Abstract
Tissue-specific genes are believed to be good drug targets due to improved safety. Here we show that this intuitive notion is not reflected in phase 1 and 2 clinical trials, despite the historic success of tissue-specific targets and their 2.3-fold overrepresentation among targets of marketed non-oncology drugs. We compare properties of tissue-specific genes and drug targets. We show that tissue-specificity of the target may also be related to efficacy of the drug. The relationship may be indirect (enrichment in Mendelian disease and PTVesc genes) or direct (elevated betweenness centrality scores for tissue-specifically produced enzymes and secreted proteins). Reduced evolutionary conservation of tissue-specific genes may represent a bottleneck for drug projects, prompting development of novel models with smaller evolutionary gap to humans. We show that the opportunities to identify tissue-specific drug targets are not exhausted and discuss potential use cases for tissue-specific genes in drug research.
Similar content being viewed by others
Introduction
Drug development is a long and costly process. Selection of the right target is a major factor influencing the probability of success of a drug development program1,2,3. Low confidence in biological target has been linked to failures in phase 2 clinical trials due to lack of efficacy1 indicating that is not completely understood how to de-risk the selection of new targets. One possibility to de-risk the discovery process is to revisit gene categories that are known to have an increased probability of yielding successful drug targets. Open opportunities to discover new targets are likely not exhausted. A recent study by Oprea et al. indicates that only 3% of human proteins are targeted by marketed or clinical trial drugs (“Tclin”) whereas 35% have an unknown biological function and are not actively studied (“Tdark”)4.
In this study, we revisit tissue-specific genes. Narrow expression in one or a few tissues is considered desirable for drug targets due to reduced risk of side effects5,6 and such genes with narrow expression are often called ‘tissue-specific’ or ‘tissue-enriched’. Studies on microarray7,8,9 and a combination of RNA-sequencing and proteomics data10,11 confirm that targets of marketed drugs are biased towards tissue-specific genes. To the best of our knowledge, the first quantitative estimate was published in 2008. Dezso et al. demonstrated that tissue-specific genes are twice more likely to become drug targets than broadly expressed house-keeping genes12. Yang et al. confirmed a 1.7-fold higher likelihood in 201613. Dezso et al. observed that tissue-specific genes may represent attractive drug targets due to their role in tissue biology and disease (e.g., brain-specific GABRB2, a receptor for the inhibitory neuromediator gamma-aminobutyric acid, is a target of sedative agents)12. These studies assessed tissue-specificity in healthy tissues. Their findings also extrapolate to diseased tissues because targets of marketed and phase 3 drugs are expressed in disease-relevant tissues even in the healthy state in 87% of the cases14. Also, an important parallel exists between tissue-specific genes and targets of marketed drugs. As first demonstrated in 2004, tissue-specific genes are enriched in Mendelian disorder genes15. The enrichment was confirmed by Yang et al. in 201613. 53% targets of marketed drugs are implicated in Mendelian disorders16. Drugs targeting genes with a genetic link to human disease are less likely to fail in clinical trials due to lack of efficacy1,16,17. Thus, there may be a relationship between tissue-specificity of the target and efficacy of the drug. In fact, a recent study by Rouillard, Hurle and Agarwal concentrated on identification of omics features distinguishing targets that succeeded and failed in phase 3 trials for non-oncology diseases18. Phase 3 trial failures were enriched in failures due to lack of efficacy. Rouillard and colleagues limited their analysis to drugs with a single mechanism-of-action target and demonstrated that narrow expression profile of a drug target is a robust predictor of success in phase 318. If we understand the relationship between tissue-specificity and efficacy and apply this knowledge to identify new, and not necessarily only tissue-specific, targets, we may ultimately reduce attrition rates in the clinic.
Here, we find that tissue-specific genes are mostly relevant for non-oncology disease indications. Application of increasingly stringent definitions of tissue-specificity leads to increasingly stronger enrichment of tissue-specific genes among marketed non-oncology drug targets. With moderately stringent definition (x = 6), we confirm a 2.3-fold enrichment among targets of non-oncology drugs and 1.8-fold enrichment in a pooled analysis for both oncology and non-oncology drug targets, which are similar to the previously published estimates12,13. We observe that this historic success of tissue-specific targets is not reflected in early clinical trials neither for oncology nor for non-oncology diseases, i.e., tissue-specific targets are underutilized. The limiting factor for development of tissue-specific targets may be the reduced conservation of tissue-specific genes between humans and animal models and the associated challenges in preclinical research. We find two factors, that could be related to efficacy of drugs targeting tissue-specific genes. First, we confirm enrichment in Mendelian disease genes and observe enrichment in potential disease genes with gain-of-function but not loss-of-function mechanism among tissue-specific genes. Second, we find that tissue-specific enzymes and secreted proteins have higher ability to spread perturbations in topological analysis of human protein-protein interactome.
