Abstract
Background
The purpose of this study was to compare the surgical, functional, and oncological outcomes between open partial nephrectomy (OPN) and laparoscopic partial nephrectomy (LPN).
Methods
This prospective, randomized study was performed on patients who underwent partial nephrectomy under general anesthesia. Patients were randomized using the closed envelope method to either LPN or OPN. Baseline demographics and surgical, functional, and oncological outcomes were compared. A per-protocol analysis was used.
Results
Randomized study was conducted on 166 patients. The LPN, in comparison to the OPN group, was associated with significantly shorter hospital stay (3 vs. 4 days), less blood transfusion (10% vs. 12%), longer operative time (134 min vs. 124 min), lower visual analog pain score (7 vs. 8), and lower estimated GFR (70.7 ± 17.5 vs. 72.3 ± 14.7).
Conclusions
Oncological and functional results were comparable between LPN and OPN. However, LPN was superior to open surgery because of less hospital stay, visual analog pain score, and blood loss.
Similar content being viewed by others
1 Background
The frequency of kidney cancer has progressively increased worldwide during the past two to three decades [1]. For localized renal cell carcinoma (RCC), the EAU (European Association of Urology) guidelines recommend surgery as the only curative method [2]. For patients with RCC greater than 7 cm, partial nephrectomy (PN) and radical nephrectomy (RN) have comparable oncologic results for localized tumors (T2a). However, if the RENAL score is more than 10 at stage T2, there is an increased risk of recurrence and a decreased overall cancer-specific survival rate [3]. Partial nephrectomy (PN) or nephron-sparing surgery (NSS) is preferable over radical nephrectomy (RN) for treating localized cT1 carcinomas due to the better oncological and quality-of-life outcomes [4, 5]. It is the procedure of choice according to the American Urological Association and the European Association of Urology [6, 7], and when feasible, this indication extends to cover all renal malignancies [8]. In addition, NSS is more effective in treating advanced stages of cancer (T2) than radical nephrectomy and results in better renal function [9, 10].
Open partial nephrectomy (OPN) is the preferred method. However, laparoscopic partial nephrectomy (LPN) has become more common in NSS due to advancements in video technology, laparoscopic instrumentation design, and the availability of hemosealant substances [8].
The only limitation of LPN is the surgeon's lack of experience [11, 12]. Therefore, for difficult malignancies (hilar tumors, apical tumors, VonHippel-Lindau syndrome, mass in horseshoe kidney, and mass in ectopic pelvic kidneys) and critical indications (bilateral tumors, chronic kidney disease (CKD) stage 1 or 2, and solitary kidney), there is still debate about whether LPN is preferable in terms of short- and long-term outcomes.
Earlier research indicated that LPN was more prone to complications and required longer operating time than OPN. However, more recent reports conclude no differences between the two methods [13, 14]. Additionally, compared to OPN, several studies have shown that LPN was linked to fewer complications and shorter periods of ischemia and hospital stay [11, 15].
Based on these previous studies, we conducted this prospective randomized clinical trial to analyze the differences between LPN and OPN in surgical, functional, and oncological outcomes.
2 Methods
Between January 2019 and January 2022, this prospective, randomized study was conducted on 166 patients of both sexes with renal masses of less than 10 cm. The inclusion criteria were patients who were planned to be treated with PN and had an exophytic renal mass (T1a, T1b, and T2a) less than 10 cm in a single kidney, a CDK stage I or II, or bilateral renal mass with functioning contralateral kidney. Patients with metastatic or locally advanced tumors, renal vein thrombosis, renal mass over 10 cm, central or hilar tumors, uncorrected coagulopathy, and those unfit for anesthesia (ASA score ≥ 3) were excluded. Patients were randomized using the closed envelope method into 83 LPN and 83 OPN (Fig. 1).
