Abstract
Materials used for orthopedic implants should not only have physical properties close to those of bones, durability and biocompatibility, but should also exhibit a sufficient degree of antibacterial functionality. Due to its excellent properties, titanium is still a widely used material for production of orthopedic implants, but the unmodified material exhibits poor antibacterial activity. In this work, the physicochemical characteristics, such as chemical composition, crystallinity, wettability, roughness, and release of Ti ions of the titanium surface modified with nanotubular layers were analyzed and its antibacterial activity against two biofilm-forming bacterial strains responsible for prosthetic joint infection (Staphylococcus aureus and Pseudomonas aeruginosa) was investigated. Electrochemical anodization (anodic oxidation) was used to prepare two types of nanotubular arrays with nanotubes differing in dimensions (with diameters of 73 and 118 nm and lengths of 572 and 343 nm, respectively). These two surface types showed similar chemistry, crystallinity, and surface energy. The surface with smaller nanotube diameter (TNT-73) but larger values of roughness parameters was more effective against S. aureus. For P. aeruginosa the sample with a larger nanotube diameter (TNT-118) had better antibacterial effect with proven cell lysis. Antibacterial properties of titanium nanotubular surfaces with potential in implantology, which in our previous work demonstrated a positive effect on the behavior of human gingival fibroblasts, were investigated in terms of surface parameters. The interplay between nanotube diameter and roughness appeared critical for the bacterial fate on nanotubular surfaces. The relationship of nanotube diameter, values of roughness parameters, and other surface properties to bacterial behavior is discussed in detail. The study is believed to shed more light on how nanotubular surface parameters and their interplay affect antibacterial activity.
Similar content being viewed by others
Introduction
Implant-associated infections are a relatively common problem accompanying the use of indwelling medical devices or tissue implants, mostly cardiac devices, or catheters1. Regarding orthopedic surgeries, periprosthetic joint infections (PJI) may occur after 1–5% of primary arthroplasties2. This is not a high incidence, however ongoing infections are persistent and progressive with difficult antibiotic treatment, often ending in revision surgeries with a high risk of re-infection (up to 50%)3, and potentially fatal outcomes4,5,6. These consequences represent a considerable burden not only for patients but also for the healthcare7,8,9. In addition, potential risk of infection grows along with the increasing number of arthroplasties10 due to population aging11, and increasing incidence of obesity12,13 and musculoskeletal system diseases14.
Microbial agents can be transferred to the implant surface during surgery or the wound closing during subsequent healing. Another way of infection transmission is from infected tissue located near the implant or by hematogenous dissemination15,16. A crucial pathological mechanism responsible for the development of PJI is the formation of a biofilm on the implant surface, which can be produced by one or more bacterial strains. This extracellular matrix (composed of extracellular polymeric substances) protects microorganisms from host immune defense and antibiotic treatment, making PJI demanding to manage17. Therefore, much attention is paid towards the development of mechanisms that will be effective in prevention of these infections, especially reducing biofilm formation18,19. Gram-positive, Gram-negative bacteria and also Candida and Mycobacterium species can act as the PJI causative agents20,21,22,23, and Staphylococcus aureus (the most common cause), Staphylococcus epidermidis and Pseudomonas aeruginosa are bacterial strains with high capacity to form biofilm on implant surfaces18,19.
Implants are prone to microbial colonization due to the disrupted local tissue response to the material caused by tissue injury and material implantation. Triggered acute and chronic inflammation along with the reaction to the foreign body with its consequences lead to impaired local immune defense (a locus minoris resistentiae)24,25. In addition, according to the “race for the surface” hypothesis, bacteria compete with human body cells to occupy the implant surface. If the cells first colonize the implant, the possibility of bacterial adherence and biofilm formation is reduced. On the other hand, the presence of the bacterial biofilm hinders cell adhesion and reduces their viability, which leads to impaired implant-tissue integration. An inadequately repaired tissue is not able to mediate sufficient immune system defense against microbes on the surface26. Therefore, there is a serious need for implants with surfaces that promote adhesion and viability of osteoblasts and at the same time prevent bacterial colonization and biofilm formation27.
Materials for the production of bone implants and artificial joints must possess appropriate physicochemical and biological characteristics28,29,30. Generally, different modifications of surface chemistry and/or morphology including various coatings are applied to functionalize surfaces in order to enhance osseointegration and antibacterial properties. Regarding implant bacterial colonization, appropriate modification must lead to an anti-adhesive, contact-killing and/or anti-biofilm surface while maintaining favorable biocompatibility31,32,33. As an example of a chemical strategy, coatings containing antibiotics, quorum-sensing quenchers, metal/metal nanoparticles or made from hydrogels are used31,34. To prevent a potential problem of antibiotic resistance, current studies have successfully tested a self-adaptive coating with regulated antibiotic release35 or a coating containing a different drug with antibacterial effect36. On the other hand, a physical approach, which involves, among other parameters, modification of the surface topography34, also shows promising results. Various techniques can be utilized to fabricate nanostructures with different morphologies33 (i.e. nanopillars, nanospikes, nanoneedles, or spinules37), which are often inspired by natural antibacterial patterns38,39. Besides, periodic40 and/or hierarchical micro/nano-structures41, Laser Induced Periodic Surface Structures (LIPSS), honeycomb-like structures, porous layers, nanotubes42, surface nanostructures of high aspect ratio43, and other geometries and formations have also been investigated for bacterial viability, growth, proliferation and/or retention42.
Besides stainless steel, cobalt-chromium alloys, ceramics and various polymers, titanium (mainly in the form of alloys) is commonly used for the manufacturing of orthopedic and dental implants44,45. This is due to its mechanical properties (high tensile strength to density ratio), poor electrical conductivity, chemical stability, high corrosion resistance, almost no immunological response45,46, low toxicity47 and good osseointegration capability48. Excellent biocompatibility of titanium can be attributed to a thin film of amorphous titanium dioxide that spontaneously forms on the surface of the metal when exposed to air48. However, the long-term process of implant integration can be less effective if the surrounding bone tissue is not of optimal quality and density, which may result in implant loosening and/or an increased risk of bacterial colonization24.
Nanotube arrays fabricated in the surface oxide layer of the titanium alloys have a positive impact on osseointegration at the each stage (adsorption of proteins, inflammatory cell adhesion/inflammatory response and adhesion of inflammatory cells, adhesion of additional relevant cells, and angiogenesis/osteogenesis), mainly due to their nanotopography49 that is very close to the nanostructure of bone50. The nanotubular layer also affects the behavior of bacterial cells, as nanotube dimensions, wettability, surface energy, surface charge, crystallinity, and roughness all play a role in surface colonization37.
Thus, it is possible to disrupt the initial adhesion of bacteria to the surface, which is considered a critical process in surface colonization, by appropriate surface characteristics51. Surface topography is the main determining factor for bacterial attachment52, on the other hand, it should maximally promote integration and formation of new tissue. Studies to date suggest that titanium surfaces with nanotubes around 70–100 nm in diameter are beneficial to the particular cells, thereby enhancing osteointegration and osteogenesis in vitro49,50,53,54,55 and also in vivo56,57,58,59. However, a plethora of studies testing antibacterial properties of nanotubular surfaces with different diameters have been conducted but results still remain inconclusive and often contradictory. It is known that nanotubes exhibit antibacterial properties upon contact, however, the interplay between surface parameters responsible for this effect has not yet been fully elucidated. Additionally, it has not yet been sufficiently clarified which of the parameters have the predominant influence. One of the contributing parameters is surface roughness. Microscale roughness is known to have a different (often an opposite) effect on bacterial adhesion than nanoscale roughness because it offers more attachment points and shelters60,61. In studies that have dealt with testing the antibacterial properties of surfaces, roughness was mostly described by arithmetic mean height Ra (Sa) and root mean square height Rq (Sq). However, these parameters only provide information about roughness amplitude and not about the shape and spatial distribution of surface features62, therefore they cannot adequately describe the relationship between roughness and bacterial behavior on the surface63,64. Also, an important thing is that surfaces with similar Ra (Sa) or Rq (Sq) values can possess significantly different topographies65,66, and therefore can differ in other roughness parameters (and vice versa), potentially having quite different effects on bacterial adhesion or retention. In a study by Stolzoff et al. titanium surfaces with similar Sq values but differing in values of number of summits in the measured area (Sds) and surface morphology showed different growth of S. aureus67. On the other hand, the surfaces in study by Sbricoli et al. had similar values of parameters Sds and developed interfacial area ratio (Sdr) but differed in Sa value, which affected Streptococcus sanguinis cells adhesion in vitro and also ex vivo68.
Electrochemical anodization (anodic oxidation) is a cost-effective method used for the production of highly ordered nanotubes on titanium surfaces69,70 offering a great possibility of modifying the nanotube morphology (diameter, length, spacing, wall thickness) simply by adjusting the process parameters (voltage, time, electrolyte composition)71,72. In this work, the anodization technique was utilized to prepare two types of arrays with nanotubes differing in their dimensions and surface roughness parameters, but with a similar surface energy in order to obtain antibacterial and/or bactericidal surface against two bacterial strains responsible for PJI (S. aureus and P. aeruginosa). The aim was to decide whether the influence of the Ti ions or mechanical properties of the surface are responsible for these effects. This work focuses on the interplay of physical and chemical factors affecting the bacterial adhesion and killing in order to thoroughly investigate the mechanisms lying beneath the antibacterial activity of titanium nanostructured surfaces and to determine which factor is potentially dominant in this process. Besides surface roughness and the release of titanium ions from nanotubular surfaces, chemical composition and crystallinity, and surface energy were taken into account.
To our knowledge, this is the first in vitro study of bacterial behavior on titanium surfaces possessing nanotubes of different diameters with comprehensively described parameters of surface roughness and including investigations of Ti ion release and effect.
Materials and methods
Sample preparation
Samples with the nanostructured surface were prepared as described previously73. Briefly, titanium foil (0.25 mm thickness, purity 99.7%, Sigma-Aldrich) was cut into pieces with size according to the application (see below). Prior to anodization, the pieces were degreased by brief boiling in a mixture of acetone and isopropanol (1:1), rinsed with deionized water and air-dried. Anodic oxidation was conducted in a conventional two-electrode electrochemical cell with a DC power supply (AX-6003P, Axiomet) at 20 V (with a sweep rate of 1 V/s) and room temperature for 75 min. A volume of 40 mL of aqueous (1 M H3PO4 and 0.15 M HF in deionized water) or non-aqueous (1 M H3PO4, 0.09 M HF and 11 vol% deionized water in ethylene glycol) electrolyte was used for preparation of two types of samples with surface nanotubes of different dimensions (TNT-118 or TNT-73, respectively). The anodized samples were immediately rinsed with distilled water, immersed in acetone for 15 min., rinsed again, sonicated in distilled water for 60 s and air-dried. Then, the samples were annealed at 450 °C in an oxygen atmosphere for 3 h and after cooling they were sonicated in distilled water for 60 s and air-dried. Degreased non-anodized titanium pieces were used as samples with unmodified surface.
