Abstract
Background
Nephron-sparing surgery (NSS) remains gold standard for the treatment of localised renal cell cancer (RCC), even in case of a normal contralateral kidney. Compared to radical nephrectomy, kidney failure and cardiovascular events are less frequent with NSS. However, the effects of different surgical approaches and of zero ischaemia on the postoperative reduction in renal function remain controversial.
We aimed to investigate the relative short- and long-term changes in estimated glomerular filtration rate (eGFR) after ischaemic or zero-ischaemic open (ONSS) and laparoscopic NSS (LNSS) for RCC, and to analyse prognostic factors for postoperative acute kidney injury (AKI) and chronic kidney disease (CKD) stage ≥3.
Methods
Data of 444 patients (211 LNSS, 233 ONSS), including 57 zero-ischaemic cases, were retrospectively analysed. Multiple regression models were used to predict relative changes in renal function. Natural cubic splines were used to demonstrate the association between ischaemia time (IT) and relative changes in renal function.
Results
IT was identified as significant risk factor for short-term relative changes in eGFR (ß = − 0.27) and development of AKI (OR, 1.02), but no effect was found on long-term relative changes in eGFR. Natural cubic splines revealed that IT had a greater effect on patients with baseline eGFR categories ≥G3 concerning short-term decrease in renal function and development of AKI. Unlike LNSS, ONSS was significantly associated with short-term decrease in renal function (ß = − 13.48) and development of AKI (OR, 3.87). Tumour diameter was associated with long-term decrease in renal function (ß = − 1.76), whereas baseline eGFR was a prognostic factor for both short- (ß = − 0.20) and long-term (ß = − 0.29) relative changes in eGFR and the development of CKD stage ≥3 (OR, 0.89).
Conclusions
IT is a significant risk factor for AKI. The short-term effect of IT is not always linear, and the impact also depends on baseline eGFR. Unlike LNSS, ONSS is associated with the development of AKI. Our findings are helpful for surgical planning, and suggest either the application of a clampless NSS technique or at least the shortest possible IT to reduce the risk of short-time impairment of the renal function, which might prevent AKI, particularly regarding patients with baseline eGFR category ≥G3.
Similar content being viewed by others
Background
The gold standard of care for managing renal cell cancer (RCC) remains surgical tumour excision [1, 2]. Currently, nephron-sparing surgery (NSS) is recommended for clinically localised tumours (cT1–2) by the European Association of Urology (EAU) and the American Urological Association (AUA) guidelines [1, 2]. Outside of specialised centres, the standard surgical procedure is open partial nephrectomy. However, an interest in the implementation of minimally invasive NSS has continuously increased [3, 4]. Several contemporary studies demonstrated oncological outcomes of patients undergoing laparoscopic NSS (LNSS) that were equivalent to those of patients undergoing open NSS (ONSS) [5,6,7].
Compared to radical nephrectomy, kidney failure and cardiovascular events are less frequent with NSS [2, 8,9,10,11,12]. However, whether NSS also improves overall survival remains controversial [11, 13,14,15,16,17,18,19,20]. Results from the only randomized trial of NSS versus radical nephrectomy (EORTC-30904), which included mainly patients with a normal baseline estimated glomerular filtration rate (eGRF) and a normal contralateral kidney, revealed that the impact of NSS on eGFR did not result in improved non-cancer related mortality and less cardiovascular events in general [11, 16, 17]. In contrast, other recent retrospective data showed that in patients who had chronic kidney disease (CKD) before surgery, lower postoperative eGFR was associated with increased mortality, independently of age and comorbidities [18], and that there is an increased risk of death from any cause or cardiovascular death with decreased postoperative renal function, but the latter study was not adjusted for the baseline renal function [19]. These results suggest that the surgery-related factors that influence the non-oncological outcome measures are much less important than internistic disorders such as diabetes, arterial hypertension, or medical CKD [11, 16, 18]. Just recently, a relationship between renal function and cancer-specific mortality was also debated [21]. However, several studies have shown a significantly increased risk of progression of renal failure, cardiovascular disease, and subsequent mortality in patients developing CKD [22,23,24], and approximately 16–40% of patients treated with NSS develop postoperative CKD stage ≥3 [25, 26], which is defined as an eGFR < 60 mL/min/1.73 m2 by the Kidney Disease: Improving Global Outcomes (KDIGO) criteria of kidney disease [27].
Reductions in renal function mainly related to renal parenchymal mass loss, renal ischaemia, and reduced baseline kidney function are seen in NSS patients, but the effects of different surgical approaches (e.g., ONSS and LNSS), and of zero ischaemia (ZI) in this aspect remain controversial. Due to the known oncological equivalence of LNSS versus ONSS for localised RCC, many are interested in understanding surgery-related factors influencing non-oncological outcome measures.
Therefore, the purpose of this work was to demonstrate the dynamics of renal function after NSS, to identify risk factors for the development of acute kidney injury (AKI) and CKD stage ≥3 after NSS, and to compare the effects of ONSS and LNSS for RCC as well as ZI (no renal clamping during surgery) on postoperative renal function.
Methods
We used our prospectively populated database and archive to retrospectively identify 444 patients who were treated with NSS for RCC at the Department of Urology of the Charité–University Hospital between 1999 and 2010. A total of 211 patients were treated with LNSS and 233 patients were treated with ONSS. Exclusion criteria were metastatic RCC, recurrent RCC, bilateral RCC, and preoperative end-stage chronic kidney disease (CKD stage 5/kidney failure). Furthermore, angiomyolipoma, oncocytoma, and other non-malignant tumours were not included in order to limit this series to only pure primary RCC patients.
This study was approved by the local ethics committee of the Charité–University Hospital Berlin. Data collection was performed in accordance with the requirements of the local ethics committee. All patients provided written informed consent.
Patient demographics, tumour characteristics, surgical characteristics, and preoperative and postoperative renal function were obtained.
Warm renal ischaemia was performed according to the surgeon’s decision. Arterial vessel clamping for hilar control was performed using bulldog clips for LNSS and Satinsky clamps or vessel loops (tourniquets) for ONSS. Tumour resection, management of the tumour ground, and renal parenchyma/collecting system reconstruction were similarly performed during LNSS and ONSS. Tumours were resected or enucleated whenever possible using standard diathermy resection techniques. Large vessels were oversewn with absorbable sutures or controlled with titanium ligating clips. The renal parenchyma defect was closed using an absorbable hemostat patch fixed by gathering sutures of the parenchyma or by using a hemostatic matrix. An injured urinary collection system was sutured and a ureteral stent was inserted when indicated at the surgeon’s discretion.
