Abstract
Background
Certain demyelinating disorders, such as neuromyelitis optica spectrum disorder (NMOSD) and myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD) exhibit serum autoantibodies against aquaporin-4 (αAQP4) and myelin oligodendrocyte glycoprotein (αMOG). The variability of the autoantibody presentation warrants further research into subtyping each case.
Methods
To elucidate the relationship between astroglial and neuronal protein concentrations in the peripheral circulation with occurrence of these autoantibodies, 86 serum samples were analyzed using immunoassays. The protein concentration of glial fibrillary acidic protein (GFAP), neurofilament light chain (NFL) and tau protein was measured in 3 groups of subcategories of suspected NMOSD: αAQP4 positive (n = 20), αMOG positive (n = 32) and αMOG/αAQP4 seronegative (n = 34). Kruskal-Wallis analysis, univariate predictor analysis, and multivariate logistic regression with ROC curves were performed.
Results
GFAP and NFL concentrations were significantly elevated in the αAQP4 positive group (p = 0.003; p = 0.042, respectively), and tau was elevated in the αMOG/αAQP4 seronegative group (p < 0.001). A logistic regression model to classify serostatus was able to separate αAQP4 seropositivity using GFAP + tau, and αMOG seropositivity using tau. The areas under the ROC curves (AUCs) were 0.77 and 0.72, respectively. Finally, a combined seropositivity versus negative status logistic regression model was generated, with AUC = 0.80.
Conclusion
The 3 markers can univariately and multivariately classify with moderate accuracy the samples with seropositivity and seronegativity for αAQP4 and αMOG.
Similar content being viewed by others
Introduction
The existence of autoantibodies against glial cell proteins, namely aquaporin-4 (αAQP4) and myelin oligodendrocyte glycoprotein (αMOG) is an important pathobiological feature of certain central nervous system (CNS) autoimmune demyelinating diseases, such as neuromyelitis optica spectrum disorder (NMOSD) and myelin oligodendrocyte glycoprotein antibody-associated disease (MOGAD) [1,2,3]. According to the 2015 diagnostic criteria [4], these diseases are: (i) characterized by longitudinally extensive transverse myelitis (TM), optic neuritis (ON), and brainstem dysfunction, among other symptoms; (ii) they are positive for αAQP4 and/or αMOG; and (iii) are a distinct entity from multiple sclerosis (MS) [5,6,7], thus requiring its exclusion. The symptoms can occur simultaneously, or can present in a limited form (e.g., isolated ON) [8], and for MOGAD, the presence of αMOG is a requirement for diagnosis [9].
Intriguingly, however, not all patients with NMOSD are positive for the above specified autoantibodies (these are known as seronegative patients), thus posing challenges in the diagnosis, prognosis and treatment of the disorder [8]. In addition, markers to predict a monophasic or relapsing disease course are lacking, as well as predictors of treatment response [8]. In certain circumstances, testing for autoantibodies in the cerebrospinal fluid (CSF), in addition to serum, is necessary since some studies have reported autoantibody positivity only in the CSF of patients with a MOGAD phenotype [10].
Biomarkers are of paramount importance in efforts to: (i) elucidate differentiation markers between NMOSD and MOGAD (and MS), (ii) assist in disease prognosis and treatment response, (iii) further understand the intra-NMOSD patient variability, (iv) determine the relapse risk, and (v) establish methods to evaluate disease severity [11]. In particular, markers of neuronal and astroglial damage, including glial fibrillary acidic protein (GFAP) [12,13,14,15], neurofilament light chain (NFL, also known as NEFL, NF-L, NfL) [16, 17] and tau [18] can shed light into relapse risk versus a monophasic course, predict treatment response and disease severity [8].
In this paper, we focus on elucidating differentiation markers between αAQP4 and αMOG positive and negative samples (αAQP4 positive = αAQP4+; αMOG positive = αMOG+; double seronegative = αMOG-/αAQP4-), and whether these markers can predict autoantibody serostatus. We did not encounter any double seropositive patients in our cohort. We tested serum samples from patients with suspected NMOSD that had recently been tested for αAQP4 and αMOG presence. We also quantified the protein concentrations (not the autoantibodies) of GFAP, NFL and tau in serum. We then examined the possible relationship between αAQP4 and αMOG with the serum markers of neuronal and astrocytic injury, namely the proteins GFAP, NFL and tau.
Materials and methods
Sample collection and analysis
Serum samples from suspected NMOSD patients were provided by the Unity Health Toronto Immunology Laboratory, Toronto, Canada, under institutional Review Board approval (ethical approval number: #19-0321-E). Patients provided a written informed consent for this study. The samples were sent to Unity Health Toronto by province of Ontario-wide third-party laboratories, for the purpose of testing them for αAQP4 and αMOG, as one of the diagnostic requirements for suspected NMOSD. The suspected NMOSD serum samples were divided into three categories: αAQP4+ (n = 20), αMOG+ (n = 32) and αMOG-/αAQP4- (n = 34). There were no samples positive for both αAQP4 and αMOG.