Surface characterization
Nanotubular layer formation on the sample surfaces was evaluated by scanning electron microscopy using Versa 3D DualBeam microscope (FEI) and dimensions of nanotubes were determined using ImageJ software (National Institutes of Health, Bethesda, Maryland, USA). Thin lamella of the nanotubular layer was cut from the sample surface by focused ion beam technique in Helios 5 UC DualBeam microscope (Thermo Scientific). Structure and chemical composition of the surface layers was further examined using a scanning transmission electron microscope JEM-2100F from Jeol operated at 200 kV and commissioned with an EDS system XMax 80 from Oxford Instruments. The nanotubular layer crystallinity was analyzed by Raman spectroscopy using inVia Raman microscope (Renishaw). Parameters of surface roughness were determined using interferometer Talysurf CCI Lite (Taylor Hobson) and data were analyzed by the TalyMap Platinum software (Taylor Hobson). The data were obtained by independent measurements of three different samples of each surface type (unmodified Ti, TNT-118, TNT-73), on a 0.3 × 0.3 mm area in the center of each sample. The surface energy was calculated from measurement of contact angles by sessile drop method using See System E (Advex Instruments). Droplet (1 µL) of liquid was deposited on three different spots of sample surface and snapshots were taken after 5 s incubation at room temperature. The deposition of each drop was repeated ten times and contact angles (with an accuracy of ± 1°) were determined by a proprietary image analysis software as the average of measurements. Four different liquids (distilled water, ethylene glycol, glycerol, and 1-bromonaphthalene) were measured and the surface energy was calculated. The Ti ion release rate from the unmodified and modified Ti surfaces was also examined. Ti samples were immersed in 2 mL of Dulbecco’s Modified Eagle's Medium/Ham's Nutrient Mixture F12 supplemented with 10% fetal bovine serum and 1% penicillin/streptomycin at 37 °C for 24, 48 and 72 h (unmodified surfaces) and 24 and 72 h (modified surfaces). Ti-ion concentrations in the medium were subsequently measured by an inductively coupled plasma mass spectrometry (ICP-MS, Agilent 8900 ICP-MS/MS, Agilent Technologies) after digestion of media samples in nitric acid at 70 °C for 3 h.
Preparation of bacterial cultures
Bacterial strains of S. aureus (CCM 4223, ATCC 29,213) and P. aeruginosa (CCM 3955, ATCC 27,853) were purchased from the Czech Collection of Microorganisms (Brno, Czech Republic). After overnight cultivation at 37 °C on blood agar, bacterial inoculums were prepared by dilution of the cultures in appropriate liquid medium to the concentration of 1–2 × 106 colony forming unit per 1 mL (CFU/mL) using measurement of optical density at 600 nm.
Measurement of the surface antibacterial activity
The plate count method was performed in accordance with the ISO221961 and JIS Z 2801 standards. Two triplicates of samples of glass slide, unmodified Ti, TNT-118 and TNT-73 types (size 25 × 25 mm) were cleaned and disinfected first. Bacterial inoculums in volume of 100 µL diluted in Mueller–Hinton broth (Oxoid) was applied on each sample and covered with sterile plastic film (20 × 20 mm). The first triplicate of each sample type was washed immediately with physiological solution, which was collected (including plastic film), to obtain the value for 0 h and the remaining triplicate was incubated at 37 °C for 24 h (24 h value) and then washed with physiological solution. Collected solutions (100 µL) from each sample type were after decimal dilution inoculated on Petri dishes with plate count agar (LabMediaServis). The dishes were incubated at 37 °C for 24 h, the number of colonies on the dishes was counted and a colony forming unit per cm2 of sample surface (CFU/cm2) was determined for each sample. Cell growth rate after 24 h and bacterial growth inhibition percentage were calculated from these values. Cover glasses were used as control surfaces for bacterial growth.
Viability of adhered bacteria
Cleaned samples of each type (size 10 × 15 mm) were placed in 12-well plate and covered with 2 mL of the bacterial inoculums diluted in brain heart infusion medium (BHI, Sigma-Aldrich) with 1% glucose and incubated at 37 °C for 24 h. After 5 h, the inoculums were replaced with fresh BHI + 1% glucose and the cultivation continued overnight. After the incubation, the samples were gently washed with physiological solution. To stain the bacterial cells attached to the surface, LIVE/DEAD BacLight Bacterial Viability and Counting Kit (Invitrogen) was used according to manufacturer’s instructions. The samples were observed by inverted fluorescence microscope (OLYMPUS IX71, Olympus) at magnification 200×. The percentage of surface coverage by live or dead cells was determined for each sample from captured fluorescence images (green or red, respectively) by ImageJ software using color threshold function. Coverage values were calculated from 7 images of different viewing fields.
Bacterial cultivation in presence of Ti ions
The diluted bacterial inoculums were cultivated in Mueller–Hinton broth containing Ti ions (Titanium atomic absorption standard solution, Merck, cat. no. 274933) at the concentrations of 0.25, 0.5, 5, 25 and 50 mg/L. The cultures were incubated in a rotary shaker at 37 °C for 24 h, and then appropriate decimal dilutions of each culture were inoculated on Petri dishes with Mueller–Hinton agar. The dishes were incubated at 37 °C for 24 h, the number of colonies on the dishes was counted and CFU/mL of input culture was determined for each Ti ion concentration. The experiment was performed in triplicate.
Analysis of bacterial adhesion on nanostructured surfaces
The cleaned samples of each type (size 10 × 15 mm) were placed into 12-well plate, covered by a 2 mL of the bacterial inoculum diluted in BHI with 1% glucose and incubated at 37 °C for 5 h. The samples were gently washed three times with a physiological solution and bacteria attached to the surface were fixated in 2% glutaraldehyde for 1 h. The fixated samples were dehydrated by immersion in ethanol solutions with increasing ethanol concentration (30%, 50%, 70%, 80%, 90%, 95% and twice 100%), for 15 min in each solution. The surfaces containing cells were examined by the LYRA 3 scanning electron microscope (Tescan). The scans were obtained with the stage tilted at 25° to measure the level of bacterial adherence. Contact angles of the bacterial cells were determined for at least fourteen cells using ImageJ software. A contact angle was measured between the extended cell base (two points of the contact) and second line that was drawn from the contact point on the base line to the first contact point with the cell side surface (third point).
Bacterial biofilm formation
The samples of all types (size 10 × 15 mm) were covered with 2 mL of bacterial inoculum diluted to 106 CFU/mL in BHI medium + 1% glucose and incubated at 37 °C for 5 h. Then, the inoculum was replaced with fresh BHI + 1% glucose and the cultivation continued overnight. After incubation, the samples were gently washed with physiological solution and observed directly without fixation. Images were captured using a digital microscope VHX-5000 (Keyence) with high-resolution zoom lens VH-Z500R/Z500T (Keyence) and the percentage of surface coverage of each sample was determined from the captured images by the ImageJ software using the brightness threshold parameter. The coverage values were calculated from 5 viewing field images.
Statistical analysis
Statistical analyses were performed using the GraphPad software (Prism) for Windows. Student's t-test was used to analyze the results. Differences with p values less than 0.05 were considered statistically significant.
Results
Preparation and characterization of Ti nanotubular surfaces
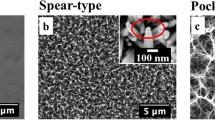
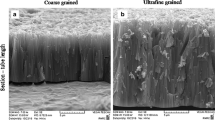
Two different electrolytes were used in the anodic oxidation process to obtain two types of surface nanotubes (NTs) differing in dimensions. The average diameter and length of NTs prepared in aqueous electrolyte (TNT-118) were 118 ± 9 nm and 343 ± 34 nm, respectively, whereas NTs prepared in non-aqueous electrolyte (TNT-73) had smaller diameter 73 ± 13 nm and higher length 572 ± 114 nm. SEM analysis showed that both sample types were covered by homogeneous nanotubular layer with highly ordered NTs (Fig. 1B,C; unmodified Ti for comparison Fig. 1A). The properties of the nanostructured surface that are related to the antibacterial effect were characterized. The surface energy (SE) of the anodized and annealed samples increased in comparison to bare Ti. The SE value for both types of samples was almost 54 mJ/m2 (TNT-118: 53.9 ± 2.1 mJ/m2, TNT-73: 53.5 ± 0.32 mJ/m2), whereas the unmodified Ti SE was 39.0 ± 5.9 mJ/m2. The surfaces with NTs were hydrophilic (contact angle 30°–40°), while the unmodified surface (contact angle ≈ 90°) was between hydrophilicity (< 90°) and hydrophobicity (> 90°)74.
The analysis of nanotubular layer chemistry by X-ray energy dispersive spectrometry revealed that both NT types combined a mixture of titanium oxides. A higher amount of TiO was found at the base of NTs, whereas as the distance from the matrix increased, the amount of TiO decreased slightly and, conversely, the amount of TiO2 was higher (Fig. 2, Table 1). Due to the post-anodization heat treatment of the anodized samples, TiO2 amorphous phase was completely transformed into a crystalline phase with a predominance of anatase, similarly as in our previous work73.
A lamella cut from the nanostructured surface for the determination of chemical composition of the nanotubular layer. ‘Ti’ indicates the titanium matrix, whereas ‘Pt’ indicates the upper part of the nanotubular layer. The positions of the areas taken for the X-ray energy dispersive spectrometry measurements are marked in red.
The parameters related to roughness of the profile (Table 2) and the surface (Table 3) were determined for all sample types. The profile roughness parameters were measured in perpendicular directions to investigate the symmetry of roughness features on the surfaces, and only the unmodified Ti surface showed significant differences in roughness parameters in the perpendicular directions (1. or 2. direction). Significant differences in the surface roughness parameters were found between the nanotubular surfaces and the unmodified Ti. Moreover, the TNT-73 was significantly different from the TNT-118 in terms of Sa, Sdr and Ssc parameters (Table 3).
The samples of the unmodified and modified Ti were incubated in medium to determine the Ti ion release rate. The ion amount relative to the surface area was determined to allow normalization of the material size. No significant difference (p > 0.05) was found in the concentration of Ti ions in the medium for the samples of bare Ti with different surface areas. Regarding nanostructured surfaces, the Ti ion release from the TNT-73 significantly decreased when compared to the unmodified Ti (p = 0.01) and the TNT-118 (p = 0.04), respectively. The Ti ion release rates from the samples are summarized in Table 4.
