Abstract
Gestational diabetes mellitus (GDM) is characterized by insulin resistance and low-grade inflammation, and most studies have demonstrated gut dysbiosis in GDM pregnancies. Overall, they were manifested as a reduction in microbiome diversity and richness, depleted short chain fatty acid (SCFA)-producing genera and a dominant of Gram-negative pathogens releasing lipopolysaccharide (LPS). The SCFAs functioned as energy substance or signaling molecules to interact with host locally and beyond the gut. LPS contributed to pathophysiology of diseases through activating Toll-like receptor 4 (TLR4) and involved in inflammatory responses. The gut microbiome dysbiosis was not only closely related with GDM, it was also vital to fetal health through vertical transmission. In this review, we summarized gut microbiota signature in GDM pregnancies of each trimester, and presented a brief introduction of microbiome derived SCFAs. We then discussed mechanisms of microbiome-host interactions in the physiopathology of GDM and associated metabolic disorders. Finally, we compared offspring microbiota composition from GDM with that from normal pregnancies, and described the possible mechanism.
Similar content being viewed by others
Introduction
During normal pregnancy, women undergo diverse physiological adaptations including increased insulin resistance (IR) [1]. In susceptible populations who are incapable of producing enough insulin, GDM occurred [2]. Besides the short and long-term adverse effects such as fetal macrosomia and type 2 diabetes (T2DM), children born to GDM mothers are at increased risk for obesity and metabolic syndrome later in life [3]. Gut microbiome is involved in body weight control, energy homeostasis and absorption of no-digestible fiber. Previous studies showed particularities of microbiome’s action during normal and GDM pregnancies [4, 5]. The common findings were reduction in short chain fatty acid (SCFA)-producing genera and dominant of Gram-negative pathogens releasing lipopolysaccharide (LPS) [6, 7]. SCFAs are closely related with maternal-fetal glycolipid parameters [8]. They functioned as energy sources for colonocytes, owned potential capacity to modulate immune-metabolic responses or gut barrier integrity, and regulated insulin secretion through promoting GLP-1 and PYY secretion [9]. They were also absorbed into the circulation and engaged specific receptors to activate downstream signaling pathways that ultimately impacted cellular processes. LPS was a bacterial endotoxin which destroyed gut mucosal barrier by activating TLR4 or decreasing SCFAs, and involved in metabolic inflammation [10]. The microbiome could be transmitted to fetus and determined early microbial composition [11]. In this review, we summarized current evidence regarding gut microbiota signature in GDM pregnancies. We then presented a brief introduction of SCFAs and discussed mechanisms of microbiome-host interactions in the physiopathology of GDM and associated metabolic disorders. Finally, we compared neonatal microbiota composition between GDM and normal pregnancies, and described the influential pathways.
Gut microbiota profile in pregnancies complicated by GDM
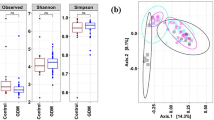
The microbiome profiles of GDM were summarized in Table 1; Fig. 1 during each trimester [4, 6, 7, 12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38]. Totally, GDM was mostly linked to an elevated Firmicutes/Bacteroidetes (F/B) ratio, decreased richness and diversity which was associated with enhanced capacity to harvest energy and akin to that found in obesity [12,13,14,15]. Microbiome in early pregnancy was considered as diagnostic marker for GDM [16,17,18]. The genera Eisenbergiella and Tyzzerella 4 were upregulated and positively correlated with fasting plasma glucose (FPG) among pregnancies diagnosed with GDM subsequently [19]. Normoglycemic women were abundant in family Prevotellaceae, order Fusobacteriales, and genus Subdoligranulum, which was negatively correlated with LDL levels [20]. The differences were negligible in another randomized controlled trial (RCT), which was due to different technology platform, demographic characteristics and diagnostic criteria [13]. It is debated that intestinal microbiota is a cause or consequence of GDM, and fecal microbiota transfer (FMT) experiments are needed. GDM-recipient mice obtained differential microbial communities demonstrated as reduced P.copri and increased IL-6 level [21].The GDM prediction model containing clinical information, microbial and inflammatory markers obtained high accuracy [21]. Although gut microbiome dysbiosis could be the first response to GDM onset, the phenotype transfer may also be caused by metabolites and eukaryotic microorganisms. It is meaningful to further unravel the underlying mechanisms in terms of these fecal derived material [21].
Gut microbiota profile in pregnancies complicated by GDM during each trimester. In GDM pregnancies during each trimester, the microbiota with decreased abundance were shown in green, and the opposite were shown in red. The distribution of some microbiome has not been consistently concluded and were shown in orange
Most studies proposed a specific microbiome composition at time of GDM diagnosis. The genera Bifidobacterium, Prevotella, and Ruminococcaceae UCG014 were significantly decreased, while Parabacteroides and Blautia were increased in GDM [22,23,24]. Most of the reduced flora were SCFA-producing genera and positively contributed to dopaminergic synapse, betalain biosynthesis, and isoquinoline alkaloid biosynthesis. They were also negatively correlated with glucose level, visceral fat area and inflammatory cytokines in single and co-occurrence network analysis, reflecting the microbe interactions within an ecosystem [25]. In pregnant women with impaired FPG, valerate and 2-hydroxybutyrate were positively related with archaeon Methanobrevibacter and genus Phascolarctobacterium, and became prognostic markers for diabetes related complications [20]. Metagenome linkage groups (MLGs) were clustered from co-abundance genes physically linked rather than independently distributed by metagenomics analysis. GDM was enriched with MLGs of Enterobacteriaceae and positively correlated with glucose level [26]. Transferring fecal microbiota from GDM to germ-free (GM) mice induced hyperglycemia and decreased SCFA-producing Akkermansia [39]. It supported the multiple parallel hits that gut microbiome dysbiosis primed SCFA imbalance and metabolic inflammation, and contributed to GDM development [25]. The efficiency of glucose control level contributed to the inconsistent findings demonstrated as upregulated [12, 23] or downregulated [22, 24] genus Bacteroides in GDM. The microbiome composition of women with successful glycemic control was more similar with those from normal pregnancies, and harbored a unique microbiome pattern abundance of genera Roseburia, Clostridium, and Bifidobacterium [27, 28]. They were negatively correlated with blood glucose level and help correct GDM conditions.
GDM status was the main factor that affected microbiome changes at late pregnancy [29]. Compared with normal pregnancies, time-dependent alterations of F/B ratio and 𝛼-diversity were not observed in GDM [18]. Genera Bifidobacterium and Ruminococcaceae were still decreased and lasted to postpartum [7, 14]. There are some cofactors that cannot be ignored given that previous upregulated Blautia and decreased Eubacterium were found to be inversed [30]. A composite microbial risk score (CMRS) was calculated based on ten GDM-related species. Its association with glycemic traits was significantly modified by habitual intake of fiber-rich plant foods [18]. In GDM with unsuccessful diet control, the genera Eubacteria and Enterobacteriaceae were significantly lower, and F/B ratio was higher before delivery [15]. GDM pregnancies adherent to nutritional recommendations demonstrated obvious decrease in Bacteroides and better metabolic-inflammatory responses [36]. Other cofactors such as pre-pregnancy BMI (p-BMI) affected microbiome profiles through interacting with diet and influenced GDM status [37]. Negligible differences were found among obese pregnancies suffering from GDM or not, and the microbiota was more stable and limited the capacity to respond to the diet [38]. Akkermansia enrichment only appeared in non-obese GDM after caloric control [38]. Additional 5 out of 17 differential abundance were found in GDM group after adjusting for p-BMI [14]. The sustained and heterogeneity of IR influenced microbiota diversity through effects on metabolic profiles. It showed that higher IR level was associated with lower microbial diversity adjusting for BMI or not [40]. Glucose level and gestational weight gain (GWG) were also essential, manifested as dominant WAL 1855D and Bacteroidetes by hierarchical clustering in excessive GWG group [41,42,43]. Hence, it is conducive to take these cofactors into account for better understanding changes of microbiota composition suffering from GDM.
To date, previous studies reported a unique microbiome pattern in GDM. Most studies examined at single time adopting 16 S rRNA sequencing without adjusting for confounding factors, and thus there are still controversies concerning associations between gut microbiome and GDM. Although GDM status was main in affecting microbiome changes, there are several factors that can influence the studies on gut microbiota of women with GDM. The physiological factors include different diagnostic criteria and demographic characteristics such as gestational age, diet habit, glucose control level, antibiotic use, p-BMI, GWG and IR level as mentioned above. The experimental factors mainly include sampling and DNA extraction method, preservation condition, and sequencing platform. After controlling the potential influencing factors, it could be more objective to reflect the relationships between microbiome characteristics and GDM development. Dynamic changes were also needed. For example, the temporal increase of microbiome-derived propionate from T1 to T2 was greater in control group [18], indicating a strong competence against glucose intolerance, although there were no significant differences at each trimester. The introduction of new methods (such as MLGs, CMRS et al.) and combination analysis (such as metabolomics) are more helpful in understanding correlations between the flora and environment.