All blood samples were collected under standard laboratory procedures, centrifuged at 3,000 x g after a 30 min coagulation at room temperature, and serum was stored at -80 °C in polypropylene tubes. Sera were then aliquoted, coded and stored at Mount Sinai Hospital, Toronto, Canada at -80 °C until processing.
An aliquot of each sample (n = 86) was coded with a unique identification number and transferred on dry ice to Meso Scale Discovery (MSD, a division of Meso Scale Diagnostics, LLC.; Rockville, MD, USA) for testing, using a 3-marker ultrasensitive electrochemiluminescence sandwich immunoassay (GFAP, NFL and tau). MSD was blinded regarding the identity of the samples and the code was broken after analysis was completed. The code connecting patient and sample identity was known only to the principal investigator (EP Diamandis).
MSD® assays
A new custom multiplex ultrasensitive immunoassay based on electrochemiluminescence detection was used to measure GFAP, tau and NFL in a 96-well plate format. This panel is now commercially available: S-PLEX® Neurology Panel 1 (Meso Scale Discovery, Rockville, MD; catalog # K15640S). The analytical sensitivities of the 3 protein assays (GFAP, NFL, tau) were 0.19pg/mL, 1.28pg/mL and 0.04pg/mL respectively, and their precision was < 15%. The assay requires 25 µL of two-fold diluted serum or plasma. The MSD website (www.mesoscale.com) and our previous publications [19, 20] provide additional information about this assay technology.
Assays at unity health Toronto
Serum samples were analyzed for immunoglobulin class IgG against AQP4 and/or MOG using a semiquantitative in vitro commercial kit (EUROIMMUN Indirect Immunofluoresence Test- IIFT; FA 1128-1005-1, FA 1128-1010-1), according to manufacturer’s recommendations. The samples were diluted ten-fold in a provided buffer and the positivity was measured through fluorescence pattern intensity (graded as 0–5). There is no upper limit to the measurement range of this kit. The manufacturer-specified analytical sensitivity and specificity for the αAQP4 IIFT were 75% and 99.9%, respectively. Similarly, for the αMOG IIFT, the analytical sensitivity and specificity were 95% and 84.9%, respectively.
Statistical analysis
Statistical analyses were performed using R (version 4.2.3 [21]). The concentration values of GFAP, NFL and tau were natural log-transformed after histograms of the 3 markers revealed skewed distributions (see Supplementary Information section, Fig. 1), and the descriptive statistics were reported. Non-parametric Kruskal-Wallis tests were applied to each biomarker, to determine if the median varied across diagnostic groups, and the P-values were adjusted for false discovery rate (FDR) (Table 1).
In parallel, univariate logistic regression models were used on the transformed values to determine if the 3 serum markers were associated with αMOG or αAQP4 status (Table 2). Exploratory multiple logistic regression was used to predict cases that were either αMOG+ or αAQP4+ from combinations of GFAP, tau and NFL. Performance metrics and a receiver operating characteristic (ROC) curve with the area under the curve (AUC) were calculated. To provide an estimate of the AUC that may be expected on an uncharacterized sample, a robust internal validation process was used to calculate the optimism-adjusted AUC [22, 23].
Results
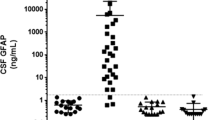
Median protein concentrations varied significantly across αMOG/αAQP4 samples (Table 1). αAQP4+ sera had the highest mean and median values for GFAP and NFL, whereas αMOG-/αAQP4- had the highest mean and median values for tau (Table 1; Fig. 1). αMOG+ had the lowest tau values (Table 1; Fig. 1). Figure 1 represents scatterplots of the protein concentrations in pg/mL in the 3 groups. The αAQP4+ group had higher median NFL values, but the αMOG-/αAQP4- group had some samples with moderately high NFL concentrations.
Scatterplots of protein concentrations of the 3 biomarkers analyzed in the αAQP4+, αMOG+ and αMOG-/αAQP4-groups. The horizontal lines represent the median of each group, and each dot represents the value of the marker in an individual sample. For numerical values and P-values, see Table 1
Figure 2 depicts pairwise plots for each pair of proteins for the two autoantibody statuses, to determine if samples from the diagnostic groups could be differentiated based on any two proteins. Due to the relatively small number of samples in each category, and the significant overlap, the presented data allow only qualitative observations based on the graphs of Fig. 2. Figure 2 (A) shows that the combination of NFL and tau (Fig. 2 (A), top left panel) seems to aggregate most of the αMOG+ to the bottom left (low concentrations for both proteins). Interestingly, however, the optimism-adjusted AUC of the tau model was 0.72 (Fig. 3 (A)) and for the NFL + tau was 0.71 (Table 3), showing that tau alone is a slightly better classifier than the NFL + tau combination. Figure 2 (B), lower panel shows that there is a subset of αAQP4+ samples that can be distinguished from the rest of the samples, with high GFAP (higher than 7 in log serum value). In addition, from an exploratory multivariable logistic regression analysis, GFAP seems to be the strongest predictor of αAQP4+ for both GFAP + NFL (Fig. 2 (B), panel bottom left) and GFAP + tau models (Fig. 2 (B), top right panel), both resulting in AUCs of 0.77, despite NFL and tau not being significant by themselves (Table 3).