Antibacterial activity of nanotubular surfaces
The plate count method and LIVE/DEAD assay were used to examine antibacterial activity of samples with nanostructured surfaces. S. aureus and P. aeruginosa served as representatives of gram positive (G+) and gram negative (G−) bacteria, respectively. The plate count method was designed to investigate adhesion and growth ability of bacteria in relation to the sample surface area, in order to allow a quantitative comparison of the antibacterial effect of different materials. Results showed a significantly reduced growth of both strains after 24 h incubation on the samples with nanostructured surfaces compared to the unmodified Ti (p < 0.05). Similar results were obtained compared to glass slides (p < 0.05) (Fig. 3A). The percentage inhibition of bacterial growth on modified surfaces relating to the unmodified Ti was significantly increased (p < 0.01) for both strains. Bacterial growth was 50–60% and 80–90% lower for S. aureus and P. aeruginosa, respectively, compared to the unmodified Ti (Fig. 3B). There were no significant differences in bacterial growth between the unmodified Ti and glass slides and between the types of modified samples for both strains after this time period (p > 0.05). S. aureus growth after 24 h incubation was less than half on the modified surfaces compared to glass and the unmodified Ti. On the other hand, P. aeruginosa growth was more than sevenfold lower on the TNT-118 and almost 11-fold lower on the TNT-73. Thus, the nanostructured surfaces showed a greater effect on inhibiting the growth of gram-negative P. aeruginosa (Fig. 3C).
Bacterial growth and growth inhibition on samples with modified surfaces. (A) Comparison of bacterial CFU counts after 24 h incubation on different sample types (a glass slide as the control, the unmodified Ti sample, TNT-118, TNT-73). Statistically significant differences are indicated as *for p < 0.05 and **for p < 0.01. The differences between the nanostructured samples and a glass slide were similar as for bare Ti. (B) Percentage of relative bacterial growth inhibition on the samples with modified surfaces after 24 h. (C) Growth folds for different surfaces.
Bacterial viability was analyzed by the LIVE/DEAD assay, which can visualize live and dead cells directly on the examined surfaces using the fluorescent dyes SYTO9, which stains all cells, and propidium iodide, which stains dead cells. On the unmodified Ti and a glass slide, the number of live cells was higher than the number of dead cells for both strains. Total number of bacterial cells was significantly lower on the anodized and annealed samples (p < 0.05). The lowest number of viable cells of S. aureus was observed on the TNT-73, in contrast to P. aeruginosa, where the lowest number of viable cells was on the TNT-118 (Fig. 4A,B, Supplementary Table 1). For both bacterial strains the ratio of live to dead cells on TNT-118 was reversed compared to TNT-73, where the number of viable cells was higher than the number of dead cells (Fig. 4A,B, Supplementary Table 1). The number of dead cells was significantly higher on modified surfaces TNT-118 compared to bare Ti and glass slide (p < 0.05) (Fig. 4A,B).
Results of LIVE/DEAD assays and observation of bacterial adhesion and morphology. Upper left: LIVE/DEAD assay of S. aureus (A) and P. aeruginosa (B) on samples with four different surface types (glass slide, unmodified Ti, TNT-118, TNT-73). Results are expressed as percentage of the total image area. Upper right: Percentage of dead cells on four different surfaces after 24 h incubation. Statistically significant differences are indicated as **for p < 0.01 and ****for p < 0.0001. The differences between the nanostructured samples and a glass slide were similar to bare Ti. Lower: A top view observation of bacterial adhesion and morphology of S. aureus (A) and P. aeruginosa (B) on unmodified titanium surface, TNT-118 and TNT-73 using scanning electron microscopy. In the case of P. aeruginosa grown on the TNT-118 sample, cells with odd (abnormal) appearance were observed (yellow arrows).
Scanning electron microscopy (SEM) was used to investigate adhesion and the morphology of bacterial cells on unmodified and modified Ti surfaces. S. aureus cells cultivated on the anodized and annealed Ti samples showed a reduced tendency to form clustering arrangement characteristic for Staphylococci compared to bare Ti. It was observed that cells cultivated on the unmodified Ti began to produce an extracellular matrix that was barely visible on the modified samples (Fig. 4A). Certain cells of P. aeruginosa that grew on the TNT-118 showed odd (abnormal) appearance (spread shape and partial transparency) (Fig. 4B).
Amount of S. aureus death cells after 24 h incubation was twofold higher on the TNT-118 and two-thirds lower on the TNT-73 than on glass or the unmodified Ti. On the other hand, for P. aeruginosa, amount of the death cells on TNT-73 and TNT-118 were three and fivefold higher compared to glass and four to ninefold higher compared to bare Ti (Fig. 5). Thus, the TNT-118 surface has a significant effect on cell death, especially in the case of P. aeruginosa.
Bacterial viability after cultivation in the presence of Ti ions
Ti ion release rate from the modified samples were similar to the unmodified Ti and the amount of ions released after 24 h incubation was lower than 10 ng per milliliter (Table 4). To analyze the effect of Ti ions on bacterial cell viability, cultures of both strains were incubated in media containing ions at five different concentrations (0.25, 0.5, 5, 25 and 50 mg/L) that were higher than the amount released from the Ti samples. After 24 h incubation, no statistically significant differences in cell growth of both strains were found among all concentration or in comparison with a control (p > 0.05) (Fig. 6).
Bacterial morphology on nanotubular surfaces
Scanning electron microscopy of samples tilted at 25° was performed to examine variability in shape among cells incubated on different surfaces. S. aureus cells differed in their roundness, therefore cell contact angles between the cell wall and the surface were analyzed for each sample type (Fig. 7A). Results showed significant differences in bacterial cell contact angles among all three sample types (p < 0.01) (Fig. 7B). Considering the observed shape of P. aeruginosa cells, it was not possible to evaluate either this or other parameters.
Contact angles of bacterial cells with material surfaces. (A) Observation of bacterial adhesion and morphology of S. aureus on the unmodified titanium surface, TNT-118 and TNT-73 using scanning electron microscopy with samples tilted at 25°. (B) Determination of cell contact angles between the cell wall and the surface for each sample type. Statistically significant differences are indicated as **for p < 0.01 and ****for p < 0.0001.
Inhibition of biofilm formation on nanotubular surfaces
Regarding the results of cell morphology obtained via scanning electron microscopy, biofilm coverage on samples of four different surface types was evaluated for S. aureus (Fig. 8). Results showed that biofilm formation was significantly reduced on the nanostructured samples compared to bare Ti (p < 0.05) and the glass slide (p < 0.0001). The lowest biofilm coverage was found on the TNT-73, which correlates with reduced growth and viability of S. aureus on this surface type.
Measurement of biofilm coverage. (A) S. aureus biofilm coverage of samples with four different surface types (glass slide, the unmodified Ti, TNT-118, TNT-73). Results are expressed as the percentage of surface coverage. Statistically significant differences are indicated as *for p < 0.05. The differences between the nanostructured samples and glass slide were similar as for bare Ti. The percentage of surface coverage was 89.2 (± 2.0) on glass slide, 84.0 (± 8.8) on unmodified Ti, 70.4 (± 4.5) on the TNT-118 and 67.8 (± 4.2) on the TNT-73. (B) S. aureus biofilm formed after an overnight incubation on different surfaces (left). The evaluation of surface coverage using the brightness threshold parameter in the ImageJ software (right).
Discussion
Titanium is a very valuable material still widely used in the implantology. However, the antibacterial properties of pristine titanium are not sufficient despite the oxide film naturally present on the surface, which is otherwise a key factor of the biocompatibility of this material75. It is known that arrays of highly ordered nanotubes formed in the thickened oxide layer enhance the antibacterial effect of nanostructured titanium76, but it is still not completely clear which parameter is the most crucial for the antibacterial ability of the nanotubular surfaces37,77. In our work, the titanium foils possessing nanotubular arrays with two different nanotube diameters (73 nm and 118 nm) were fabricated as in our previous work, where behavior of human gingival fibroblasts on these nanotubular surfaces was examined73. The results of the study showed that the TNT-118 promotes cell viability and the TNT-73 supports cell adhesion. Both surface types positively affect cell morphology, as increased cell area and decreased stiffness were measured after cultivation on the nanotubular surfaces73. To complete the information panel, in this work, antibacterial activity was comprehensively investigated from the point of view of titanium ion release, surface roughness and topography, nanotube diameter and other physicochemical parameters to provide deeper insight into the effect of the nanotubular surface parameters on the bacterial behavior.
Adhesion of bacteria to the implant surface is considered to be the initial step in the pathogenesis of the prosthetic joint infection. The interactions between bacterial cells and the material are affected by properties of the cells (e.g. shape, hydrophilicity/hydrophobicity, surface charge, zeta potential, membrane composition and stiffness78), environmental factors (body fluid composition, shear flow stress, etc.) and material surface characteristics (morphology, topography, roughness, stiffness, chemistry, charge, wettability, and surface energy)51,79,80. Therefore, microbial attachment, and the subsequent onset of infection, can be significantly reduced by appropriate surface modifications. Based on the mechanism of action, surfaces may exhibit anti-adhesive and/or bactericidal properties63,81.
In our work, the antibacterial effect was significantly manifested when cells came into contact with the nanotubular arrays (Fig. 3A,B). Surface chemistry plays an important role in the antibacterial activity of nanotubular surfaces82. The top part of the nanotubes of both tested sample types contained TiO2 in a crystalline phase composed mainly of anatase (Fig. 2, Table 1), which enhances the antibacterial effect of the surface72,83,84. Heat-treatment and the crystallinity both impact surface hydrophilicity85, and thus contribute to the antibacterial properties86. This is also related to the surface energy (SE)84. Samples with both types of nanotubes showed increased SE (Chapter 3.1.) compared to the unmodified Ti, hence, they should support bacterial adhesion. However, in the process of bacterial adhesion, the SE of the bacterial cell wall must be taken into account, because bacterial adhesion is a complex process that is driven not only by the properties of the material surface and the liquid environment, but also by the physicochemical properties of the bacterial cells, where the SE of the cell wall makes a substantial contribution. For bacterial adhesion to be established, adhesion energy (consisting of the of the bacteria–solid, bacteria–liquid, and solid–liquid interfacial free energy contributions) must be negative. An important parameter is the value of the SE difference between the material and the cell wall within equal liquid environment, as a smaller value means more negative adhesion energy leading potentially to an increase in adhesion of the bacterial cells87,88.