The possible implications of microbiome derived SCFAs in pregnancy and GDM
SCFAs are synthesized from gut microbiota through fermentation of non-digestible fibers, proteins and glycoproteins. Acetate, propionate and butyrate constituted > 95% of SCFA contents, and the proportion of each is appropriately 60:20:20. The bacteria responsible for acetate production is widely distributed, whereas the production pathways for propionate and butyrate appear highly conserved and substrate specific [44]. Propionate is produced through succinate, acrylate or propanediol pathway from Bacterioidetes and some Firmicutes (Veillonlla, Megasphera et al.) [45]. Specific families belonging to Clostridiales produced butyrate through butyryl-CoA, phosphotransbutyrykase and butyrate pathways [45, 46].
The roles of SCFA have been identified during normal pregnancy, GDM, obesity and multiple sclerosis. They were closely related with metabolic parameters and provide evidence for intervention potential. During normal pregnancy, circulating propionate was negatively associated with leptin, infant length and body weight [8]. Butyrate in human milk was inversely associated with infant weight and BMI at 3 and 12 months, offering beneficial effects in weight gain and adiposity [47]. Caesarean section (CS)-delivered infants uniquely produced excess butyrate through enriched bacteria, and provided novel insights between delivery mode and infant health [48]. Acetic, propionic and butyric acid were all positively correlated with total cholesterol (TCHO), high density lipoprotein (HDL) and triglycerides (TG). HDL was only positively related with propionate in overweight/obese pregnancies [49]. As for anthropometric parameters and carbohydrate metabolism, the three dominant SCFAs were positively related with p-BMI, HbA1c contents, glucose value at three OGTT timepoints, and inversely related with body weight gain and insulin level [50]. GDM pregnancies are more capable of oxidizing sugars than lipids and characterized by IR and low-grade inflammation. In GDM, propionate was positively correlated with insulin in T2 and maintained until T3 [51]. The butyrate was negatively correlated with WBC counts, neutrophil counts, p-BMI, GWG per week before GDM diagnosis, and ponderal index, but positively correlated with TCHO and LDL levels in all pregnancies [51]. Another study found no relationships between main SCFAs and clinical parameters in GDM [52]. This could be explained in terms of their roles as energetic substrates or signaling molecules, and will be discussed below.
These observations were largely relied on measurements of stool or circulating SCFAs. However, it is still unclear whether the stool SCFA output was suitable to represent luminal production. Circulating SCFA contents were more representative since approximately 95% of colonic SCFAs were absorbed into blood and connected with metabolic health [53].
Mechanisms of microbiome-host interactions in GDM and metabolic disorders through SCFAs
SCFAs exerted metabolic effects as energy sources in local and peripheral tissues
SCFAs are important mediators between gut microbiome and host. Butyrate constituted 60–70% energy source for epithelial cells through β-oxidation. It promoted intestinal epithelial cell growth and enhanced gut barrier integrity, thus impeded bacteria from gut lumen for entering the circulation and avoided GDM onset [54]. Butyrate and acetate were direct substrates for cholesterol and fatty acids synthesis, and induced decrease in lipolysis and improved IR in liver and adipose tissue [55]. They also reduced lipid accumulation in an AMPK-dependent manner. Butyrate was converted to butyryl-CoA and further increased CPT1A activity, accelerated fatty acid oxidation (FAO) and promoted inducible regulatory T cell differentiation for maintenance of immune-metabolic homeostasis [56]. Acetate also exerted anti-lipolytic effect by reducing free fatty acid flux to the liver and attenuated fatty liver induced deterioration in glucose intolerance [57]. The propionate was precursor for glucose synthesis in liver. The intestinal gluconeogenesis promoted glucose release in portal vein, which resulted in decreased hepatic glucose production and increased energy expenditure through a brain-related mechanism [58]. The beneficial effects of diet enriched in propionate and butyrate were abolished in mice deficient in intestinal gluconeogenesis. Daily propionate supplementation was associated with decreased 2 h post-prandial glucose level due to decreased digestion of bread-derived starch. It was speculated that SCFAs entered an appropriate point of the Krebs cycle and mitigated the need for glucose as the sole energy substrate [59]. A high-fiber diet significantly increased key enzymes production of acetate (formate-tetrahydrofolate ligase) and butyrate (butyryl-coenzyme A) in T2DM, and stimulated GLP-1 secretion [60]. More evidence is needed on the role of butyrate alone or combined with propionate in energy regulation. There were few studies on SCFA as energy sources in GDM. Considering the characteristics of metabolic disorders, it is possible that similar mechanisms are preserved in GDM pregnancies when imbalance between energy storage and release occurred.
SCFAs have biphasic effects on energy control due to different types and concentrations. In humans, there is a strong biological gradient from production site to downstream tissues. In the proximal part of colon with increased availability of carbohydrates and water, the concentration is nearly 70-140mM, and decreased to 20-70mM in the distal part [61]. The output of splanchnic propionate or butyrate reached millimolar concentrations given that the hepatic SCFA utilization balanced its production under physiological status [62]. In the blood, the levels are ranged from 100–200µM for acetate, and 1–20µM for propionate and butyrate [63]. The overflow of SCFAs caused adverse effects due to lipogenic effect and energy accumulation. In TLR5-deficient mice, the overgrowth microbiome was accompanied by elevated SCFA levels, leading to increased hepatic de novo lipogenesis and metabolic impairment [64]. Totally, it is important to understand their biological effects to achieve clinical translation.
The potential roles of SCFA as signaling molecules through GPCRs and/or HDACs
GPCRs
SCFAs acted locally or systemically as signaling molecules through coupling with G-protein coupled receptors (GPCRs) or histone deacetylases (HDACs) (Fig. 2). GPCR41/43 were most important and ubiquitously expressed in intestinal epithelial cells (IEC), liver, and gestational tissues [65]. Previous data suggested that SCFAs promoted GLP-1 and PYY release in enteric L cells through GPCR41/43 directly. Mice lacking them exhibited glucose tolerance impairment [66]. GPCR43 regulated innate lymphoid cell proliferation and IL-22 expression via Akt-Stat3 axis, and afforded protection from intestinal inflammation [67]. Butyrate also promoted IL-22 production through aryl hydrocarbon receptor (AHR) and HIF-1α in GPCR41/HDAC dependent manner [68]. The antimicrobial peptides (AMPs) are important components produced by IEC in maintaining immune homeostasis. SCFA supplement induced RegIIIγ and β-defensins, and avoided IgA responses in wild type but not in GPCR43−/− mice by activating mTOR and Stat3 [69, 70].
The direct or indirect roles of microbiome on GDM and metabolic disorder development. In metabolic disorders, the SCFA functioned as energy sources (blue) or signaling molecules through GPCRs and/or HDACs (black) in local intestinal tract and periapical tissues. The gut microbiome influenced placental structure and functions through direct translocation or SCFAs, which established gut-placenta axis. The LPS overproduction is another characteristic of gut microbiota dysbiosis (pink). LPS alone or in combination with SCFA reduction involved in the occurrence and development of GDM
The impacts of SCFAs go beyond local cells. In white adipose tissue (WAT) of DHA/EPA-treated db/db mice, the GPCR41/43 and beigeing program markers (PRDM16, PPARγ) were upregulated, accompanied by elevated propionate, butyrate, Bifidobacterium and Lactobacillus, and improved glucose status [71]. It is supplied that DHA/EPA enhanced SCFA generation and WAT beigeing through GPCRs, linked gut to adipose and established the gut-organ axis. High-fiber diet was less likely to develop diabetic nephropathy with improved microbiome structure and elevated SCFA concentrations. The protective effects were disappeared in mice lacking genes encoding GPCR43/109A [72]. GPCRs functioned by binding to different subtypes. In human renal cortical epithelial cells, propionate elicited inhibitory effects by phosphorylation of p38MAPK and JNK through Gβγ (i/o) subtype [73]. However, GPCR43 contributed to inflammasome activation and played pathogenic roles in macrophages [74]. Therefore, GPCR43 exerted dual effects depending on cell types and locations in peripheral tissues. For normal labor, the elevated receptors are essential through dampening down pro-inflammatory responses [75]. GPCR43−/− pregnant mice developed fasting hyperglycemia, diminished β-cells expansion and decreased circulating propionate, explaining microbiome contributions on gestational glucose homeostasis [76]. In high-fat diet (HFD) rats before and during gestation, the contents of propionate, GPCR43 and placental labyrinth zone thickness were significantly decreased which destroyed nutrient provision and heightened inflammation through propionate-GPCR43 axis [77]. However, 5mM butyrate and 10mM propionate incubating for 1 h significantly suppressed expressions of pro-inflammatory cytokines, chemokines in placental explants through ERK activation independent of GPCR [78]. In primary human cells isolated from myometrium and fetal membranes, preincubation 5mM butyrate and 20mM propionate for 1 h increased adhesion molecules in GPCR independent manner [79]. Considering the double effects of SCFA-receptor interactions, more experiments are warranted.
