Abstract
Background
High ratio of the carbon dioxide veno-arterial difference to the oxygen arterial-venous difference (PvaCO2/CavO2) is associated with fluid bolus (FB) induced increase in oxygen consumption (VO2). This study investigated whether PvaCO2/CavO2 was associated with decreases in blood-lactate levels FB in critically ill patients with hyperlactatemia.
Methods
This prospective observational study examined adult patients in the intensive care unit (ICU) with lactate levels > 1.5 mmol/L who received FBs. Blood-lactate levels were measured before and after FB under unchanged metabolic, respiratory, and hemodynamic conditions. The primary outcome was blood-lactate levels after FB. Significant decreases in blood-lactate levels were considered as blood-lactate levels < 1.5 mmol/L or a decrease of more than 10% compared to baseline.
Results
The study enrolled 40 critically ill patients, and their median concentration of blood lactate was 2.6 [IQR:1.9 − 3.8] mmol/L. There were 27 (68%) patients with PvaCO2/CavO2 ≥ 1.4 mmHg/ml, and 10 of them had an increase in oxygen consumption (dVO2) ≥ 15% after FB, while 13 (32%) patients had PvaCO2/CavO2 < 1.4 mmHg/ml before FB, and none of them had dVO2 ≥ 15% after FB. FB increased the cardiac index in patients with high and low preinfusion PvaCO2/CavO2 (13.4% [IQR: 8.3 − 20.2] vs. 8.8% [IQR: 2.9 − 17.4], p = 0.34). Baseline PvaCO2/CavO2 was not found to be associated with a decrease in blood lactate after FB (OR: 0.88 [95% CI: 0.39 − 1.98], p = 0.76). A positive correlation was observed between changes in blood lactate and baseline PvaCO2/CavO2 (r = 0.35, p = 0.02).
Conclusions
In critically ill patients with hyperlactatemia, PvaCO2/CavO2 before FB cannot be used to predict decreases in blood-lactate levels after FB. Increased PvaCO2/CavO2 is associated with less decrease in blood-lactate levels.
Similar content being viewed by others
Introduction
Blood-lactate concentrations are frequently measured at the bedside in critically ill patients, and high lactate levels have been widely used as a marker of tissue hypoxia [1]. However, blood lactate is not frequently used as a trigger to administrate fluid bolus (FB) in this setting [2] unless very high lactate concentrations are observed. Circulating lactate levels are the product of the balance between lactate generation, metabolism, and clearance rate. As such, hyperlactatemia may not reflect only tissue hypoxia, but also the equilibration between production and utilization of lactate [3]. Therefore, giving FB based on only high lactate levels might lead to an inadequate or excessive fluid administration in critically ill patients [4, 5].
The ratio of the veno-arterial difference of carbon dioxide partial pressure to over the artero-venous difference in oxygen content (PvaCO2/CavO2) has been suggested as a marker of tissue hypoxia that can be easily measured at bedside [6]. An increased value represents an inequivalence between global CO2 production and oxygen consumption, which is typically found in anaerobic metabolism [6, 7]. Thus, FB administration in patients with high PvaCO2/CavO2 may have significant metabolic effects as the expected improvement in oxygen delivery can decrease anaerobic metabolism and lactate production.
Previous studies have demonstrated that high PvaCO2/CavO2 was associated with an increase in oxygen consumption (VO2) after FB [8, 9]. However, the association of baseline PvaCO2/CavO2 in significant lactate decreases after FB has not been established yet and its role in treating patients with hyperlactatemia is under investigation [10]. The goal of this study was to test the hypothesis that a high PvaCO2/CavO2 is associated with decreasing blood-lactate levels during FB and whether it has clinical utility to guide fluid treatment in this regard. To do so, we evaluated blood-lactate kinetics and preinfusion PvaCO2/CavO2 in critically ill patients with hyperlactatemia who received FB.
Methods
Design and setting
This is prospective observational study enrolled patients treated in the 33-bed Intensive Care Unit (ICU) of Brugmann Hospital in Brussels, Belgium. The patients received FB between January and June 2015. Approval was obtained from the local Ethics Committee (CE2014/122), and written informed consent was obtained by the patient’s next of kin accordingly. The decisions about the indication, type, amount, and speed of FB were made by the treating physician.