Figure 3 depicts the ROC curves for (A) the αMOG status (positive or negative) based on tau as a discriminator, and (B) the αAQP4 status based on GFAP alone and GFAP + tau combination. The calculated AUCs in each subfigure represent the non-adjusted values, while bootstrap-adjusted values were 0.01 units smaller. In Fig. 3 (A), although not corrected for over-fitting, the sensitivity of the model at optimal tau cutoff was 0.5 (0.32, 0.68 CI), the specificity 0.87 (0.75, 0.95 CI), the positive predictive value 0.70 (0.47, 0.87 CI), the negative predictive value 0.75 (0.62, 0.85 CI) and the accuracy 0.73 (0.63, 0.82 CI). Similarly, in Fig. 3 (B), the combined model (GFAP + tau) exhibited a better sensitivity of 0.35 (0.15, 0.59 CI) versus 0.30 (0.12, 0.54 CI) for GFAP alone. For the combined GFAP + tau model, at optimal cutoffs, the specificity was 0.94 (0.85, 0.98 CI), the positive predictive value was 0.64 (0.31, 0.89 CI), the negative predictive value was 0.83 (0.72, 0.90 CI) and the accuracy was 0.80 (0.70, 0.88 CI).
(A) ROC curve for predicting αMOG+ from tau values. The bootstrapped optimism-adjusted AUC is 0.72 (unadjusted value = 0.73). The AUC values from combining NFL + tau or GFAP + tau were lower than for tau alone (data not shown). (B) ROC curves for predicting αAQP4+ status using GFAP (red) and GFAP + tau (blue). The non-adjusted and bootstrapped AUC values of GFAP alone are 0.75 (adjusted) and 0.75 (non-adjusted) and for GFAP + tau are 0.78 and 0.77, respectively
A multivariable logistic regression model was also developed to separate the samples with positive autoantibody status from the double-negative status based on GFAP and tau, after the Kruskal-Wallis test showed significantly different medians for both markers (p < 0.001). Figure 4 depicts a binary classification (either autoantibody positive or negative), with (A) showing a scatterplot of the log transformed GFAP versus tau values, and (B) showing the ROC curve for this binary classification (using GFAP and tau), with an AUC = 0.81 (adjusted 0.80). Particularly for (A), at optimal cutoffs, the sensitivity of the model is 0.87 (0.74, 0.94 CI), the specificity 0.68 (0.49, 0.83 CI), the positive predictive value 0.80 (0.68, 0.90 CI), the negative predictive value 0.77 (0.58, 0.90 CI) and the accuracy 0.79 (0.69, 0.87 CI).
Multivariable logistic regression was used to separate the cases with αAQP4+ or αMOG+ from the cases with a double negative status. (A) The scatterplot of the log-transformed GFAP vs. tau. The dashed line indicates the prediction of αAQP4+ or αMOG+ versus αMOG-/αAQP4-. (B) The ROC curve has an unadjusted AUC of 0.81 (0.80 after optimism-adjustment)
Discussion
Markers of neuronal and astroglial damage are indicative of CNS injury, and they are released into the CSF with subsequent leakage in the periphery, where they can be quantified [8, 24, 25]. In NMOSD, this is hypothesized to occur with the timing of sampling, with relapsing episodes showing high concentration of these markers, while during remission there are lower levels [8].
In this study, we aimed to examine the possible relationship between αAQP4 and αMOG with GFAP, NFL and tau, to find complementary biomarkers of differentiation in the αAQP4+, αMOG+ and αMOG-/αAQP4- groups in samples from patients with suspected NMOSD. The clear separation of the patient groups is crucial, since inappropriate treatments following a false diagnosis may exacerbate symptoms [11, 26,27,28]. With current assays showing low sensitivity for αAQP4 [29] and being dependent on treatment and clinical status [30, 31], and better, newer assays not being used in the clinic as of yet [32], strong interrelated differentiators should be useful.
Several studies in αAQP4+, αMOG+ and αMOG-/αAQP4- NMOSD patients have previously analyzed GFAP, NFL and tau in serum [33,34,35,36]. GFAP is the main cytoskeletal filamentous protein of mature astrocytes, involved in supporting the glial cell structure and strength, as well as supporting neurons and the Blood-Brain Barrier (BBB) [13, 37]. During astrogliosis or brain-related injury, GFAP is excreted into the circulation [12, 24], thus being a good biomarker of traumatic brain injury (TBI) [38], MS [39, 40], dementia [41, 42], brain tumors [43,44,45], and other neurological diseases [46]. NFL, along with other neurofilament proteins, is an intracellular protein in neurons that partakes in axonal stability and radial growth, and it is released after neuroaxonal damage [17]. Just like GFAP, NFL is a promising biomarker of neurodegeneration in MS [17, 47], dementia [48], TBI [38, 49], amyotrophic lateral sclerosis (ALS) and other neurological diseases [48, 50]. NFL is especially important in its ability to reflect ongoing axonal degeneration, thus shedding light on the pathophysiology of NMOSD and its subcategorizations [38]. Lastly, tau is a microtubule-associated protein that is important in neuronal health and function, with multiple alterations being seen in disease [51, 52]. Aberrant tau forms deposited in the blood (and CSF) are a biomarker of tauopathies, Alzheimer’s disease (AD) and other dementias [51, 53, 54], Creutzfeldt-Jakob disease [55] and other brain related neuropathies [56, 57].