HDACs
HDACs played essential roles in modifying chromosomal structure and gene expression [65]. Butyrate strongly inhibited HDAC activity and upregulated IL-10 with 0.5mM for 48 h through MAPK signaling for immunological tolerance maintenance in B10 cells [80]. In IECs, butyrate repressed indoleamine 2,3-dioxygenase 1 (IDO1) expression in dose-dependent manner ranging from 0.5 to 8mM for 24 h [81]. In neutrophils and bovine mammary epithelial cells, the propionate (≥ 4mM) and butyrate (≥ 0.4mM) reduced TNF-α and CINC-2αβ production, and higher concentrations (12mM for propionate and 1.6mM for butyrate) inhibited NO and cytokines production [82]. However, 4mM butyrate and propionate induced neutrophil chemotaxis in a time-dependent manner over 20 h only through inhibiting class I and II HDACs [83]. The HDAC 2 and 8 was mostly inhibited by propionate and butyrate, and HDAC3 was additionally inactivated by butyrate [84]. This demonstrated that butyrate and propionate induced proliferation or apoptosis through specific HDAC depending on the concentrations and cell types. “Butyrate paradox” also contributed which promoted cell proliferation cultured in normal medium by functioning as oxidative energy sources, while inhibited cells cultured in high-glucose medium as HDAC inhibitors being metabolized at relatively low levels [85].
In human umbilical vein endothelial cells, the anti-inflammatory effects of SCFAs were facilitated by simultaneously activating GPCRs and inhibiting HDACs [86]. Through activating GPCRs, IL-6 was significantly reduced by pre-incubation with 10mM acetate for 16 h, 0.3mM propionate and 0.1mM butyrate for 24 h. IL-8 was obviously decreased by acetate. HDAC activity was inhibited in the condition of 0.1mM butyrate and 0.3mM propionate with 12 h treatment, 5mM butyrate with 6 h treatment, or 10mM propionate after 48 h treatment. This indicated that whether SCFA acted as energetic substrates or signaling molecules depended on its concentration and target tissue. Summarily, most experiments were carried out using nontoxic SCFA concentrations found in the intestinal tract, which are higher than those in the blood. More studies are warranted to investigate the bilateral effects on trophoblast-derived cells and the associations with gestational complications. In addition to “indirect” associations between gut microbiome and placenta, the biological plausibility has also involved the immediate translocation of gut pathogens to invade the fetal-placental unit, which provided new perspective on microbiome-placenta axis in disease development [87, 88].
LPS-induced low grade inflammation and gut permeability
LPS overproduction is one of characteristics of gut microbiota dysbiosis, which induced inflammatory responses and diabetes development (Fig. 3). It resulted in reduced expression of tight junction proteins (TJP) including zonula occludens-1 (ZO-1), claudin and occludin. The breakdown of tight junction function led to abnormal gut permeability and LPS translocation [89]. Bacteroides vulgatus and Ruminococcus gnavus were significantly positively correlated with LPS biosynthesis in GDM [29]. Subsequently, LPS initiated inflammation via TLR-mediated MyD88-dependent pathway and transcription of IL-6 and TNF-α. It also stimulated inflammatory mediators in MyD88-independent signaling through TLR4-TRAM-TRIF-TRAF3 cascades [90, 91]. In HFD rats characterized by enhanced IR, fecal LPS level was increased parallel with upregulated MCP-α and IL1-β in plasma. The SCFA-producing genera Bacteroidetes, Prevotella spp. and Lactobacillus spp. were decreased in HFD group [92]. LPS stimulation obviously upregulated the expression of GPCR41/43 and proinflammatory cytokines, and were attenuated when incubating with 20mM acetate or propionate for 8 and 24 h [93]. Mitochondrial antiviral signaling protein (MAVS) is a component of innate immunity to maintain intestinal integrity. LPS administration accelerated injuries in MAVS knockout diabetic mice and showed more severe kidney injuries and elevated IL-17 expression [94]. The gut barrier dysfunction, decreased SCFA concentration and activated TLR4/NF-κB pathway were reversed by chemical compounds [95, 96], and blocked in intestinal flora deficient mice [97]. It proved that SCFAs were important regulators of TJP to protect barrier integrity, inhibit LPS-stimulated inflammation, attenuate oxidative stress and improve metabolic parameters through GPCRs and/or HDACs.
The effects of LPS and inflammation on microbiome in GDM. LPS overproduction is one of characteristics of gut microbiota dysbiosis in GDM. It resulted in reduced expression of tight junction proteins (TJP) which led to abnormal gut permeability and LPS translocation. This further influenced inflammatory responses on distal organs and whole body in MyD88 dependent and independent manner
The effects of GDM status and therapy on gut microbiota and metabolism in offspring and potential mechanisms
The characteristics of gut microbiota and metabolism in GDM infants and transmission mechanisms
The exposure to prenatal metabolic stress contributed to health outcomes in offspring. The vertical transmission of maternal gut microbiome triggered metabolic disease later in life, particularly from pregnancy to 1–2 years after birth [11, 98]. The infants born from GDM mothers showed decreased α and β-diversity in meconium, higher abundance of pro-inflammatory taxa including Escherichia, Parabacteroides and Bacteroides, and decreased Prevotella and Lactobacillus [99, 100]. The genus Bacteroides was related to type 1 diabetes (T1DM) development [101]. The genus Prevotella is a taxonomic biomarker of normal gestational glucose control and associated with higher insulin sensitivity [102]. The microbial co-occurrence network showed balanced correlations and less disrupted ecology in control group, while genus Rothia and Clostridium sensustricto were increased in infants born to women with GDM which caused infection and metabolic disease of childhood [103]. The disturbed microbiota also contributed to increased BMI Z-score at 12 months of age which suggested risks of childhood obesity [99, 104]. The oral Veillonella was associated with periodontal diseases and was depleted in gut microbiome among offspring born to GDM during first week of life and 9 months later [102, 104]. In a study followed up until 5 years postpartum, genera Anaerotruncus and Victivallis were all more abundant in children of GDM women, and the former was positively related with glucose intolerance and gut permeability [105]. These results suggested that microbiome variations during early life could be sustained and may be associated with abnormal glucose metabolism in later life. The β-diversity and flora constitution were more similar between mother and her own child varying by the same trend when compared with unrelated children, revealing the intergenerational concordance associated with GDM [106, 107]. Maternal diet also influenced infant microbiome colonization. The infants born to mothers with CHOICE or higher-complex carbohydrate diet exhibited greater Clostridiaceae and Bifidobacterial, and decreased Enterococcaceae. The reduced opportunistic pathogens were incapable of activating immune-metabolic responses [107, 108]. In animal studies, the Lactobacillus spp. was significantly lower and the potentially pathogenic flora such as E. coli was more abundant in HFD offspring, and contributed to higher serum glucose level, TG and HDL level until adulthood [109]. Low-calorie sweeteners addition during pregnancy exaggerated gut microbiota dysbiosis and directly influence glucose intolerance at weaning of offspring through FMT experiments [110]. Recent study found that the species Lactobacillus mentioned above and its metabolite phenyllactic acid (PLA) limited HFD-induced obesity during early life in a peroxisome proliferator-activated receptor γ (PPAR-γ) dependent manner in IECs [111]. Maternal and post-weaning high fat diet also led to higher fasting glucose and HOMA-IR level and decreased Bacteroidetes abundance at 32 weeks of age in offspring, which was obviously associated with glucose response to the glucose load [112]. In conclusion, current studies showed that gut microbiota profile was disturbed in GDM offspring and influenced metabolic status. More animal researches are warrant to provide direct evidence to explore the mechanism of early life microbial changes on metabolism later in life.
For mechanism study, the dysbiosis in GDM continued and influenced offspring through FMT experiments, manifested as increased Oscillibacter and depleted Akkermansia, Parvibacter and SCFA contents [113, 114]. In obese mice induced by HFD, the reshaped maternal gut microbiome and decreased placental GPCR43 resulted in lipid dysmetabolism of fetal liver and reprogramming [77]. Propionate promoted embryonic sympathetic neuronal and enteroendocrine differentiation directly through GPCR41/43, and improved obesity resistance [115]. In maternal low-fiber diet model, butyrate supplement improved cognitive function and synaptic plasticity in offspring through inhibiting HDAC4 [116]. The mother-to-neonate microbiota transmission was influenced by several factors such as nutritional habits, delivery mode and breastfeeding [100, 117, 118]. Overall, more direct evidence was needed to explore the mechanism by which GDM mothers influence their offspring in gut microbiome dependent pathway.