Results
Our results section is structured as follows. We investigate the prevalence of tissue-specific genes among targets of candidate and marketed drugs. Next, we explore properties that may explain depletion of tissue-specific genes among targets of drugs in early clinical trials and their overrepresentation among targets of marketed drugs. Finally, we highlight open opportunities to develop tissue-specific genes as drug targets.
We talk about genes as drug targets because the previous studies demonstrated enrichment in tissue-specific genes among drug targets based on mRNA expression12,13. We also define tissue-specificity based on RNA-sequencing data. We assume that the messenger RNAs are translated to their protein products, which, in turn, interact with the drugs. The concordance between gene expression and protein abundance is debated19,20, but a recent Ribo-seq study in rat suggests that 70 (heart) to 85% (liver) of transcribed mRNA are forwarded to translation21.
Tissue-specific drug targets were more relevant for non-oncology indications
Tissue-specific genes constituted a small fraction of all human protein-coding genes (Supplementary Data 1). We applied nine increasingly stringent definitions of tissue-specificity x from 2 to 10 meaning at least x-fold difference in magnitude of the highest and the second highest per-tissue Z-score. For example, SLC43A1 (https://gtexportal.org/home/gene/SLC43A1), SCTR (https://gtexportal.org/home/gene/SCTR) and INS (https://gtexportal.org/home/gene/ENSG00000254647.2) were tissue-specific for pancreas at x = 2, 6 and 10, respectively. The most liberal definition x = 2 resulted in 4,573 of 18,377 (24.9%) tissue-specific genes. 1,018 genes (5.5%) satisfied moderately stringent definition x = 6, while only 557 (3.0%) genes satisfied the most stringent definition x = 10.
If tissue-specificity was irrelevant for drug target discovery, the proportions of tissue-specific genes among drug targets would follow the ‘background’ distribution among all protein-coding genes. By contrast, we observed increasingly stronger deviations from the ‘background’ distribution with increasingly stringent definitions of tissue-specificity (Fig. 1). Targets for oncology and non-oncology disease indications were considered separately because they are selected following different discovery paradigms (e.g., different acceptability of side effects, selection of proteins harbouring cancer-specific mutations as targets etc). Targets of phase 1 drugs were significantly depleted of tissue-specific genes for both oncology and non-oncology indications even at the most liberal x = 2. The discrepancies in prevalence of tissue-specific genes between oncology and non-oncology targets started to emerge in phase 2. Enrichment in tissue-specific genes among targets of phase 3 drugs was observed for both non-oncology and oncology indications. Interestingly, the tissue-specific phase 3 oncology targets were aberrantly expressed in cancer (e.g., GNRHR is pituitary-specific in non-diseased state but ectopically expressed in endometrial cancers) or were targets of therapies accompanying cytostatic agents (e.g., hemoglobin as target of experimental drugs increasing tissue oxygenation to sensitize tumors to main therapy, NCT00083304). Targets of marketed non-oncology drugs were enriched in tissue-specific genes, but targets of marketed oncology drugs were depleted in tissue-specific genes. The enrichment among targets of marketed non-oncology drugs was stronger (2.3-fold at x = 6 and up to 3-fold at x = 10) than the previous estimates12,13, which was probably because previous studies did not make a distinction between oncology and non-oncology drug targets. Indeed, a pooled analysis for oncology and non-oncology drug targets indicated a significant 1.8-fold enrichment at moderately stringent x = 6, p-value 2e-6 (Supplementary Fig. S1). Targets of withdrawn non-oncology drugs were also enriched in tissue-specific genes. The reason for withdrawal from the market was toxicity with few exceptions like unintended use for self-poisoning (barbiturates) and lack of efficacy (drotrecogin alpha). Targets of withdrawn drugs had 95% overlap with targets of marketed drugs (57 of 60, from which only 3 were for oncology indications). Hence, withdrawal of these drugs from the market could not be uniquely attributed to their mechanism-of-action targets. For example, cholinergic nicotinic receptors CHRNA1, CHRND and CHRNG are targets of curare-like neuromuscular blocking agents. Rapacuronium bromide was withdrawn from the market due to adverse events while other drugs like vecuronium continue to be used.