In our study, we found that GFAP is significantly higher in αAQP4+ samples compared to αMOG+ and αMOG-/αAQP4- (Fig. 1; Table 1). The one sample in the αMOG-/αAQP4- group that exhibits high GFAP concentration (1,338 pg/mL) could be attributed to: (i) the patient having recently experienced a neurological attack, (ii) the elevated GFAP being a marker of a future episode, or (iii) they had recently experienced an independent TBI event. Importantly, GFAP concentration was a significant univariate predictor of αAQP4 status (Table 2), and GFAP concentration was significant in the multivariable logistic regression for αAQP4 status (Table 3). It was also used as part of the model to classify samples based on their autoantibody seropositivity, with an AUC of 0.80 after optimism-adjustment (Fig. 4). The detection of high GFAP in αAQP4 + samples provides insights into the molecular pathomechanism of NMOSD, and it hints at αAQP4 causing extensive astroglial damage and/or astrogliosis, which later drains into the circulation through arachnoid villi, the glymphatic system or the BBB and blood-CSF barriers [12].
There are a few clinical studies that have analyzed GFAP in serum of patients with NMOSD, specifically with αAQP4 status, reporting conflicting results. In the first study, GFAP was elevated in patients with αAQP4+ and concurrent ON when compared with αAQP4- MS [58]. The same group later analyzed GFAP concentration in NMOSD versus RRMS, MS ON, various other ON-opathies and neurological controls, and found that median serum GFAP was significantly higher when compared with most groups, but not neurological controls [59]. Contrary to the previous analysis, they showed that the GFAP levels did not correlate with AQP4 serostatus, even though in the αAQP4+ relapsing isolated ON group, GFAP was significantly higher than in αAQP4- patients [59]. Similarly, in a study done by Fujii and colleagues, GFAP was not different between αAQP4+ and αAQP4- samples [60]. It must be noted, however, that the number of samples per group (n = 10 for αAQP4+, n = 7 for αAQP4-) were few and for their assay, the serum levels of GFAP were under their limit of detection in > 50% of the samples [60].
Using single-molecule array (SIMOA), Schindler and colleagues found that, although serum GFAP and NFL in αAQP4+ NMOSD had a higher median concentration than in αMOG+ patients and healthy controls, the difference was non-significant [36]. Importantly, αAQP4+ cases with GFAP > 90 pg/mL at baseline had a shorter time to a subsequent attack, hinting at the prognostic value of this marker that previous studies had failed to report [36]. A recent clinical trial corroborated that finding, with serum GFAP showing predictive capacity for future attacks [61]. A 2019 study compared relapse/remission αAQP4+ NMOSD with healthy controls (HC) and relapse/remission RRMS, finding that relapse αAQP4+ NMOSD had significantly higher serum GFAP and NFL in comparison to HC, and higher serum GFAP than remission αAQP4+ NMOSD and relapse/remission RRMS [33]. Finally, studies in CSF have consistently found that GFAP is higher in patients with αAQP4+ and αMOG-/αAQP4- compared to αMOG+ patients and patients with MS or noninflammatory neurological controls; although in some analyses, the highest levels correlated with occurrence of myelitis rather than ON or brain lesions [62,63,64]. In our analysis, we did not have access to αAQP4+ CSF samples, and thus, we cannot confirm their results.
For NFL, studies have not found large differences in the serum of αAQP4+, αMOG+ and αMOG-/αAQP4- groups. For example, using SIMOA, Lee et al. reported that the levels of NFL in patients with TM did not differ, regardless of the autoantibody titers [65]. Intriguingly, NFL levels correlated with expanded disability status scale (EDSS) scores in the αAQP4+ NMOSD and αMOG+ MOGAD TM groups [65]. Mariotto and colleagues found that serum NFL was significantly higher in αAQP4+ than MS and HC, with a weaker difference between αAQP4+ and αMOG+ and αMOG-/αAQP4- [66]. In CSF, on the other hand, NFL titers were higher in NMOSD compared to MS and other neurological diseases with those values correlating with increased disability [67]. Unfortunately, they did not separate αAQP4+ and αAQP4- cases, thus underutilizing this vital differentiation parameter. In our findings, the αAQP4+ group had a significantly higher NFL concentration than the other groups, but as seen in Fig. 1, the overlap is too large to be of clinical use.