The effects of GDM therapy on gut microbiota and metabolism in offspring
Gut microbiota had become intervention target for GDM given its important roles in disease development. Combined nutritional and exercise therapy are first-line treatments and exert profound effects on GDM pregnancies and offspring [119, 120]. The pharmacological intervention is added if optimal glucose levels are not obtained. The effects of insulin on gut microbiota has not been extensively studied. One study found that the proportion of Clostridiales, Lactobacillus and Bacteroidetes were higher in women accepting insulin treatment and could be transferred to newborns [121]. In a hyperglycemic mouse model induced by HFD, Bacteroidtes was obviously downregulated and Firmicutes, Deferribacteres and Actinobacteria were increased after insulin therapy [122]. In addition to insulin, optional agents such as metformin, probiotics, prebiotics and synbiotics have been gradually promoted due to their regulatory effects on gut flora and metabolism in humans. The effectiveness and safety have been verified through clinical and animal studies. Here, we mainly focus on their effects on gut flora and metabolism in offspring.
Metformin
Metformin is considered to change intestinal microbiota profiles and improve metabolic problems. Most clinical studies were performed among patients suffering from T2DM. One study aimed to elucidate differences in maternal microbiota composition and function in GDM treated with metformin or insulin. It was showed that genus Firmicutes and Peptostreptococcaceae were declined while Proteobacteria and Enterobacteriaceae were increased with metformin therapy [123]. The enriched members were inversely correlated with maternal mean postprandial glycemia and gestational weight gain. Further analysis with a large sample size adopting metagenome/transcriptomics and follow-up to offspring is encouraged. In an animal experiment, metformin significantly reduced maternal Verrucomicrobia abundance and upregulated claudin-3 level induced by HFD [124]. In the fetal intestine, the level of pro-inflammatory marker IL-6 and apoptotic cells were also obviously inhibited [124]. Another study found that the expression levels of other TJPs such as ZO-1, occludin and claudin-4 were restored in adult male offspring after maternal metformin treatment [125]. The genera Clostridium and Lactobacillus were both enriched, and improved the body fat composition in themselves and the offspring [125].
Probiotics, prebiotics and synbiotics
Probiotic is defined as live microorganism which when administered in adequate amounts confers a health benefit on the host [126]. Prebiotics are selectively used by host microorganisms particularly Lactobacilli and Bifidobacterium and can be found in wheat, bananas and onion [126, 127]. The synbiotic is commonly composed of a probiotic combined with a prebiotic, and target on autochthonous microorganisms [126]. Single or multiple strains of probiotics supplementation during normal pregnancy exerted beneficial effects on infant microbiome and metabolism [128]. According to RCT related to GDM, the probiotics and/or fish oil intervention did not prevent GDM in overweight and obese women [129, 130]. However, they exhibited therapeutic effects and controlled glucose and lipid metabolism in women when GDM occurred [131, 132]. The effects did not transfer to neonates and influence their body weight or immune system [132, 133]. More clinical studies focus on infant microbiome and metabolism born to GDM were needed. In HFD animal model, maternal probiotics intervention ameliorated fecal microbiota dysbiosis at weaning, and the male pups was more susceptible [134]. Among adult pups, the glucose and insulin levels were decreased only in female pups accompanied by increased Bacteroidetes S24-7, which was negative correlated with glucose level [134]. The sex-dependent effect may be linked to sex hormones and the underling mechanism is unclear. In the pig offspring, maternal probiotics and synbiotics supplementation also increased the abundance of several beneficial bacteria such as Actinobacteria, Clostridium, Gemmiger, Blautia, and Roseburia. The colonic acetate and butyrate concentrations were simultaneously increased [135]. The prebiotics such as polydextrose and oligo-fructose was associated with a better metabolic status as presented by a strong clearance of glucose especially in female offspring and lower LPS level. They also increased abundance of Bacteroides and Bifidobacterium spp at early stage [136, 137]. However, some studies found that maternal supplementation of probiotics and prebiotics with HFD exerted few and even harmful effects on offspring microbiome and metabolism [138,139,140]. This suggested that the type, amount, treatment period of these agents and the physiological conditions were essential in influencing the results.
The epigenetic links between GDM and gut microbiome and their effects on offspring metabolism
The basic epigenetic signals including DNA methylation, histone modifications, noncoding RNA regulation and chromatin remodeling were considered to be involved in GDM pathophysiology. Fetal development could be further influenced by regulating genes required for the epigenomic reprogramming process in the utero. The altered microbiota seemed to be one of the most important participants of this process [141]. The microbiome derived SCFAs were widely accepted as substances in epigenetic regulation through targeting on GPCRs and/or HDACs discussed above, which served as a link between maternal microbiome and fetal health in GDM. Butyrate also regulated DNA methylation by downregulating DNMT1, demethylating downstream genes such as p21 [142]. Besides, the SCFA-producing genera Bifidobacterium spp and Roseburia exerted anti-inflammatory effects by reducing DNA methylation TRIB1 gene-mediated COX-2 expression and upregulating PGC1𝛼 gene respectively in neonatal diabetes [143]. Metformin crossed the placenta freely and had epigenetic effects on fetus via AMPK signaling [144]. Other microbiota synthesized metabolites such as biotin, folate and betaine were also involved in chromatin remodeling by modifying histones or in 5-methyltetrahydrofolate metabolism [142]. In conclusion, gut microbiota may involve in GDM pathology in an epigenetic dependent manner through its metabolites, which can be vertically transmitted to their offspring [142, 145]. Any factors influencing microbiome composition including epigenetics diets, probiotics/prebiotics and metformin, could change gene levels involved in epigenetic and posttranscriptional regulation [145]. This provided new perspectives for GDM intervention mechanism.
Conclusion
Based on previous studies, the gut microbiome and derived SCFAs involved in GDM initiation and development, and further exerted influences on their offspring. SCFAs had strong ability in regulating immune-metabolic responses, while the underlying mechanisms remained unclear. The epigenetic regulation may be essential. The SCFA-coupled GPCRs and HDACs were ubiquitously expressed in gestational and embryonic tissues. Depending on concentrations and cell types, SCFAs bound to different downstream molecules and involved in specific physiological processes, which laid the foundation of microbiota-placenta or microbiota-fetus axis establishment. Recent FMT studies showed that the microbiome influenced placental structure and development, especially nutrient transport functions through SCFAs [146, 147]. Multi-omics approach reveled close relationships between host metabolomes in evaluating risks of neonatal inborn errors of metabolism, providing new evidence of effects of maternal gut flora on offspring. However, few studies have analyzed the relationship between gut microbiota and GDM development through the genetics, metabolomics and gut microbiota. It is needed to determine differences between normal and GDM pregnancies, and their concordance variations with offspring. Based on these, the gut microbiota interventions might become novel technology to reduce GDM risk, the GDM-induced complication risks and childhood metabolic disorders.
Data availability
No datasets were generated or analysed during the current study.
References
Bowman CE, Arany Z, Wolfgang MJ. Regulation of maternal-fetal metabolic communication. Cell Mol Life Sci. 2021;78:1455–86.
Sferruzzi-Perri AN, Lopez-Tello J, Napso T, Yong HEJ. Exploring the causes and consequences of maternal metabolic maladaptations during pregnancy: lessons from animal models. Placenta. 2020;98:43–51.
Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358(19):1991–2002.
Cortez RV, Taddei CR, Sparvoli LG, Ângelo AGS, Padilha M, Mattar R, et al. Microbiome and its relation to gestational diabetes. Endocrine. 2019;64(2):254–64.
Medici Dualib P, Ogassavara J, Mattar R, Mariko Koga da Silva E, Atala Dib S, de Almeida Pititto B. Gut microbiota and gestational diabetes Mellitus: a systematic review. Diabetes Res Clin Pract. 2021;180:109078.
Wu Y, Bible PW, Long S, Ming WK, Ding W, Long Y, et al. Metagenomic analysis reveals gestational diabetes mellitus-related microbial regulators of glucose tolerance. Acta Diabetol. 2020;57(5):569–81.
Zhang H, Qi C, Zhao Y, Lu M, Li X, Zhou J, et al. Depletion of gut secretory immunoglobulin a coated Lactobacillus reuteri is associated with gestational diabetes mellitus-related intestinal mucosal barrier damage. Food Funct. 2021;12(21):10783–94.
Priyadarshini M, Thomas A, Reisetter AC, Scholtens DM, Wolever TM, Josefson JL, et al. Maternal short-chain fatty acids are associated with metabolic parameters in mothers and newborns. Transl Res. 2014;164(2):153–7.