In terms of the nanoscale, surface roughness as well as topography affect the surface SE, wettability, and bacterial adhesion77,89. The results of our study showed that the samples with nanotubular surfaces differ from the unmodified Ti and from each other significantly with respect to roughness parameters, with the TNT-73 having the largest values in the surface structure parameters (Table 3). In the literature, a roughness threshold with the Ra value of 0.2 μm is generally accepted for titanium surfaces, with lower values having likely no effect on the number of attached bacteria64,90,91. Our results show that all surface types have the Ra value at or below the threshold, with the lowest value for the unmodified Ti (Table 2), but all three sample types exhibit a difference in bacterial colonization (Figs. 3, 4). The Ra (Sa) and Rq (Sq) are the most widely used parameters to describe the surface roughness across studies. However, these parameters provide the information about surface texture, i.e. only in the vertical direction (height and depth). Therefore, it is more advisable to determine surface structure parameters (e.g. Sds, Sdr, Sdq, Ssc), as they allow to obtain a more accurate 3D image of the surface topography90. The TNT-73 is the most complex and structured of the three surfaces compared in our study, with height (Sa, Sz) and spatial (Sds) topographic features contributing to the extended overall developed area (Sdr)92,93. In general, an increased surface area promotes bacterial attachment and biofilm formation90,94. However, nanoscale roughness hinders adhesion of bacteria51 as it reduces the real contact area of the surface90,95. Our results confirm this fact, since the highest number of bacterial cells was observed on the unmodified Ti, which has the lowest surface area (Sdr), and also the lowest values of other surface structure parameters (Table 3). The Sdr value results from the values of number of summits in a measured area (Sds) and surface amplitude parameters Sa (arithmetic mean height of the surface), Sq (root mean square height of the surface) and Sz (maximum height of the surface)93,96,97. Due to their interconnection, there is a high correlation between parameters Sdr, Sdq (the value represents a root mean square gradient of the surface) and Ssc (arithmetic mean summit curvature)93,96,97. In our results, the unmodified Ti have the smallest values of Sdq and Ssc, indicating a smoother surface type, as it has flatter slopes of surface structures with more rounded tops. The TNT-73 samples have the largest values of these parameters resulting in a sharper surface, because the surface structures have steeper slopes with sharp-edged vertices98. Regarding titanium samples with the treated surfaces but without nanotubular arrays, the results of a study by D’Ercole et al. demonstrated an association of higher values of Sdr and Sdq (more articulated surfaces) with a smaller number of live bacteria. However, biofilm formation was positively correlated with surface wettability regardless of roughness parameters, which could be due to surface pre-coating with saliva99. On the other hand, a study by Pacha-Olivenza et al. showed that bacterial adhesion increased with increasing values of surface structure parameters90. However, the values ranged more in the micro scale, and the values of the surface with the highest bacterial cell coverage were ten times higher than the values of the surface structure parameters of the sample types in our study90. In addition, the parameter Sdr comprises also amplitude Sa and number of summits Sds, and the ratio of values of these parameters may also affect adhesion of bacteria rather than a value of Sdr alone. Moreover, a shape of surface structure can also contribute to bacterial adhesion92.
Roughness parameters can provide valuable information regarding not only bacterial adhesion but also the retention of bacterial cells. Rough surfaces possessing features in microscale can better protect the bacteria from shear flow forces than smooth ones, giving them enough time to establish irreversible attachment100. It is known that microscale valleys of roughness (in form of grooves or pits) can promote cell retention when they are close to microbial dimensions in width and depth61,101,102. In our work, values of the parameter Sz were 3.6, 4.0 and 4.5 μm for the unmodified Ti, TNT-118 and TNT-73, respectively, thus they fell into the microscale. Appropriate spacing between peaks of roughness can help accommodate cells103 as the increased contact area104 results in reduced adhesion energy105. Parameter Rsm (mean profile elements spacing) can describe average peak-to-peak distance, and in our results its values ranged from 5.7 to 7.3 μm. The ratio between parameters Rz (maximum height per section) and Rsm was calculated for all surface types to describe the relation between feature depth/feature width of the structures on their surfaces and bacterial colonization, as this aspect ratio affects the contact area between bacterial cells and the surface106. The value of the aspect ratio of the unmodified Ti was approximately twice as high than of the modified Ti, and the higher the number, the deeper the surface roughness structures. Therefore, the features of the surfaces are close to the dimensions of the bacterial cells (S. aureus diameter range from 0.5 to 1.5 μm, P. aeruginosa has about 0.5–1 µm in width and 1–5 µm in length107,108) and may facilitate the cell retention102,109,110. In some cases, roughness may positively affect retention rather than bacterial adhesion100. Therefore, roughness parameters should also be considered in relation to bacterial retention, as it is a crucial factor for biofilm formation111. Regarding biofilm formation, spatial (Sds) and hybrid (Ssc) parameters of surface roughness seem to be more indicative than amplitude parameters alone (Sa, Sq)112.
Differences in the values of roughness parameters may also explain the differences in bacterial cell shape observed by the SEM on both types of nanotubular surfaces and unmodified Ti, with S. aureus cells having the most rounded shape on the TNT-73 (Fig. 7). This sample type possesses the largest total surface area (Sdr) but offers the lowest real contact area as it has the highest values of Sa, Sq, Sds, Sdq and Ssc. Thus, the surface contains a large number of nanoscale peaks with steep slopes and rather sharper tops on which bacterial cells “sit”. According to the thermodynamic theories and models used to predict the energy of interaction between a bacterial cell and a surface in aqueous environment (X/DLVO, surface element integration technique, Derjaguin integration), the total free energy gain is lower on a rougher surface (TNT-73) than on a “flatter” surface with low values of the roughness parameters (bare Ti), therefore bacterial adhesion is much weaker on the rougher surface63,100. The initial adhesion of the cells is also significantly affected by the hydrodynamic conditions of the environment100, and since the S. aureus cells have a weaker contact with the TNT-73 surface, it can be inferred that the cells may roll off the surface under the fluid flow before they can establish irreversible attachment. Additionally, the TNT-73 sample offers the largest total surface area (plus less empty space as the nanotubes have a smaller diameter) that is negatively charged, causing electrostatic repulsion of negatively charged S. aureus cells113. This fact may also contribute to reduction of bacterial colonization. Hypothetically S. aureus cells exhibit a less spherical morphology on the TNT-118 than on the TNT-73 due to the wider nanotube diameter, thus wider gaps. Cells can slightly deform and elongate due to cell gravity to overcome inner pore emptiness and maximize the contact area to increase the total free energy gain63.
Surface roughness is one of the determinants of surface wettability, and also plays a key role in bacterial adhesion100. The degree of wettability can be deduced from the variation in the shape of the surface profile described by the ratio between Rp (mean peak height) and Rz. According to literature, the Rp/Rz ratio higher than 0.5 means that the roughness profile has rather sharp peaks, and a lower ratio indicates peaks with more rounded tops114,115, which is related to surface wettability, as rounded profile promotes dispersion of liquids116,117. However, our work showed opposite trends, as the nanotubular surfaces with a higher Rp/Rz ratio (just above the threshold between round and sharp peaks) exhibited higher hydrophilicity than the unmodified Ti with a lower Rp/Rz ratio. Although surface roughness is important to wettability, it is still a part of the topography profile.
It is generally accepted that roughness and hydrophilicity increase with increasing nanotube diameter58,77,88,118,119. However, some studies suggest that the effect of nanotube diameter on wettability may only manifest when the roughness is higher than 10 nm66,86,118,120, but does not reach the microscale level121. Additionally, it seems that increasing diameter still has some positive effect on wettability if roughness is similar65,122. Moreover, the surfaces with higher nanotube diameter and lower roughness and vice versa may exhibit similar hydrophilicity and SE123. Similarly, both types of the nanostructured surfaces used in our work did not show any significant difference in either hydrophilicity or SE. The TNT-118 has a larger diameter but lower values of roughness parameters compared to TNT-73, and thus an interplay may exist between higher/lower roughness and smaller/larger diameter, leading to similar wettability. It seems that in the case of nanotubular arrays surface diameter has a more pronounced effect on hydrophilicity than roughness. However, the contribution of post-anodization heat treatment must also be taken into consideration124.
Sample surfaces fabricated in our study differ in the diameter of nanotubes (73 and 118 nm for TNT-73 and TNT-118, respectively), a dimensional parameter that plays an important role in antibacterial activity77. Our results showed a higher number of dead cells of both S. aureus and P. aeruginosa on TNT-118 (Fig. 4, A, B). Several studies have demonstrated a statistically significant association of a higher antibacterial effect on both gram-negative and gram-positive bacterial species of nanotubes with a larger diameter86,88,118,119,121,122,125,126,127,128. Li et al. have formulated a hypothesis that the antibacterial ability of nanotubular surfaces initially increases and then decreases as nanotube diameter increases. Initially, the nanoscale roughness and hydrophilicity increase in accordance with increasing diameter, continuously enhancing the antibacterial ability. When the diameter reaches a certain dimension, the roughness approaches the micron level, which may be more likely to promote bacterial attachment77. However, results of our study do not support this hypothesis, because nanotubes with a larger diameter have lower roughness values (Tables 2, 3) and both nanotubular surfaces exhibited similar hydrophilicity73. Other studies have shown opposite results (higher antibacterial effect of nanotubes with a smaller diameter), which can be explained by the fact that multiple factors contribute to the bacteria–surface interactions. Discrepancies in the results can be attributed to differences in the parameters of the anodic oxidation process129 leading to nanostructured surfaces with slightly different physicochemical properties, as well as specific characteristics of bacterial strains72,88,118,119,121,126,130,131, and experimental design. Post-anodization heat treatment72,86,127,128, cultivation conditions such as length of incubation72,119,121,126,131,132,133, the use of UV light during incubation83,134, the use of (artificial) saliva123,130 or a simulated body fluid medium66, and other factors such as sterilization method66, UV treatment72,123, or gradient of nanotube diameters135 may also had a non-negligible effect on the results of antibacterial testing of nanotubular surfaces. Studies that simultaneously investigated biofilm coverage showed a correlation to results of anti-adhesion tests136 with most reduced formation of biofilm on nanotubes with larger diameter up to a certain value119,123,127. Moreover, these nanotubes manifested an effect at the gene level, as increased downregulation of genes associated with the initial adhesion, cell proliferation and clustering, and biofilm formation was observed88,119. A study of the gram-negative bacterium Shewanella oneidensis showed decreasing biofilm formation with increasing nanotube diameter, which correlated with decreasing roughness and effective surface area and increasing wettability120. However, in the case of our results, similar biofilm coverage was detected on both surface types (Fig. 8), even though the TNT-73 surface has a significantly larger effective surface area than the TNT-118 (Table 3). A possible explanation is that both surface types have similar SE and wettability73, and the nanotube diameter and roughness parameters play a negligible role in the biofilm formation of S. aureus. Other studies have also shown a correlation between lower S. aureus biofilm coverage and the higher wettability of nanotubular surfaces66,119. On the other hand, the results of a study by Lewandowska et al. did not confirm this relationship133.
