Abstract
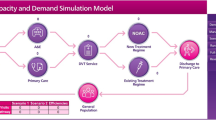
Squeezed budgets and funding cuts are expected to become a feature of the healthcare landscape in the future, forcing decision makers such as service managers, clinicians and commissioners to find effective ways of allocating scarce resources. This paper discusses the development of a decision support toolkit (DST) that facilitates the improvement of services by identifying cost savings and efficiencies within the pathway of care. With the help of National Health Service and commercial experts, we developed a discrete event simulation model for deep vein thrombosis (DVT) patients and adapted the socio-technical allocation of resources (STAR) approach to answer crucial questions like what sort of interventions should we spend our money on? Where will we get the most value for our investment? How will we explain the choices we have made? The DST enables users to model their own services by working with the DST interface allowing users to specify local DVT services. They can input local estimates, or data of service demands and capacities, thus creating a baseline discrete event simulation model. The user can then compare the baseline with potential changes in the patient pathway in the safety of a virtual environment. By making such changes key decision makers can easily understand the impact on activity, cost, staffing levels, skill-mix, utilisation of resources and, more importantly, it allows them to find the interventions that have the highest benefit to patients and provide best value for money.



Similar content being viewed by others
References
Airoldi M, Morton A, Smith AEJ and Bevan G (2014). STAR—people powered prioritization: A 21st-century solution to allocation headaches. Medical Decision Making 34(8):965–975.
Bauersachs R, Berkowitz SD, Brenner B, Buller HR, Decousus H and Gallus AS (2010). Oral rivaroxaban for symptomatic venous thromboembolism. The New England Journal of Medicine 363(26):2499–2510.
Brailsford SC, Lattimer VA, Turnaras P and Turnbull JC (2004). Emergency and on demand health care: Modelling a large complex system. Journal of the Operational Research Society 55(1):34–42.
Brennan A, Chick SE and Davies R (2006). A taxonomy of model structures for economic evaluation of health technologies. Health Economics 15(12):1295–1310.
Codrington-Virtue A, Whittlestone P, Kelly J and Chaussalet TJ (2005). An interactive framework for developing simulation models of hospital accident and emergency services. In: Medical and care compunetics 2. Studies in health technology and informatics (114). IOS Press: Oxford, UK, pp. 277–283. ISBN 1586035207.
Comas M, Arrospide rigaA, Mar J, Sala M, Vilaprinyo´ E, et al. (2014). Budget impact analysis of switching to digital mammography in a population-based breast cancer screening program: A discrete event simulation model. PLoS One 9(5):e97459. doi:10.1371/journal.pone.0097459.
Demir E, Vasilakis C, Lebcir M and Southern D (2015). A simulation-based decision support tool for informing the management of patients with Parkinson’s disease. International Journal of Production Research 53(24):7238–7251.
Getsios D, Marton JP, Revankar N, Ward AJ, Wilke RJ, Rublee D, Ishak KJ and Xenakis JG (2013). Smoking cessation treatment and outcomes patterns simulation: A new framework for evaluating the potential health and economic impact of smoking cessation interventions. PharmacoEconomics 31(9):767–780.
Goodacre S, Sampson F, Stevenson M, Wailoo A, Sutton A, Thomas S, et al. (2006). Measurement of the clinical and cost-effectiveness of non-invasive diagnostic testing strategies for deep vein thrombosis. Health Technology Assessment 10(15):1–168.
Gunal M and Pidd M (2010). Discrete event simulation for performance modelling in health care: A review of the literature. Journal of Simulation 4(1):42–51.
Higashi H and Barendregt JJ (2011). Cost-effectiveness of total hip and knee replacements for the Australian population with osteoarthritis: Discrete-event simulation model. PLoS One 6(9):e25403. doi:10.1371/journal.pone.0025403.
Igarashi A, Goto R, Suwa K, Yoshikawa R, Ward AJ and Moller J (2016). Cost-effectiveness analysis of smoking cessation interventions in Japan using a discrete-event simulation. Applied Health Economics and Health Policy 14(1):77–87.
Katsaliaki K and Mustafee N (2011). Application of simulation within the healthcare context. Journal of the Operational Research Society 62(8):1431–1451.
Keeling D, Baglin T, Tait C, Watson H, Perry D, Baglin C, et al. (2011). Guidelines on oral anticoagulation with warfarin - fourth edition. British Journal of Haematology 154(3):311–324.
Macal CM and North MJ (2010). Tutorial on agent-based modelling and simulation. Journal of Simulation 4(3):151–162.
Martinez C, Rietbrock S, Bamber L and Cohen AT (2011). Incidence of venous thromboembolism (VTE) in the general population—VTE Epidemiology Group study. In: XXIII Conference of The International Society on Thrombosis and Haematosis (ISTH).
Mayorga ME, Reifsnider OS, Wheeler SB and Kohler RE (2014). A discrete event simulation model to estimate population level health and economic impacts of smoking cessation interventions. In: Tolk A, Diallo SY, Ryzhov IO, Yilmaz L, Buckley S, and Miller JA (eds). Proceedings of the 2014 Winter Simulation Conference, pp. 1257–1268.