Larraufie P, Doré J, Lapaque N, Blottière HM. TLR ligands and butyrate increase pyy expression through two distinct but inter-regulated pathways. Cell Microbiol 2017;19(2).
Velloso LA, Folli F, Saad MJ. TLR4 at the crossroads of nutrients, gut microbiota, and metabolic inflammation. Endocr Rev. 2015;36(3):245–71.
Xiao L, Zhao F. Microbial transmission, colonisation and succession: from pregnancy to infancy. Gut. 2023;72(4):772–86.
Chen T, Zhang Y, Zhang Y, Shan C, Zhang Y, Fang K, et al. Relationships between gut microbiota, plasma glucose and gestational diabetes mellitus. J Diabetes Investig. 2021;12(4):641–50.
Mokkala K, Paulin N, Houttu N, Koivuniemi E, Pellonperä O, Khan S, et al. Metagenomics analysis of gut microbiota in response to diet intervention and gestational diabetes in overweight and obese women: a randomised, double-blind, placebo-controlled clinical trial. Gut. 2021;70(2):309–18.
Crusell MKW, Hansen TH, Nielsen T, Allin KH, Rühlemann MC, Damm P, et al. Gestational diabetes is associated with change in the gut microbiota composition in third trimester of pregnancy and postpartum. Microbiome. 2018;6(1):89.
Huang L, Sililas P, Thonusin C, Luewan S, Chattipakorn SC. Early gut dysbiosis could be an indicator of unsuccessful diet control in gestational diabetes mellitus. J Diabetes. 2021;13(12):1054–8.
Zheng W, Xu Q, Huang W, Yan Q, Chen Y, Zhang L et al. Gestational diabetes Mellitus is Associated with reduced dynamics of Gut Microbiota during the first half of pregnancy. mSystems. 2020;5(2).
Hu P, Chen X, Chu X, Fan M, Ye Y, Wang Y et al. Association of Gut Microbiota during early pregnancy with risk of Incident Gestational Diabetes Mellitus. J Clin Endocrinol Metab. 2021.
Sun Z, Pan XF, Li X, Jiang L, Hu P, Wang Y, et al. The Gut Microbiome Dynamically Associates with Host Glucose Metabolism throughout pregnancy: longitudinal findings from a Matched Case-Control Study of Gestational Diabetes Mellitus. Adv Sci (Weinh). 2023;10(10):e2205289.
Ma S, You Y, Huang L, Long S, Zhang J, Guo C, et al. Alterations in gut microbiota of gestational diabetes patients during the first trimester of pregnancy. Front Cell Infect Microbiol. 2020;10:58.
Vavreckova M, Galanova N, Kostovcik M, Krystynik O, Ivanovova E, Roubalova R, et al. Specific gut bacterial and fungal microbiota pattern in the first half of pregnancy is linked to the development of gestational diabetes mellitus in the cohort including obese women. Front Endocrinol (Lausanne). 2022;13:970825.
Pinto Y, Frishman S, Turjeman S, Eshel A, Nuriel-Ohayon M, Shrossel O, et al. Gestational diabetes is driven by microbiota-induced inflammation months before diagnosis. Gut. 2023;72(5):918–28.
Chen F, Gan Y, Li Y, He W, Wu W, Wang K, et al. Association of gestational diabetes mellitus with changes in gut microbiota composition at the species level. BMC Microbiol. 2021;21(1):147.
Su Y, Wang HK, Gan XP, Chen L, Cao YN, Cheng DC, et al. Alterations of gut microbiota in gestational diabetes patients during the second trimester of pregnancy in the Shanghai Han population. J Transl Med. 2021;19(1):366.
Wei J, Qing Y, Zhou H, Liu J, Qi C, Gao J. 16S rRNA gene amplicon sequencing of gut microbiota in gestational diabetes mellitus and their correlation with disease risk factors. J Endocrinol Invest. 2022;45(2):279–89.
Ye D, Huang J, Wu J, Xie K, Gao X, Yan K, et al. Integrative metagenomic and metabolomic analyses reveal gut microbiota-derived multiple hits connected to development of gestational diabetes mellitus in humans. Gut Microbes. 2023;15(1):2154552.
Kuang YS, Lu JH, Li SH, Li JH, Yuan MY, He JR, et al. Connections between the human gut microbiome and gestational diabetes mellitus. Gigascience. 2017;6(8):1–12.
Ye G, Zhang L, Wang M, Chen Y, Gu S, Wang K, et al. The gut microbiota in women suffering from Gestational Diabetes Mellitus with the failure of Glycemic Control by Lifestyle Modification. J Diabetes Res. 2019;2019:6081248.
Chen J, Yang Y, Yu N, Sun W, Yang Y, Zhao M. Relationship between gut microbiome characteristics and the effect of nutritional therapy on glycemic control in pregnant women with gestational diabetes mellitus. PLoS ONE. 2022;17(4):e0267045.
Li M, Zhang G, Cui L, Zhang L, Zhou Q, Mu C, et al. Dynamic changes in gut microbiota during pregnancy among Chinese women and influencing factors: a prospective cohort study. Front Microbiol. 2023;14:1114228.
Dong L, Han L, Duan T, Lin S, Li J, Liu X. Integrated microbiome-metabolome analysis reveals novel associations between fecal microbiota and hyperglycemia-related changes of plasma metabolome in gestational diabetes mellitus. RSC Adv. 2020;10(4):2027–36.
Mullins TP, Tomsett KI, Gallo LA, Callaway LK, McIntyre HD, Dekker Nitert M, et al. Maternal gut microbiota displays minor changes in overweight and obese women with GDM. Nutr Metab Cardiovasc Dis. 2021;31(7):2131–9.
Xu Y, Zhang M, Zhang J, Sun Z, Ran L, Ban Y, et al. Differential intestinal and oral microbiota features associated with gestational diabetes and maternal inflammation. Am J Physiol Endocrinol Metab. 2020;319(2):E247–53.
Zhang X, Wang P, Ma L, Guo R, Zhang Y, Wang P, et al. Differences in the oral and intestinal microbiotas in pregnant women varying in periodontitis and gestational diabetes mellitus conditions. J Oral Microbiol. 2021;13(1):1883382.
Li G, Yin P, Chu S, Gao W, Cui S, Guo S, et al. Correlation analysis between GDM and Gut Microbial Composition in late pregnancy. J Diabetes Res. 2021;2021:8892849.
Wang X, Liu H, Li Y, Huang S, Zhang L, Cao C, et al. Altered gut bacterial and metabolic signatures and their interaction in gestational diabetes mellitus. Gut Microbes. 2020;12(1):1–13.
Ferrocino I, Ponzo V, Gambino R, Zarovska A, Leone F, Monzeglio C, et al. Changes in the gut microbiota composition during pregnancy in patients with gestational diabetes mellitus (GDM). Sci Rep. 2018;8(1):12216.
Tanaka K, Harata G, Miyazawa K, He F, Tanigaki S, Kobayashi Y. The gut microbiota of non-obese Japanese pregnant women with gestational diabetes mellitus. Biosci Microbiota Food Health. 2022;41(1):4–11.
Dualib PM, Taddei CR, Fernandes G, Carvalho CRS, Sparvoli LG, Silva IT et al. Gut microbiota across normal Gestation and Gestational Diabetes Mellitus: a cohort analysis. Metabolites. 2022;12(9).
Liu Y, Qin S, Feng Y, Song Y, Lv N, Liu F, et al. Perturbations of gut microbiota in gestational diabetes mellitus patients induce hyperglycemia in germ-free mice. J Dev Orig Health Dis. 2020;11(6):580–8.
Zouiouich S, Loftfield E, Huybrechts I, Viallon V, Louca P, Vogtmann E, et al. Markers of metabolic health and gut microbiome diversity: findings from two population-based cohort studies. Diabetologia. 2021;64(8):1749–59.
Sun YY, Juan J, Xu QQ, Su RN, Hirst JE, Yang HX. Increasing insulin resistance predicts adverse pregnancy outcomes in women with gestational diabetes mellitus. J Diabetes. 2020;12(6):438–46.
Yang H, Guo R, Li S, Liang F, Tian C, Zhao X, et al. Systematic analysis of gut microbiota in pregnant women and its correlations with individual heterogeneity. NPJ Biofilms Microbiomes. 2020;6(1):32.
Stanislawski MA, Dabelea D, Wagner BD, Sontag MK, Lozupone CA, Eggesbø M. Pre-pregnancy weight, gestational weight gain, and the gut microbiota of mothers and their infants. Microbiome. 2017;5(1):113.
Morrison DJ, Preston T. Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism. Gut Microbes. 2016;7(3):189–200.