Tissue-specific genes were overrepresented among targets of phase 3 drugs and targets of marketed non-oncology drugs. Prevalence of tissue-specific genes among targets of drugs for (a) non-oncology and (b) oncology indications. Percentages of tissue-specific genes among targets of drugs in each phase of clinical development were plotted in comparison to the ‘background’ distribution among all protein coding-genes (black line). Tissue-specificity was defined at nine increasingly stringent constraints x = 2 to 10. (c) Fisher test p-value and fold enrichment for each gene category and each constraint x. Enrichment values >1 indicated over-representation of tissue-specific genes while values <1 indicated under-representation of tissue-specific genes. Nominal p-values < 0.05 were considered statistically significant.
Tissue-specific targets of marketed drugs were less reused as targets of candidate drugs
The overlap between targets of withdrawn and marketed drugs motivated us to examine ‘recycling’ of drug targets. Target genes can reenter clinical trials when new drugs are developed for the same (e.g., generations of H2 histamine receptor HRH2 blockers as anti-ulcer drugs) or a novel indication. For example, IGF1R is targeted by recombinant insulin growth factor 1 Mecasermin for growth failure in children (marketed agonist drug) and is evaluated as target for treatment of solid tumours (antagonist drug PL-225B in phase 1 trial NCT01779336).
For simplicity of presentation, we limited this and all subsequent analyses to tissue-specific genes satisfying the liberal x = 2, moderately stringent x = 6 and the most stringent x = 10 definitions of tissue-specificity. Tissue-specific targets of marketed drugs were less frequently reused by clinical trial drugs than non-tissue specific targets (Fig. 2a) and had less chemical compounds in clinical development (Fig. 2b). For example, tissue-specific targets of marketed drugs satisfying x = 6 were reused 1.9 times less frequently than non-tissue specific targets that did not satisfy any of the definitions x (66.3% vs 34.3%, Fisher test, p-value 3e-5). Furthermore, tissue-specific genes represented older subsets of drug targets (Fig. 2c), although the differences were not statistically significant.
Tissue-specific targets represented less frequently reused (a,b) and older (c) subsets of targets of marketed drugs. a Numbers and percentages of targets of marketed drugs that were targeted by candidate drugs in clinical trials, i.e., reused. (b) Number of candidate drugs per re-used target. (c) Year of regulatory approval by FDA or another agency of the first drugs modulating tissue-specific targets compared to non-tissue-specific targets of marketed drugs. For example, carglumic acid was the first marketed drug modulating CPS1 and it was approved in 2010.
In summary, tissue-specific targets were not actively explored in phase 1 clinical trials and tissue-specific targets of marketed drugs were less reused. We investigated possible explanations for these trends.
Tissue-specific genes were less evolutionary conserved
Evolutionary properties may explain the reduced utilization of tissue-specific targets. Wenhua Lv et al. demonstrated that targets of FDA-approved drugs are more evolutionary conserved than non-target genes22. By contrast, in 2004, Winter, Goodstasdt and Ponting investigated expression of 4,960 human genes in 27 tissues and demonstrated that tissue-specific genes are less evolutionary conserved in mice than broadly expressed genes using Ka/Ks ratios15. To clarify, Ka/Ks is the rate of nonsynonymous Ka to synonymous Ks amino acid changes in a pair of orthologs. Fractional values of Ka/Ks are indicative of negative selection pressure favoring between-species conservation of an amino acid sequence. By contrast, Ka/Ks values exceeding 1 may in some cases indicate that positive selection pressure has favored evolutionary divergence of orthologs, as exemplified by immune genes adapted to species-specific pathogens23,24,25,26.