Inclusion and exclusion criteria
Critically ill adult patients (> 18 years of age) with blood-lactate levels > 1.5 mmol/L who received FBs in less than 50 min were considered eligible for the study [11]. The exclusion criteria were: 1) a lack of jugular or subclavian venous catheter and arterial catheter; 2) FB using Ringer’s lactate solutions, to avoid any increasing of blood lactate due to fluid administration; 3) other interventions within 30 min before FB or during FB (i.e., introduction or increase of inotrope dosage, ventilator mode changes, or the initiation of mechanical ventilation); 4) patients on extracorporeal membrane oxygenation (ECMO) support; 5) patients with diabetic ketoacidosis (blood glucose > 300 mg/dL, positive urine ketone test, pH < 7.35 in arterial blood gas analysis); 6) treatment with metformin within 48 h before FB; 7) clinical suspicion of epileptic crisis or physical effort or as a cause of hyperlactatemia; and 8) patients with diagnosis of metastatic malignancy or leukaemia or malaria.
Data and sample collections
Demographics, the type of fluids used for FB, concomitant treatments (mechanical ventilation, inotropic agents), and laboratory data were collected for each patient. The Acute Physiology and Chronic Health Evaluation (APACHE) II score upon admission was used to assess disease severity. Before and after FB, we measured the cardiac index (CI) using Doppler echocardiography and performed arterial and central venous blood gas analyses (which were sampled simultaneously), including haemoglobin, arterial and venous oxygen pressure (PaO2 and PvO2, respectively), and oxygen saturation (SaO2 and ScvO2).
The arterial and venous oxygen content (CaO2, CvO2), oxygen delivery (DO2), oxygen consumption (VO2), and the oxygen extraction ratio (OER) were computed using validated formulas [12]. Also, the venous-to-arterial carbon dioxide tension (PvaCO2) and the venous-to-arterial carbon dioxide tension/arterial-venous oxygen content difference ratio (PvaCO2/CavO2) were calculated. Each patient was assessed once.
Definitions and outcome
Sepsis and septic shock were defined according to Sepsis-3 definition [13]. Enhanced oxygen extraction was defined as OER > 40% and/or ScvO2 < 60%. A significant decrease in lactate concentrations was defined as: a) post-FB lactate < 1.5 mmol/L) or b) a decrease of more than 10% from baseline values [14]. High PvaCO2/CavO2 was defined as a value ≥ 1.4 [15]. A significant increase in VO2 was defined as an augmentation (dVO2) ≥ 15% from baseline [8]. The primary outcome was the predictive value of PvaCO2/CavO2 for significant lactate decrease after FB. Secondary outcomes included: a) the association of lactate and PvaCO2/CavO2 before and after FB and b) the association of changes in VO2 and blood lactate changes after FB.
Statistical analysis
Statistical analyses were done in R through the R-studio interface (www.r-project.org, R version 3.3.1). Descriptive statistics were computed for all study variables. A Kolmogorov–Smirnov test was used, and histograms and normal-quantile plots were examined to verify the normality of the distribution of continuous variables. Absolute changes (Δ = After FB value – Before FB value) and relative changes (d = [(After FB value – Before FB value)/ Before FB value] × 100) of different variables were evaluated. Discrete variables were expressed as counts (percentages) and continuous variables as the means ± SDs or medians with interquartile ranges (IQR).
A student’s t-test or Wilcoxon signed-rank test was performed as appropriate. Categorical variables were compared using Fisher’s exact test. Univariate logistic regression analysis was done to assess the association of PvaCO2/CavO2 with a significant decrease in blood-lactate levels after FB. Sensitivity analysis was also performed for a significant increase in dVO2 after FB. Odds ratios (OR) with 95% confidence intervals (CI) were computed. Spearman’s correlation and scatter diagrams were used to assess correlations between values. Statistical significance was defined using p < 0.05.