Martin-Gallausiaux C, Marinelli L, Blottière HM, Larraufie P, Lapaque N. SCFA: mechanisms and functional importance in the gut. Proc Nutr Soc. 2021;80(1):37–49.
Louis P, Hold GL, Flint HJ. The gut microbiota, bacterial metabolites and colorectal cancer. Nat Rev Microbiol. 2014;12(10):661–72.
Prentice PM, Schoemaker MH, Vervoort J, Hettinga K, Lambers TT, van Tol EAF, et al. Human Milk Short-Chain Fatty Acid Composition is Associated with Adiposity outcomes in infants. J Nutr. 2019;149(5):716–22.
Mueller NT, Differding MK, Østbye T, Hoyo C, Benjamin-Neelon SE. Association of birth mode of delivery with infant faecal microbiota, potential pathobionts, and short chain fatty acids: a longitudinal study over the first year of life. BJOG. 2021;128(8):1293–303.
Ziętek M, Celewicz Z, Kikut J, Szczuko M. Implications of SCFAs on the parameters of the lipid and hepatic Profile in pregnant women. Nutrients. 2021;13(6).
Szczuko M, Kikut J, Maciejewska D, Kulpa D, Celewicz Z, Ziętek M. The associations of SCFA with Anthropometric Parameters and Carbohydrate Metabolism in pregnant women. Int J Mol Sci. 2020;21(23).
Wang S, Liu Y, Qin S, Yang H. Composition of maternal circulating short-chain fatty acids in gestational diabetes Mellitus and their associations with placental metabolism. Nutrients. 2022;14:18.
Gao Y, Chen H, Li J, Ren S, Yang Z, Zhou Y, et al. Alterations of gut microbiota-derived metabolites in gestational diabetes mellitus and clinical significance. J Clin Lab Anal. 2022;36(4):e24333.
Müller M, Hernández MAG, Goossens GH, Reijnders D, Holst JJ, Jocken JWE, et al. Circulating but not faecal short-chain fatty acids are related to insulin sensitivity, lipolysis and GLP-1 concentrations in humans. Sci Rep. 2019;9(1):12515.
Canfora EE, Jocken JW, Blaak EE. Short-chain fatty acids in control of body weight and insulin sensitivity. Nat Rev Endocrinol. 2015;11:577–91.
den Besten G, Bleeker A, Gerding A, van Eunen K, Havinga R, van Dijk TH, et al. Short-chain fatty acids protect Against High-Fat Diet-Induced obesity via a PPARγ-Dependent switch from Lipogenesis to Fat Oxidation. Diabetes. 2015;64(7):2398–408.
Hao F, Tian M, Zhang X, Jin X, Jiang Y, Sun X et al. Butyrate enhances CPT1A activity to promote fatty acid oxidation and iTreg differentiation. Proc Natl Acad Sci U S A. 2021;118(22).
Tan J, McKenzie C, Potamitis M, Thorburn AN, Mackay CR, Macia L. The role of short-chain fatty acids in health and disease. Adv Immunol. 2014;121:91–119.
De Vadder F, Kovatcheva-Datchary P, Goncalves D, Vinera J, Zitoun C, Duchampt A, et al. Microbiota-generated metabolites promote metabolic benefits via gut-brain neural circuits. Cell. 2014;156(1–2):84–96.
Todesco T, Rao AV, Bosello O, Jenkins DJ. Propionate lowers blood glucose and alters lipid metabolism in healthy subjects. Am J Clin Nutr. 1991;54(5):860–5.
Zhao L, Zhang F, Ding X, Wu G, Lam YY, Wang X, et al. Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science. 2018;359(6380):1151–6.
Ziętek M, Celewicz Z, Szczuko M. Short-chain fatty acids, maternal microbiota and metabolism in pregnancy. Nutrients. 2021;13(4).
Olofsson LE, Bäckhed F. The metabolic role and therapeutic potential of the Microbiome. Endocr Rev. 2022.
Priyadarshini M, Wicksteed B, Schiltz GE, Gilchrist A, Layden BT. SCFA Receptors in pancreatic β cells: novel diabetes targets? Trends Endocrinol Metab. 2016;27(9):653–64.
Singh V, Chassaing B, Zhang L, San Yeoh B, Xiao X, Kumar M, et al. Microbiota-dependent hepatic lipogenesis mediated by Stearoyl CoA Desaturase 1 (SCD1) promotes metabolic syndrome in TLR5-Deficient mice. Cell Metab. 2015;22(6):983–96.
He J, Zhang P, Shen L, Niu L, Tan Y, Chen L et al. Short-chain fatty acids and their association with signalling pathways in inflammation, glucose and lipid metabolism. Int J Mol Sci. 2020;21(17).
Tolhurst G, Heffron H, Lam YS, Parker HE, Habib AM, Diakogiannaki E, et al. Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein-coupled receptor FFAR2. Diabetes. 2012;61(2):364–71.
Chun E, Lavoie S, Fonseca-Pereira D, Bae S, Michaud M, Hoveyda HR, et al. Metabolite-sensing receptor Ffar2 regulates Colonic Group 3 innate lymphoid cells and gut immunity. Immunity. 2019;51(5):871–e8846.
Yang W, Yu T, Huang X, Bilotta AJ, Xu L, Lu Y, et al. Intestinal microbiota-derived short-chain fatty acids regulation of immune cell IL-22 production and gut immunity. Nat Commun. 2020;11(1):4457.
Zhao Y, Chen F, Wu W, Sun M, Bilotta AJ, Yao S, et al. GPR43 mediates microbiota metabolite SCFA regulation of antimicrobial peptide expression in intestinal epithelial cells via activation of mTOR and STAT3. Mucosal Immunol. 2018;11(3):752–62.
Wu W, Sun M, Chen F, Cao AT, Liu H, Zhao Y, et al. Microbiota metabolite short-chain fatty acid acetate promotes intestinal IgA response to microbiota which is mediated by GPR43. Mucosal Immunol. 2017;10(4):946–56.
Zhuang P, Li H, Jia W, Shou Q, Zhu Y, Mao L, et al. Eicosapentaenoic and docosahexaenoic acids attenuate hyperglycemia through the microbiome-gut-organs axis in db/db mice. Microbiome. 2021;9(1):185.
Li YJ, Chen X, Kwan TK, Loh YW, Singer J, Liu Y, et al. Dietary Fiber protects against Diabetic Nephropathy through short-chain fatty acid-mediated activation of G protein-coupled receptors GPR43 and GPR109A. J Am Soc Nephrol. 2020;31(6):1267–81.
Kobayashi M, Mikami D, Kimura H, Kamiyama K, Morikawa Y, Yokoi S, et al. Short-chain fatty acids, GPR41 and GPR43 ligands, inhibit TNF-α-induced MCP-1 expression by modulating p38 and JNK signaling pathways in human renal cortical epithelial cells. Biochem Biophys Res Commun. 2017;486(2):499–505.
Vieira AT, Macia L, Galvão I, Martins FS, Canesso MC, Amaral FA, et al. A role for gut microbiota and the metabolite-sensing receptor GPR43 in a murine model of gout. Arthritis Rheumatol. 2015;67(6):1646–56.
Boro P, Kumaresan A, Singh AK, Gupta D, Kumar S, Manimaran A, et al. Expression of short chain fatty acid receptors and pro-inflammatory cytokines in utero-placental tissues is altered in cows developing retention of fetal membranes. Placenta. 2014;35(7):455–60.
Fuller M, Priyadarshini M, Gibbons SM, Angueira AR, Brodsky M, Hayes MG, et al. The short-chain fatty acid receptor, FFA2, contributes to gestational glucose homeostasis. Am J Physiol Endocrinol Metab. 2015;309(10):E840–851.
Wang YW, Yu HR, Tiao MM, Tain YL, Lin IC, Sheen JM, et al. Maternal obesity related to high Fat Diet induces placenta remodeling and gut microbiome shaping that are responsible for fetal liver lipid dysmetabolism. Front Nutr. 2021;8:736944.
Roy R, Nguyen-Ngo C, Lappas M. Short-chain fatty acids as novel therapeutics for gestational diabetes. J Mol Endocrinol. 2020;65(2):21–34.
Moylan HEC, Nguyen-Ngo C, Lim R, Lappas M. The short-chain fatty acids butyrate and propionate protect against inflammation-induced activation of mediators involved in active labor: implications for preterm birth. Mol Hum Reprod. 2020;26(6):452–68.
Zou F, Qiu Y, Huang Y, Zou H, Cheng X, Niu Q, et al. Effects of short-chain fatty acids in inhibiting HDAC and activating p38 MAPK are critical for promoting B10 cell generation and function. Cell Death Dis. 2021;12(6):582.