We performed analysis of evolutionary conservation on a genome-wide scale and expanded to other species. We examined percentages of human genes without 1-to-1 orthologs, Ka/Ks ratios and protein sequence similarity for human protein-coding genes and their counterparts in mice and 6 other common animal model species. The analysis of Ka/Ks ratios was limited to mammalian species as the evolutionary distances between human and the two non-mammalian species were too large. We confirmed that tissue-specific genes were significantly less evolutionary conserved than all protein-coding genes, in contrast to targets of not only marketed but also clinical trial drugs (Fig. 3 for mice and Supplementary Figs S2–S7 for other species, statistical analysis results for each species in Supplementary Dataset 3). Increased percentages of genes without 1-to-1 orthologs, elevated Ka/Ks ratios and reduced percentages of sequence similarity for orthologs of tissue-specific genes indicated increased risk of translational gaps because the conservation of protein sequence is considered a proxy for conservation of biological function27 and 1-to-many or many-to-many orthologs arising through duplication tend to diverge in function with time28,29. FDA requires pharmacological effects and toxicological data from preclinical testing in animal models (https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=312.23), so reduced evolutionary conservation of tissue-specific genes may represent a bottleneck for preclinical development and explain underrepresentation of tissue-specific genes among targets that entered phase 1 trials.
Tissue-specific genes were less evolutionary conserved in mice compared to all protein-coding genes and drug targets. (a) Percentages of genes without 1-to-1 orthologs in mice. 1-to-1 ortholog refers to a human gene with one unique counterpart in mouse as opposed to 1-to-many or many-to-many orthologs that arise from duplication or gene fusion events. (b) Ka/Ks ratios for human-mouse 1-to-1 orthologs. (c) Sequence similarity of human protein-coding genes and their 1-to-1 orthologs in mice.
In summary, underrepresentation of tissue-specific targets in phase 1 clinical trials could be related to potential translational challenges. Despite these challenges, tissue-specific genes were enriched among targets of marketed non-oncology drugs. We hypothesized that tissue-specificity was related to efficacy and not only to safety.
Relationship between tissue-specificity of the targets and efficacy of the drugs
Prevalence of disease genes
Drugs, that modulate targets with genetic evidence for a human disease, are less likely to fail in clinical trials for lack of efficacy1,16,17. Genetic evidence likely indirectly contributes to drug efficacy because knowledge of human genetics can help to understand the biological function of the target, find target engagement biomarkers for clinical trials and estimate dose-response curves30 and these factors can enhance the chances of a drug program to succeed1,3,5,6.
We compared the prevalence of OMIM31, Protein Truncating Variants escaping nonsense mediated decay (PTVesc) genes32 and loss-of-function tolerant and intolerant33,34 genes among tissue-specific genes and drug targets. OMIM genes have an entry in the Online Mendelian Inheritance in Man® Morbid Map database32, are well-known disease genes and are likely to be explored in target discovery. Loss-of-function intolerant genes are potential disease genes that harbour significantly fewer loss-of function variants than could be expected, are subject to strong purifying selection within the human population and are largely non-redundant with OMIM33. PTVesc genes are an emerging class of candidate genes that can cause disease by gain-of-function mechanism. PTVesc genes are significantly depleted of genetic variants that result in nonsense-mediated-decay-escaping mRNA and production of truncated proteins with altered function (e.g., PNPLA3 and APOL1)32. Methods for detection of PTVesc are recently developed, so PTVesc genes are unlikely to be explored to the same extent as OMIM genes. Tissue-specific genes were enriched in both OMIM and PTVesc genes (Fig. 4a and Fig. 4b, full statistical analysis in Supplementary Dataset 3). With moderately stringent definition x = 6, tissue-specific genes were 1.3-fold enriched in OMIM genes (272 of 1,018, 26.7% > 3,870 of 18,377, 21.1%, Fisher test, Bonferroni adjusted p-value 0.006) and 1.5-fold enriched in PTVesc genes (159 of 1,018, 15.6% > 1,913 of 18,377, 10.4%, Bonferroni adjusted p-value 7.4e-5). As expected, drug targets for oncology and non-oncology indications across all phases of clinical development were enriched only in OMIM genes (Fig. 4a). By contrast, the prevalence of PTVesc genes among drug targets did not significantly deviate from the overall prevalence among protein-coding genes (Fig. 4b). Tissue-specific genes were enriched in loss-of-function tolerant (ExAC consortium pLI < = 0.1) and depleted of loss-of-function intolerant (ExAC pLI > = 0.9) genes compared to all protein-coding genes (Fig. 4c, full statistical analysis in Supplementary Dataset 3). By contrast, targets of oncology drugs were enriched in loss-of-function intolerant and depleted of tolerant genes. Targets of marketed non-oncology drugs had comparable prevalence of loss-of-function tolerant and intolerant genes compared to all protein-coding genes. We also analyzed a continuous loss-of-function tolerance metric LOEUF published by the gnomAD consortium34 and confirmed the results obtained with ExAC consortium data (Fig. 4d). Loss-of-function tolerance metrics for tissue-specific genes were more similar to non-oncology that oncology drug targets and confirmed that tissue-specific genes were more likely to become targets for non-oncology drugs. Also, increased tolerance of tissue-specific genes to loss-of-function variation could have implications for strategies to discover disease phenotypes associated with tissue-specific genes. Future research efforts need to consider early insights from the ExAC consortium flagship paper indicating that the degree of loss-of-function tolerance has an impact on the probability that the gene is detected in a GWAS study or has eQTLs and that recessive disease genes tend to be more loss-of-function tolerant than all human genes33.