To assess the clinical stage of the renal tumor and R.E.N.A.L score system, the patients underwent pelvi-abdominal U/S, multiphasic CT abdomen and pelvis with contrast, or MRIif the patient had elevated kidney function (creatinine > 1.5 gm. /dl). Patients were followed up for one year. R.E.N.A.L score system was used to classify the tumors. Components are: (R) diameter of the mass; (E) exophytic vs. endophytic properties; (N) nearness to the collecting system; (A) anterior or posterior; and (L) location relative to polar lines. Lesions with a nephrometry score of 4–6 points were designated as low complexity, 7–9 as moderate complexity, and 10–12 as the highest complexity lesions [1].
The current research followed the Declaration of Helsinki for studies involving humans, and the study was approved by the faculty Ethical Committee (ID: RC8.11.2022). All participants provided written informed consent before participation.
2.1 LPN procedure
The details of the operative technique were previously outlined in the literature [16]. Operations were performed under general anesthesia. Patients were positioned in a modified lateral kidney posture. Pneumoperitoneum was initiated using the Veress needle technique and trocar placement. Dissection to the renal hilum was done for good and sufficient exposure of the renal vessels.
Good exposure of the tumor and marking of the excision site were done with electrocautery. Clamping of renal vessels was achieved using laparoscopic Bulldog appliers. A visual assessment was performed during renal mass excision to determine the suitable depth of normal parenchyma to be excised to achieve a negative surgical margin. If an accidental collecting system injury was encountered, repair with suture calyceorrhaphy was done before bed hemostasis, and bipolar coagulation was cautiously applied away from the sutures (Fig. 2-A).
Large vessels were sutured with Vicryl 4/0 and secured with Weck hem-o-lok clips to achieve safe and stable hemostasis (Fig. 2-B). Unclamping and re-assessment of the hemostasis were done to secure residual bleeding points. Approximation of the edges of renal parenchyma was made using suturing in both groups. The sample was taken out using a Pfannenstiel incision after being placed in an EndoCatch bag. Surgical drain was placed in the paracolic gutter.
2.2 OPN procedure
General anesthesia was induced, and then an extraperitoneal flank trans-costal incision (11th rib) was made in each case to acquire access for surgery. Kidney dissection until the pedicle was done with selective artery and vein separation. The fat surrounding the kidney was removed, except for the fat attached to the tumor, and the kidney was then closely examined for any potential satellite lesions. Hot ischemia was applied to all cases using a Bulldog or Satiniski clamp to constrict the vein and artery. Then, the tumor was resected with about five millimeters of renal parenchyma as a surgical margin.
Small blood vessels were coagulated, while 4/0 polyglycolic acid was used to oversew large blood vessels, providing the necessary hemostasis against parenchymal hemorrhage. In addition, hemostatic agents such as gel foam were used. With 4/0 polyglycolic acid, the calyces and renal pelvis were rebuilt following their opening. The renal fibrous capsule of the kidney was closed without using parenchymal sutures to avoid damage or tear unless the defect was too extensive. Good intraoperative hydration was ensured. Furosemide and 20% mannitol (1 ml/kg) were given before renal ischemia to reduce damage and reperfusion injury.
We prospectively gathered general characteristics for each subject, including age, sex, smoking status, BMI, baseline HB, baseline GFR, baseline creatinine, American Society of Anaesthesiologists (ASA) score, and comorbidities. Clinical condition characteristics included laterality, complaint, renal score, clinical stage, Fuhrman grade, pathology, and complications. Operative findings included hospital stay, operative time, warm ischemia time, and estimated blood loss. Postoperative data included postoperative GFR, PADUA score, visual analog pain score, stenting, blood transfusion, functional outcomes, such as changes in GFR and creatinine level, and oncological outcomes, such as positive surgical margin. All patients' medical and surgical problems and operating notes were compiled. The day before surgery, the Padua score was assigned. Preoperative aspects and dimensions used for an anatomical (PADUA) renal masses score of 6–7, 8–9, and 10–14 were deemed low, moderate, and high complexity lesions, respectively [17]. The Clavien-Dindo classification was employed to record postoperative complications prospectively [18].
Transfusion was typically performed when a patient's hemoglobin level was below 8 g/dL in a healthy person or below 9 g/dL in a patient with ischemic heart disease.
The primary outcome was the hospital stay between the studied groups. Secondary outcomes were operative time, warm ischemia time, estimated blood loss, PADUA score, visual analog pain score, stenting, blood transfusion, changes in GFR and creatinine, and positive surgical margin.