Martin-Gallausiaux C, Larraufie P, Jarry A, Béguet-Crespel F, Marinelli L, Ledue F, et al. Butyrate produced by commensal Bacteria down-regulates c (IDO-1) expression via a dual mechanism in human intestinal epithelial cells. Front Immunol. 2018;9:2838.
Vinolo MA, Rodrigues HG, Hatanaka E, Sato FT, Sampaio SC, Curi R. Suppressive effect of short-chain fatty acids on production of proinflammatory mediators by neutrophils. J Nutr Biochem. 2011;22(9):849–55.
Aoyama M, Kotani J, Usami M. Butyrate and propionate induced activated or non-activated neutrophil apoptosis via HDAC inhibitor activity but without activating GPR-41/GPR-43 pathways. Nutrition. 2010;26(6):653–61.
Silva LG, Ferguson BS, Avila AS, Faciola AP. Sodium propionate and sodium butyrate effects on histone deacetylase (HDAC) activity, histone acetylation, and inflammatory gene expression in bovine mammary epithelial cells. J Anim Sci. 2018;96(12):5244–52.
Donohoe DR, Collins LB, Wali A, Bigler R, Sun W, Bultman SJ. The Warburg effect dictates the mechanism of butyrate-mediated histone acetylation and cell proliferation. Mol Cell. 2012;48(4):612–26.
Li M, van Esch B, Henricks PAJ, Folkerts G, Garssen J. The anti-inflammatory effects of short chain fatty acids on Lipopolysaccharide- or tumor necrosis factor α-Stimulated endothelial cells via activation of GPR41/43 and inhibition of HDACs. Front Pharmacol. 2018;9:533.
Bendek MJ, Canedo-Marroquín G, Realini O, Retamal IN, Hernández M, Hoare A et al. Periodontitis and Gestational Diabetes Mellitus: a potential inflammatory vicious cycle. Int J Mol Sci. 2021;22(21).
Chen X, Li P, Liu M, Zheng H, He Y, Chen MX, et al. Gut dysbiosis induces the development of pre-eclampsia through bacterial translocation. Gut. 2020;69(3):513–22.
Saad MJ, Santos A, Prada PO. Linking gut microbiota and inflammation to obesity and insulin resistance. Physiol (Bethesda). 2016;31(4):283–93.
Dauphinee SM, Karsan A. Lipopolysaccharide signaling in endothelial cells. Lab Invest. 2006;86(1):9–22.
Vallance TM, Zeuner MT, Williams HF, Widera D, Vaiyapuri S. Toll-like receptor 4 signalling and its impact on platelet function, thrombosis, and Haemostasis. Mediators Inflamm. 2017;2017:9605894.
Lau E, Marques C, Pestana D, Santoalha M, Carvalho D, Freitas P, et al. The role of I-FABP as a biomarker of intestinal barrier dysfunction driven by gut microbiota changes in obesity. Nutr Metab (Lond). 2016;13:31.
Voltolini C, Battersby S, Etherington SL, Petraglia F, Norman JE, Jabbour HN. A novel antiinflammatory role for the short-chain fatty acids in human labor. Endocrinology. 2012;153(1):395–403.
Linh HT, Iwata Y, Senda Y, Sakai-Takemori Y, Nakade Y, Oshima M et al. Intestinal bacterial translocation contributes to Diabetic kidney disease. J Am Soc Nephrol. 2022.
Liu M, Huang B, Wang L, Lu Q, Liu R. Peanut skin procyanidins ameliorate insulin resistance via modulation of gut microbiota and gut barrier in type 2 diabetic mice. J Sci Food Agric. 2022.
Liu D, Zhang Y, Liu Y, Hou L, Li S, Tian H, et al. Berberine modulates gut microbiota and reduces insulin resistance via the TLR4 signaling pathway. Exp Clin Endocrinol Diabetes. 2018;126(8):513–20.
Liu Y, Sun R, Lin X, Wu L, Chen H, Shen S, et al. Procyanidins and its metabolites by gut microbiome improves insulin resistance in gestational diabetes mellitus mice model via regulating NF-κB and NLRP3 inflammasome pathway. Biomed Pharmacother. 2022;151:113078.
Dora C, Haines A, Balbus J, Fletcher E, Adair-Rohani H, Alabaster G, et al. Indicators linking health and sustainability in the post-2015 development agenda. Lancet. 2015;385(9965):380–91.
Zhu Q, Yang X, Zhang Y, Shan C, Shi Z. Role of the gut microbiota in the increased infant body Mass Index Induced by Gestational Diabetes Mellitus. mSystems. 2022;7(5):e0046522.
Ponzo V, Ferrocino I, Zarovska A, Amenta MB, Leone F, Monzeglio C, et al. The microbiota composition of the offspring of patients with gestational diabetes mellitus (GDM). PLoS ONE. 2019;14(12):e0226545.
Soderborg TK, Carpenter CM, Janssen RC, Weir TL, Robertson CE, Ir D, et al. Gestational diabetes is uniquely Associated with altered early seeding of the infant gut microbiota. Front Endocrinol (Lausanne). 2020;11:603021.
Crusell MKW, Hansen TH, Nielsen T, Allin KH, Rühlemann MC, Damm P, et al. Comparative studies of the gut microbiota in the offspring of mothers with and without gestational diabetes. Front Cell Infect Microbiol. 2020;10:536282.
Chen T, Qin Y, Chen M, Zhang Y, Wang X, Dong T, et al. Gestational diabetes mellitus is associated with the neonatal gut microbiota and metabolome. BMC Med. 2021;19(1):120.
Song Q, Xiao B, Huang H, Ma L, Zhang JV, Zhu Y. Influences of gestational diabetes mellitus on the oral microbiota in offspring from birth to 1 month old. BMC Pregnancy Childbirth. 2022;22(1):289.
Hasan S, Aho V, Pereira P, Paulin L, Koivusalo SB, Auvinen P, et al. Gut microbiome in gestational diabetes: a cross-sectional study of mothers and offspring 5 years postpartum. Acta Obstet Gynecol Scand. 2018;97(1):38–46.
Wang J, Zheng J, Shi W, Du N, Xu X, Zhang Y, et al. Dysbiosis of maternal and neonatal microbiota associated with gestational diabetes mellitus. Gut. 2018;67(9):1614–25.
Nieto-Ruiz A, Cerdó T, Jordano B, Torres-Espínola FJ, Escudero-Marín M, García-Ricobaraza M, et al. Maternal weight, gut microbiota, and the association with early childhood behavior: the PREOBE follow-up study. Child Adolesc Psychiatry Ment Health. 2023;17(1):41.
Sugino KY, Hernandez TL, Barbour LA, Kofonow JM, Frank DN, Friedman JE. A maternal higher-complex carbohydrate diet increases bifidobacteria and alters early life acquisition of the infant microbiome in women with gestational diabetes mellitus. Front Endocrinol (Lausanne). 2022;13:921464.
Djekkoun N, Depeint F, Guibourdenche M, Sabbouri H, Corona A, Rhazi L, et al. Perigestational exposure of a combination of a high-fat diet and pesticide impacts the metabolic and microbiotic status of dams and pups; a preventive strategy based on prebiotics. Eur J Nutr. 2023;62(3):1253–65.
Nettleton JE, Cho NA, Klancic T, Nicolucci AC, Shearer J, Borgland SL, et al. Maternal low-dose aspartame and stevia consumption with an obesogenic diet alters metabolism, gut microbiota and mesolimbic reward system in rat dams and their offspring. Gut. 2020;69(10):1807–17.
Shelton CD, Sing E, Mo J, Shealy NG, Yoo W, Thomas J, et al. An early-life microbiota metabolite protects against obesity by regulating intestinal lipid metabolism. Cell Host Microbe. 2023;31(10):1604–e161910.
Zheng J, Xiao X, Zhang Q, Yu M, Xu J, Qi C et al. The effects of maternal and post-weaning diet interaction on glucose metabolism and gut microbiota in male mice offspring. Biosci Rep. 2016;36(3).
Qin S, Wang Y, Wang S, Ning B, Huai J, Yang H. Gut microbiota in women with gestational diabetes mellitus has potential impact on metabolism in pregnant mice and their offspring. Front Microbiol. 2022;13:870422.
Zheng J, Zhang L, Gao Y, Wu H, Zhang J. The dynamic effects of maternal high-calorie diet on glycolipid metabolism and gut microbiota from weaning to adulthood in offspring mice. Front Nutr. 2022;9:941969.
Kimura I, Miyamoto J, Ohue-Kitano R, Watanabe K, Yamada T, Onuki M et al. Maternal gut microbiota in pregnancy influences offspring metabolic phenotype in mice. Science. 2020;367(6481).
Yu L, Zhong X, He Y, Shi Y. Butyrate, but not propionate, reverses maternal diet-induced neurocognitive deficits in offspring. Pharmacol Res. 2020;160:105082.
