in a cohort of STEMI patients treated with primary percutaneous coronary intervention (pPCI).
Methods
Study design
In this single-centre prospective observational study, we included 201 STEMI patients admitted to the coronary care unit of Innsbruck University Hospital. The flow chart of the present study is presented in Fig. 1. Inclusion criteria were first-time STEMI diagnosed in accordance with the redefined ESC/ACC committee criteria [8] and revascularization by pPCI within 12 h after symptom onset. Exclusion criteria were age under 18 years, any history of prior myocardial infarction or coronary intervention, an estimated glomerular filtration rate < 30 ml/min/1.73 m2, Killip class > II and any contraindication to CMR examination (pacemaker, aneurysm clips, orbital foreign body, claustrophobia, known or suggested contrast agent allergy to gadolinium). Furthermore, patients with bundle branch or fascicular block were excluded.
A standard 12-lead surface ECG (voltage: 10 mm/mV; speed: 25 mm/s) was conducted at discharge, at a median of 2 days (Interquartile range [IQR 1–4] after STEMI. Complete (54-criteria/32-point) [5] and simplified (37-criteria/29-point) [9] Selvester QRS scoring systems were evaluated manually by two experienced investigators, blinded to CMR results. Both scoring systems were determined by consideration of 54 and 37 criteria, respectively, based on Q or R wave duration, R or S wave amplitude and R/Q or R/S amplitude ratios. Biochemical measurements of high-sensitivity cardiac troponin T (hs-cTnT) were determined according to the standard protocols of our working group as described in detail previously [10]. A detailed medical history as well as physical examination were carried out during hospitalization and informed consent was obtained from all patients prior study inclusion. The present study protocol was approved by the local research ethics committee in concordance with the Declaration of Helsinki.
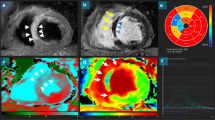
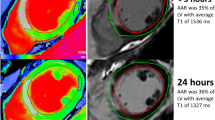
Cardiac magnetic resonance imaging
All CMR scans were performed on a 1.5-T MR imaging unit (AVANTO-scanner, Siemens, Erlangen, Germany) at 3 days (IQR 2–4) as well as 127 days (IQR 121–143) after reperfused STEMI. The detailed imaging and post-processing protocol of our research group was published in detail previously [11]. In brief, volumetric analyses were conducted on short-axis cine images using breath-hold, retrospective ECG-triggered trueFISP bright-blood sequences and for post-processing, standard software (ARGUS, Siemens, Erlangen, Germany) was used. Papillary muscles were attached to the LV volume. 15 min after the application of a 0.2 mmol/kg bolus of contrast agent (Gadovist®, Bayer Vital, Leverkusen, Germany), late gadolinium enhancement (LGE) images were acquired using an ECG-triggered phase-sensitive inversion recovery (PSIR) sequence. LGE extent was determined quantitatively on each slice using IMPAX EE workstation (Agfa HealthCare, Bonn, Germany). “Hyperenhancement” was defined as a threshold of + 5 SD above the signal intensity of remote myocardium in the opposite myocardial segment of the LV [12]. Infarct size (IS) was defined as percentage of LV myocardial mass. Microvascular obstruction (MVO) was characterized as persisting area of “hypoenhancement” within the infarcted myocardium [13]. Experienced readers analyzed all CMR images, blinded to clinical data as well as ECG results.
Statistical analysis
IBM SPSS Statistics 24.0 (IBM, Armonk, NY, USA) and MedCalc Version 15.8 (Ostend, Belgium) were used for statistical analyses. Continuous variables were expressed as median with corresponding IQR. Categorical variables were presented as absolute numbers with corresponding percentages. Chi-square test was used to assess differences in categorical variables. Differences in continuous variables between two groups were evaluated by Mann–Whitney U-test. Receiver operating characteristic (ROC) curve analysis was applied to evaluate area under the curve (AUC) for the prediction of acute as well as chronic IS and MVO. AUC values were compared according to a method published by DeLong et al. [14]. For multivariable analysis, binary logistic regression analysis was used. A baseline univariable model was created including simplified and complete QRS score as well as hs-cTnT for the prediction of myocardial damage. All parameters showing a p-value of < 0.05 in univariable analysis were further included in multivariable analyses. Cut-offs for both QRS scores and large IS were defined by the median of the present cohort. For all analyses, a two-tailed p-value of < 0.05 was considered as statistically significant.