MIMS. (n.d.). Prescription drug database. Retrieved March 1, 2014, from http://www.mims.co.uk/.
NICE. (2014a). Deep vein thrombosis: Introduction. Retrieved from http://www.nhs.uk/conditions/Deep-vein-thrombosis/Pages/Introduction.aspx.
NICE (2014b). Cost-effectiveness modelling using patient-level simulation. Retrieved 29 January 2016 from http://www.nicedsu.org.uk/Patientlevel-simulation-TSD(2892880).htm.
Noble SI., Shelley MD, Coles B, Williams SM, Wilcock A and Johnson MJ (2008). Management of venous thromboembolism in patients with advanced cancer: A systematic review and meta-analysis. The Lancet Oncology 9(6):577–584.
ONS (2013). Office of National Statistics (ONS) mid-2013 population estimates: Pivot table analysis tool for the United Kingdom. Last accessed 29 July 2014.
Payment by Result (2013). Payment by Results in the NHS: tariff for 2012 to 2013. Retrieved June 23, 2013, from https://www.gov.uk/government/publications/confirmation-of-payment-by-results-pbr-arrangements-for-2012-13.
Payment by Result (2014). Payment by results in the NHS: Tariff for 2013 to 2014. https://www.gov.uk/government/publications/payment-by-results-pbr-operational-guidance-and-tariffs. Last accessed 06 September 2016.
Pilgrim H and Chilcott J (2008). Assessment of a 7-day turnaround for the reporting of cervical smear results using discrete event simulation. Journal of the Operational Research Society 59(7):902–910.
Pilgrim H, Tappenden P, Chilcott J, Bending M, Trueman P, Shorthouse A and Tappenden J (2009). The costs and benefits of bowel cancer service developments using discrete event simulation. Journal of the Operational Research Society 60(10):1305–1314.
PSSRU. (2013). Unit Costs of Health and Social Care. Retrieved June 1, 2013, from http://www.pssru.ac.uk/project-pages/unit-costs/2013/#sections.
Rohleder TR, Lewkonia P, Bischak DP, Duffy P and Hendijani R (2011). Using simulation modeling to improve patient flow at an outpatient orthopaedic clinic. Health Care Management Science 14(2):135–145.
Rose P, James R., Chapman O, and Marshall S (2011). A real world evaluation to describe the characteristics, outcomes and resource use associated with patients being managed by a secondary care based anticoagulation service. Value in Health 14(7):A387–A388.
Scottish Intercollegiate Guidelines Network. (2010). Prevention and management of venous thromboembolism. Retrieved March 1, 2014, from http://www.sign.ac.uk/pdf/sign122.pdf.
Stahl EJ, Rattner D, Wiklund R, Lester J, Beinfeld M and Gazelle S (2004). Reorganizing the system of care surrounding laparoscopic surgery: A cost-effectiveness analysis using discrete event simulation. Medical Decision Making 24(5):461–471.
Verjan CR, Augusto V and Xie X (2013). Economic comparison between Hospital at Home and traditional hospitalization using a simulation-based approach. Journal of Enterprise Information Management 26(1):135–153.
Wells PS, Anderson DR, Rodger M, Forgie M, Kearon C, Dreyer J, et al. (2003). Evaluation of D-Dimer in the Diagnosis of Suspected Deep-Vein Thrombosis. The New England Journal of Medicine 349(13):1227–1235.
Winter M, Keeling D, Sharpen F, Cohen H and Vallance P (2005). Procedures for the outpatient management of patients with deep vein thrombosis. Clinical and Laboratory Haematology 27(1):61–66.