2.3 Sample size calculation
The sample size was calculated using G*power software version 3.1.9.2 based on an expected effect size of hospital stay between the studied groups (d = 0.6) [19], with alpha and power adjusted at 0.05 and 0.8, respectively. The minimum number of patients to be recruited was 90 patients (45 per group). The sample size was increased to 120 patients (60 per group) to compensate for the expected loss of follow-up and the possible use of nonparametric tests.
2.4 Statistical analysis
SPSS 28.0 for Windows was used to analyze the data (SPSS Inc., USA). The Kolmogorov–Smirnov test, which assumes normality at P > 0.05, was used to determine whether the distribution of the variables under analysis was normal. The per-protocol approach was used for analysis. For parametric data, the information was summarized using the mean and standard deviation (SD). For nonparametric data, medians and interquartile ranges (IQR) were used. For qualitative data, numbers and percentages were used. Comparisons between laparoscopic and open surgery groups at baseline and follow-up were done using the student t test for parametric data and the Mann–Whitney test for nonparametric data. The Chi-square test was utilized for qualitative data. The acceptable significance level in this study was P < 0.05.
3 Results
The LPN and OPN patients were comparable regarding the baseline characteristics, including age, gender, BMI, Hb, GFR, creatinine, ASA score, and comorbidities, such as hypertension and diabetes mellitus (Table 1).
Additionally, the two groups were comparable regarding clinical characteristics, including laterality, complaint, RENAL score, Fuhrman grade, specimen pathology, and Calvien grade. Regarding the clinical stage, T1a and T1b were higher in the LPN group than in the OPN group (36.7% vs. 30.7% and 63.3% vs. 54.7%, respectively) (Table 2).
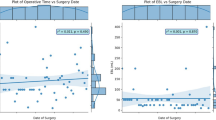
Regarding surgical outcomes, hospital stay and estimated blood loss were significantly lower in the LPN group than in the OPN group. In contrast, operative time was significantly longer in the LPN group than in the OPN group (P < 0.001). Warm ischemic time was comparable in both groups (P = 0.349). PADUA score, pain score, 6-h pain score (Fig. 3), and blood transfusion were significantly lower in the LPN group than in the OPN group (P = 0.028). Postoperative stenting was comparable between the two groups (P = 1.0) (Table 3, 4).
Regarding functional outcomes, postoperative GFR was significantly lower in the LPN group than in the OPN group (P < 0.001) (Table 4). Regarding oncological outcomes, positive surgical margins were comparable between the two groups (P = 0.143) (Table 4).
4 Discussion
Approximately 13–27% of abdominal examinations reveal a renal lesion because of the extensive use of abdominal imaging, which increases renal mass detection [20]. According to worldwide recommendations, PN or NSS is the gold standard for treating localized renal masses whenever possible [21]. Open surgery served as the best and only treatment option for PN for a very long time. However, LPN has recently become more popular because it lessens the invasiveness of open surgery.
Our results revealed that patients in the LPN and OPN groups were comparable in the baseline general and clinical characteristics. A significant difference was observed in the clinical stage; T1a and T1b were higher in the LPN group than in the OPN group (36.7% vs. 30.7% and 63.3% vs. 54.7%, respectively).
In contrast, all patients with clinical stage T2a (eleven patients) underwent OPN. Their tumor characteristics were T2a, Bosniak4,5 and exophytic. So we counseled these patients about renal exploration for partial nephrectomy and the possibility of radical nephrectomy. Renal mass was dissected from the normal parenchyma via avascular plane along the fibrous pseudocapsule. We did a partial nephrectomy by enucleation to preserve more parenchyma during PN.
This study shows that open nephron-sparing surgery indications could be expanding beyond the 7 cm cutoff, and patients with large tumors who are potential candidates for open NSS should be highly selected and well informed of potential complication risks.
Three cases were converted to open due to continuous parenchymal bleeding, unsatisfactory bleeding control after laparoscopic bulldog removal, obscured visual field, and the inability of hot ischemia again.