Results
Baseline characteristics
We included 201 STEMI patients undergoing pPCI with a median treatment delay of 194 (IQR 128–378) minutes. The mean age of the overall cohort was 56 (IQR 50–67) years. The baseline characteristics are provided in detail by Table 1.
Clinical associates of QRS scores
Patients with complete QRS scores > median of 12 points were older (p = 0.001), showed higher heart rate (p = 0.041), higher hs-cTnT levels (p < 0.001), larger IS in acute (p = 0.004) and chronic (p = 0.008) setting and higher presence of MVO (p = 0.020).
Patients with simplified QRS scores > median of 4 points were older (p = 0.004), presented with higher body mass index levels (p = 0.044), had higher rates of anterior infarct localisation (p < 0.001), higher hs-cTnT levels (p < 0.001), larger IS in acute (p = 0.001) and chronic (p = 0.003) setting and higher presence of MVO (p = 0.013).
QRS scoring system and myocardial damage
Univariable and multivariable associations between both QRS scoring systems as well as hs-cTnT and myocardial damage are summarized in Table 2. In univariable logistic regression analysis, all three included parameters showed significant association with IS and MVO. In multivariable analysis, including complete, simplified QRS score and peak hs-cTnT, peak hs-cTnT emerged as independent predictor of acute (p < 0.001) as well as chronic (p < 0.001) IS and MVO (p < 0.001). AUC values of both QRS scoring systems and hs-cTnT are presented in detail by Table 3. AUC values of complete and simplified QRS score were comparable for the prediction of acute IS (AUC = 0.64, 95% confidence interval (CI) 0.56 to 0.72, p = 0.001; AUC = 0.67, 95% CI 0.59 to 0.74, p < 0.001, respectively), chronic IS (AUC = 0.63, 95% CI 0.55 to 0.71, p = 0.002; AUC = 0.68, 95% CI 0.60 to 0.75, p < 0.001, respectively) and MVO (AUC = 0.64, 95% CI 0.56 to 0.72, p = 0.001; AUC = 0.66, 95% CI 0.58 to 0.73, p < 0.001, respectively). Peak hs-cTnT resulted in a higher AUC for the prediction of acute (AUC = 0.88, 95% CI 0.83 to 0.93, p < 0.001) and chronic IS (AUC = 0.91, 95% CI 0.88 to 0.95, p < 0.001) as well as for the prediction of MVO (AUC = 0.81, 95% CI 0.75 to 0.87, p < 0.001) (Fig. 2).
Receiver operating characteristic curves for the prediction of acute IS (> 15% of LVMM) (a), chronic IS (> 10% of LVMM) (b) and presence of MVO (c): Peak hs-cTnT, complete and simplified QRS score. Abbreviations: IS=Infarct size; LVMM = Left ventricular myocardial mass; hs-cTnT = High-sensitivity cardiac troponin T; MVO = Microvascular obstruction
Discussion
This is the first CMR study evaluating a direct comparison of the complete and simplified QRS scoring system as well as in comparison with hs-cTnT for the prediction of myocardial damage in STEMI patients undergoing pPCI. The major findings of the present study can be summarized as follows: Complete and simplified QRS score showed comparable predictive value for acute and chronic IS estimation as well as MVO. However, peak hs-cTnT showed higher predictive value for the assessment of myocardial damage. Taken together, both scoring systems could not show any benefit regarding infarct severity assessment after reperfused STEMI in the era of hs-cTnT.