In our experiments, the lowest number of live and dead (total) S. aureus cells was observed on the TNT-73 (Fig. 4A), and, interestingly, these results corresponded to the cell morphology observed on the material using SEM, where cells on this sample type had the lowest contact angle, therefore the most spherical shape (Fig. 7). In addition, low bacterial cell counts lead to reduced bacterial biofilm formation (Fig. 8), as either impaired cell adhesion and/or cell killing (both due to surface topography) are crucial for biofilm prevention137. In case of S. aureus, nanotubes with narrower diameter (73 nm) showed a better anti-adhesive and anti-proliferation effect, whereas nanotubes with a larger diameter (118 nm) were rather bactericidal (Fig. 4A). Liu et al.119 observed S. aureus cells with damaged cell walls after cultivation on a surface possessing nanotubes with diameter 97 nm and significantly reduced cell membrane integrity of cells cultivated on nanotubes with diameter 53 nm and 97 nm. Regarding P. aeruginosa, cells with a spread shape and partial transparency caused by lysis were observed on the TNT-118 (Fig. 4B), and also the lowest number of live cells and the highest number of dead cells were observed on this sample type. On the other hand, no lysed cells were found on TNT-73. It is well known that particular nanoscale surface topographies can cause damage to cell membranes by piercing upon contact, especially in the case of gram-negative bacteria138,139,140. In nature, this bactericidal surface ability is typical for nanopillar-structured cicada wings141. However, in the case of nanotubular topography, the rupture of bacterial cells is caused by protrusions of the tube walls, which affect osmotic pressures of the inner and outer subshells and stretching of the membrane over the nanotubular gaps. The larger the area of bacterium in contact with the surface, the greater the stretching of the membrane77,119. Nanotube diameter may therefore be a key parameter in killing bacteria because the TNT-118 nanotubes have wider inner gaps. This observation could also explain the bactericidal effect of the TNT-118 on S. aureus (Fig. 4A), as the cells appeared more stretched on this surface compared to TNT-73 (Fig. 7A).
The nanotubular surfaces had slightly different antibacterial effect on S. aureus compared to P. aeruginosa,which exhibited a lower cell growth (Fig. 3C) and a higher cell death (Fig. 5) on both nanotubular types. This difference can be attributed to the varying topography (roughness, diameter), as the other parameters (chemistry, crystallinity, SE, wettability) are similar, and also to differences between bacterial species in the physicochemical properties of the cells (size, shape, membrane composition and rigidity, etc.)141,142,143. Gram-negative bacteria have thinner cell walls than gram-positive bacteria, with a thinner peptidoglycan layer and are therefore less rigid and more susceptible to membrane damage144. Moreover, a study of gram-negative Escherichia coli revealed a significant downregulation of genes related to the structure of cell membranes after cultivation on titanium surfaces with a nanotube diameter of 100 nm88. Nevertheless, it should be taken into account that excessive cell death may be counterproductive as it can lead to a decrease in the antibacterial effectiveness of the surface. The excessive release of DNA and proteins from dead cells may further promote the initial adhesion of living bacteria86,145,146.
The release of Ti ions from the surface is one of the aspects of material biocompatibility, as it can negatively affect the integration of the implant with the bone, which can progress up to aseptic osteolysis47,147. Titanium ions are always released in a certain amount from unmodified Ti material and also from titanium surfaces modified by nanostructuring74. The question remains whether Ti ions in the amount released from nanotubular surfaces are involved in the antibacterial activity. In our study, the Ti ion concentration ranging from 250 µg/L to 50 mg/L was used to test the effect of Ti ions on the viability of S. aureus and P. aeruginosa. No significant difference was observed compared to the pure medium (Fig. 6). Several studies have demonstrated the antibacterial activity of Ti ions against various gram-positive and gram-negative bacteria species. However, the ion concentrations that exhibited a negative impact on the bacterial viability far exceeded the amount of ions that can be released from titanium surfaces, whether bare or nanostructured148,149,150,151. Our results showed that the concentration of Ti ions measured in the medium incubated with the TNT-73 sample was 1.71 µg/L/cm2/h, which was half that of the medium incubated with the pristine Ti foil (Table 4). The amount of ions released from unmodified titanium can range from 0.1 µg/L/cm2/h up to 17 µg/L/cm2/h, depending on various determinants152,153,154,155,156,157. Regarding the rate of ion release, the physicochemical properties of the material (e.g. active surface area) play an important role, in addition to the physicochemical characteristics of the environment, such as the composition and pH of surrounding body fluids, presence of bacteria, specific proteins, oxygen, etc.74,154,155,156,157,158,159,160,161,162,163,164. Among others, the microbial corrosion must be considered especially for dental implants with permanent bacterial contact165,166,167. The negative effects of bacterial activity can be accelerated after the formation of a microbial biofilm168. However, the results of our study showed that Ti ions in the amount released from the nanotubular surfaces should not affect the antibacterial properties of the surfaces.
A limitation of this study is the lack of investigation into the adhesion capacity of the nanotubular surfaces for various proteins. In relation to bacterial colonization of the implants, it is always necessary to consider the effect of surface properties on adsorption of proteins present in the surface environment, as this process mediates the initial adhesion of bacterial cells72. The layer of bound proteins alters physicochemical properties of the surface (e.g. topography, roughness, wettability), and besides, functional groups of proteins can enhance or inhibit cell adhesion130. Nanotubular surfaces fabricated via electrochemical anodization exhibit increased SE169, which can lead to increased protein adsorption66,123 and can grow along with the nanotube diameter58,121,169. However, studies by Kulkarni et al. showed that the total available area (given by the diameter and length of the nanotubes and the spacing between their tops) is more important for protein binding than the nanotube diameter itself170,171. Therefore, the surface with the highest available area (including the contribution of roughness) possesses the highest capacity for protein adsorption, which is in our case the TNT-73 (Table 3). In addition, protein parameters, especially size171 and charge170, play an important role in adhesion. Therefore, nanotubes with the same diameter can bind different proteins differently55.
Conclusion
Two types of nanotubular surfaces with a confirmed positive effect on the behavior of human gingival fibroblasts were used in this study. The surfaces, differing in nanotube diameter but possessing similar chemistry, crystallinity (predominant anatase phase), and surface energy showed different effect on bacterial behavior with respect to bacterial cell properties (e.g. membrane rigidity, composition, shape). A material with a smaller nanotube diameter (median 73 nm; TNT-73) but larger values of roughness parameters was more effective against S. aureus. SEM images of tilted samples showed that on this surface type, the spherical cells have the smallest cell contact angle, thus resulting in the smallest contact area, making it highly likely for them to roll off the surface under fluid flow. On the other hand, for P. aeruginosa the sample with a larger nanotube diameter (median 118 nm; TNT-118) exhibited a better antibacterial effect, as the cell lysis on this surface type was clearly visible in SEM images. Regarding the release of Ti ions into the medium, the surface with smaller nanotubes released half as much as unmodified Ti. However, no effect of Ti ions on bacterial viability was observed within the wide range of concentrations used. From the point of view of the physical parameters of nanotubular surfaces, the interplay between nanotube diameter and surface roughness is decisive for the fate of bacteria. However, it is always necessary to take into account the differences in the properties of the bacterial cells of the species used, the influence of the environment, and the experimental design.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- NTs:
-
Surface nanotubes
- PJI:
-
Periprosthetic joint infections
- Ra:
-
Arithmetic mean height
- Rp:
-
Mean peak height
- Rq:
-
Root mean square height
- Rsm:
-
Mean profile elements spacing
- Rz:
-
Maximum height per section
- Sa:
-
Arithmetic mean height of the surface
- Sdq:
-
Root mean square gradient of the surface
- Sdr:
-
Developed interfacial area ratio of the surface
- Sds:
-
Density of summits
- SE:
-
Surface energy
- SEM:
-
Scanning electron microscopy
- Sq:
-
Root mean square height of the surface
- Ssc:
-
Arithmetic mean summit curvature
- Sz:
-
Maximum height of the surface
- TNT-118:
-
Titanium with nanotubular array possessing nanotubes with diameter of 118 nm
- TNT-73:
-
Titanium with nanotubular array possessing nanotubes with diameter of 73 nm
References
VanEpps, J. S. & Younger, J. G. Implantable device-related infection. Shock 46, 597–608 (2016).
Esteban, J. & Gómez-Barrena, E. An update about molecular biology techniques to detect orthopaedic implant-related infections. EFORT Open Rev. 6, 93–100 (2021).
Cyphert, E. L., Zhang, N., Learn, G. D., Hernandez, C. J. & von Recum, H. A. Recent advances in the evaluation of antimicrobial materials for resolution of orthopedic implant-associated infections in vivo. ACS Infect. Dis. 7, 3125–3160 (2021).
Natsuhara, K. M., Shelton, T. J., Meehan, J. P. & Lum, Z. C. Mortality during total hip periprosthetic joint infection. J. Arthroplasty 34, S337–S342 (2019).
Drain, N. P. et al. High mortality after total knee arthroplasty periprosthetic joint infection is related to preoperative morbidity and the disease process but not treatment. J. Arthroplasty 37, 1383–1389 (2022).
Fischbacher, A. & Borens, O. Prosthetic-joint Infections: Mortality over the last 10 years. J. Bone Jt. Infect. 4, 198–202 (2019).
Pirisi, L., Pennestrì, F., Viganò, M. & Banfi, G. Prevalence and burden of orthopaedic implantable-device infections in Italy: A hospital-based national study. BMC Infect. Dis. 20, 337 (2020).
Mponponsuo, K. et al. Economic burden of surgical management of prosthetic joint infections following hip and knee replacements in Alberta, Canada: An analysis and comparison of two major urban centers. J. Hosp. Infect. S0195–6701(22), 00132–00133 (2022).
Premkumar, A. et al. Projected economic burden of periprosthetic joint infection of the hip and knee in the United States. J. Arthroplasty 36, 1484-1489.e3 (2021).
Shichman, I. et al. Projections and epidemiology of primary hip and knee arthroplasty in medicare patients to 2040–2060. JB JS Open Access 8, e22.00112 (2023).
Matsuoka, H., Nanmo, H., Nojiri, S., Nagao, M. & Nishizaki, Y. Projected numbers of knee and hip arthroplasties up to the year 2030 in Japan. J. Orthop. Sci. 28, 161–166 (2023).
Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 15, 288–298 (2019).
Powell, A., Teichtahl, A. J., Wluka, A. E. & Cicuttini, F. M. Obesity: A preventable risk factor for large joint osteoarthritis which may act through biomechanical factors. Br. J. Sports Med. 39, 4–5 (2005).
Hernigou, P. & Scarlat, M. M. Growth in musculoskeletal pathology worldwide: The role of Société Internationale de Chirurgie Orthopédique et de Traumatologie and publications. Int. Orthop. 46, 1913–1920 (2022).