In our analysis, we found that median tau concentration was significantly higher in αMOG-/αAQP4- than in the other groups. Although other significant differences are observable, due to the high intra-group range, there is no clear cut-off distinction between all the other groups. In the literature, serum tau has been evaluated in αMOG+, with results showing that its concentration is higher during relapse than remission [68]. Overall, however, αAQP4+ samples had comparable levels to αMOG+ [68], as seen in our results. Despite this, tau concentrations were able to distinguish αMOG + in the univariate and multivariate logistic regression analysis (Tables 2 and 3), with an AUC = 0.72 (optimism-adjusted; Fig. 3). In parallel, it was integrated in the classification models to produce a more significant result for αAQP4 + classification, with AUC increasing from 0.75 to 0.77 (optimism-adjusted; Fig. 3).
Limitations
Our study has several limitations, including: (i) lack of definitive diagnosis in the suspected NMOSD samples, (ii) lack of longitudinal follow-up or relapse/remission data, (iii) examining only 3 candidate serum markers, when more molecules could have been added, such as myelin basic protein, S100B, neurofilament heavy chain, etc., (iv) limited number of samples, (v) lack of paired serum with CSF samples to elucidate CNS-periphery correlation.
Data availability
The excel file with the concentrations of the three biomarkers and their concentrations are available by request from the corresponding author.
Abbreviations
- αAQP4:
-
autoantibody to aquaporin-4
- αMOG:
-
autoantibody to myelin oligodendrocyte glycoprotein
- AUC:
-
area under the ROC curve
- CNS:
-
central nervous system
- NMOSD:
-
neuromyelitis optica spectrum disorder
- MOGAD:
-
myelin oligodendrocyte glycoprotein antibody-associated disease
- TM:
-
transverse myelitis
- ON:
-
optic neuritis
- MS:
-
multiple sclerosis
- CSF:
-
cerebrospinal fluid
- GFAP:
-
glial fibrillary acidic protein
- NFL/NfL/NEFL/NF-L:
-
neurofilament light chain
- αAQP4+:
-
αAQP4 positive
- αMOG+:
-
αMOG positive
- αMOG-/αAQP4-:
-
double seronegative for MOG and AQP4
- PPMS:
-
primary progressive MS
- RRMS:
-
relapsing-remitting MS
- PRMS:
-
progressive-relapsing MS
- CIS:
-
clinically isolated syndrome
- MSD:
-
Meso Scale Discovery
- FDR:
-
false discovery rate
- BBB:
-
blood-brain barrier
- TBI:
-
traumatic brain injury
- AD:
-
Alzheimer’s Disease
- HC:
-
healthy controls
- SIMOA:
-
single-molecule array
- EDSS:
-
expanded disability status scale
- ROC:
-
receiving operating characteristic
References
Arciénega II, Brunet JF, Bloch J, Badaut J. Cell locations for AQP1, AQP4 and 9 in the non-human primate brain. Neuroscience. 2010;167(4):1103–14.
Ikeshima-Kataoka H. Neuroimmunological implications of AQP4 in astrocytes. Int J Mol Sci. 2016;17(8):1306.
Jarius S, Ruprecht K, Kleiter I, Borisow N, Asgari N, Pitarokoili K, et al. MOG-IgG in NMO and related disorders: a multicenter study of 50 patients. Part 1: frequency, syndrome specificity, influence of disease activity, long-term course, association with AQP4-IgG, and origin. J Neuroinflammation. 2016;13:279.
Wingerchuk DM, Banwell B, Bennett JL, Cabre P, Carroll W, Chitnis T, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015;85(2):177–89.
Lennon VA, Wingerchuk DM, Kryzer TJ, Pittock SJ, Lucchinetti CF, Fujihara K, et al. A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. Lancet Lond Engl. 2004;364(9451):2106–12.
Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018;17(2):162–73.
Mewes D, Kuchling J, Schindler P, Khalil AAA, Jarius S, Paul F, et al. Diagnosis of Neuromyelitis Optica Spectrum Disorder (NMOSD) and MOG antibody-Associated Disease (MOGAD). Klin Monatsbl Augenheilkd. 2022;239(11):1315–24.
Dinoto A, Sechi E, Flanagan EP, Ferrari S, Solla P, Mariotto S, et al. Serum and cerebrospinal fluid biomarkers in Neuromyelitis Optica Spectrum Disorder and myelin oligodendrocyte glycoprotein Associated Disease. Front Neurol. 2022;13:866824.
Jarius S, Paul F, Aktas O, Asgari N, Dale RC, de Seze J, et al. [MOG encephalomyelitis: international recommendations on diagnosis and antibody testing]. Nervenarzt. 2018;89(12):1388–99.
Carta S, Höftberger R, Bolzan A, Bozzetti S, Bonetti B, Scarpelli M, et al. Antibodies to MOG in CSF only: pathological findings support the diagnostic value. Acta Neuropathol (Berl). 2021;141(5):801–4.
Kümpfel T, Giglhuber K, Aktas O, Ayzenberg I, Bellmann-Strobl J, Häußler V et al. Update on the diagnosis and treatment of neuromyelitis optica spectrum disorders (NMOSD) – revised recommendations of the Neuromyelitis Optica Study Group (NEMOS). Part II: Attack therapy and long-term management. J Neurol. 2023 [cited 2023 Sep 13]; https://doi.org/10.1007/s00415-023-11910-z.