Tissue-specific genes were enriched in disease genes with potential gain-of-function mechanism but not loss-of-function mechanism. The bars show percentages of (a) OMIM, (b) PTVesc and (c) loss-of-function tolerant (ExAC pLI < = 0.1) and intolerant (pLI > = 0.9) genes in each gene category. Violin plots in (d) show loss-of-function tolerance as a continuous score according to the gnomAD consortium data. Higher values indicate higher tolerance to loss-of-function variation.
In total, 386 of 1,018 (37.9%) tissue-specific genes at x = 6, 1,400 of 4,573 (30.6%) at x = 2 and 250 of 557 (44.9%) at x = 10 were OMIM genes or PTVesc genes or both. For comparison, 5,362 of 18,377 (29.2%) protein-coding genes were OMIM or/and PTVesc genes. Thus, tissue-specific genes were more likely to provide necessary information for development of efficacious drugs through human genetics than protein-coding genes overall.
Network analysis
The ability to spread perturbations and cause phenotypic changes is a key property of drug targets, which is reflected by topological properties in protein-protein interaction (PPI) networks35. We performed network analysis on STRING v10.536 (Supplementary Data 2) because tissue-specific proteins are well represented in this data base37. We investigated the sources of supporting evidence for PPIs (Supplementary Fig. S8). Tissue-specific genes did not markedly differ from all protein-coding genes in this respect. The only potential source of bias for network analysis was the amount of publications linked to a specific protein (Kendall tau b = 0.31). The calculations were performed on the largest connected component including 19,574 proteins and 5,676,527 PPIs. The unweighted network diameter was 6. We evaluated 5 centrality scores (illustrated in Supplementary Fig. S9). We included three control gene sets with known ability to affect phenotype. Essential genes38 and OMIM genes served as positive controls. Genes with rare homozygous loss-of-function rhLOF variants and without clinical manifestation or impact on medication prescription rate served as negative no-phenotype controls (British-Pakistani, ExAC and Icelandic individuals, Suppl. Table 2 from39).
Topological properties of the proteins accurately reflected their ability to spread perturbations through the network as indicated by low centrality scores for negative controls rhLOF and high centrality scores for positive control genes (Supplementary Fig. 10). Interestingly, PTVesc genes, that we expected to behave similar to OMIM positive controls, had comparable or slightly lower median centrality scores than all protein-coding genes suggesting that some aspects of signal propagation may not be captured by PPIs. Elevated betweenness centrality was the only topological property that could distinguish tissue-specific genes from all protein-coding genes (Table 1). The trend was nominally significant at x = 6 and passed the correction for multiple testing at x = 2 and x = 10. Specifically, enzymes and secreted proteins, that were expressed in a tissue-specific manner, had higher betweenness centrality scores than other tissue-specific genes (Table 2). Our results were consistent with the previous study on regulatory networks, in which Sonawane et al. applied a less stringent definition of tissue-specificity and found that tissue-specific genes serve as “bottlenecks” on signaling paths40.