Results
Study population
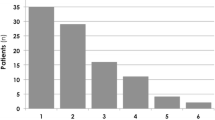
Out of a total of 80 patients who received FBs during the study period, 40 patients (age 71 ± 15 years) met the entry criteria and were included in the analysis (Figure S1). There were 25 patients (58%) who were admitted for medical reasons, and the majority of the patients (n = 24, 55%) had sepsis at the time of FB. Colloids were used in 22 patients (54%) (Geloplasma®, Fresenius-Kabi AG, Bad Homburg, Germany), and crystalloids were used in 18 (46%) (Plasma-Lyte A, Baxter Healthcare, Deerfield, IL). The elapsed time between the baseline sample and the sample after the FB was 33 (27 − 42) min; the main reason for FB was persistent elevated levels of blood lactate (Table S1).
Before FB, high PvaCO2/CavO2 ≥ 1.4 was observed in 27 patients (68%). No significant differences were found between patients with high and low PvaCO2/CavO2 at baseline (Table 1) except for a higher incidence of diabetes and pulmonary infection in patients with low PvaCO2/CavO2. No significant differences in changes in systemic haemodynamics were observed between the two groups (Table 2). FB increased central venous pressure and cardiac output in both group of patients.
Association of PvaCO2/CavO2 with significant blood-lactate decrease after FB
There were 10 patients (25%) who had a significant decrease in blood-lactate levels after FB. All exept one of them had a PvaCO2/CavO2 < 1 mmHg/mL (1.34 (1.01 − 1.71) mmHg/mL) (Figure S2). Logistic regression analyses did not demonstrate any association between the baseline PvaCO2/CavO2 as a continuous value and significant decreases in lactate levels after FB (OR: 0.88 [95% CI: 0.39 − 1.98], p = 0.76). A PvaCO2/CavO2 ≥ 1.4 was also not associated with significant decreases of blood lactate after FB (OR: 0.36 [95% CI: 0.08 − 1.59], p = 0.18). There was no evidence of moderation of the associations of PvaCO2/CavO2 with decreases of blood lactate after FB by the changes of VO2 ≥ 15% (no interaction; p = 0.31). Preinfusion PvaCO2/CavO2 was weakly and positively correlated with blood lactate changes during FB (r = 0.31, p = 0.04) (Fig. 1, Figure S2).
Changes in blood-lactate levels (Δ Lactate) during fluid bolus according to the baseline ratio of carbon dioxide veno-arterial difference to arterial-venous oxygen difference (PvaCO2/CavO2). Blue points: patients with increase in oxygen consumption (VO2) ≥ 15%, black points: patients with change in oxygen consumption < 15%. Vertical dotted line corresponds to PvaCO2/CavO2 of 1.4 mmHg/mL
Association of blood-lactate levels and PvaCO2/CavO2 before and after FB
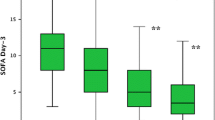
No significant correlation was observed between blood-lactate levels before and after FB. A statistically significant but weak negative correlation was observed between the changes in blood lactate and PvaCO2/CavO2 (r = -0.41, p = 0.01) (Fig. 2, Figures S3 & S4).
Association of oxygen consumption and blood lactate changes during FB
There were 10 patients (25%) who had a significant increase in VO2 after FB, and none of them had low PvaCO2/CavO2 before FB. Among patients with elevated baseline PvaCO2/CavO2, no statistically significant differences were observed in baseline values of PvaCO2 (8.7 (7.7 − 11.2) mmHg vs. 8.9 (7.2 − 10.1) mmHg, p = 0.96) or in baseline values of ScvO2 (70 (61 − 78) % vs. 69 (61 − 74) %, p = 0.76) between those with or without an increase in VO2. Changes in VO2 were weakly and positively correlated with lactate changes (r = 0.36, p = 0.02) (Fig. 3, Figure S5).
Discussion
The results of this study can be summarized as follows: 1) in critically ill patients with hyperlactatemia, elevated PvaCO2/CavO2 is not associated with decreases in blood-lactate levels after FB and cannot be used to predict them, 2) increases in oxygen consumption observed only in patients with elevated baseline PvaCO2/CavO2 were not associated with blood lactate decreases after FB and 3) in patients with hyperlactatemia, blood-lactate levels and changes during FB were not corelated with PvaCO2/CavO2 values and changes.