To monitor renal function, baseline serum creatinine was measured preoperatively (time 0), during the hospitalisation course (times A and B), and during variable postoperative follow-up times (times C, D, and E) according to oncological follow-up investigations. Data were retrospectively collected for the highest serum creatinine value during the planned hospital stay (time A), serum creatinine prior to discharge from hospital (time B), approximately 6 weeks (time C) and 12 months (time D) after surgery, and at the latest recorded follow-up time (time E). The median measurement time was 1 day (interquartile range [IQR], 1–2) postoperatively for time A, 4 days (IQR, 2–6) postoperatively for time B, 47 days (IQR, 30–105) postoperatively for time C, 13 months (IQR, 12–15) postoperatively for time D, and 50 months (IQR, 35–81) postoperatively for time E. Glomerular filtration rate (GFR) was estimated based on the Modification of Diet in Renal Disease (MDRD) formula [28]. Estimated GFR (eGFR) was calculated to investigate the absolute and relative (%) changes in renal function between time 0 and postoperative times A–E in the overall NSS cohort (NSS-C) and in the following subgroups: NSS group with intraoperative renal ischaemia (NSS-RI), NSS group without intraoperative renal ischaemia (NSS-NRI), LNSS group with intraoperative renal ischaemia (LNSS-RI), ONSS group with intraoperative renal ischaemia (ONSS-RI), NSS group with development of postoperative AKI (NSS-AKI), NSS group without development of postoperative AKI (NSS-NAKI), NSS group with baseline eGFR category G1 (NSS-G1), NSS group with baseline eGFR category G2 (NSS-G2), and NSS group with baseline eGFR category ≥G3 (NSS ≥ G3).
Kidney function was staged based on eGFR categories G1–G5 according to the Kidney Disease: Improving Global Outcomes (KDIGO) criteria [27] at baseline and all follow-up times. CKD stage ≥3 was defined by eGFR < 60 mL/min/1.73 m2 (eGFR category ≥G3) independent of markers of renal damage [27]. An increase in serum creatinine levels of at least ≥50% or ≥ 0.3 mg/dL within 48 h postoperatively was considered AKI [29].
Statistical analyses were completed using SPSS Statistics version 23.0 (IBM Corp., Armonk, NY, USA) and R (http://www.r-project.org). Continuous variables were summarised by medians with IQR, whereas sample proportions were used to describe categorical and binary outcomes. To compare distributions, we used the Mann-Whitney U test (2 groups) or Kruskal-Wallis test (more than 2 groups) for continuous responses; we used Pearson’s chi-squared test for categorical responses. Friedman’s test was used to assess absolute and relative (%) changes in eGFR over time (measurement times A–E vs. baseline).
We used multiple linear and logistic regression models to predict the short-term relative changes in eGFR from baseline at time A (model 1) and the long-term relative changes in time D (model 2), and to identify predictors of AKI (model 3) and CKD stage ≥3 (eGFR < 60 mL/min/1.73 m2) at time D (model 4). We implemented two different versions of each model: (a) one including ischaemia time (IT) linearly, and (b) one using categorical variables (ZI vs. ischaemia in general or 21–30 min of ischaemia [reference] vs. different ITs of 0 min [ZI], 1–10 min, 11–20 min, > 30 min) as well as the interaction between ZI and eGFR categories (G1 [reference] vs. G2 or vs. ≥G3).
Natural cubic splines were used to demonstrate the association between IT and relative change in eGFR at time A in model 1 and at time D in model 2 according to baseline eGFR categories G1, G2, and ≥ G3. The same approach was used to describe the association between IT and the probability of AKI and its interaction with baseline eGFR categories G1, G2, and ≥ G3 in model 3, and to describe the association between IT and the probability of new-onset CKD stage ≥3 at time D in model 4.
Due to missing data (26.6% for AKI, 9.9% for IT, and 54.3 and 47.3% for relative changes in eGFR from baseline at times D and E, respectively), regression models were based on the pooled estimates from 100 imputed datasets. We used the MICE package by R to implement multiple imputations by chained equations [30, 31]. All outcome and independent variables included in the subsequent analyses and additional variables that could provide useful information were used. A p-value < 0.05 was considered statistically significant.
Results
Epidemiological, oncological, and surgical characteristics of the treated patient cohort, subdivided into the LNSS approach group and ONSS approach group, are shown in Table 1. Statistically significant differences between the LNSS and ONSS groups were seen in terms of the preoperative haemoglobin level, tumour diameter, tumour stage, and baseline renal function. Baseline eGFR was higher for the LNSS-RI group compared to the ONSS-RI group (85.5 [IQR, 72.1–96.2] vs. 75.4 [IQR, 61.5–90.2] mL/min; p = 0.03), but did not differ between the NSS-RI group and NSS-NRI group (79.5 [IQR, 66.3–93.9] vs. 80.4 [IQR, 59.4–91.1] mL/min; p = 0.36). In the NSS-C group, 18.5% of patients had eGFR category ≥G3 at the time of surgery. Hence, the proportion of patients with eGFR category ≥G3 was 13.7% in the LNSS cohort and 22.7% in the ONSS cohort (p = 0.01) at baseline. This distribution was similar for subgroups LNSS-RI and ONSS-RI, with 11.9 and 22.8% (p = 0.001) having eGFR category ≥G3 at the time of surgery, respectively. There was an insignificantly higher rate of patients with eGFR category ≥G3 in the NSS-NRI group compared to the NSS-RI group (24.6% vs. 16.9%; p = 0.17).
The median tumour diameter was 0.8 cm smaller for the LNSS group compared to the ONSS group (p < 0.001) and was 0.5 cm smaller for the NSS-NRI group compared to the NSS-RI group (2.7 [IQR 2.0–3.5] vs. 3.2 [IQR 2.2–4.0] cm; p = 0.04). Operative time was 45 min longer (p < 0.001) and IT was 2 min shorter (p = 0.04) for the LNSS group. The ischaemia rate was 87.8% for the LNSS group and 67.8% for the ONSS group (p < 0.001). In total, 57 patients (12.8%) underwent ZI surgery; 38.5% of the patients in the NSS-C group developed AKI postoperatively as follows: stage 1, 33.9%; stage 2, 4.3%; and stage 3, 0.3%. Significant differences were observed for the surgical approach, baseline eGFR categories, and IT (Table 2a). AKI stages 1, 2, and 3 were detected in 40.2, 7.5, and 0.9% of patients in the ONSS cohort and in 28.3, 2.0, and 0.0% of patients in the LNSS cohort, respectively (p = 0.001).