Izakovicova, P., Borens, O. & Trampuz, A. Periprosthetic joint infection: Current concepts and outlook. EFORT Open Rev. 4, 482–494 (2019).
Rakow, A., Perka, C., Trampuz, A. & Renz, N. Origin and characteristics of haematogenous periprosthetic joint infection. Clin. Microbiol. Infect. 25, 845–850 (2019).
Staats, A., Li, D., Sullivan, A. C. & Stoodley, P. Biofilm formation in periprosthetic joint infections. Ann. Jt. 6, 43 (2021).
Davidson, D. J., Spratt, D. & Liddle, A. D. Implant materials and prosthetic joint infection: The battle with the biofilm. EFORT Open Rev. 4, 633–639 (2019).
Visperas, A., Santana, D., Klika, A. K., Higuera-Rueda, C. A. & Piuzzi, N. S. Current treatments for biofilm-associated periprosthetic joint infection and new potential strategies. J. Orthop. Res. 40, 1477–1491 (2022).
Peng, H.-M. et al. Microbiology of periprosthetic hip and knee infections in surgically revised cases from 34 centers in Mainland China. Infect. Drug Resist. 14, 2411–2418 (2021).
Benito, N. et al. The different microbial etiology of prosthetic joint infections according to route of acquisition and time after prosthesis implantation, including the role of multidrug-resistant organisms. J. Clin. Med. 8, 673 (2019).
Fröschen, F. S., Randau, T. M., Franz, A., Molitor, E. & Hischebeth, G. T. R. Microbiological profiles of patients with periprosthetic joint infection of the hip or knee. Diagnostics 12, 1654 (2022).
Papalini, C. et al. Prosthetic joint infection diagnosis applying the three-level European Bone and Joint Infection Society (EBJIS) approach. Eur. J. Clin. Microbiol. Infect. Dis. 41, 771–778 (2022).
Arciola, C. R., Campoccia, D. & Montanaro, L. Implant infections: Adhesion, biofilm formation and immune evasion. Nat. Rev. Microbiol. 16, 397–409 (2018).
Seebach, E. & Kubatzky, K. F. Chronic implant-related bone infections—Can immune modulation be a therapeutic strategy?. Front. Immunol. 10, 1724 (2019).
Shiels, S. M., Mangum, L. H. & Wenke, J. C. Revisiting the “race for the surface” in a pre-clinical model of implant infection. Eur. Cell Mater. 39, 77–95 (2020).
Chu, L. et al. Preferential colonization of osteoblasts over co-cultured bacteria on a bifunctional biomaterial surface. Front. Microbiol. 9, 2219 (2018).
Gobbi, S. J., Gobbi, V. J. & Rocha, Y. Requirements for selection/development of a biomaterial. Biomed. J. Sci. Tech. Res. 14, 10674–10679 (2019).
Huzum, B. et al. Biocompatibility assessment of biomaterials used in orthopedic devices: An overview (Review). Exp. Ther. Med. 22, 1315 (2021).
Ma, C., Du, T., Niu, X. & Fan, Y. Biomechanics and mechanobiology of the bone matrix. Bone Res. 10, 59 (2022).
Bohara, S. & Suthakorn, J. Surface coating of orthopedic implant to enhance the osseointegration and reduction of bacterial colonization: A review. Biomater. Res. 26, 26 (2022).
Han, X. et al. Surface modification techniques of titanium and titanium alloys for biomedical orthopaedics applications: A review. Colloids Surf. B: Biointerfaces 227, 113339 (2023).
Zhu, G., Wang, G. & Li, J. J. Advances in implant surface modifications to improve osseointegration. Mater. Adv. 2, 6901–6927 (2021).
Uneputty, A. et al. Strategies applied to modify structured and smooth surfaces: A step closer to reduce bacterial adhesion and biofilm formation. Colloid Interface Sci. Commun. 46, 100560 (2022).
Zhang, L. et al. Infection-responsive long-term antibacterial bone plates for open fracture therapy. Bioact. Mater. 25, 1–12 (2023).
Sun, T. et al. Simvastatin-hydroxyapatite coatings prevent biofilm formation and improve bone formation in implant-associated infections. Bioact. Mater. 21, 44–56 (2023).
Chopra, D., Gulati, K. & Ivanovski, S. Understanding and optimizing the antibacterial functions of anodized nano-engineered titanium implants. Acta Biomater. 127, 80–101 (2021).
Ge, X. et al. Cicada-inspired fluoridated hydroxyapatite nanostructured surfaces synthesized by electrochemical additive manufacturing. Mater. Des. 193, 108790 (2020).
Jenkins, J. et al. Antibacterial effects of nanopillar surfaces are mediated by cell impedance, penetration and induction of oxidative stress. Nat. Commun. 11, 1626 (2020).
Ge, X. et al. Bacterial responses to periodic micropillar array: Bacterial responses to periodic micropillar array. J. Biomed. Mater. Res. 103, 384–396 (2015).
Ge, X. et al. Micro/nano-structured TiO2 surface with dual-functional antibacterial effects for biomedical applications. Bioact. Mater. 4, 346–357 (2019).
Georgakopoulos-Soares, I., Papazoglou, E. L., Karmiris-Obratański, P., Karkalos, N. E. & Markopoulos, A. P. Surface antibacterial properties enhanced through engineered textures and surface roughness: A review. Colloids Surf. B: Biointerfaces 231, 113584 (2023).
Linklater, D. P. et al. High aspect ratio nanostructures kill bacteria via storage and release of mechanical energy. ACS Nano 12, 6657–6667 (2018).
Sarraf, M., Rezvani Ghomi, E., Alipour, S., Ramakrishna, S. & Liana, S. N. A state-of-the-art review of the fabrication and characteristics of titanium and its alloys for biomedical applications. Bio-des Manuf. 5, 371–395 (2022).
Szczęsny, G. et al. A review on biomaterials for orthopaedic surgery and traumatology: From past to present. Materials 15, 3622 (2022).
Kaur, M. & Singh, K. Review on titanium and titanium based alloys as biomaterials for orthopaedic applications. Mater. Sci. Eng. C. 102, 844–862 (2019).
Kim, K. T., Eo, M. Y., Nguyen, T. T. H. & Kim, S. M. General review of titanium toxicity. Int. J. Implant Dent. 5, 10 (2019).
Hanawa, T. Titanium-tissue interface reaction and its control with surface treatment. Front. Bioeng. Biotechnol. 7, 170 (2019).
Wu, B., Tang, Y., Wang, K., Zhou, X. & Xiang, L. Nanostructured titanium implant surface facilitating osseointegration from protein adsorption to osteogenesis: The example of TiO2 NTAs. IJN 17, 1865–1879 (2022).
Su, E. P. et al. Effects of titanium nanotubes on the osseointegration, cell differentiation, mineralisation and antibacterial properties of orthopaedic implant surfaces. Bone Jt. J. 100-B, 9–16 (2018).
Zheng, S. et al. Implication of surface properties, bacterial motility, and hydrodynamic conditions on bacterial surface sensing and their initial adhesion. Front. Bioeng. Biotechnol. 9, 643722 (2021).
Zhai, S. et al. Overview of strategies to improve the antibacterial property of dental implants. Front. Bioeng. Biotechnol. 11, 1267128 (2023).
Singhatanadgit, W., Toso, M., Pratheepsawangwong, B., Pimpin, A. & Srituravanich, W. Titanium dioxide nanotubes of defined diameter enhance mesenchymal stem cell proliferation via JNK- and ERK-dependent up-regulation of fibroblast growth factor-2 by T lymphocytes. J. Biomater. Appl. 33, 997–1010 (2019).
Oh, S. et al. Stem cell fate dictated solely by altered nanotube dimension. Proc. Natl. Acad. Sci. USA 106, 2130–2135 (2009).
Voltrova, B. et al. Different diameters of titanium dioxide nanotubes modulate Saos-2 osteoblast-like cell adhesion and osteogenic differentiation and nanomechanical properties of the surface. RSC Adv. 9, 11341–11355 (2019).
Wang, F., Li, C., Zhang, S. & Liu, H. Role of TiO2 nanotubes on the surface of implants in osseointegration in animal models: A systematic review and meta-analysis. J. Prosthodont. 29, 501–510 (2020).
Wang, N. et al. Effects of TiO2 nanotubes with different diameters on gene expression and osseointegration of implants in minipigs. Biomaterials 32, 6900–6911 (2011).
Lv, L. et al. The nanoscale geometry of TiO2 nanotubes influences the osteogenic differentiation of human adipose-derived stem cells by modulating H3K4 trimethylation. Biomaterials 39, 193–205 (2015).
Alves-Rezende, M. C. R. et al. The role of TiO2 nanotube surface on osseointegration of titanium implants: Biomechanical and histological study in rats. Microscopy Res. Tech. 83, 817–823 (2020).
Sterzenbach, T., Helbig, R., Hannig, C. & Hannig, M. Bioadhesion in the oral cavity and approaches for biofilm management by surface modifications. Clin. Oral Invest. 24, 4237–4260 (2020).
Verran, J., Packer, A., Kelly, P. J. & Whitehead, K. A. Use of the atomic force microscope to determine the strength of bacterial attachment to grooved surface features. J. Adhes. Sci. Technol. 24, 2271–2285 (2010).
Crawford, R. J., Webb, H. K., Truong, V. K., Hasan, J. & Ivanova, E. P. Surface topographical factors influencing bacterial attachment. Adv. Colloid Interface Sci. 179–182, 142–149 (2012).
Wu, S., Zhang, B., Liu, Y., Suo, X. & Li, H. Influence of surface topography on bacterial adhesion: A review (Review). Biointerphases 13, 060801 (2018).
Wassmann, T., Kreis, S., Behr, M. & Buergers, R. The influence of surface texture and wettability on initial bacterial adhesion on titanium and zirconium oxide dental implants. Int. J. Implant Dent. 3, 32 (2017).
Kingsak, M., Maturavongsadit, P., Jiang, H. & Wang, Q. Cellular responses to nanoscale substrate topography of TiO2 nanotube arrays: Cell morphology and adhesion. Biomater. Transl. 3, 221–233 (2022).
Kummer, K. M. et al. Effects of different sterilization techniques and varying anodized TiO2 nanotube dimensions on bacteria growth. J. Biomed. Mater. Res. 101B, 677–688 (2013).
Stolzoff, M. et al. Decreased bacterial growth on titanium nanoscale topographies created by ion beam assisted evaporation. IJN 12, 1161–1169 (2017).
Sbricoli, L. et al. Bacterial adhesion to grade 4 and grade 5 turned and mildly acid-etched titanium implant surfaces: An in vitro and ex vivo study. Appl. Sci. 11, 7185 (2021).