Previous studies have suggested using the PvaCO2/CavO2 ratio measured after the end of resuscitation for predicting failure for decreasing blood-lactate levels in patients with hyperlactatemia [15,16,17]. Similar to these studies, we found that decreasing blood-lactate levels are less likely in patients with elevated PvaCO2/CavO2 before FB. Conversely, and similar to another study [15], patients with low baseline PvaCO2/CavO2 had a higher likelihood for decreasing blood lactate levels. Thus, the results of our study extend the knowledge about the FB effects on blood lactate in critically ill patients according to baseline PvaCO2/CavO2, suggesting that FB has limited effects on decreasing lactate levels in patients with elevated baseline PvaCO2/CavO2. Additionally, the reduction in blood lactate levels observed in patients with normal baseline PvaCO2/CavO2 values may not be associated with an improvement of aerobic metabolism after FB.
Herein, PvaCO2/CavO2 was used as an alternative of respiratory quotient. The failure of high PvaCO2/CavO2 to predict decreases in blood lactate levels after FB could be due to the unreliable correlation of this ratio with the occurrence of anaerobic metabolism in this mixed population of critically ill patients [18]. Similar to previous studies [8, 9] several patients with hyperlactatemia and high PvaCO2/CavO2 increased VO2 after FB, which implies oxygen delivery/consumption dependence. However, high oxygen extraction state was observed only in few patients with elevated PvaCO2/CavO2, which may contradict this hypothesis.Therefore, we conclude that in our cohort of non-selected critically ill patients with hyperlactatemia, elevated PvaCO2/CavO2 may reflect not only anaerobic metabolism as a result of tissue hypoxia (i.e. hypoperfusion), but also as a result of tissue dysoxia (i.e. impairment in oxygen utilization) [19].
Significant decreases in blood lactate after FB were observed in patients with PvaCO2/CavO2 < 1.4 mmHg/mL, but not in the patients with PvaCO2/CavO2 < 1 mmHg/mL. PvaCO2/CavO2 ≥ 1.4 mmHg/mL was defined abnormal based on the previous studies that have demonstrated that this cut-off can predict persistent hyperlactatemia in critically ill patients [6, 15]. Incidentally, other authors have suggested higher cut-off values to predict increases in VO2 after FB [8, 9, 20]. However, in another study, a cut-off of > 1 mmHg/mL was found to adequately predict mortality [17]. Hence, our results suggest that the anaerobic threshold of critically ill patients with hyperlactatemia may vary across the patients [21]. Nevertheless, a value of PvaCO2/CavO2 < 1 mmHg/mL may be used to exclude anaerobic metabolism and decreasing blood lactate levels after FB.
Increases in oxygen consumption after FB were not associated with a decrease in blood-lactate levels. Notably, we found that the patients who had an increase oxygen consumption after FB were less likely to present a significant decrease in blood-lactate levels. Different factors can explain this phenomenon. Calculation of VO2 based on the reverse Fick principle may not be accurate [22, 23]. Inadequate hemodynamic resuscitation can be an additional explanation, even though a sufficient dose of fluid at high rate was administrated [24]. Furthermore, increased tissue perfusion during FB may cause a paradoxical elevation in blood lactate levels due to ‘washout’ phenomenon [25,26,27,28] or accelerated aerobic glycolysis [29, 30]. Of note, a weak correlation between VO2 and blood lactate changes was observed. Thus, based on our results, high PvaCO2/CavO2 before FB is associated with VO2 dependency on DO2, similar to previous studies [8, 9], but also with failure of FB to decrease blood lactate. In these patients, whether no change or even increase in blood lactate levels indicates FB failure to improve peripheral perfusion should be further evaluated in future studies.
Not surprisingly, the majority of the patients with hyperlactatemia had an elevated PvaCO2/CavO2 since either of these variables increases due to anaerobic metabolism. Nevertheless, there was no correlation between PvaCO2/CavO2 and blood-lactate levels. Hence, our results suggest that PvaCO2/CavO2 can be used as a complementary marker for the evaluation of patients with hyperlactatemia and the effects of FB. For instance, we observed a negative correlation of changes in blood lactate and PvaCO2/CavO2 during FB. A plausible explanation for this phenomenon could be that decreases in blood lactate illustrate an improvement in tissue oxygenation, and PvaCO2/CavO2 illustrates oxygen debt repayment after perfusion improvement [31, 32].