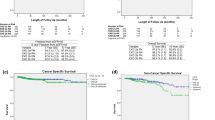
Table 3 and Fig. 1a-j show the absolute and relative (%) changes in eGFR from baseline at postoperative measurement times A-E in the NSS-C group (Fig. 1a/b) and subgroups according to the application of ischaemia (Fig. 1c/d), surgical approach (Fig. 1e/f), and occurrence of postoperative AKI (Fig. 1g/h), and according to baseline renal function (Fig. 1i/j). The highest relative renal function reduction was seen at a median of 1 day postoperatively (IQR, 1–2) (time A) in the NSS-C group and in all subgroups; all compared subgroups showed significantly different eGFR reductions at time A. No statistically significant difference between the compared subgroups was seen at a median of 13 months postoperatively (IQR, 12–15) (time D) and at the last follow-up, which occurred at a median of 50 months postoperatively (IQR, 35–81) (time E). In contrast, the NSS-AKI group consistently showed significantly higher absolute and relative reductions of eGFR compared to the NSS-NAKI group at all postoperative measurement times (p < 0.001).
Box plots showing the postoperative course of the absolute (a/c/e/g/i) and relative (b/d/f/h/j) change (%) in eGFR at measurement times A-E for (a/b) the overall NSS cohort (NSS-C), (c/d) the NSS group with intraoperative renal ischaemia (NSS-RI) and without intraoperative renal ischaemia (NSS-NRI), (e/f) the LNSS group with intraoperative renal ischaemia (LNSS-RI), the ONSS group with intraoperative renal ischaemia (ONSS-RI), (g/h) the NSS group with postoperative AKI (NSS-AKI), the NSS group without postoperative AKI (NSS-NAKI), and (i/j) NSS group with a baseline eGFR category G1 (NSS-G1), NSS group with a baseline eGFR category G2 (NSS-G2), and NSS group with a baseline eGFR category ≥G3 (NSS ≥ G3). Definition of measurement times a-e: (a) highest change in eGFR from baseline during the planned hospital stay at a median of 1 day postoperatively (IQR, 1–2), (b) change in eGFR from baseline prior to discharge from hospital at a median of 4 days postoperatively (IQR, 2–6), (c) change in eGFR from baseline at a median of 47 days postoperatively (IQR, 30–105), (d) a median of 13 months postoperatively (IQR, 12–15), and (e) a median of 50 months postoperatively (IQR, 35–81). Asterisks indicate significant changes from baseline in the level of absolute and relative changes in eGFR over the course of the observation period (Friedman’s test as a post hoc pairwise multiple comparison test) or between the compared groups at each measurement time (non-parametric Mann-Whitney U test). * p < 0.05, ** p < 0.01, *** p < 0.001, (ns) not significant. eGFR, estimated glomerular filtration rate; NSS, nephron-sparing surgery; LNSS, laparoscopic nephron-sparing surgery; ONSS, open nephron-sparing surgery; AKI, acute kidney injury; IQR, interquartile range
Regarding the complete follow-up period, the rate of new-onset CKD stage ≥3 was + 27.9% for the NSS-C group. Table 2b summarises data for different subgroups.
Results of the multiple linear and logistic regression models investigating predictors for the postoperative short-term (model 1) and long-term (model 2) relative changes in renal function or postoperative development of AKI (model 3) and new-onset CKD stage ≥3 (model 4) are summarised in Table 3a-d.
In regression model 1 (Table 4a), baseline eGFR, ONSS, BMI, IT, major complications, and operative time were independent predictors of a greater short-term relative decrease in eGFR from baseline at time A (1 day postoperatively; IQR, 1–2 days). In regression model 2 (Table 4b), baseline eGFR, tumour diameter, and higher relative decrease of the eGFR at time A (outcome variable in model 1) were all significantly related to greater long-term relative decreases in eGFR at time D (13 months postoperatively; IQR, 12–15 months).
Risk factors for postoperative AKI within 48 h in model 3 (Table 4c) were ONSS, male sex, higher BMI, longer IT, and longer operative time.
Including only patients with preoperative eGFR category <G3, regression model 4 (Table 4d) showed that lower baseline eGFR was a significant risk factor for development of new-onset CKD stage ≥3 at time D.
In our regression analyses using IT as an independent categorical variable, renal ischaemia compared to ZI showed a significantly greater relative decrease in short-term renal function in model 1 (regression coefficient [ß], − 9.4; 95% CI, − 14.6 to − 4.2; p < 0.001); however, no differences were seen in models 2–4. In addition, depending on the baseline eGFR categories, ZI did not affect the development of postoperative AKI in a significantly different manner (data not shown).
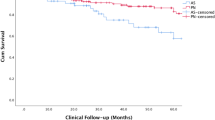
Therefore, we used the plot of natural cubic splines (Fig. 2) to estimate the correlation between IT and relative change in eGFR in models 1 and 2 (Fig. 2a and c) and to better demonstrate its interaction with baseline eGFR categories. Additionally, Fig. 2b and d similarly show the correlation between IT and the probability of postoperative AKI and CKD stage ≥3 in models 3 and 4. Based on the results of the regression analysis, some clear assertions can be made regarding the natural cubic splines, including that IT impacts the short-term relative change in eGFR and has greater effects on patients with baseline eGFR categories ≥G3, with the largest effect in this group occurring during the first 15 min of IT (Fig. 2a). The risk for development of AKI within 48 h postoperatively increases with increasing IT, but the effect of IT on AKI risk strongly depends on baseline renal function. Although eGFR category ≥G3 showed a steep increase in the risk for AKI during the first 20 min of ischaemia, the risk for AKI with G1 and, in particular, G2 visibly starts to increase only after 20 min of IT.
Plots of natural cubic splines including zero ischaemia to estimate the correlation between ischaemia time and (a) the relative (%) change in eGFR from baseline at time A (highest change in eGFR during the planned hospital stay prior to discharge (median, 1 day p.o.; IQR, 1–2) in model 1, (b) at time D (median, 13 months p.o.; IQR, 12–15) in model 2, (c) correlation between ischaemia time and the risk of AKI within 48 h p.o. in model 3 and its interaction with baseline renal function, respectively, and (d) correlation between ischaemia time and the risk of new-onset CKD stage ≥3 at time D. CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; p.o., postoperatively; IQR, interquartile range
Regarding long-term outcomes of NSS, renal function was not significantly affected by IT in any of the baseline eGFR categories; however, reduction in renal function appears to depend on baseline eGFR, with category G1 showing the smallest reduction (Fig. 2c). No strong correlation was seen between the rate of new-onset CKD stage ≥3 and IT (Fig. 2d).