Smaller masses might be removed laparoscopically based on the experience of the surgeon. However, open surgery is more technically straightforward and less likely to result in tumor rupture, particularly in large masses or with surgeons with less experience in laparoscopic surgery [22].
These results are comparable with Luciani et al. [20], who documented that all patients with high tumor stage underwent OPN. Additionally, Gong et al. [23] documented that the mean tumor size was lower in the laparoscopic cohort.
The current study results indicated that hospital stay and estimated blood losses were significantly lower in the LPN group compared to the OPN group. These results are explained by the following: (a) Laparoscopic proficiency as a result of accumulated knowledge and technical advancements; (b) Laparoscopic magnification allows for precise renal artery dissection and repair of the damaged collecting system; (c) Continuous suturing and the use of Hemo-lok to clamp the suture rather than the standard ligature on the surface of the kidney.
Operative time was significantly longer in the LPN group than in the OPN group, while warm ischemia time was insignificantly different between the two techniques. These findings are comparable with Liu et al. [24] and Luciani et al. [21], who reported shorter hospital stay and less blood loss in the LPN than in the OPN. However, shorter operative time was observed in these studies [21, 24]. Different surgeons' experiences may be a suitable explanation for the longer operative time obtained in our study, as LPN is a technique that has a learning curve. The pooled results of a systematic review and meta-analysis demonstrated the same findings regarding hospitalization and blood loss [1]. Another study reported shorter surgical time, lower operative blood loss, and a shorter hospital stay [25].
Other studies have shown no differences between OPN and LPN [26, 27]. Moreover, shorter ischemia time was reported for LPN [11, 15]. However, these results may be deceptive, given the lack of precise tumor features. Young et al. [28] reported an operative time of 145.3 min in LPN compared to 155.2 min in the OPN and a blood loss of 123 ml in the LPN compared to 135 ml in the OPN.
Our results demonstrated significantly lower PADUA score, pain score, and blood transfusion in the LPN group compared to the OPN group. Additionally, significantly lower postoperative GFR was reported. These findings align with Yu et al. [1], who stated that the LPN group had a significantly lower blood transfusion than the OPN approach. Also, Liu et al. [24] documented that 3-month GFR was significantly lower in the LPN group than in the OPN group. However, Luciani et al. [21] reported an insignificant difference in PADUA score between the OPN and the LPN groups. Furthermore, Hager et al. [29] studied laparoscopic access and demonstrated a lower pain score at rest and movement.
The analysis of oncological outcomes indicated that positive surgical margins (PSM) were comparable between the two groups (P > 0.05). In contrast, Chengyu et al. [30] revealed a higher PSM in the LPN group. However, their subgroup analysis agrees with our results, showing no significant differences in PSM between the two groups for the T1a stage.
Despite being level-1 evidence, this study has some limitations, including being a single-center study. Additionally, using the per-protocol analysis approach could limit the extent to which the findings can be generalized. All patients with T2a clinical stage underwent OPN. Despite these limitations, this study shows that open nephron-sparing surgery indications could be expanding beyond the 7 cm cutoff, and patients with large tumors who are potential candidates for open NSS should be highly selected and well informed of potential complications. Further studies are needed to compare OPN versus LPN in T2 tumors. Furthermore, the study did not compare the postoperative quality of life and cost between both techniques.
5 Conclusions
Oncological and functional results were comparable between LPN and OPN; however, LPN was superior to open surgery regarding hospital stay, visual analog pain score, and blood loss.
Availability of data and materials
The datasets used and analyzed for the current work are available upon reasonable request from the corresponding author.