Abdelhak A, Foschi M, Abu-Rumeileh S, Yue JK, D’Anna L, Huss A, et al. Blood GFAP as an emerging biomarker in brain and spinal cord disorders. Nat Rev Neurol. 2022;18(3):158–72.
Eng LF, Vanderhaeghen JJ, Bignami A, Gerstl B. An acidic protein isolated from fibrous astrocytes. Brain Res. 1971;28(2):351–4.
Saraste M, Bezukladova S, Matilainen M, Sucksdorff M, Kuhle J, Leppert D, et al. Increased serum glial fibrillary acidic protein associates with microstructural white matter damage in multiple sclerosis: GFAP and DTI. Mult Scler Relat Disord. 2021;50:102810.
Björklund H, Eriksdotter-Nilsson M, Dahl D, Rose G, Hoffer B, Olson L. Image analysis of GFA-positive astrocytes from adolescence to senescence. Exp Brain Res. 1985;58(1):163–70.
Lycke JN, Karlsson JE, Andersen O, Rosengren LE. Neurofilament protein in cerebrospinal fluid: a potential marker of activity in multiple sclerosis. J Neurol Neurosurg Psychiatry. 1998;64(3):402–4.
Varhaug KN, Torkildsen Ø, Myhr KM, Vedeler CA. Neurofilament Light Chain as a Biomarker in Multiple Sclerosis. Front Neurol. 2019 [cited 2023 Aug 2];10. Available from: https://www.frontiersin.org/articles/https://doi.org/10.3389/fneur.2019.00338.
Mandelkow EM, Mandelkow E. Biochemistry and Cell Biology of tau protein in Neurofibrillary Degeneration. Cold Spring Harb Perspect Med. 2012;2(7):a006247.
Ren AH, Soosaipillai A, Mathew A, Nikolenko G, Sardesai L, Stengelin M, et al. Utility of a fifth-generation ultrasensitive prostate-specific Antigen assay for monitoring prostate Cancer patients after Radical Prostatectomy with 3 years of Follow-Up. Clin Chem. 2020;66(10):1329–38.
Diamandis EP, Stanczyk FZ, Wheeler S, Mathew A, Stengelin M, Nikolenko G, et al. Serum complexed and free prostate-specific antigen (PSA) for the diagnosis of the polycystic ovarian syndrome (PCOS). Clin Chem Lab Med. 2017;55(11):1789–97.
R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing: R Core Team. 2023. Available from: https://www.R-project.org/.
Steyerberg EW, Harrell FE, Borsboom GJJM, Eijkemans MJC, Vergouwe Y, Habbema JDF. Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol. 2001;54(8):774–81.
Harrell FE, Slaughter J. Regression modeling strategies: with applications to Linear models, logistic regression, and Survival Analysis. Springer; 2001.
Yang Z, Wang KKW. Glial fibrillary acidic protein: from intermediate filament assembly and gliosis to neurobiomarker. Trends Neurosci. 2015;38(6):364–74.
Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4(147):147ra111.
Kleiter I, Hellwig K, Berthele A, Kümpfel T, Linker RA, Hartung HP, et al. Failure of natalizumab to prevent relapses in neuromyelitis optica. Arch Neurol. 2012;69(2):239–45.
Min JH, Kim BJ, Lee KH. Development of extensive brain lesions following fingolimod (FTY720) treatment in a patient with neuromyelitis optica spectrum disorder. Mult Scler Houndmills Basingstoke Engl. 2012;18(1):113–5.
Palace J, Leite MI, Nairne A, Vincent A. Interferon Beta treatment in neuromyelitis optica: increase in relapses and aquaporin 4 antibody titers. Arch Neurol. 2010;67(8):1016–7.
Waters PJ, Pittock SJ, Bennett JL, Jarius S, Weinshenker BG, Wingerchuk DM. Evaluation of aquaporin-4 antibody assays. Clin Exp Neuroimmunol. 2014;5(3):290–303.
Cohen M, De Sèze J, Marignier R, Lebrun C. False positivity of anti aquaporin-4 antibodies in natalizumab-treated patients. Mult Scler Houndmills Basingstoke Engl. 2016;22(9):1231–4.
Waters PJ, McKeon A, Leite MI, Rajasekharan S, Lennon VA, Villalobos A, et al. Serologic diagnosis of NMO: a multicenter comparison of aquaporin-4-IgG assays. Neurology. 2012;78(9):665–71. discussion 669.
Fu Y, Bi J, Yan Y, Sun X, Li K, Kim SY et al. Rapid Immunodot AQP4 Assay for Neuromyelitis Optica Spectrum Disorder. JAMA Neurol. 2023 [cited 2023 Sep 7]; https://doi.org/10.1001/jamaneurol.2023.2974.