Discussion
NSS offers similar oncological efficacy for localised RCC as radical nephrectomy and is the current gold standard for the treatment of small renal tumours, even in the presence of a normal contralateral kidney [1, 2]. Recently, the EAU guidelines have been expanded with regard to the recommendation for NSS to include cT2 tumours in selected cases [2]. Approximately 25% of patients with a kidney tumour, normal serum creatinine, and a normal contralateral kidney experience preoperative CKD stage ≥3 [22, 32]. These patients can benefit from the enhanced preservation of renal function after NSS relative to radical nephrectomy, thereby minimising the risk of CKD progression and improving overall survival rates [10, 12, 16, 20, 22, 23, 33]. However, patients treated with NSS have a 16–40% chance of postoperatively developing new-onset CKD stage ≥3 [25, 26]. Despite partial nephrectomy, approximately 90% of the global renal function in patients with bilateral kidneys, and 80% of the global renal function in patients with a solitary kidney are preserved [34]. Key features associated with long-term preservation of renal function include ischaemia type, the amount of healthy renal parenchyma preservation (quantity of nephrons saved), and baseline kidney function (quality of nephrons prior to surgery) [34,35,36,37,38,39,40]. Other debated factors related to postoperative renal function are the surgical approach, namely LNSS or ONSS [5, 25, 41, 42], ZI NSS, and the effect of IT [37, 43]. Our study aimed to identify risk factors for the development of AKI and CKD stage ≥3 following NSS. We compared the effects of ONSS and LNSS and the effects of IT and ZI on postoperative short- and long-term renal function in the treatment of RCC patients.
In our cohort of 211 LNSS and 233 ONSS patients (444 patients) with localised RCC, medians of 11.0% and 14.1% reductions in eGFR were detected at medians of 13 months postoperatively (IQR, 12–15) and 50 months postoperatively (IQR, 35–81), respectively. No statistically significant change in eGFR was seen from a median of 47 days postoperatively (IQR, 30–105) until the last follow-up (median, 50 months postoperatively; IQR, 35–81 months) in the overall cohort and in all investigated subgroups. This is in line with previously published data showing little increase in renal function from approximately 6 weeks after NSS [34, 42, 44, 45]. We could not substantiate a statistically significant difference in the relative reduction of renal function during long-term follow-up after NSS according to the surgical approach, application of intraoperative renal ischaemia or ZI, and IT. However, the NSS-NAKI group showed the lowest and the NSS-AKI group showed the highest renal function decrease during long-term follow-up. In our multiple regression model, AKI was not a significant predictor for the relative long-term change in renal function. The main factors of the regression model that predicted renal function at a median of 13 months postoperatively (IQR, 12–15) were baseline eGFR, short-term relative change in renal function at a median of 1 day postoperatively (IQR, 1–2), and tumour diameter. Furthermore, the LNSS group, ZI group, and patients with better baseline kidney function had significantly lower relative reductions in renal function immediately postoperatively. This was consistently reflected in our regression model showing that ONSS, lower baseline eGFR, longer IT, higher BMI, longer operative time, and severe postoperative complications were risk factors for a relative decrease in renal function immediately postoperatively.
Effects of the surgical approach on postoperative renal function are inconsistently described in the literature. Adamy et al. also used the MDRD formula to estimate GFR and showed a more pronounced initial postoperative decrease in renal function with ONSS and slightly but significantly better recovery of the renal function with LNSS [42]. Funahashi et al. also detected a greater decrease in renal function after ONSS [46]. Just recently, Antonelli et al. described a bigger risk for a greater than 25% immediate impaired renal function after ONSS and LNSS when compared to robot-assisted laparoscopic partial nephrectomy with ONSS, showing a bigger odds ratio than LNSS (5.26, p < 0.001 vs. 2.86, p = 0.004) [24]. However, other human and animal studies were unable to find differences in postoperative renal function after various surgical approaches [6, 39, 47,48,49]. In contrast, Marszalek et al. showed an 11-fold higher decrease in eGFR 24 h after LNSS compared to ONSS with renal clamping; a similar renal function decrease was found after 3.6 years (− 10.6% vs. -10.9%; p = 0.7). However, tumour diameters were equal with LNSS and ONSS, and IT was longer with ONSS in their study. The authors explained their results with evidence of direct and indirect (e.g., renal blood flow) negative impacts of the capnoperitoneum [5, 50]. In contrast, animal experiments have provided indirect evidence suggesting that transient ischaemic preconditioning caused by pneumoperitoneum could limit renal ischaemia/reperfusion injury in laparoscopic surgery [51, 52], potentially indicating a more protective effect with LNSS. However, there was a smaller short-term decrease in renal function in LNSS compared to ONSS in the ZI group (− 9.0 [IQR -23.1 to 4.9] vs. -20.5 [IQR -34.5 to 2.4] %); this difference was not significant (p = 0.21).
In our study, the AKI rate was 38.5%, which is similar to previously published data [53]; However, AKI rates after NSS vary between 18 and 54% depending on AKI criteria applied and conditions with solitary or bilateral kidneys [12, 39, 48, 49, 54]. ONSS and male sex were the main risk factors for AKI according to our multiple regression model. There is evidence that longer IT and operative time are risk factors for postoperative AKI after NSS [39, 48, 49, 53], which was confirmed by our data. In our study, every minute of surgery increased the risk of AKI significantly by 1.0%, and every minute of ischaemia increased the risk by 2.0%. In our multiple regression analysis, ZI was significantly associated with a reduced short-term decrease of renal function, but this did not result in a significantly lower risk of AKI (p = 0.4).
Additionally, Rajan et al. previously showed that lower baseline eGFR increases the risk for AKI after NSS [53]. In our study, AKI rates were 1.7-fold and 2.4-fold higher in the baseline eGFR categories G2 and ≥ G3 compared to G1, but the baseline renal function was not found to be an independent predictor of AKI in our multiple regression model. Studies by Zhang et al. also failed to identify baseline renal function to be a risk factor for postoperative AKI after NSS [39, 49]. In contrast, our plots of natural cubic splines uniquely illustrated the association between IT and AKI risk with different effects depending on baseline renal function. These findings indicate that patients with baseline eGFR < 60 mL/min/1.73 m2 are at higher risk for AKI after NSS if renal ischaemia is applied.
Recently, Zhang et al. published a cohort study of 83 patients with solitary kidneys and showed that parenchymal mass reduction and IT are risk factors for postoperative AKI. Adjusting for parenchymal mass reduction, AKI was associated with 5–12% worse functional recovery depending on the AKI stage [39]. This is comparable to our results, although we could not identify AKI as a significant risk factor for long-term decreases in renal function after NSS. In our regression model, which was adjusted for tumour diameter as a surrogate parameter for removed renal parenchyma, we predicted a 0.2% relative reduction of eGFR at a median of 13 months postoperatively (IQR, 12–15) for every percentage of relative decrease of eGFR at a median of 1 day (IQR, 1–2) after NSS.