QRS scoring system and myocardial damage
The extent of myocardial necrosis is one of the strongest determinants of clinical outcome in STEMI patients [1, 15]. ECG represents a cost-effective, non-invasive and globally available tool allowing an estimation of myocardial damage in the setting of STEMI. Various ECG scoring systems for the assessment of IS have been developed [6, 16, 17]. Selvester et al. developed the QRS score based on knowledge of the normal sequence of ventricular depolarization in dogs and expanded this model to the standard 12-lead ECG and body surface in a simulated male human torso [18, 19]. From this model, criteria for the quantitation of myocardial infarcts from the ECG were developed [20]. Several previous studies have illustrated the usefulness of Selvester QRS scoring system for assessing myocardial necrosis [21, 22]. Before the era of hs-cTnT, positive correlation was found between Selvester QRS score and serum creatine kinase for IS estimation [23, 24]. In the last years, hs-cTnT has been proposed as biomarker of choice for the assessment of myocardial damage in acute STEMI [25]. Tjandrawidjaja et al. described significant relation between peak troponin T and complete QRS score in a large STEMI cohort [26]. In line with the latter study, we also found significant association between both QRS scoring systems and hs-cTnT. Nowadays CMR represents the gold standard for estimating IS in vivo [1]. Concordant with our study, only moderate correlation was found between CMR derived IS and complete Selvester QRS score [21, 27].
Besides IS, microvascular injury emerged as strong predictor of adverse cardiovascular events after STEMI [15, 28, 29]. Previous data reported a rate of MVO up to 55% in patients after revascularized STEMI [28]. This is consistent with the present data, naming a rate of MVO in 51% of our study population. Data concerning the relationship between Selvester QRS score and MVO are limited [21]. Watanabe et al. reported in a small cohort of 62 patients with acute myocardial infarction significant correlation between simplified QRS score and CMR determined MVO volume [30]. Anyway, previous studies did not directly compare associations between complete and simplified QRS score with microvascular injury. The present study provides deeper insights as we investigated a direct comparison of both QRS scores regarding MVO. In this comparison, both QRS scoring systems showed comparable predictive value for estimating MVO. These results confirm the theory of the association between high QRS scores with irreversible myocardial damage [30]. However, concordant with our data, hs-cTnT still represents one of the best parameters evaluating microvascular injury [31, 32].
Limitations
Limitations of the present study have to be declared. Firstly, we included relatively stable STEMI patients with Killip class < III in order to perform high-quality CMR imaging. Therefore, these data may not be generalizable for patients in worse clinical condition. Nevertheless, the majority of STEMI patients represent with Killip class < III [33]. Secondly, Selvester QRS scores were evaluated at a single time point, and therefore their predictive value might be different if measured on other time points. Thirdly, T2-weighted edema was not included in the present study mostly due to the limited validity of this imaging sequence [34, 35].
Conclusions
Complete and simplified Selvester QRS score showed comparable predictive value for the assessment of CMR derived IS and MVO in reperfused STEMI. However, compared to peak hs-cTnT, the clinical reference method for the assessment of myocardial damage, both QRS scoring systems revealed inferior predictive value.
Availability of data and materials
The raw data of this study will not be shared publically because they will be applied for further researches of this series, but authors do agree that the data can be shared individually if requested.
Abbreviations
- AUC:
-
Area under the curve
- CI:
-
Confidence interval
- CMR:
-
Cardiac magnetic resonance
- ECG:
-
Electrocardiography
- hs-cTnT:
-
High-sensitivity cardiac troponin T
- IQR:
-
Interquartile range
- IS:
-
Infarct size
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricular
- LVMM:
-
Left ventricular myocardial mass
- MVO:
-
Microvascular obstruction
- pPCI:
-
Primary percutaneous coronary intervention
- PSIR:
-
Phase sensitive inversion recovery
- ROC:
-
Receiver operator characteristics
- SD:
-
Standard deviation
- STEMI:
-
ST-segment elevation myocardial infarction
References
Reinstadler SJ, Thiele H, Eitel I. Risk stratification by cardiac magnetic resonance imaging after ST-elevation myocardial infarction. Curr Opin Cardiol. 2015;30(6):681–9.
Klug G, Metzler B. Assessing myocardial recovery following ST-segment elevation myocardial infarction: short- and long-term perspectives using cardiovascular magnetic resonance. Expert Rev Cardiovasc Ther. 2013;11(2):203–19.
Reindl M, Reinstadler SJ, Feistritzer HJ, Niess L, Koch C, Mayr A, et al. Persistent T-wave inversion predicts myocardial damage after ST-elevation myocardial infarction. Int J Cardiol. 2017;241:76–82.
Selvester RH, Wagner GS, Hindman NB. The Selvester QRS Scoring system for estimating myocardial infarct size. The development and application of the system. Arch Intern Med. 1985;145(10):1877–81.