Open opportunities
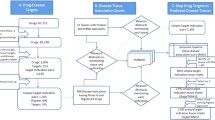
We estimated the numbers of tissue-specific genes with some initial indication of druggability and human genetic evidence through OMIM and PTVesc (Fig. 5 for x = 6, Supplementary Fig. S11 for x = 2 and Supplementary Fig. S12 for x = 10) and observed that the opportunities were not exhausted. In total, only 100 of 1,018 (9.8%) tissue-specific gene satisfying the moderately stringent definition x = 6 were explored as targets of marketed or clinical trial drugs. 284 of the remaining 918 (30.9%) tissue-specific genes were classified as Tdark in the TCRD data base41, i.e., were poorly researched with unknown biological function. 529 of 918 (57.6%) showed some indication of druggability by small molecule or antibody approaches and 211 of 918 (22.9%) had both indications of druggability and human genetic evidence (Fig. 5). The definition of druggability constantly expands, and targets that cannot be modulated with small molecules or antibodies may be druggable with other approaches in the future.
Tissue-specific genes (x = 6) that were not yet explored as targets of marketed or clinical trial drugs but were potentially druggable or had human genetic evidence. Dots indicate overlapping sets, while bars on the top indicate overlap size. For example, the fifth column indicates that 40 secreted proteins had known crystal structures and did not have other indications of druggability. Proteins classified as Tchem in the TCRD data base have potent compounds with binding affinities in the nanomolar (G-protein coupled receptors, nuclear hormone receptors, kinases) or lower micromolar range (ion channels and other target categories). Such chemical compounds can be optimized and transitioned to clinical trials. Secreted proteins may be amenable to antibody therapies. Other tissue-specific genes have some knowledge around them to start a chemical development program. Chemical compounds with binding activities in ChEMBL v23, possibly less potent than the criteria used to define Tchem, offer hints to infer structure-activity relationships, to discover and optimize a lead compound. Known crystal structure may be used to identify binding pockets and design binding molecules. Known drug targets in the same protein family may aid chemical discovery through sequence similarity and homology modelling.
Discussion
The limitation of our study is that we conducted a retrospective analysis of tissue-specific genes compared to drug targets. Targets of phase 1 drugs reflect the most recent research. By contrast, targets of marketed drugs have undergone at least a decade in preclinical and clinical development and reflect older research. Theoretically, overrepresentation of tissue-specific targets on the market and depletion in phase 1 could reflect a historic shift in target selection paradigms. However, Rouillard and colleagues18 studied phase 3 drugs (projects with comparable “age”) and demonstrated that drugs modulating tissue-specific targets are more likely to succeed in phase 3 and gain regulatory approval. Hence, the data presented in Fig. 1 and Supplementary Fig. S1 do not merely represent a historic trend and we are justified to state that drugs modulating tissue-specific targets are indeed more likely to progress in the clinic. Also, we have based the analysis on the GTEx tissue panel. We selected this tissue panel because it both includes large number of tissues, which are necessary to make robust conclusions about tissue-specificity, and, to the best of our knowledge, the largest sample size per tissue, which is crucial for robust calculation of Z-scores because they are derived from mean expression values. Some tissues (e.g., bone marrow) and disease samples are not included in GTEx. We recommend to use databases such as TiGER42, TiSGeD43, VeryGene44 and TissGDB45 if tissue-specificity in disease or tissues absent in GTEx represent the focus of reader’s research.
In contrast to previous works reporting increased tissue-specificity of drug targets7,8,9,10,11,12,13, we applied nine definitions of tissue-specificity of varying stringency and considered targets of oncology and non-oncology dugs separately. This analysis approach enabled us to establish that tissue-specific genes are mostly relevant for non-oncology disease indications. We observed that increasingly stringent definitions of tissue-specificity lead to increasingly stronger overrepresentation of tissue-specific genes among targets of marketed non-oncology drugs with statistically significant enrichment starting from x = 3. The statistical significance was reached staring from x = 6 in a pooled analysis for both oncology and non-oncology indications. We found that a substantial proportion of tissue-specific genes have genetic evidence that could facilitate drug development. In fact, combining simple criteria of tissue-specificity with genetic evidence for target prioritization could be a potentially effective de-risking strategy for non-oncology indications (Fig. 6) but this strategy should also be validated in prospective studies.
Combining tissue-specificity with genetic evidence may represent an effective de-risking strategy for non-oncology drug targets. The graph shows prevalence of genes that are both tissue-specific at each x and have an OMIM Morbid Map entry or are PTVesc among drug targets compared to all protein-coding genes. The table below contains fold enrichment and p-values. Enrichment <1 indicates depletion in tissue-specific genes with human genetic evidence.