We detected a rate of new-onset CKD stage ≥3 of 27.9% in the overall cohort (NSS-C) until the latest recorded follow-up time. Our multiple regression model showed that baseline eGFR was the only significant predictor for CKD stage ≥3 at a median of 13 months (IQR, 12–15) after NSS, with an increasing risk of 11.0% for every baseline eGFR unit smaller. IT, ZI, AKI, or one of the two surgical approaches (LNSS-RI vs. ONSS-RI) were not significant prognostic factors for new-onset CKD stage ≥3.
The 27.9% rate of de novo CKD stage ≥3 in our study was comparable to previous data [25, 55, 56]. Clark et al. observed a postoperative rate of CKD stage ≥3 of 29.0% [55]. Muramaki et al. observed a rate of 39.4% [25], with no difference between LNSS and ONSS. Regression analysis predicting CKD-free survival or CKD development were not completely conformable, although both studies identified increasing age and lower baseline kidney function, but not IT, as independent risk factors. This was just recently confirmed by Lee et al. who showed that even prolonged warm IT was not associated with increased incidence of CKD [57]. However, the effect of ZI was not addressed in these studies.
Our study should be interpreted with consideration of its limitations. Retrospective data collection led to missing follow-up values, fairly large interquartile ranges for the measurement times C and E, and might have caused bias in the presented results. We were not able to investigate data regarding renal parenchyma preserved [39, 40, 49, 54] or tumour complexity described by a multimodal nephrometric score such as the RENAL [58] and PADUA [59] Nephrometry Score, or renal tumour contact surface area [60], which might have influenced the short-term change in renal function. Instead, we decided to use the tumour diameter, tumour location, and IT in the regression analyses as adjusting surrogate parameters for the amount of renal parenchyma removed. This strategy is supported by a study by Meyer et al., who used a precise three-dimensional volumetric analysis to prove that IT, tumour size, and endophytic/exophytic properties of a localised renal mass are the most important determinants of renal parenchymal volume loss [61]. However, AKI is currently stratified by increase in serum creatinine levels above baseline, with different classification schemes reporting different AKI rates (e.g., AKI criteria of KDIGO adopted for this study) resulting in higher AKI rates compared to the RIFLE (Risk, Injury, Failure, Loss of kidney function, and End-stage kidney disease) classification [62]. Moreover, this classical approach to define AKI does not take into account the reduction in nephron mass that occurs with NSS, and thus may overestimate the true incidence or grade of AKI [39]. Furthermore, changes in renal function measured by serum creatinine and eGFR might not be sufficiently accurate, especially when investigating patients with a normal contralateral kidney which compensates for loss of renal function. The MDRD equation we used is validated only until the age of 70 and was originally validated only for patients with CKD. Moreover, the MDRD equation categorised 7% more patients as having new-onset CKD after NSS compared to the CKD-EPI equation [56].
Conclusions
Despite these limitations, the findings of this study suggest that AKI within 48 h postoperatively and CKD stage ≥3 develop in nearly 40.0 and 28.0% of patients after NSS for RCC, respectively. Baseline kidney function plays a key role in postoperative short-term and long-term relative changes in renal function, whereas renal ischaemia per se and longer IT negatively impact the short-term renal function and increase the risk for AKI. ONSS is significantly associated with an increased short-term impairment of renal function and increased risk for AKI. The tumour diameter and percentage change in renal function after a median of 1 day postoperatively appeared to constitute surrogate parameters to predict the percentage change in renal function after a median of 13 months postoperatively. The development of AKI was not directly associated with baseline renal function, but the impact of IT causes different dynamics in AKI rates depending on the baseline eGFR category. Otherwise, ZI surgery was not shown to influence long-term outcome variables significantly, which was recently confirmed by split renal scintigraphy [63].
Our findings are helpful for surgical planning, and they suggest either the application of a clampless NSS technique or at least the shortest possible IT to reduce the risk of short-term impairment of the renal function, which might prevent AKI, particularly regarding patients with baseline eGFR category ≥G3, and might reduce long-term impairment of renal function. The reason for the beneficial effects of LNSS on short-term renal function remains unclear, but different techniques of clamping of the renal artery (e.g., bulldog clamps in LNSS or Satinsky clamps in ONSS, like in or study), different renal/cortical reconstruction techniques, assuming tighter cortical renorrhaphy in ONSS [64], or a selection bias of higher tumour complexity in the open cases performed, may have influenced the worse short-term renal outcome observed in ONSS. Future investigations and strategies are needed to reduce ischaemia/reperfusion injury. Well-designed high quality prospective studies are needed to evaluate both the impact of nephrometric scores and renal ischemia/zero-ischemia on the renal functional outcomes in patients undergoing NSS for renal tumours (e.g. trial NTC02287987, [65]. Furthermore, studies evaluating renal function preservation after NSS should control for reconstructive renal injury. In addition, a modified definition of AKI in terms of surgery-related kidney injury that uses specific markers for renal tubular injury independently from a varying blood creatinine level, e.g. urinary biomarkers [66, 67], might help to better describe the postoperative short-term renal function and to predict the long-term renal function.
Change history
07 March 2019
Following publication
Abbreviations
- AKI:
-
Acute Kidney Injury
- AUA:
-
American Urological Association
- BMI:
-
Body Mass Index
- CKD:
-
Chronic kidney disease
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- CT:
-
Computed Tomography
- EAU:
-
European Association of Urology
- eGFR:
-
Estimated Glomerular Filtration Rate
- f:
-
Female
- IQR:
-
Interquartile range
- IT:
-
Ischaemia time
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- LNSS:
-
Laparoscopic nephron-sparing surgery
- LNSS-RI:
-
Laparoscopic nephron-sparing surgery group with intraoperative renal ischaemia
- m:
-
Male
- MDRD:
-
Modification of Diet in Renal Disease
- MRI:
-
Magnetic Resonance Imaging
- n:
-
Number
- NSS ≥ G3:
-
Nephron-sparing surgery group with baseline estimated glomerular filtration rate category ≥G3
- NSS:
-
Nephron-sparing surgery
- NSS-AKI:
-
Nephron-sparing surgery group with development of postoperative acute kidney injury
- NSS-C:
-
Overall nephron-sparing surgery cohort
- NSS-G1:
-
Nephron-sparing surgery group with baseline estimated glomerular filtration rate category G1
- NSS-G2:
-
Nephron-sparing surgery group with baseline estimated glomerular filtration rate category G2
- NSS-NAKI:
-
Nephron-sparing surgery group without development of postoperative acute kidney injury
- NSS-NRI:
-
Nephron-sparing surgery group without intraoperative renal ischaemia
- NSS-RI:
-
Nephron-sparing surgery group with intraoperative renal ischaemia
- ONSS:
-
Open nephron-sparing surgery
- ONSS-RI:
-
Open nephron-sparing surgery group with intraoperative renal ischaemia
- OR:
-
Odds Ratio
- p.o.:
-
Postoperative
- RCC:
-
Renal cell cancer
- ref.:
-
Reference
- RIFLE:
-
Risk, Injury, Failure, Loss of kidney function, and End-stage kidney disease
- UICC:
-
Union Internationale Contre le Cancer
- ZI:
-
Zero ischaemia
References
Campbell SC, Novick AC, Belldegrun A, Blute ML, Chow GK, Derweesh IH, et al. Guideline for management of the clinical T1 renal mass. J Urol. 2009;182:1271–9. https://doi.org/10.1016/j.juro.2009.07.004.