The strength of this study was that we evaluated the predictive value of PvaCO2/CavO2 in a non-selected critically ill population with mild hyperlactatemia treated with FB. Patients in this cohort presented a high range of PvaCO2/CavO2, and a significant number of patients had low PvaCO2/CavO2. We evaluated changes in blood lactate close to the time of the FB in stable conditions, and non-major variation in metabolism was expected.
Nevertheless, this study has several limitations. First, no formal sample power calculation was done and not predictive test were performed. However, the results are in the opposite direction of our hypothesis, and the possibility of finding different results with a higher sample size is low. Additionaly, based on our findings we conclude that PvaCO2/CavO2 cannot have clinical relevant predictive value for decreasing blood lactate levels after FB. Second, therapeutic interventions that can affect lactate levels before and after FB were not standardized. However, all the patients were treated under standard local therapeutic strategies. Third, only central venous and not mixed venous-to-arterial carbon dioxide tension differences were evaluated. Fourth, other parameters that can affect the amount PvaCO2 such as temperature, metabolic acidosis, and Haldane effect were not assessed in this study. Fifth, we did not evaluate that within-subject variability might significantly influence our results, as relatively low values of baseline blood lactate were observed. Sixth, possible liver dysfunction effects on lactate metabolism was not evaluated.
Conclusions
Elevated PvaCO2/CavO2 are not associated with FB induced blood lactate decreases. In this small cohort of critically ill patients with hyperlactatemia, high preinfusion PvaCO2/CavO2 was associated with less decrease in blood-lactate levels after FB.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- PvaCO2 :
-
Carbon dioxide veno-arterial difference
- CavO2 :
-
Oxygen arterial-venous difference
- VO2 :
-
Oxygen consumption
- FB:
-
Fluid bolus
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- DO2 :
-
Oxygen delivery
- OER:
-
Oxygen extraction ratio
References
Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013;369(18):1726–34. https://doi.org/10.1056/NEJMra1208943.
Cecconi M, Hofer C, Teboul JL, et al. Fluid challenges in intensive care: the FENICE study: a global inception cohort study [published correction appears in intensive care med. Intensive Care Med. 2015;41(9):1737–8. https://doi.org/10.1007/s00134-015-3850-x. 2015;41(9):1529-1537.
Levy B. Lactate and shock state: The metabolic view. Curr Opin Crit Care. 2006;12(4):315–21.
Jansen TC, van Bommel J, Schoonderbeek FJ, et al. Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010;182(6):752–61. https://doi.org/10.1164/rccm.200912-1918OC.
Hernández G, Ospina-Tascón GA, Damiani LP, et al. Effect of a resuscitation strategy targeting peripheral perfusion status vs serum lactate levels on 28-day mortality among patients with septic shock: the ANDROMEDA-SHOCK randomized clinical trial. JAMA. 2019;321(7):654–64. https://doi.org/10.1001/jama.2019.0071.
Mekontso-Dessap A, Castelain V, Anguel N, et al. Combination of venoarterial PCO2 difference with arteriovenous O2 content difference to detect anaerobic metabolism in patients. Intensive Care Med. 2002;28(3):272–7. https://doi.org/10.1007/s00134-002-1215-8.
Wasserman K, Whipp BJ, Koyl SN, Beaver WL. Anaerobic threshold and respiratory gas exchange during exercise. J Appl Physiol. 1973;35(2):236–43. https://doi.org/10.1152/jappl.1973.35.2.236.
Monnet X, Julien F, Ait-Hamou N, et al. Lactate and venoarterial carbon dioxide difference/arterial-venous oxygen difference ratio, but not central venous oxygen saturation, predict increase in oxygen consumption in fluid responders. Crit Care Med. 2013;41(6):1412–20. https://doi.org/10.1097/CCM.0b013e318275cece.