Bounous EP Jr, Califf RM, Harrell FE Jr, Hinohara T, Mark DB, Ideker RE, et al. Prognostic value of the simplified Selvester QRS score in patients with coronary artery disease. J Am Coll Cardiol. 1988;11(1):35–41.
Seino Y, Staniloff HM, Shell WE, Mickle D, Shah PK, Vyden JK. Evaluation of a QRS scoring system in acute myocardial infarction: relation to infarct size, early stage left ventricular ejection fraction, and exercise performance. Am J Cardiol. 1983;52(1):37–42.
Wagner GS, Freye CJ, Palmeri ST, Roark SF, Stack NC, Ideker RE, et al. Evaluation of a QRS scoring system for estimating myocardial infarct size. I. Specificity and observer agreement. Circulation. 1982;65(2):342–7.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012;33(20):2551–67.
Haisty WK Jr, Pahlm O, Wagner NB, Pope JE, Wagner GS. Performance of the automated complete Selvester QRS scoring system in normal subjects and patients with single and multiple myocardial infarctions. J Am Coll Cardiol. 1992;19(2):341–6.
Reindl M, Reinstadler SJ, Feistritzer HJ, Klug G, Tiller C, Mair J, et al. Relation of inflammatory markers with myocardial and microvascular injury in patients with reperfused ST-elevation myocardial infarction. Eur Heart J Acute Cardiovasc Care. 2017;6(7):640–9.
Reinstadler SJ, Klug G, Feistritzer HJ, Kofler M, Pernter B, Gobel G, et al. Prognostic value of left ventricular global function index in patients after ST-segment elevation myocardial infarction. Eur Heart J Cardiovasc Imaging. 2016;17(2):169–76.
Bondarenko O, Beek AM, Hofman MB, Kuhl HP, Twisk JW, van Dockum WG, et al. Standardizing the definition of hyperenhancement in the quantitative assessment of infarct size and myocardial viability using delayed contrast-enhanced CMR. J Cardiovasc Magn Reson. 2005;7(2):481–5.
Reindl M, Reinstadler SJ, Feistritzer HJ, Mueller L, Koch C, Mayr A, et al. Fibroblast growth factor 23 as novel biomarker for early risk stratification after ST-elevation myocardial infarction. Heart. 2017;103(11):856–62.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–45.
Reinstadler SJ, Stiermaier T, Fuernau G, de Waha S, Desch S, Metzler B, et al. The challenges and impact of microvascular injury in ST-elevation myocardial infarction. Expert Rev Cardiovasc Ther. 2016;14(4):431–43.
Roubin GS, Shen WF, Kelly DT, Harris PJ. The QRS scoring system for estimating myocardial infarct size: clinical, angiographic and prognostic correlations. J Am Coll Cardiol. 1983;2(1):38–44.
Blackburn H, Keys A, Simonson E, Rautaharju P, Punsar S. The electrocardiogram in population studies. A classification system. Circulation. 1960;21:1160–75.
Scher AM, Young AC. The pathway of ventricular depolarization in the dog. Circ Res. 1956;4(4):461–9.
Selvester RH, Collier CR, Pearson RB. Analog computer model of the Vectorcardiogram. Circulation. 1965;31:45–53.
Selvester RH, Solomon JC, Gillespie TL. Digital computer model of a total body electrocardiographic surface map. An adult male-torso simulation with lungs. Circulation. 1968;38(4):684–90.
Holmes LE, Nguyen TL, Hee L, Otton J, Moses DA, French JK, et al. Electrocardiographic measurement of infarct size compared to cardiac MRI in reperfused first time ST-segment elevation myocardial infarction. Int J Cardiol. 2016;220:389–94.
Pahlm US, Chaitman BR, Rautaharju PM, Selvester RH, Wagner GS. Comparison of the various electrocardiographic scoring codes for estimating anatomically documented sizes of single and multiple infarcts of the left ventricle. Am J Cardiol. 1998;81(7):809–15.
Hindman N, Grande P, Harrell FE Jr, Anderson C, Harrison D, Ideker RE, et al. Relation between electrocardiographic and enzymatic methods of estimating acute myocardial infarct size. Am J Cardiol. 1986;58(1):31–5.