Watanabe M, Nakamura Y, Michalak Z, Isobe N, Barro C, Leppert D, et al. Serum GFAP and neurofilament light as biomarkers of disease activity and disability in NMOSD. Neurology. 2019;93(13):e1299–311.
Aktas O, Smith MA, Rees WA, Bennett JL, She D, Katz E, et al. Serum glial fibrillary acidic protein: a Neuromyelitis Optica Spectrum Disorder Biomarker. Ann Neurol. 2021;89(5):895–910.
Kim H, Lee EJ, Lim YM, Kim KK. Glial Fibrillary Acidic Protein in Blood as a Disease Biomarker of Neuromyelitis Optica Spectrum Disorders. Front Neurol. 2022 [cited 2022 Nov 7];13. Available from: https://www.frontiersin.org/articles/https://doi.org/10.3389/fneur.2022.865730.
Schindler P, Grittner U, Oechtering J, Leppert D, Siebert N, Duchow AS, et al. Serum GFAP and NfL as disease severity and prognostic biomarkers in patients with aquaporin-4 antibody-positive neuromyelitis optica spectrum disorder. J Neuroinflammation. 2021;18(1):105.
Eng LF, Ghirnikar RS, Lee YL. Glial fibrillary acidic protein: GFAP-thirty-one years (1969–2000). Neurochem Res. 2000;25(9–10):1439–51.
Wang KK, Yang Z, Zhu T, Shi Y, Rubenstein R, Tyndall JA, et al. An update on diagnostic and prognostic biomarkers for traumatic brain injury. Expert Rev Mol Diagn. 2018;18(2):165–80.
Abdelhak A, Huss A, Kassubek J, Tumani H, Otto M. Serum GFAP as a biomarker for disease severity in multiple sclerosis. Sci Rep. 2018;8(1):14798.
Högel H, Rissanen E, Barro C, Matilainen M, Nylund M, Kuhle J, et al. Serum glial fibrillary acidic protein correlates with multiple sclerosis disease severity. Mult Scler J. 2020;26(2):210–9.
Mecocci P, Parnetti L, Romano G, Scarelli A, Chionne F, Cecchetti R, et al. Serum anti-GFAP and anti-S100 autoantibodies in brain aging, Alzheimer’s disease and vascular dementia. J Neuroimmunol. 1995;57(1–2):165–70.
Heimfarth L, Passos FRS, Monteiro BS, Araújo AA, de Quintans Júnior S, de Quintans LJ. Serum glial fibrillary acidic protein is a body fluid biomarker: a valuable prognostic for neurological disease - A systematic review. Int Immunopharmacol. 2022;107:108624.
Jung CS, Foerch C, Schänzer A, Heck A, Plate KH, Seifert V, et al. Serum GFAP is a diagnostic marker for glioblastoma multiforme. Brain. 2007;130(12):3336–41.
Jacque CM, Vinner C, Kujas M, Raoul M, Racadot J, Baumann NA. Determination of glial fibrillary acidic protein (GFAP) in human brain tumors. J Neurol Sci. 1978;35(1):147–55.
Ghorbani A, Avery LM, Sohaei D, Soosaipillai A, Richer M, Horbinski C, et al. Discovery of novel glioma serum biomarkers by proximity extension assay. Clin Proteom. 2023;20(1):12.
Kovacs GG. Cellular reactions of the central nervous system. Handb Clin Neurol. 2017;145:13–23.
Cantó E, Barro C, Zhao C, Caillier SJ, Michalak Z, Bove R, et al. Association between serum neurofilament light chain levels and long-term Disease Course among patients with multiple sclerosis followed up for 12 years. JAMA Neurol. 2019;76(11):1359–66.
Rosengren LE, Karlsson JE, Karlsson JO, Persson LI, Wikkelsø C. Patients with amyotrophic lateral sclerosis and other neurodegenerative diseases have increased levels of neurofilament protein in CSF. J Neurochem. 1996;67(5):2013–8.
Gao W, Zhang Z, Lv X, Wu Q, Yan J, Mao G, et al. Neurofilament light chain level in traumatic brain injury. Med (Baltim). 2020;99(38):e22363.
Tortelli R, Ruggieri M, Cortese R, D’Errico E, Capozzo R, Leo A, et al. Elevated cerebrospinal fluid neurofilament light levels in patients with amyotrophic lateral sclerosis: a possible marker of disease severity and progression. Eur J Neurol. 2012;19(12):1561–7.
Wang JZ, Liu F. Microtubule-associated protein tau in development, degeneration and protection of neurons. Prog Neurobiol. 2008;85(2):148–75.
Goedert M, Spillantini MG, Jakes R, Rutherford D, Crowther RA. Multiple isoforms of human microtubule-associated protein tau: sequences and localization in neurofibrillary tangles of Alzheimer’s disease. Neuron. 1989;3(4):519–26.
Pase MP, Beiser AS, Himali JJ, Satizabal CL, Aparicio HJ, DeCarli C, et al. Assessment of plasma total tau level as a predictive biomarker for dementia and related endophenotypes. JAMA Neurol. 2019;76(5):598–606.