Mallat J, Lemyze M, Meddour M, et al. Ratios of central venous-to-arterial carbon dioxide content or tension to arteriovenous oxygen content are better markers of global anaerobic metabolism than lactate in septic shock patients. Ann Intensive Care. 2016;6(1):10. https://doi.org/10.1186/s13613-016-0110-3.
Caruso V, Besch G, Nguyen M, et al. Treatment of hyperlactatemia in acute circulatory failure based on CO2-O2-derived indices: study protocol for a prospective, multicentric, single, blind, randomized superiority study (The LACTEL Study). Front Cardiovasc Med. 2022;9:898406. https://doi.org/10.3389/fcvm.2022.898406.
Vellinga NAR, Boerma EC, Koopmans M, et al. Mildly elevated lactate levels are associated with microcirculatory flow abnormalities and increased mortality: a microSOAP post hoc analysis. Crit Care. 2017;21(1):255. https://doi.org/10.1186/s13054-017-1842-7.
Scheeren TWL, Wicke JN, Teboul JL. Understanding the carbon dioxide gaps. Curr Opin Crit Care. 2018;24(3):181–9. https://doi.org/10.1097/MCC.0000000000000493.
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–10. https://doi.org/10.1001/jama.2016.0287.
Zhou X, Liu D, Su L, et al. Use of stepwise lactate kinetics-oriented hemodynamic therapy could improve the clinical outcomes of patients with sepsis-associated hyperlactatemia. Crit Care. 2017;21(1):33. https://doi.org/10.1186/s13054-017-1617-1.
Mesquida J, Saludes P, Gruartmoner G, et al. Central venous-to-arterial carbon dioxide difference combined with arterial-to-venous oxygen content difference is associated with lactate evolution in the hemodynamic resuscitation process in early septic shock. Crit Care. 2015;19(1):126. https://doi.org/10.1186/s13054-015-0858-0.
He HW, Liu DW, Long Y, Wang XT. High central venous-to-arterial CO2 difference/arterial-central venous O2 difference ratio is associated with poor lactate clearance in septic patients after resuscitation. J Crit Care. 2016;31(1):76–81. https://doi.org/10.1016/j.jcrc.2015.10.017.
Ospina-Tascón GA, Umaña M, Bermúdez W, et al. Combination of arterial lactate levels and venous-arterial CO2 to arterial-venous O 2 content difference ratio as markers of resuscitation in patients with septic shock. Intensive Care Med. 2015;41(5):796–805. https://doi.org/10.1007/s00134-015-3720-6.
Abou-Arab O, Braik R, Huette P, Bouhemad B, Lorne E, Guinot PG. The ratios of central venous to arterial carbon dioxide content and tension to arteriovenous oxygen content are not associated with overall anaerobic metabolism in postoperative cardiac surgery patients. PLoS One. 2018;13(10):e0205950. https://doi.org/10.1371/journal.pone.0205950.
Saludes P, Proença L, Gruartmoner G, et al. In response to: “understanding elevated Pv-aCO2 gap and Pv-aCO2/Ca-vO2 ratio in venous hyperoxia condition.” J Clin Monit Comput. 2017;31(6):1325–7. https://doi.org/10.1007/s10877-017-0006-2.
Du W, Long Y, Wang XT, Liu DW. The use of the ratio between the veno-arterial carbon dioxide difference and the arterial-venous oxygen difference to guide resuscitation in cardiac surgery patients with hyperlactatemia and normal central venous oxygen saturation. Chin Med J (Engl). 2015;128(10):1306–13. https://doi.org/10.4103/0366-6999.156770.
Older P. Anaerobic threshold, is it a magic number to determine fitness for surgery? Perioper Med (Lond). 2013;2(1):2. https://doi.org/10.1186/2047-0525-2-2. Published 21 Feb 2013.
Cheong KF, Lee TL. Oxygen consumption–a comparison between calculation by Fick’s principle and measurement by indirect calorimetry. Med J Malaysia. 1997;52(1):70–5.
Inadomi C, Terao Y, Yamashita K, Fukusaki M, Takada M, Sumikawa K. Comparison of oxygen consumption calculated by Fick’s principle (using a central venous catheter) and measured by indirect calorimetry. J Anesth. 2008;22(2):163–6. https://doi.org/10.1007/s00540-007-0588-9.