We conclude that tissue-specific genes are a promising source for target discovery. Feasibility-related hurdles in development of tissue-specific targets could be circumvented by development of in vivo models (e.g., humanized mice, human IPS-derived organoids transplanted in animal models). In addition, genes that are currently considered undruggable could be amenable to novel therapeutic approaches. For example, tissue-specific genes causing monogenic Mendelian diseases are potential targets for genome editing with CRISPR/Cas9 (e.g., SERPINA1 in alpha-1 antitrypsin deficiency46). Tissue-specific genes could also be used for targeted delivery (e.g., oncolytic viral therapies like urothelium-specific adenovirus CG8840 with bladder-specific UPK2 promoter for bladder cancer47 or N-acetylgalactosamine (GalNAc)-conjugated antisense oligonucleotide drugs binding to ASGR1 for targeted delivery to hepatocytes48). Also, tissue-specific genes with protein products entering the bloodstream may find applications as biomarkers (KLK3 in prostate cancer) or replacement therapies (e.g., insulin in type 1 diabetes).
Materials and Methods
Gene expression
Gene-level RPKM values were downloaded from The Genotype-Tissue Expression Consortium49 (https://gtexportal.org/home/, release 6). The per-tissue mean RPKM for each gene was subjected to Z-transformation across tissues and then to a second Z-transformation across genes to bring all Z-scores to the same scale. We identified 18,377 protein-coding genes with HGNC approved gene symbol50. The non-alternative loci data set was obtained from the HGNC Database (www.genenames.org, 30.08.2017).
Definitions of tissue-specificity
We applied peak-based definitions of tissue-specificity. The peak x was defined as the difference between the highest and the second highest per-tissue Z-scores for each gene. Nine increasingly stringent definitions were applied: Zsecond largest <1/x * Zmax, where Zmax denoted the Z-score in the tissue with the highest expression, Zsecond largest denoted the Z-score in tissue with the second highest expression and x was an integer from 2 to 10. So, x = 2 indicated at least two-fold difference in Z-scores, i.e., difference by at least 2 standard deviations from the overall mean. Such definitions allowed genes to be expressed in multiple tissues, as long as the expression in the tissue with the maximal expression was distinctly higher than in all other tissues. Since the definitions were based on the inequality Zsecond largest <1/x * Zmax, stringent x automatically implied that all more liberal x were also satisfied while the opposite statement was not automatically true. For example, secretin receptor was considered pancreas-specific at x = 6 and accordingly at all more liberal constraints x 2 to 5 but did not satisfy more stringent constraints x 7 to 10 (https://gtexportal.org/home/gene/SCTR). Also, by definition, genes satisfying a more stringent x are a subset of genes satisfying more liberal x (e.g., x = 10 are a subset of genes satisfying x = 9, which in turn are a subset of genes satisfying x = 8 etc).
Drug targets
Mechanism-of-action targets of marketed and clinical trial drugs, disease indications and year of first approval for marketed drugs were extracted from ChEMBL version 2351. Drugs were classified as phase 1, 2, 3 or marketed drugs based on the maximal phase they reached in clinical trials. Disease indications were mapped to Disease Ontology52. Proteins were classified as oncology or non-oncology targets based on parent terms in Disease Ontology. If a protein was targeted by at least 1 oncology drug, it was considered an oncology target.
Meta-data
Example compounds with exact Ki or IC50 activity values against human proteins, measured in assays with direct interaction and the highest confidence score = 9, were retrieved from ChEMBL v2351. Mapping from ENSEMBL identifiers to PDB were obtained from GENECODE consortium53 version 27. Mapping to enzyme EC numbers, Uniprot and NCBI Gene (Entrez) identifiers were extracted from the HGNC non-alternative loci data set50. Target Development Level (TDL) was retrieved from TCRD version 4.6.241. Subcellular localization and protein family information were obtained from UniProt/SwissProt54. Probabilities of being loss-of-function intolerant (pLI) were retrieved from Supplementary Data of the ExAC consortium flagship publication33. Associations with Mendelian diseases were retrieved from OMIM Morbid Map31 (copyright John Hopkins University, AstraZeneca purchased license JHU agreement number A30699 and reference number C03746). We included only binary indicator variables (has/does not have an entry in the Morbid Map). Number of PubMed-indexed articles linked to each gene was retrieved from NCBI Gene55 https://www.ncbi.nlm.nih.gov/gene/ on the 02.01.2018. Human to mouse orthologs, Ka/Ks ratios and percentages of sequence identity and similarity were extracted from ENSEMBL Compara56 version 95. The lists of essential genes38, PTVesc32 and rhLOF39 genes and human transcription factors57 were obtained from supplementary data of the respective publications. Biological function of the genes was described according to the NCBI Gene/RefSeq summary58 unless explicitly indicated otherwise.