Ljungberg B, Bensalah K, Canfield S, Dabestani S, Hofmann F, Hora M, et al. EAU Guidelines on Renal Cell Carcinoma: 2014 Update. Eur Urol. 2015;67:913–24. https://doi.org/10.1016/j.eururo.2015.01.005.
MacLennan S, Imamura M, Lapitan MC, Omar MI, Lam TBL, Hilvano-Cabungcal AM, et al. Systematic review of perioperative and quality-of-life outcomes following surgical management of localised renal cancer. Eur Urol. 2012;62:1097–117. https://doi.org/10.1016/j.eururo.2012.07.028.
Liss MA, Wang S, Palazzi K, Jabaji R, Patel N, Lee HJ, et al. Evaluation of national trends in the utilization of partial nephrectomy in relation to the publication of the American urologic association guidelines for the management of clinical T1 renal masses. BMC Urol. 2014;14:101. https://doi.org/10.1186/1471-2490-14-101.
Marszalek M, Meixl H, Polajnar M, Rauchenwald M, Jeschke K, Madersbacher S. Laparoscopic and open partial nephrectomy: a matched-pair comparison of 200 patients. Eur Urol. 2009;55:1171–8. https://doi.org/10.1016/j.eururo.2009.01.042.
Gill IS, Kavoussi LR, Lane BR, Blute ML, Babineau D, Colombo JR, et al. Comparison of 1,800 laparoscopic and open partial nephrectomies for single renal tumors. J Urol. 2007;178:41–6. https://doi.org/10.1016/j.juro.2007.03.038.
Lane BR, Gill IS. 7-year oncological outcomes after laparoscopic and open partial nephrectomy. J Urol. 2010;183:473–9. https://doi.org/10.1016/j.juro.2009.10.023.
Capitanio U, Terrone C, Antonelli A, Minervini A, Volpe A, Furlan M, et al. Nephron-sparing techniques independently decrease the risk of cardiovascular events relative to radical nephrectomy in patients with a T1a-T1b renal mass and normal preoperative renal function. Eur Urol. 2015;67:683–9. https://doi.org/10.1016/j.eururo.2014.09.027.
MacLennan S, Imamura M, Lapitan MC, Omar MI, Lam TBL, Hilvano-Cabungcal AM, et al. Systematic review of oncological outcomes following surgical management of localised renal cancer. Eur Urol. 2012;61:972–93. https://doi.org/10.1016/j.eururo.2012.02.039.
Kim SP, Thompson RH, Boorjian SA, Weight CJ, Han LC, Murad MH, et al. Comparative effectiveness for survival and renal function of partial and radical nephrectomy for localized renal tumors: a systematic review and meta-analysis. J Urol. 2012;188:51–7. https://doi.org/10.1016/j.juro.2012.03.006.
Scosyrev E, Messing EM, Sylvester R, Campbell S, Van Poppel H. Renal function after nephron-sparing surgery versus radical nephrectomy: results from EORTC randomized trial 30904. Eur Urol. 2014;65:372–7. https://doi.org/10.1016/j.eururo.2013.06.044.
Kim CS, Bae EH, Ma SK, Kweon S-S, Kim SW. Impact of partial nephrectomy on kidney function in patients with renal cell carcinoma. BMC Nephrol. 2014;15:181. https://doi.org/10.1186/1471-2369-15-181.
Thompson RH. Partial versus radical nephrectomy: the debate regarding renal function ends while the survival controversy continues. Eur Urol. 2014;65:378–9; discussion 379–380. https://doi.org/10.1016/j.eururo.2013.07.036.
Kim SP, Campbell SC, Gill I, Lane BR, Van Poppel H, Smaldone MC, et al. Collaborative review of risk benefit trade-offs between partial and radical nephrectomy in the Management of Anatomically Complex Renal Masses. Eur Urol. 2017;72:64–75. https://doi.org/10.1016/j.eururo.2016.11.038.
Shuch B, Hanley J, Lai J, Vourganti S, Kim SP, Setodji CM, et al. Overall survival advantage with partial nephrectomy: a bias of observational data? Cancer. 2013;119:2981–9. https://doi.org/10.1002/cncr.28141.
Van Poppel H, Da Pozzo L, Albrecht W, Matveev V, Bono A, Borkowski A, et al. A prospective, randomised EORTC intergroup phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol. 2011;59:543–52. https://doi.org/10.1016/j.eururo.2010.12.013.
Scosyrev E, Messing EM, Sylvester R, Van Poppel H. Exploratory subgroup analyses of renal function and overall survival in European Organization for Research and Treatment of Cancer randomized trial of nephron-sparing surgery versus radical nephrectomy. Eur Urol Focus. 2017;3:599–605. https://doi.org/10.1016/j.euf.2017.02.015.
Lane BR, Campbell SC, Demirjian S, Fergany AF. Surgically induced chronic kidney disease may be associated with a lower risk of progression and mortality than medical chronic kidney disease. J Urol. 2013;189:1649–55. https://doi.org/10.1016/j.juro.2012.11.121.
Weight CJ, Larson BT, Fergany AF, Gao T, Lane BR, Campbell SC, et al. Nephrectomy induced chronic renal insufficiency is associated with increased risk of cardiovascular death and death from any cause in patients with localized cT1b renal masses. J Urol. 2010;183:1317–23. https://doi.org/10.1016/j.juro.2009.12.030.
Weight CJ, Lieser G, Larson BT, Gao T, Lane BR, Campbell SC, et al. Partial nephrectomy is associated with improved overall survival compared to radical nephrectomy in patients with unanticipated benign renal tumours. Eur Urol. 2010;58:293–8. https://doi.org/10.1016/j.eururo.2010.04.033.
Antonelli A, Minervini A, Sandri M, Bertini R, Bertolo R, Carini M, et al. Below safety limits, every unit of glomerular filtration rate counts: assessing the relationship between renal function and Cancer-specific mortality in renal cell carcinoma. Eur Urol. 2018;74:661–7. https://doi.org/10.1016/j.eururo.2018.07.029.