Vincent JL, Cecconi M, De Backer D. The fluid challenge. Crit Care. 2020;24(1):703. https://doi.org/10.1186/s13054-020-03443-y.
Leavy JA, Weil MH, Rackow EC. “Lactate washout” following circulatory arrest. JAMA. 1988;260(5):662–4.
Falk JL, Rackow EC, Leavy J, Astiz ME, Weil MH. Delayed lactate clearance in patients surviving circulatory shock. Acute Care. 1985;11(3–4):212–5.
Yang M. Muscle lactate concentration during experimental hemorrhagic shock. J Anesth. 1998;12(2):76–80.
Scott S, Antonaglia V, Guiotto G, Paladino F, Schiraldi F. Two-hour lactate clearance predicts negative outcome in patients with cardiorespiratory insufficiency. Crit Care Res Pract. 2010;2010:1–6.
Wutrich Y, Barraud D, Conrad M, Cravoisy-Popovic A, Nace L, Bollaert PE, et al. Early increase in arterial lactate concentration under epinephrine infusion is associated with a better prognosis during shock. Shock. 2010;34(1):4–9.
Garcia-Alvarez M, Marik P, Bellomo R. Sepsis-associated hyperlactatemia. Crit Care. 2014;18(5):1–11.
Margaria R, Edwards HT, Dill DB. The possible mechanisms of contracting and paying the oxygen debt and the rôle of lactic acid in muscular contraction. Am J Physiol Content. 1933;106(3):689–715. https://doi.org/10.1152/ajplegacy.1933.106.3.689.
Ganushchak YM, Kurniawati ER, van der Horst ICC, et al. Patterns of oxygen debt repayment in cardiogenic shock patients sustained with extracorporeal life support: a retrospective study. J Crit Care. 2022;71:154044. https://doi.org/10.1016/j.jcrc.2022.154044.
Funding
No fundings received for this study.
Author information
Authors and Affiliations
Contributions
KK, CP, TN and FST: study conception and design, data analysis and interpretation, drafted the manuscript, SS: data analysis and interpretation, drafted the manuscript, and approved the submitted version of the manuscript, DV, RA, JD: revised the manuscript for critical content and approved the submitted version of the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is an observational study approved by the ethic committee of CHU-Brugmann (CE2014/122). Informed consents were obtained from the patients or family members. All methods were performed all methods were performed in accordance with the relevant guidelines and regulations (Declaration of Helsinki).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Figure S1. Flow chart of patients selection. Table S1. Principal reasons for fluid bolus. Figure S2. Prevalence of the patients who had significant decrease in blood lactate levels during fluid bolus (FB) according to pre-infusion arterial-venous oxygen difference ratio (PvaCO2/CavO2). Dotted line: trendline (regression analysis). Figure S3. Changes in blood lactate levels ( Δ Lactate) during fluid bolus according to the baseline carbon dioxide veno-arterial difference to arterial-venous oxygen difference ratio (PvaCO2/CavO2), in patient without (Pannel A) or with (Pannel B) enhanced oxygen extraction. Figure S4. Correlation between blood lactate levels and arterio-venous oxygen difference ratio(PvaCO2/ CavO2) before (panel A) and after (panel B) fluid bolus (FB) and correlation of the changes (panel C) during FB in patients without enhanced oxygen extraction. Figure S5. Correlation between blood lactate levels and arterio-venous oxygen differenceratio (PvaCO2/ CavO2) before (panel A) and after (panel B) fluid bolus (FB) and correlation of the changes (panel C) during FB in patients with enhanced oxygenextraction. Figure S6. Correlation between blood lactate levels changes and oxygen consumption changes during fluid bolus, in patient without (Pannel A) or with (Pannel B) enhanced oxygen extraction.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kaefer, K., Pierrakos, C., Nguyen, T. et al. Ratio of carbon dioxide veno-arterial difference to oxygen arterial-venous difference is not associated with lactate decrease after fluid bolus in critically ill patients with hyperlactatemia: results from a prospective observational study. BMC Anesthesiol 23, 37 (2023). https://doi.org/10.1186/s12871-023-01993-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-023-01993-6