Acknowledgments
We would like to thank the following DVT Nurses for their valuable input towards establishing the DVT pathway: Jo Eggleston, University Hospitals NHS Trust; Emma Kinnaird, Bristol Royal Infirmary; Sarah Stockhall, Royal Liverpool University Hospital; Zara Lester, Royal Eye Infirmary; Carole Oughton, Broomfield Hospital and Marilyn Rees, Lansdowne Hospital.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
The input parameters associated with the DVT model
Estimate | Distribution | References | |
|---|---|---|---|
Demand | |||
Please specify prevalence rate of DVT within your population | 104.6 per 100,0000 population | Poisson | Martinez et al (2011) |
Please specify the proportion of patients with Cancer | 12.20% | Multinomial | Martinez et al (2011) |
Please specify the % of the diagnosed population with RECURRENT DVT | 19% | Multinomial | Martinez et al (2011) |
Please specify the annual increase for each year (1–5) of patient arrivals | User specified | Bernoulli | N/A |
Diagnosis | |||
What is the percentage of DVT patients arriving from the following sources? | |||
Percentage arriving from the GP Direct | User specified/Expert opinion | Multinomial | N/A |
Percentage arriving from Community Care | User specified/Expert opinion | Multinomial | N/A |
Percentage arriving from outpatients | User specified/Expert opinion | Multinomial | N/A |
Percentage arriving from accident and emergency (A&E) | User specified/Expert opinion | Multinomial | N/A |
What percentage of DVT patients will… | |||
Have a ‘Wells Score’ of greater than 2 | 46% | Bernoulli | Wells et al (2003) |
Have a ‘Wells Score’ of less than or equal to 2 | 54% | Bernoulli | Wells et al (2003) |
What percentage of DVT patients will have a… | |||
Positive ‘D-Dimer’ test result | 30% | Bernoulli | Wells et al (2003) |
Negative ‘D-Dimer’ test result | 70% | Bernoulli | Wells et al (2003) |
What % of people will have a | |||
Positive first ultrasound | 24% | Bernoulli | Goodacre et al (2006) |
Positive repeat ultrasound | 1% | Bernoulli | Goodacre et al (2006) |
What percentage of DVT patients will have | |||
Unprovoked | 44.80% | Multinomial | Martinez et al (2011) |
Provoked | 36.20% | Multinomial | Martinez et al (2011) |
Recurrent | 19.0% | Multinomial | Martinez et al (2011) |
Treatment | |||
What percentage of patients will receive the following options? | |||
Standard of Care (LMWH + Warfarin) | User specified/expert opinion | Bernoulli | N/A |
New treatment | User specified/expert opinion | Bernoulli | N/A |
Please define the % of patients and length of treatment | |||
Recurrent | Bauersachs et al (2010) | ||
3 months | 3% | Multinomial | |
6 months | 42% | Multinomial | |
12 months | 55% | Multinomial | |
Provoked | |||
3 months | 22% | Multinomial | |
6 months | 63% | Multinomial | |
12 months | 15% | Multinomial | |
Unprovoked | |||
3 months | 6% | Multinomial | |
6 months | 63% | Multinomial | |
12 months | 31% | Multinomial | |
Please indicate the length of treatment for cancer patients | |||
6 months | 100% | Fixed | Noble et al (2008) |
Please indicate the number of follow-up visits required within | Warfarin | ||
3 months of treatment | 9 | Poisson | Winter et al (2005), Rose et al (2011), Keeling et al (2011) |
6 months of treatment | 14 | Poisson | |
12 months of treatment | 24 | Poisson | |
Please define the number of days LMWH injections are required for patients on | LMWH | ||
LMWH | 8 days | Fixed | (Scottish Intercollegiate Guidelines Network, 2010) |
For those in ‘New Treatment’, please specify the number of first and follow-up visits for the following treatment durations: | New treatment | ||
3 months | 2 | Poisson | New treatment prescribing information (PI) |
6 months | 2 | Poisson | |
12 months | 2 | Poisson | |
On average how much staff time does it take to conduct a FIRST visit to the DVT clinic | User specified/expert opinion | Average | N/A |
Please indicate the % of time each type of staff is responsible | |||
Haematologist | User specified/expert opinion | Multinomial | N/A |
Nurse | User specified/expert opinion | Multinomial | N/A |
Radiologist | User specified/expert opinion | Multinomial | Expert opinion |
On average how much staff time does it take to conduct a FOLLOW-UP visit to the DVT Clinic | User specified/expert opinion | Average | Expert opinion |
Please indicate the percentage of time each type of staff is responsible | |||
Haematologist | User specified/expert opinion | Multinomial | Expert opinion |
Nurse | User specified/expert opinion | Multinomial | Expert opinion |
Radiologist | User specified/expert opinion | Multinomial | Expert opinion |
Costing | |||
Cost of FIRST visit to haematology/DVT clinic | £247 | Fixed | Payment by Result (2013) |
Cost of FOLLOW-UP visit to haematology/DVT clinic | £113 | Fixed | Payment by Result (2013) |
Cost of FIRST visit to community DVT clinic | User specified/expert opinion | Fixed | N/A |
Cost of FOLLOW-UP visit to community DVT clinic | User specified/expert opinion | Fixed | N/A |
New treatment price per tablet | £2.10 | Fixed | (MIMS) |
LMWH (NON-CANCER) cost per day | £9.77 | Fixed | (MIMS), assuming an average patient weight of 80 kg |
LMWH (CANCER) cost per day month 1 | £8.47 | Fixed | (MIMS) assuming an average weight of a patient 69–82 kg |
Warfarin cost per day | £0.07 | Fixed | (MIMS) |
Salary—hourly cost | |||
Haematologist | £139 | Fixed | PSSRU (2013) |
Nurse | £123 | Fixed | PSSRU (2013) |
Radiologist | £139 | Fixed | PSSRU (2013) |
Number of resources | |||
Haematologist | User specified/expert opinion | Fixed | N/A |
Nurse | User specified/expert opinion | Fixed | N/A |
Radiologist | User specified/expert opinion | Fixed | N/A |
Rights and permissions
About this article
Cite this article
Demir, E., Southern, D. Enabling better management of patients: discrete event simulation combined with the STAR approach. J Oper Res Soc 68, 577–590 (2017). https://doi.org/10.1057/s41274-016-0029-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1057/s41274-016-0029-y