Abbreviations
- ASA:
-
American Society of Anaesthesiologists
- CT:
-
Computerized tomography
- E-GFR:
-
Estimated GFR
- GFR:
-
Glomerular filtration rate
- HS:
-
Highly significant
- IQR:
-
Interquartile ranges
- LPN:
-
Laparoscopic partial nephrectomy
- NSS:
-
Nephron-sparing surgery
- OPN:
-
Open partial nephrectomy
- PN:
-
Partial nephrectomy
- RCC:
-
Renal cell carcinoma
- RN:
-
Radical nephrectomy
- SD:
-
Standard deviation
References
Yu Y, Wang W, Xiong Z, Yang Z, Li J, Shen Y et al (2021) Comparison of perioperative outcomes between laparoscopic and open partial nephrectomy for different complexity renal cell carcinoma based on the R.E.N.A.L. nephrometry score. Cancer Manag Res 13:7455–7461
Zhang Y, Ellinger J, Ritter M, Schmidt-Wolf IGH (2020) Clinical studies applying cytokine-induced killer cells for the treatment of renal cell carcinoma. Cancers (Basel) 12(9):2471
Simone G, Tuderti G, Anceschi U, Papalia R, Ferriero M, Misuraca L et al (2017) Oncological outcomes of minimally invasive partial versus minimally invasive radical nephrectomy for cT1-2/N0/M0 clear cell renal cell carcinoma: a propensity score-matched analysis. World J Urol 35(5):789–794
Koo KC, Kim JC, Cho KS, Choi YD, Hong SJ, Yang SC et al (2016) Oncological outcomes after partial vs radical nephrectomy in renal cell carcinomas of ≤7 cm with presumed renal sinus fat invasion on preoperative imaging. BJU Int 117(1):87–93
Suo X, Chen J, Zhao Y, Tang Q, Yang X, Yuan Y et al (2021) Clinicopathological and radiological significance of the collateral vessels of renal cell carcinoma on preoperative computed tomography. Sci Rep 11(1):5187
Ebbing J, Menzel F, Frumento P, Miller K, Ralla B, Fuller TF et al (2019) Outcome of kidney function after ischaemic and zero-ischaemic laparoscopic and open nephron-sparing surgery for renal cell cancer. BMC Nephrol 20(1):40
Mina-Riascos SH, Vitagliano G, García-Perdomo HA (2020) Effectiveness and safety of partial nephrectomy-no ischemia vs. warm ischemia: Systematic review and meta-analysis. Investig Clin Urol 61(5):464–474
Abdelhafez M, Bastian A, Rausch S, Stenzl A, Bedke J, Kruck S (2017) Laparoscopic versus open partial nephrectomy: comparison of overall and subgroup outcomes. Anticancer Res 37(1):261–265
Becker F, Roos FC, Janssen M, Brenner W, Hampel C, Siemer S et al (2011) Short-term functional and oncologic outcomes of nephron-sparing surgery for renal tumours ≥ 7 cm. Eur Urol 59(6):931–937
Simmons MN, Weight CJ, Gill IS (2009) Laparoscopic radical versus partial nephrectomy for tumors >4 cm: intermediate-term oncologic and functional outcomes. Urology 73(5):1077–1082
Marszalek M, Meixl H, Polajnar M, Rauchenwald M, Jeschke K, Madersbacher S (2009) Laparoscopic and open partial nephrectomy: a matched-pair comparison of 200 patients. Eur Urol 55(5):1171–1178
Schwentner C, Alloussi SH, Radmayr C, Colleselli D, Schilling D, Sievert K-D et al (2009) Contemporary minimal-invasive nephron-sparing surgery. Cent Eur J Urol 62(4)
Gill IS, Matin SF, Desai MM, Kaouk JH, Steinberg A, Mascha E et al (2003) Comparative analysis of laparoscopic versus open partial nephrectomy for renal tumors in 200 patients. J Urol 170(1):64–68
Becker A, Pradel L, Kluth L, Schmid M, Eichelberg C, Ahyai S et al (2015) Laparoscopic versus open partial nephrectomy for clinical T1 renal masses: no impact of surgical approach on perioperative complications and long-term postoperative quality of life. World J Urol 33(3):421–426
Sun M, Abdollah F, Shariat SF, Schmitges J, Trinh QD, Tian Z et al (2012) Propensity-score matched comparison of complications, blood transfusions, length of stay, and in-hospital mortality between open and laparoscopic partial nephrectomy: a national series. Eur J Surg Oncol 38(1):80–87
Aron M, Gill IS (2007) Minimally invasive nephron-sparing surgery (MINSS) for renal tumours part I: laparoscopic partial nephrectomy. Eur Urol 51(2):337–346 (discussion 46–7)