Grande P, Hindman NB, Saunamaki K, Prather JD, Hinohara T, Wagner GS. A comprehensive estimation of acute myocardial infarct size using enzymatic, electrocardiographic and mechanical methods. Am J Cardiol. 1987;59(15):1239–44.
Mair J. High-sensitivity cardiac troponins in everyday clinical practice. World J Cardiol. 2014;6(4):175–82.
Tjandrawidjaja MC, Fu Y, Westerhout CM, Wagner GS, Granger CB, Armstrong PW, et al. Usefulness of the QRS score as a strong prognostic marker in patients discharged after undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Am J Cardiol. 2010;106(5):630–4.
Carlsen EA, Bang LE, Ahtarovski KA, Engstrom T, Kober L, Kelbaek H, et al. Comparison of Selvester QRS score with magnetic resonance imaging measured infarct size in patients with ST elevation myocardial infarction. J Electrocardiol. 2012;45(4):414–9.
Reindl M, Reinstadler SJ, Feistritzer HJ, Theurl M, Basic D, Eigler C, et al. Relation of Low-Density Lipoprotein Cholesterol With Microvascular Injury and Clinical Outcome in Revascularized ST-Elevation Myocardial Infarction. J Am Heart Assoc. 2017;6:10.
Wu KC, Zerhouni EA, Judd RM, Lugo-Olivieri CH, Barouch LA, Schulman SP, et al. Prognostic significance of microvascular obstruction by magnetic resonance imaging in patients with acute myocardial infarction. Circulation. 1998;97(8):765–72.
Watanabe N, Isobe S, Okumura T, Mori H, Yamada T, Nishimura K, et al. Relationship between QRS score and microvascular obstruction after acute anterior myocardial infarction. J Cardiol. 2016;67(4):321–6.
Mayr A, Klug G, Schocke M, Trieb T, Mair J, Pedarnig K, et al. Late microvascular obstruction after acute myocardial infarction: relation with cardiac and inflammatory markers. Int J Cardiol. 2012;157(3):391–6.
Klug G, Mayr A, Mair J, Schocke M, Nocker M, Trieb T, et al. Role of biomarkers in assessment of early infarct size after successful p-PCI for STEMI. Clin Res Cardiol. 2011;100(6):501–10.
El-Menyar A, Zubaid M, AlMahmeed W, Sulaiman K, AlNabti A, Singh R, et al. Killip classification in patients with acute coronary syndrome: insight from a multicenter registry. Am J Emerg Med. 2012;30(1):97–103.
Friedrich MG, Kim HW, Kim RJ. T2-weighted imaging to assess post-infarct myocardium at risk. JACC Cardiovasc Imaging. 2011;4(9):1014–21.
Kim HW, Van Assche L, Jennings RB, Wince WB, Jensen CJ, Rehwald WG, et al. Relationship of T2-weighted MRI myocardial Hyperintensity and the ischemic area-at-risk. Circ Res. 2015;117(3):254–65.
Acknowledgements
Not applicable.
Funding
This study was supported by grants from the ‘Austrian Society of Cardiology’, the “Tiroler Wissenschaftsfonds” and by an intramural funding program of the Medical University Innsbruck for young scientists MUI-START, Project 2015-06-01.
The funding sources had no influence on the design of this study, its execution, analyses, interpretation of the data and scientific writing.
Author information
Authors and Affiliations
Contributions
CT was the primary author, defined the aims and the design of the study, interpreted the results and was the major contributor of writing the manuscript. MR, SJR and MH helped interpreting as well as analysing the data and proofread the manuscript. MS, AP, NH and IL provided help in data collection and proof reading. AM and GK provided their long-lasting knowledge in CMR imaging for interpreting and analysing CMR images. BM acted as the major project investigator and provided help in designing the study and proof reading. The manuscript was read and approved by all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study complies with the ethical guidelines of the 1975 Declaration of Helsinki and was approved by the local ethics committee of Medical University of Innsbruck. Written informed consent was obtained from all patients prior to inclusion into the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tiller, C., Reindl, M., Reinstadler, S.J. et al. Complete versus simplified Selvester QRS score for infarct severity assessment in ST-elevation myocardial infarction. BMC Cardiovasc Disord 19, 285 (2019). https://doi.org/10.1186/s12872-019-1230-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-019-1230-0