Huang WC, Levey AS, Serio AM, Snyder M, Vickers AJ, Raj GV, et al. Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol. 2006;7:735–40. https://doi.org/10.1016/S1470-2045(06)70803-8.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–305. https://doi.org/10.1056/NEJMoa041031.
Antonelli A, Mari A, Longo N, Novara G, Porpiglia F, Schiavina R, et al. Role of clinical and surgical factors for the prediction of immediate, early and late functional results, and its relationship with cardiovascular outcome after partial nephrectomy: results from the prospective multicenter RECORd 1 project. J Urol. 2018;199:927–32. https://doi.org/10.1016/j.juro.2017.11.065.
Muramaki M, Miyake H, Sakai I, Fujisawa M. Prognostic factors influencing postoperative development of chronic kidney disease in patients with small renal tumors who underwent partial nephrectomy. Curr Urol. 2013;6:129–35. https://doi.org/10.1159/000343526.
Malcolm JB, Bagrodia A, Derweesh IH, Mehrazin R, Diblasio CJ, Wake RW, et al. Comparison of rates and risk factors for developing chronic renal insufficiency, proteinuria and metabolic acidosis after radical or partial nephrectomy. BJU Int. 2009;104:476–81. https://doi.org/10.1111/j.1464-410X.2009.08376.x.
Ckd Evaluation & Management | Kdigo n.d. https://kdigo.org/guidelines/ckd-evaluation-and-management/. Accessed 25 Nov 2016.
Rocco MV, Gassman JJ, Wang SR, Kaplan RM. Cross-sectional study of quality of life and symptoms in chronic renal disease patients: the modification of diet in renal disease study. Am J Kidney Dis Off J Natl Kidney Found. 1997;29:888–96.
Acute Kidney Injury | Kdigo n.d. https://kdigo.org/guidelines/acute-kidney-injury/. Accessed 25 Nov 2016.
Little RJA. Missing-data adjustments in large surveys (with discussion). J Bus Econ Stat. 1988;6:287–301.
Schenker N, Taylor J. Partially parametric techniques for multiple imputation. Comput Stat Data Anal. 1996;22:425–46.
Lane BR, Babineau DC, Poggio ED, Weight CJ, Larson BT, Gill IS, et al. Factors predicting renal functional outcome after partial nephrectomy. J Urol. 2008;180:2363–8; discussion 2368–2369. https://doi.org/10.1016/j.juro.2008.08.036.
Huang WC, Elkin EB, Levey AS, Jang TL, Russo P. Partial nephrectomy versus radical nephrectomy in patients with small renal tumors--is there a difference in mortality and cardiovascular outcomes? J Urol. 2009;181:55–61; discussion 61–62. https://doi.org/10.1016/j.juro.2008.09.017.
Mir MC, Ercole C, Takagi T, Zhang Z, Velet L, Remer EM, et al. Decline in renal function after partial nephrectomy: etiology and prevention. J Urol. 2015;193:1889–98. https://doi.org/10.1016/j.juro.2015.01.093.
Mir MC, Pavan N, Parekh DJ. Current paradigm for ischemia in kidney surgery. J Urol. 2016;195:1655–63. https://doi.org/10.1016/j.juro.2015.09.099.
Kim SP, Thompson RH. Kidney function after partial nephrectomy: current thinking. Curr Opin Urol. 2013;23:105–11. https://doi.org/10.1097/MOU.0b013e32835d8ec1.
Volpe A, Blute ML, Ficarra V, Gill IS, Kutikov A, Porpiglia F, et al. Renal ischemia and function after partial nephrectomy: a collaborative review of the literature. Eur Urol. 2015;68:61–74. https://doi.org/10.1016/j.eururo.2015.01.025.
Klatte T, Ficarra V, Gratzke C, Kaouk J, Kutikov A, Macchi V, et al. A literature review of renal surgical anatomy and surgical strategies for partial nephrectomy. Eur Urol. 2015;68:980–92. https://doi.org/10.1016/j.eururo.2015.04.010.
Zhang Z, Zhao J, Dong W, Remer E, Li J, Demirjian S, et al. Acute kidney injury after partial nephrectomy: role of parenchymal mass reduction and ischemia and impact on subsequent functional recovery. Eur Urol. 2016;69:745–52. https://doi.org/10.1016/j.eururo.2015.10.023.
Dong W, Wu J, Suk-Ouichai C, Caraballo Antonio E, Remer E, Li J, et al. Devascularized parenchymal mass associated with partial nephrectomy: predictive factors and impact on functional recovery. J Urol. 2017. https://doi.org/10.1016/j.juro.2017.04.020.
Song C, Bang JK, Park HK, Ahn H. Factors influencing renal function reduction after partial nephrectomy. J Urol. 2009;181:48–53; discussion 53–54. https://doi.org/10.1016/j.juro.2008.09.030.
Adamy A, Favaretto RL, Nogueira L, Savage C, Russo P, Coleman J, et al. Recovery of renal function after open and laparoscopic partial nephrectomy. Eur Urol. 2010;58:596–601. https://doi.org/10.1016/j.eururo.2010.05.044.
Rod X, Peyronnet B, Seisen T, Pradere B, Gomez FD, Verhoest G, et al. Impact of ischaemia time on renal function after partial nephrectomy: a systematic review. BJU Int. 2016;118:692–705. https://doi.org/10.1111/bju.13580.
Ghoneim TP, Sjoberg DD, Lowrance W, Shariat SF, Savage C, Bernstein M, et al. Partial nephrectomy for renal tumors in solitary kidneys: postoperative renal function dynamics. World J Urol. 2015;33:2023–9. https://doi.org/10.1007/s00345-015-1581-9.
Porpiglia F, Fiori C, Bertolo R, Morra I, Russo R, Piccoli G, et al. Long-term functional evaluation of the treated kidney in a prospective series of patients who underwent laparoscopic partial nephrectomy for small renal tumors. Eur Urol. 2012;62:130–5. https://doi.org/10.1016/j.eururo.2012.02.001.
Funahashi Y, Hattori R, Yamamoto T, Kamihira O, Kato K, Gotoh M. Ischemic renal damage after nephron-sparing surgery in patients with normal contralateral kidney. Eur Urol. 2009;55:209–15. https://doi.org/10.1016/j.eururo.2008.07.048.
Laven BA, Orvieto MA, Chuang MS, Ritch CR, Murray P, Harland RC, et al. Renal tolerance to prolonged warm ischemia time in a laparoscopic versus open surgery porcine model. J Urol. 2004;172:2471–4.
Thompson RH, Lane BR, Lohse CM, Leibovich BC, Fergany A, Frank I, et al. Every minute counts when the renal hilum is clamped during partial nephrectomy. Eur Urol. 2010;58:340–5. https://doi.org/10.1016/j.eururo.2010.05.047.