Henriksen K, Byrjalsen I, Christiansen C, Karsdal MA. Relationship between serum levels of tau fragments and clinical progression of Alzheimer’s Disease. J Alzheimers Dis. 2015;43(4):1331–41.
Staffaroni AM, Kramer AO, Casey M, Kang H, Rojas JC, Orrú CD, et al. Association of Blood and Cerebrospinal Fluid Tau Level and other biomarkers with survival time in sporadic Creutzfeldt-Jakob Disease. JAMA Neurol. 2019;76(8):969–77.
Demirel ÖF, Cetin I, Turan Ş, Yıldız N, Sağlam T, Duran A. Total tau and Phosphorylated Tau Protein Serum Levels in patients with Schizophrenia compared with controls. Psychiatr Q. 2017;88(4):921–8.
Mirzaii-Dizgah MH, Mirzaii-Dizgah MR, Mirzaii-Dizgah I. Serum and saliva total tau protein as a marker for relapsing-remitting multiple sclerosis. Med Hypotheses. 2020;135:109476.
Storoni M, Petzold A, Plant GT. The use of serum glial fibrillary acidic protein measurements in the diagnosis of neuromyelitis optica spectrum optic neuritis. PLoS ONE. 2011;6(8):e23489.
Storoni M, Verbeek MM, Illes Z, Marignier R, Teunissen CE, Grabowska M, et al. Serum GFAP levels in optic neuropathies. J Neurol Sci. 2012;317(1):117–22.
Fujii C, Tokuda T, Ishigami N, Mizuno T, Nakagawa M. Usefulness of serum S100B as a marker for the acute phase of aquaporin-4 autoimmune syndrome. Neurosci Lett. 2011;494(1):86–8.
Aktas O, Hartung HP, Smith MA, Rees WA, Fujihara K, Paul F, et al. Serum neurofilament light chain levels at attack predict post-attack disability worsening and are mitigated by inebilizumab: analysis of four potential biomarkers in neuromyelitis optica spectrum disorder. J Neurol Neurosurg Psychiatry. 2023;94(9):757–68.
Takano R, Misu T, Takahashi T, Sato S, Fujihara K, Itoyama Y. Astrocytic damage is far more severe than demyelination in NMO: a clinical CSF biomarker study. Neurology. 2010;75(3):208–16.
Wei Y, Chang H, Li X, Du L, Xu W, Cong H, et al. CSF-S100B is a potential candidate biomarker for Neuromyelitis Optica Spectrum Disorders. BioMed Res Int. 2018;2018:5381239.
Kleerekooper I, Herbert MK, Kuiperij HB, Sato DK, Fujihara K, Callegaro D, et al. CSF levels of glutamine synthetase and GFAP to explore astrocytic damage in seronegative NMOSD. J Neurol Neurosurg Psychiatry. 2020;91(6):605–11.
Lee HL, Seok JM, Chung YH, Min JH, Baek SH, Kim SM, et al. Serum neurofilament and glial fibrillary acidic protein in idiopathic and seropositive transverse myelitis. Mult Scler Relat Disord. 2023;79:104957.
Mariotto S, Farinazzo A, Monaco S, Gajofatto A, Zanusso G, Schanda K, et al. Serum neurofilament light chain in NMOSD and related disorders: comparison according to Aquaporin-4 and myelin oligodendrocyte glycoprotein antibodies Status. Mult Scler J - Exp Transl Clin. 2017;3(4):2055217317743098.
Wang H, Wang C, Qiu W, Lu Z, Hu X, Wang K. Cerebrospinal fluid light and heavy neurofilaments in neuromyelitis optica. Neurochem Int. 2013;63(8):805–8.
Kim H, Lee EJ, Kim S, Choi LK, Kim K, Kim HW, et al. Serum biomarkers in myelin oligodendrocyte glycoprotein antibody–associated disease. Neurol Neuroimmunol Neuroinflammation. 2020;7(3):e708.
Acknowledgements
Not applicable.
Funding
Research reported in this publication was supported by the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under Award Number U01NS114144. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
MKC conceptualized and designed the study, performed data collection and shipping, data analysis and drafted the manuscript. LMA performed data analysis and contributed to drafting the manuscript. MDP assisted in conceptualizing and designing the study and in data collection. SS performed the sample collection and sample shipment. DR conceptualized and designed the study. CD, RC, TG, MW, MS, AM, GS and JW performed the sample analysis. EPD and IP conceptualized and designed the study and revised the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
CD, RC, TG, MW, MS, AM, and GS are employees and JW is an officer of Meso Scale Diagnostics, LLC. Otherwise, the authors did not identify any potential, perceived or real conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12014_2024_9466_MOESM1_ESM.docx
Supplementary Material 1: Figure 1. Histogram of the logged distributions of GFAP, NFL and tau in all 86 serum samples.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chatanaka, M.K., Avery, L.M., Pasic, M.D. et al. The relationship between serum astroglial and neuronal markers and AQP4 and MOG autoantibodies. Clin Proteom 21, 28 (2024). https://doi.org/10.1186/s12014-024-09466-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12014-024-09466-9