Fu, Y. & Mo, A. A review on the electrochemically self-organized titania nanotube arrays: Synthesis, modifications, and biomedical applications. Nanoscale Res. Lett. 13, 187 (2018).
Zakir, O. et al. A review on TiO2 nanotubes: Synthesis strategies, modifications, and applications. J. Solid State Electrochem. 27, 2289–2307 (2023).
Khudhair, D. et al. Anodization parameters influencing the morphology and electrical properties of TiO2 nanotubes for living cell interfacing and investigations. Mater. Sci. Eng.: C 59, 1125–1142 (2016).
Aguirre Ocampo, R. et al. Effect of surface characteristics on the antibacterial properties of titanium dioxide nanotubes produced in aqueous electrolytes with carboxymethyl cellulose. J. Biomed. Mater. Res. 109, 104–121 (2021).
Vrchovecká, K., Kuta, J., Uher, M., Přibyl, J. & Pávková, G. M. Effect of titanium nanostructured surface on fibroblast behavior. J. Biomed. Mater. Res. 111, 1333–1343 (2023).
Vrchovecká, K. et al. A release of Ti-ions from nanostructured titanium oxide surfaces. Surf. Interfaces 29, 101699 (2022).
Pesode, P. A. & Barve, S. B. Recent advances on the antibacterial coating on titanium implant by micro-Arc oxidation process. Mater. Today: Proc. 47, 5652–5662 (2021).
Liu, J. et al. Nano-modified titanium implant materials: A way toward improved antibacterial properties. Front. Bioeng. Biotechnol. 8, 576969 (2020).
Li, Y. et al. Enhanced antibacterial properties of orthopedic implants by titanium nanotube surface modification: A review of current techniques. IJN 14, 7217–7236 (2019).
Ivanova, E. P. et al. Impact of nanoscale roughness of titanium thin film surfaces on bacterial retention. Langmuir 26, 1973–1982 (2010).
Kreve, S. & Reis, A. C. D. Bacterial adhesion to biomaterials: What regulates this attachment? A review. Jpn. Dent. Sci. Rev. 57, 85–96 (2021).
Ramachandran, B., & Muthuvijayan, V. Surface engineering approaches for controlling biofilms and wound infections. In ACS Symposium Series (eds Rathinam, N. K., Sani, R. K.) 101–123 (American Chemical Society, 2019) [cited 2023 Dec 18]. https://doi.org/10.1021/bk-2019-1323.ch005
Yang, X. et al. Antibacterial surfaces: Strategies and applications. Sci. China Technol. Sci. 65, 1000–1010 (2022).
Puckett, S. D., Taylor, E., Raimondo, T. & Webster, T. J. The relationship between the nanostructure of titanium surfaces and bacterial attachment. Biomaterials 31, 706–713 (2010).
Li, H. et al. Antibacterial activity of TiO2 nanotubes: Influence of crystal phase, morphology and Ag deposition. Appl. Surf. Sci. 284, 179–183 (2013).
Mazare, A. et al. Corrosion, antibacterial activity and haemocompatibility of TiO2 nanotubes as a function of their annealing temperature. Corros. Sci. 103, 215–222 (2016).
Xue, J. et al. The surface wettability of TiO2 nanotube arrays: Which is more important—Morphology or chemical composition?. J. Porous Mater. 26, 91–98 (2019).
Ercan, B., Taylor, E., Alpaslan, E. & Webster, T. J. Diameter of titanium nanotubes influences anti-bacterial efficacy. Nanotechnology 22, 295102 (2011).
Zhang, X. et al. Quantitatively predicting bacterial adhesion using surface free energy determined with a spectrophotometric method. Environ. Sci. Technol. 49, 6164–6171 (2015).
Ji, X. et al. Different antibacterial mechanisms of titania nanotube arrays at various growth phases of E. coli. Trans. Nonferrous Met. Soc. China 31, 3821–3830 (2021).
Yu, J., Zhou, M., Zhang, L. & Wei, H. Antibacterial adhesion strategy for dental titanium implant surfaces: From mechanisms to application. JFB 13, 169 (2022).
Pacha-Olivenza, M. Á. et al. Relevance of topographic parameters on the adhesion and proliferation of human gingival fibroblasts and oral bacterial strains. BioMed Res. Int. 2019, 1–13 (2019).
Wiessner, A. et al. In vivo biofilm formation on novel PEEK, titanium, and zirconia implant abutment materials. IJMS 24, 1779 (2023).
Annunziata, M. et al. Bacterial adhesion to direct laser metal formed and mildly acid etched implant surfaces. Surf. Coat. Technol. 328, 390–397 (2017).
Pawlus, P., Reizer, R. & Wieczorowski, M. Functional importance of surface texture parameters. Materials 14, 5326 (2021).
Souza, J. G. S. et al. Targeting implant-associated infections: Titanium surface loaded with antimicrobial. iScience 24, 102008 (2021).
Lüdecke, C. et al. Nanorough titanium surfaces reduce adhesion of Escherichia coli and Staphylococcus aureus via nano adhesion points. Colloids Surf. B: Biointerfaces 145, 617–625 (2016).
Świercz, R. & Oniszczuk-Świercz, D. Experimental investigation of surface layer properties of high thermal conductivity tool steel after electrical discharge machining. Metals 7, 550 (2017).
Pawlus, P., Reizer, R. & Zelasko, W. Prediction of parameters of equivalent sum rough surfaces. Materials 13, 4898 (2020).
Dudás, I. & Varga, G. 3D topography for environmentally friendly machined surfaces. J. Phys.: Conf. Ser. 13, 24–27 (2005).
D’Ercole, S. et al. A novel 3D titanium surface produced by selective laser sintering to counteract Streptococcus oralis Biofilm Formation. Appl. Sci. 11, 11915 (2021).
Cheng, Y., Feng, G. & Moraru, C. I. Micro- and nanotopography sensitive bacterial attachment mechanisms: A review. Front. Microbiol. 10, 191 (2019).
Whitehead, K. A. & Verran, J. The effect of surface topography on the retention of microorganisms. Food Bioproducts Process. 84, 253–259 (2006).
Whitehead, K. A., Colligon, J. & Verran, J. Retention of microbial cells in substratum surface features of micrometer and sub-micrometer dimensions. Colloids Surf. B: Biointerfaces 41, 129–138 (2005).
Lorenzetti, M. et al. The influence of surface modification on bacterial adhesion to titanium-based substrates. ACS Appl. Mater. Interfaces 7, 1644–1651 (2015).
Seddiki, O., Harnagea, C., Levesque, L., Mantovani, D. & Rosei, F. Evidence of antibacterial activity on titanium surfaces through nanotextures. Appl. Surf. Sci. 308, 275–284 (2014).
Katsikogianni, M. & Missirlis, Y. Concise review of mechanisms of bacterial adhesion to biomaterials and of techniques used in estimating bacteria-material interactions. ECM 8, 37–57 (2004).
Meinshausen, A.-K. et al. Aspect ratio of nano/microstructures determines Staphylococcus aureus adhesion on PET and titanium surfaces. J. Appl. Microbiol. 131, 1498–1514 (2021).
Akanbi, O. E., Njom, H. A., Fri, J., Otigbu, A. C. & Clarke, A. M. Antimicrobial susceptibility of Staphylococcus aureus isolated from recreational waters and beach sand in Eastern Cape Province of South Africa. IJERPH 14, 1001 (2017).
Diggle, S. P. & Whiteley, M. Microbe profile: Pseudomonas aeruginosa: Opportunistic pathogen and lab rat: This article is part of the Microbe Profiles collection. Microbiology 166, 30–33 (2020).
Whitehead, K. A. & Verran, J. The effect of surface properties and application method on the retention of Pseudomonas aeruginosa on uncoated and titanium-coated stainless steel. Int. Biodeterior. Biodegrad. 60, 74–80 (2007).
Pellegrino, L., Kriem, L. S., Robles, E. S. J. & Cabral, J. T. Microbial response to micrometer-scale multiaxial wrinkled surfaces. ACS Appl. Mater. Interfaces 14, 31463–31473 (2022).
Whitehead, K. A. & Verran, J. Formation, architecture and functionality of microbial biofilms in the food industry. Curr. Opin. Food Sci. 2, 84–91 (2015).
Flausino, J. S. et al. Biofilm formation on different materials for tooth restoration: Analysis of surface characteristics. J. Mater. Sci. 49, 6820–6829 (2014).
Gross, M., Cramton, S. E., Götz, F. & Peschel, A. Key role of teichoic acid net charge in Staphylococcus aureus colonization of artificial surfaces. Infect. Immun. 69, 3423–3426 (2001).
Whitehead, S. A., Shearer, A. C., Watts, D. C. & Wilson, N. H. F. Comparison of methods for measuring surface roughness of ceramic. J. Oral Rehabilit. 22, 421–427 (1995).
Whitehead, S. A., Shearer, A. C., Watts, D. C. & Wilson, N. H. F. Comparison of two stylus methods for measuring surface texture. Dent. Mater. 15, 79–86 (1999).
Braz, J. K. F. S. et al. Plasma nitriding under low temperature improves the endothelial cell biocompatibility of 316L stainless steel. Biotechnol. Lett. 41, 503–510 (2019).
Nunes Filho, A. et al. Titanium surface chemical composition interferes in the Pseudomonas aeruginosa biofilm formation. Artif. Organs 42, 193–199 (2018).
Peng, Z. et al. Dual effects and mechanism of TiO2 nanotube arrays in reducing bacterial colonization and enhancing C3H10T1/2 cell adhesion. IJN 8, 3093 (2013).
Liu, P. et al. Early antimicrobial evaluation of nanostructured surfaces based on bacterial biological properties. ACS Biomater. Sci. Eng. 8, 4976–4986 (2022).
Anitha, V. C. et al. Biofilm formation on a TiO2 nanotube with controlled pore diameter and surface wettability. Nanotechnology 26, 065102 (2015).
Xu, Z. et al. Enhanced human gingival fibroblast response and reduced Porphyromonas gingivalis adhesion with titania nanotubes. BioMed Res. Int. 2020, 1–10 (2020).
Simi, V. S. & Rajendran, N. Influence of tunable diameter on the electrochemical behavior and antibacterial activity of titania nanotube arrays for biomedical applications. Mater. Charact. 129, 67–79 (2017).
Kobayashi, M. et al. The effect of ultraviolet treatment on TiO2 nanotubes: A study of surface characteristics, bacterial adhesion, and gingival fibroblast response. Metals 12, 80 (2022).
Shin, D. H., Shokuhfar, T., Choi, C. K., Lee, S.-H. & Friedrich, C. Wettability changes of TiO2 nanotube surfaces. Nanotechnology 22, 315704 (2011).