Zhang Z, Zhao J, Velet L, Ercole CE, Remer EM, Mir CM, et al. Functional recovery from extended warm ischemia associated with partial nephrectomy. Urology. 2016;87:106–13. https://doi.org/10.1016/j.urology.2015.08.034.
Cisek LJ, Gobet RM, Peters CA. Pneumoperitoneum produces reversible renal dysfunction in animals with normal and chronically reduced renal function. J Endourol Endourol Soc. 1998;12:95–100. https://doi.org/10.1089/end.1998.12.95.
Yilmaz S, Koken T, Tokyol C, Kahraman A, Akbulut G, Serteser M, et al. Can preconditioning reduce laparoscopy-induced tissue injury? Surg Endosc. 2003;17:819–24. https://doi.org/10.1007/s00464-002-9096-z.
Toosy N, McMorris EL, Grace PA, Mathie RT. Ischaemic preconditioning protects the rat kidney from reperfusion injury. BJU Int. 1999;84:489–94.
Rajan S, Babazade R, Govindarajan SR, Pal R, You J, Mascha EJ, et al. Perioperative factors associated with acute kidney injury after partial nephrectomy. Br J Anaesth. 2016;116:70–6. https://doi.org/10.1093/bja/aev416.
Lane BR, Russo P, Uzzo RG, Hernandez AV, Boorjian SA, Thompson RH, et al. Comparison of cold and warm ischemia during partial nephrectomy in 660 solitary kidneys reveals predominant role of nonmodifiable factors in determining ultimate renal function. J Urol. 2011;185:421–7. https://doi.org/10.1016/j.juro.2010.09.131.
Clark MA, Shikanov S, Raman JD, Smith B, Kaag M, Russo P, et al. Chronic kidney disease before and after partial nephrectomy. J Urol. 2011;185:43–8. https://doi.org/10.1016/j.juro.2010.09.019.
Shikanov S, Clark MA, Raman JD, Smith B, Kaag M, Russo P, et al. Chronic kidney disease epidemiology collaboration versus modification of diet in renal disease equations for renal function evaluation in patients undergoing partial nephrectomy. J Urol. 2010;184:1867–71. https://doi.org/10.1016/j.juro.2010.06.104.
Lee H, Song BD, Byun S-S, Lee SE, Hong SK. Impact of warm ischaemia time on postoperative renal function after partial nephrectomy for clinical T1 renal cell carcinoma: a propensity score-matched study. BJU Int. 2018;121:46–52. https://doi.org/10.1111/bju.13968.
Kutikov A, Uzzo RG. The R.E.N.A.L. nephrometry score: a comprehensive standardized system for quantitating renal tumor size, location and depth. J Urol. 2009;182:844–53. https://doi.org/10.1016/j.juro.2009.05.035.
Ficarra V, Novara G, Secco S, Macchi V, Porzionato A, De Caro R, et al. Preoperative aspects and dimensions used for an anatomical (PADUA) classification of renal tumours in patients who are candidates for nephron-sparing surgery. Eur Urol. 2009;56:786–93. https://doi.org/10.1016/j.eururo.2009.07.040.
Leslie S, Gill IS, de Castro Abreu AL, Rahmanuddin S, Gill KS, Nguyen M, et al. Renal tumor contact surface area: a novel parameter for predicting complexity and outcomes of partial nephrectomy. Eur Urol. 2014;66:884–93. https://doi.org/10.1016/j.eururo.2014.03.010.
Meyer A, Woldu SL, Weinberg AC, Thoreson GR, Pierorazio P, Matulay JT, et al. Predicting renal parenchymal loss after nephron sparing surgery. J Urol. 2015;194:658–63. https://doi.org/10.1016/j.juro.2015.03.098.
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative workgroup. Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the second international consensus conference of the acute Dialysis quality initiative (ADQI) group. Crit Care Lond Engl. 2004;8:R204–12. https://doi.org/10.1186/cc2872.
Porpiglia F, Bertolo R, Amparore D, Podio V, Angusti T, Veltri A, et al. Evaluation of functional outcomes after laparoscopic partial nephrectomy using renal scintigraphy: clamped vs clampless technique. BJU Int. 2015;115:606–12. https://doi.org/10.1111/bju.12834.
Bahler CD, Sundaram CP. Effect of renal reconstruction on renal function after partial nephrectomy. J Endourol. 2016;30(Suppl 1):S37–41. https://doi.org/10.1089/end.2016.0055.
Cindolo L, Antonelli A, Sandri M, Annino F, Celia A, De Concilio B, et al. The role of vascular clamping during robot-assisted partial nephrectomy for localised renal cancer: rationale and design of the CLOCK randomised phase III study. Minerva Urol E Nefrol Ital J Urol Nephrol. 2019. https://doi.org/10.23736/S0393-2249.18.03357-X.
Ebbing J, Seibert FS, Pagonas N, Bauer F, Miller K, Kempkensteffen C, et al. Dynamics of urinary calprotectin after renal Ischaemia. PLoS One. 2016;11:e0146395. https://doi.org/10.1371/journal.pone.0146395.
Antonelli A, Allinovi M, Cocci A, Russo GI, Schiavina R, Rocco B, et al. The predictive role of biomarkers for the detection of acute kidney injury after partial or radical nephrectomy: a systematic review of the literature. Eur Urol Focus. 2018. https://doi.org/10.1016/j.euf.2018.09.020.
Acknowledgements
We thank Selina Ackermann, scientific assistant, University Hospital Basel, Switzerland for editing the manuscript.
Funding
None.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to relevant data protection formalities but are available from the corresponding author J.E. on reasonable request.
Author information
Authors and Affiliations
Contributions
JE designed the study, did some of the statistical analyses, interpreted the data, and drafted the manuscript. CK critically revised the manuscript for important intellectual content and interpreted the data. FM, BR, BE, TFF, JB, and TW were involved in the data aquisition and interpretation, and revised the manuscript for important intellectual content. KM, JWC, CA, HHS, PA, and CW were involved in revising the manuscript for important intellectual content as well as data interpretation. PF was involved in the multivariate analyses of the data, performed the multiple imputations of missing data, and drafted the natural cubic splines. All authors read, gave comments, and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Data collection was performed and written informed consent obtained in accordance with the requirements of the local ethics committee of the Charité - Universitätsmedizin Berlin.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional information
The original version of this article was revised: Figure 1 and the caption of Table 4 have been corrected.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Ebbing, J., Menzel, F., Frumento, P. et al. Outcome of kidney function after ischaemic and zero-ischaemic laparoscopic and open nephron-sparing surgery for renal cell cancer. BMC Nephrol 20, 40 (2019). https://doi.org/10.1186/s12882-019-1215-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12882-019-1215-3