Shao Y, Forster SC, Tsaliki E, Vervier K, Strang A, Simpson N, et al. Stunted microbiota and opportunistic pathogen colonization in caesarean-section birth. Nature. 2019;574(7776):117–21.
Xue C, Xie Q, Zhang C, Hu Y, Song X, Jia Y, et al. Vertical transmission of the gut microbiota influences glucose metabolism in offspring of mice with hyperglycaemia in pregnancy. Microbiome. 2022;10(1):122.
Zhou L, Xiao X, Li M, Zhang Q, Yu M, Zheng J, et al. Maternal Exercise improves high-Fat Diet-Induced metabolic abnormalities and gut microbiota profiles in mouse dams and offspring. Front Cell Infect Microbiol. 2020;10:292.
Bhagavata Srinivasan SP, Raipuria M, Bahari H, Kaakoush NO, Morris MJ. Impacts of Diet and Exercise on maternal gut microbiota are transferred to offspring. Front Endocrinol (Lausanne). 2018;9:716.
Huang L, Sililas P, Thonusin C, Tongsong T, Luewan S, Chattipakorn N, et al. Association between gut microbiota and insulin therapy in Women with Gestational Diabetes Mellitus. Can J Diabetes. 2022;46(8):804–e8122.
Wang H, Tang W, Zhang P, Zhang Z, He J, Zhu D, et al. Modulation of gut microbiota contributes to effects of intensive insulin therapy on intestinal morphological alteration in high-fat-diet-treated mice. Acta Diabetol. 2020;57(4):455–67.
Molina-Vega M, Picón-César MJ, Gutiérrez-Repiso C, Fernández-Valero A, Lima-Rubio F, González-Romero S, et al. Metformin action over gut microbiota is related to weight and glycemic control in gestational diabetes mellitus: a randomized trial. Biomed Pharmacother. 2022;145:112465.
Huang SW, Ou YC, Tang KS, Yu HR, Huang LT, Tain YL, et al. Metformin ameliorates maternal high-fat diet-induced maternal dysbiosis and fetal liver apoptosis. Lipids Health Dis. 2021;20(1):100.
Song L, Cui J, Hu S, Wang R, Li H, Sun B. Maternal Treatment with Metformin Persistently Ameliorates High-Fat Diet-Induced Metabolic Symptoms and Modulates Gut Microbiota in Rat Offspring. Nutrients. 2022;14(17).g.
Swanson KS, Gibson GR, Hutkins R, Reimer RA, Reid G, Verbeke K, et al. The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of synbiotics. Nat Rev Gastroenterol Hepatol. 2020;17(11):687–701.
Wang S, Peng R, Qin S, Liu Y, Yang H, Ma J. Effects of oligosaccharide-sialic acid (OS) compound on maternal-newborn gut microbiome, glucose metabolism and systematic immunity in pregnancy: protocol for a randomised controlled study. BMJ Open. 2019;9(9):e026583.
Zaidi AZ, Moore SE, Okala SG. Impact of maternal nutritional supplementation during pregnancy and lactation on the infant gut or breastmilk microbiota: a systematic review. Nutrients. 2021;13(4).
Callaway LK, McIntyre HD, Barrett HL, Foxcroft K, Tremellen A, Lingwood BE, et al. Probiotics for the Prevention of Gestational Diabetes Mellitus in overweight and obese women: findings from the SPRING double-blind randomized controlled trial. Diabetes Care. 2019;42(3):364–71.
Pellonperä O, Mokkala K, Houttu N, Vahlberg T, Koivuniemi E, Tertti K, et al. Efficacy of Fish Oil and/or probiotic intervention on the incidence of gestational diabetes Mellitus in an At-Risk group of overweight and obese women: a Randomized, Placebo-Controlled, double-blind clinical trial. Diabetes Care. 2019;42(6):1009–17.
Mu J, Guo X, Zhou Y, Cao G. The effects of Probiotics/Synbiotics on glucose and lipid metabolism in women with gestational diabetes Mellitus: a Meta-analysis of Randomized controlled trials. Nutrients. 2023;15(6).
Shadid R, Haarman M, Knol J, Theis W, Beermann C, Rjosk-Dendorfer D, et al. Effects of galactooligosaccharide and long-chain fructooligosaccharide supplementation during pregnancy on maternal and neonatal microbiota and immunity–a randomized, double-blind, placebo-controlled study. Am J Clin Nutr. 2007;86(5):1426–37.
Wang CC, Tung YT, Chang HC, Lin CH, Chen YC. Effect of Probiotic supplementation on Newborn Birth Weight for Mother with Gestational Diabetes Mellitus or Overweight/Obesity: a systematic review and Meta-analysis. Nutrients. 2020;12(11).
Guo Y, Wang Z, Chen L, Tang L, Wen S, Liu Y, et al. Diet induced maternal obesity affects offspring gut microbiota and persists into young adulthood. Food Funct. 2018;9(8):4317–27.
Zhu Q, Song M, Azad MAK, Cheng Y, Liu Y, Liu Y, et al. Probiotics or synbiotics addition to sows’ diets alters colonic microbiome composition and metabolome profiles of offspring pigs. Front Microbiol. 2022;13:934890.
Maragkoudaki X, Naylor M, Papacleovoulou G, Stolarczyk E, Rees D, Pombo JM, et al. Supplementation with a prebiotic (polydextrose) in obese mouse pregnancy improves maternal glucose homeostasis and protects against offspring obesity. Int J Obes (Lond). 2020;44(12):2382–93.
Paul HA, Collins KH, Nicolucci AC, Urbanski SJ, Hart DA, Vogel HJ, et al. Maternal prebiotic supplementation reduces fatty liver development in offspring through altered microbial and metabolomic profiles in rats. Faseb j. 2019;33(4):5153–67.
Mennitti LV, Oyama LM, de Oliveira JL, Hachul AC, Santamarina AB, de Santana AA, et al. Oligofructose supplementation during pregnancy and lactation impairs offspring development and alters the intestinal properties of 21-d-old pups. Lipids Health Dis. 2014;13:26.
Azagra-Boronat I, Tres A, Massot-Cladera M, Franch À, Castell M, Guardiola F et al. Lactobacillus fermentum CECT5716 supplementation in rats during pregnancy and lactation impacts maternal and offspring lipid Profile, Immune System and Microbiota. Cells. 2020;9(3).
Duan X, Ma G, Lin Y, Xu J, Yang P, Xiao X. Effect of a high-Fat Diet and Probiotic supplementation on the gut microbiota of maternal mice at term pregnancy and offspring at three-week Postpartum. Curr Microbiol. 2023;80(11):358.
Mora-Janiszewska O, Faryniak-Zuzak A, Darmochwał-Kolarz D. Epigenetic links between Microbiota and Gestational Diabetes. Int J Mol Sci. 2022;23(3).
Bankole T, Winn H, Li Y. Dietary impacts on gestational diabetes: connection between gut microbiome and epigenetic mechanisms. Nutrients. 2022;14(24).
Alsharairi NA. Exploring the Diet-Gut Microbiota-Epigenetics Crosstalk relevant to neonatal diabetes. Genes (Basel). 2023;14(5).
Bridgeman SC, Ellison GC, Melton PE, Newsholme P, Mamotte CDS. Epigenetic effects of metformin: from molecular mechanisms to clinical implications. Diabetes Obes Metab. 2018;20(7):1553–62.
Lizárraga D, Gómez-Gil B, García-Gasca T, Ávalos-Soriano A, Casarini L, Salazar-Oroz A et al. Gestational diabetes mellitus: genetic factors, epigenetic alterations, and microbial composition. Acta Diabetol. 2023.
Lopez-Tello J, Schofield Z, Kiu R, Dalby MJ, van Sinderen D, Le Gall G, et al. Maternal gut microbiota Bifidobacterium promotes placental morphogenesis, nutrient transport and fetal growth in mice. Cell Mol Life Sci. 2022;79(7):386.
Pronovost GN, Yu KB, Coley-O’Rourke EJL, Telang SS, Chen AS, Vuong HE, et al. The maternal microbiome promotes placental development in mice. Sci Adv. 2023;9(40):eadk1887.
Acknowledgements
Not applicable.
Funding
This work was supported by the National Key Research and Development Program of China (No. 2021YFC2700700), National Natural Science Foundation of China (81830044).
Author information
Authors and Affiliations
Contributions
HY conceived the project and is responsible for the overall content as the guarantor. SW contributed to literature search and writing. ZC provided valuable suggestions.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, S., Cui, Z. & Yang, H. Interactions between host and gut microbiota in gestational diabetes mellitus and their impacts on offspring. BMC Microbiol 24, 161 (2024). https://doi.org/10.1186/s12866-024-03255-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12866-024-03255-y