Draghi, L., Preda, V., Moscatelli, M., Santin, M. & Chiesa, R. Gentamicin-loaded TiO2 nanotubes as improved antimicrobial surfaces for orthopedic implants. Front. Mater. 7, 233 (2020).
Rajeswari, S., Nandini, V., Perumal, A. & Gowda, T. Influence of titania nanotubes diameter on its antibacterial efficacy against periodontal pathogens: An In vitro analysis. J. Pharm. Bioallied Sci. 13, 284 (2021).
Lin, W. et al. Inhibited bacterial biofilm formation and improved osteogenic activity on gentamicin-loaded titania nanotubes with various diameters. IJN 9, 1215–1230 (2014).
Xu, Z. et al. Increased mesenchymal stem cell response and decreased Staphylococcus aureus adhesion on titania nanotubes without pharmaceuticals. BioMed Res. Int. 2015, 1–9 (2015).
İzmir, M. & Ercan, B. Anodization of titanium alloys for orthopedic applications. Front. Chem. Sci. Eng. 13, 28–45 (2019).
Narendrakumar, K. et al. Adherence of oral streptococci to nanostructured titanium surfaces. Dent. Mater. 31, 1460–1468 (2015).
Kulkarni, M. et al. Interaction of nanostructured TiO2 biointerfaces with stem cells and biofilm-forming bacteria. Mater. Sci. Eng.: C. 77, 500–507 (2017).
Shi, X. et al. Antibacterial activities of TiO2 nanotubes on Porphyromonas gingivalis. RSC Adv. 5, 34237–34242 (2015).
Lewandowska, Ż et al. The evaluation of the impact of titania nanotube covers morphology and crystal phase on their biological properties. J. Mater. Sci.: Mater. Med. 26, 163 (2015).
Zhao, C. et al. Preparation and antibacterial activity of titanium nanotubes loaded with Ag nanoparticles in the dark and under the UV light. Appl. Surf. Sci. 280, 8–14 (2013).
Song, R. et al. Facile construction of structural gradient of TiO2 nanotube arrays on medical titanium for high throughput evaluation of biocompatibility and antibacterial property. ACS Appl. Bio Mater. 1, 1056–1065 (2018).
Feng, E. et al. Improved osteogenic activity and inhibited bacterial biofilm formation on andrographolide-loaded titania nanotubes. Ann. Transl. Med. 8, 987–987 (2020).
Li, W., Thian, E. S., Wang, M., Wang, Z. & Ren, L. Surface design for antibacterial materials: From fundamentals to advanced strategies. Adv. Sci. 8, 2100368 (2021).
Wandiyanto, J. V. et al. Outsmarting superbugs: Bactericidal activity of nanostructured titanium surfaces against methicillin- and gentamicin-resistant Staphylococcus aureus ATCC 33592. J. Mater. Chem. B 7, 4424–4431 (2019).
Lee, S. W., Phillips, K. S., Gu, H., Kazemzadeh-Narbat, M. & Ren, D. How microbes read the map: Effects of implant topography on bacterial adhesion and biofilm formation. Biomaterials 268, 120595 (2021).
Yang, X. et al. Recent progress on bioinspired antibacterial surfaces for biomedical application. Biomimetics 7, 88 (2022).
Song, F., Koo, H. & Ren, D. Effects of material properties on bacterial adhesion and biofilm formation. J. Dent. Res. 94, 1027–1034 (2015).
San-Martin-Galindo, P. et al. Modulation of virulence factors of Staphylococcus aureus by nanostructured surfaces. Mater. Des. 208, 109879 (2021).
Ghilini, F., Pissinis, D. E., Miñán, A., Schilardi, P. L. & Diaz, C. How functionalized surfaces can inhibit bacterial adhesion and viability. ACS Biomater. Sci. Eng. 5, 4920–4936 (2019).
Harper, C. E. & Hernandez, C. J. Cell biomechanics and mechanobiology in bacteria: Challenges and opportunities. APL Bioeng. 4, 021501 (2020).
Morales-García, A. L. et al. The role of extracellular DNA in microbial attachment to oxidized silicon surfaces in the presence of Ca2+ and Na+. Langmuir 37, 9838–9850 (2021).
Desai, S., Sanghrajka, K. & Gajjar, D. High adhesion and increased cell death contribute to strong biofilm formation in Klebsiella pneumoniae. Pathogens 8, 277 (2019).
Biguetti, C. C. et al. Effects of titanium corrosion products on in vivo biological response: A basis for the understanding of osseointegration failures mechanisms. Front. Mater. 8, 651970 (2021).
Weller, J. et al. The role of bacterial corrosion on recolonization of titanium implant surfaces: An in vitro study. Clin. Implant Dent. Relat. Res. 24, 664–675 (2022).
Vaidya, M., McBain, A. J., Banks, C. E. & Whitehead, K. A. Single and combined antimicrobial efficacies for nine metal ion solutions against Klebsiella pneumoniae, Acinetobacter baumannii and Enterococcus faecium. Int. Biodeterior. Biodegrad. 141, 39–43 (2019).
Yu, T. S. Effect of titanium-ion on the growth of various bacterial species. J. Microbiol. 42, 47–50 (2004).
Park, S. M., Kim, H. S. & Yu, T. S. Effect of titanium ion and resistance encoding plasmid of Pseudomonas aeruginosa ATCC 10145. J. Microbiol. 44, 255–262 (2006).
Punset, M. et al. Citric acid passivation of titanium dental implants for minimizing bacterial colonization impact. Coatings 11, 214 (2021).
Gil, F. J., Sánchez, L. A., Espías, A. & Planell, J. A. In vitro corrosion behaviour and metallic ion release of different prosthodontic alloys. Int. Dent. J. 49, 361–367 (1999).
Joseph, L. A., Israel, O. K. & Edet, E. J. Comparative evaluation of metal ions release from titanium and Ti–6Al–7Nb into bio-fluids. Dent. Res. J. 6, 7–11 (2009).
Mutlu-Sagesen, L., Ergun, G. & Karabulut, E. Ion release from metal-ceramic alloys in three different media. Dent. Mater. J. 30, 598–610 (2011).
Fage, S. W., Muris, J., Jakobsen, S. S. & Thyssen, J. P. Titanium: A review on exposure, release, penetration, allergy, epidemiology, and clinical reactivity. Contact Dermat. 74, 323–345 (2016).
Hirayama, T. et al. Ion release from casts of commercially pure titanium in mixed solutions of organic acids contained in human saliva. J. Jpn. Prosthodont. Soc. 52, 501–506 (2008).
Strietzel, R., Hösch, A., Kalbfleisch, H. & Buch, D. In vitro corrosion of titanium. Biomaterials 19, 1495–1499 (1998).
Koike, M. & Fujii, H. The corrosion resistance of pure titanium in organic acids. Biomaterials 22, 2931–2936 (2001).
Koike, M. & Fujii, H. In vitro assessment of corrosive properties of titanium as a biomaterial. J. Oral Rehabilit. 28, 540–548 (2001).
Nakagawa, M., Matsuya, S. & Udoh, K. Corrosion behavior of pure titanium and titanium alloys in fluoride-containing solutions. Dent. Mater. J. 20, 305–314 (2001).
Okazaki, Y. & Gotoh, E. Comparison of metal release from various metallic biomaterials in vitro. Biomaterials 26, 11–21 (2005).
Yu, F., Addison, O., Baker, S. J. & Davenport, A. J. Lipopolysaccharide inhibits or accelerates biomedical titanium corrosion depending on environmental acidity. Int. J. Oral Sci. 7, 179–186 (2015).
Yu, X. et al. Osteoclast-mediated biocorrosion of pure titanium in an inflammatory microenvironment. Mater. Sci. Eng.: C. 119, 111610 (2021).
Noumbissi, S., Scarano, A. & Gupta, S. A literature review study on atomic ions dissolution of titanium and its alloys in implant dentistry. Materials 12, 368 (2019).
Dini, C. et al. Progression of bio-tribocorrosion in implant dentistry. Front. Mech. Eng. 6, 1 (2020).
Xu, L., Yu, X., Chen, W., Zhang, S. & Qiu, J. Biocorrosion of pure and SLA titanium surfaces in the presence of Porphyromonas gingivalis and its effects on osteoblast behavior. RSC Adv. 10, 8198–8206 (2020).
Costa, R. C. et al. Correction to: Microbial corrosion in titanium-based dental implants: How tiny bacteria can create a big problem?. J. Bio Tribo. Corros. 7, 151 (2021).
Kulkarni, M. et al. Wettability studies of topologically distinct titanium surfaces. Colloids Surf. B: Biointerfaces 129, 47–53 (2015).
Kulkarni, M. et al. Protein interactions with layers of TiO2 nanotube and nanopore arrays: Morphology and surface charge influence. Acta Biomater. 45, 357–366 (2016).
Kulkarni, M. et al. Binding of plasma proteins to titanium dioxide nanotubes with different diameters. IJN 10, 1359 (2015).
Acknowledgements
Authors thank Research Infrastructure RECETOX RI (No. LM2018121), financed by the Ministry of Education, Youth and Sports, and Operational Programme Research, Development, and Innovation—project CETOCOEN EXCELLENCE (No. CZ.02.1.01/0.0/0.0/17_043/0009632) for supportive background. CIISB, Instruct-CZ Centre of Instruct-ERIC EU consortium, funded by MEYS CR infrastructure project LM2023042 and European Regional Development Fund-Project “UP CIISB” (No. CZ.02.1.01/0.0/0.0/18_046/0015974), is gratefully acknowledged for the financial support of the measurements at the CF Nanobiotechnology and Cryo-electron microscopy and tomography core facility CEITEC MU.
Funding
This work was supported by the Czech Science Foundation/Standard Projects [GA20-11321S]; and the Masaryk University/Specific research—support for student projects [MUNI/A/1370/2022 (1/2023–12/2023)].
Author information
Authors and Affiliations
Contributions
J.Š. conceptualized a working hypothesis, performed statistical analysis, interpreted all data, and wrote and edit the manuscript. T.F. performer all microbiological experiments, optimized methodology, analyzed data and contributed to the manuscript writing. E.S. determined parameters of surface roughness. K.V. prepared titanium surfaces with nanotubular arrays, performed SEM analysis, measured surface wettability, and prepared samples for determination of Ti ion release rate. M.U. analyzed crystallinity of the nanotubes. K.Č. supervised microbiological part of this study. J.P. determined surface energy. A.D. analyzed structure and chemical composition of the nanotubes. M.P.G. conceptualized a working hypothesis, acquired funding, and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Šístková, J., Fialová, T., Svoboda, E. et al. Insight into antibacterial effect of titanium nanotubular surfaces with focus on Staphylococcus aureus and Pseudomonas aeruginosa. Sci Rep 14, 17303 (2024). https://doi.org/10.1038/s41598-024-68266-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68266-1
- Springer Nature Limited