Ficarra V, Novara G, Secco S, Macchi V, Porzionato A, De Caro R et al (2009) Preoperative aspects and dimensions used for an anatomical (PADUA) classification of renal tumours in patients who are candidates for nephron-sparing surgery. Eur Urol 56(5):786–793
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Klaassen Z, Kohut RM, Patel D, Terris MK, Madi R (2014) A single surgeon’s experience with open, laparoscopic, and robotic partial nephrectomy. Int Scholarly Res Notices 2014:430914
Gill IS, Aron M, Gervais DA, Jewett MA (2010) Clinical practice. Small renal mass. N Engl J Med 362(7):624–634
Luciani LG, Chiodini S, Mattevi D, Cai T, Puglisi M, Mantovani W et al (2017) Robotic-assisted partial nephrectomy provides better operative outcomes as compared to the laparoscopic and open approaches: results from a prospective cohort study. J Robot Surg 11(3):333–339
Angst E, Hiatt JR, Gloor B, Reber HA, Hines OJ (2010) Laparoscopic surgery for cancer: a systematic review and a way forward. J Am Coll Surg 211(3):412–423
Gong EM, Orvieto MA, Zorn KC, Lucioni A, Steinberg GD, Shalhav AL (2008) Comparison of laparoscopic and open partial nephrectomy in clinical T1a renal tumors. J Endourol 22(5):953–957
Liu Z, Wang P, Xia D, Lou YF, Pan HF, Wang S (2013) Comparison between laparoscopic and open partial nephrectomy: surgical, oncologic, and functional outcomes. Kaohsiung J Med Sci 29(11):624–628
Gill IS, Kavoussi LR, Lane BR, Blute ML, Babineau D, Colombo JR Jr et al (2007) Comparison of 1,800 laparoscopic and open partial nephrectomies for single renal tumors. J Urol 178(1):41–46
Breda A, Finelli A, Janetschek G, Porpiglia F, Montorsi F (2009) Complications of laparoscopic surgery for renal masses: prevention, management, and comparison with the open experience. Eur Urol 55(4):836–850
Sprenkle PC, Power N, Ghoneim T, Touijer KA, Dalbagni G, Russo P et al (2012) Comparison of open and minimally invasive partial nephrectomy for renal tumors 4–7 centimeters. Eur Urol 61(3):593–599
Yu Y, Wang W, Xiong Z, Yang Z, Li J, Shen Y, Gu B (2021) Comparison of perioperative outcomes between laparoscopic and open partial nephrectomy for different complexity renal cell carcinoma based on the R.E.N.A.L. nephrometry score. Cancer Manag Res 13:7455–7461. https://doi.org/10.2147/CMAR.S324457
Hager B, Herzog SA, Hager B, Sandner-Kiesling A, Zigeuner R, Pummer K (2019) Comparison of early postoperative pain after partial tumour nephrectomy by flank, transabdominal or laparoscopic access. Br J Pain 13(3):177–184
You C, Yuelin Du, Wang H, Peng L, Wei T et al (2020) Laparoscopic versus open partial nephrectomy: a systemic review and meta-analysis of surgical, oncological and functional outcomes. Front Oncol 10:583979
Acknowledgements
None.
Funding
There are none to be declared.
Author information
Authors and Affiliations
Contributions
BE: design of the work, interpretation of data, the acquisition, analysis, original draft, substantively revised manuscript. RG: interpretation of data, methodology, TG: data collection, methodology, interpretation of data. MM: data collection, manuscript writing. IS: supervision, data analysis, manuscript review. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Benha Faculty of Medicine (ID: RC8112022). And the Declarations of Helsinki guidelines were followed. All patients gave written consent before participation.
Consent for publication
Not applicable.
Competing interests
No interest conflicts declared.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Elmohamady, B.N., Goma, R., Gharib, T. et al. Laparoscopic versus open partial nephrectomy: prospective randomized study for assessment of surgical, functional, and oncological outcomes. Afr J Urol 29, 64 (2023). https://doi.org/10.1186/s12301-023-00397-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-023-00397-9