Network analysis
Human protein-protein interaction network was downloaded from STRING v 10.5 (file 9606.protein.links.detailed.v10.5.tsv)36. Topological properties were calculated with igraph59 version 1.2.1. Weighted k-shell decomposition was computed as described in60. Combined evidence scores were used as edge weights for strength, eigenvector centrality and k-shell calculations, i.e., the overall ‘influence’ of a node was proportional to the number of its neighbors combined with confidence in its PPIs. Edge weights were taken as (1 – combined evidence score) for centrality measures based on shortest paths, i.e., shortest paths were the ‘least uncertainty paths’.
Statistical analysis
We applied Fisher exact test for count data because sample sizes were small in some instances (e.g., 3 tissue-specific targets in phase 1 at x = 6) and to be consistent in other analyses. Mann-Whitney U test was used to test differences between groups for continuous variables. Wilcoxon test with explicit handling of tied values in exactRankTests61 version 0.8–29 was used to test differences in year of first approval. Tests for enrichment or depletion were one-tailed, other tests were two-tailed. Bonferroni correction for multiple testing was applied as appropriate. P-values < 0.05 were considered significant. Statistical analyses were summarized in Supplementary Dataset 3. Figures were generated with ggplot262 version 3.0.0, viridis63 version 0.5.1 and UpSetR64 version 1.3.3. Analyses were performed in R65 version 3.4.1.
Data Availability
All data, that were generated in this study, are provided as Supplementary data sets. Annotated Z-score tables for protein-coding genes including the tissue-specific gene and drug target subsets are provided in Supplementary Data 1. Network topology properties are provided in Supplementary Data 2. Columns, that were used as input data for figures, are labelled within each supplementary data set. Summary-level data behind the figures are included in the Supplementary Dataset 3. Source data for evolutionary conservation can be retrieved directly from Ensembl Compara56 v 95. gnomAD consortium data can be retrieved directly from https://gnomad.broadinstitute.org/.
References
Cook, D. et al. Lessons learned from the fate of AstraZeneca’s drug pipeline: a five-dimensional framework. Nat Rev Drug Discov 13, 419–431 (2014).
Shih, H. P., Zhang, X. & Aronov, A. M. Drug discovery effectiveness from the standpoint of therapeutic mechanisms and indications. Nat Rev Drug Discov 17, 19–33 (2018).
Bunnage, M. E. Getting pharmaceutical R&D back on target. Nat Chem Biol 7, 335–339 (2011).
Oprea, T. I. et al. Unexplored therapeutic opportunities in the human genome. Nat Rev Drug Discov 17, 317–332 (2018).
Debouck, C. & Goodfellow, P. N. DNA microarrays in drug discovery and development. Nat Genet 21, 48–50 (1999).
Gashaw, I., Ellinghaus, P., Sommer, A. & Asadullah, K. What makes a good drug target? Drug Discov Today 16, 1037–1043 (2011).
Xu, H. et al. Learning the drug target-likeness of a protein. Proteomics 7, 4255–4263 (2007).
Yao, L. & Rzhetsky, A. Quantitative systems-level determinants of human genes targeted by successful drugs. Genome Res 18, 206–213 (2008).
Kim, B., Jo, J., Han, J., Park, C. & Lee, H. In silico re-identification of properties of drug target proteins. BMC Bioinformatics 18, 248, https://doi.org/10.1186/s12859-017-1639-3 (2017).
Emig, D. & Albrecht, M. Tissue-specific proteins and functional implications. J Proteome Res 10, 1893–1903 (2011).
Uhlen, M. et al. Proteomics. Tissue-based map of the human proteome. Science 347, 1260419, https://doi.org/10.1126/science.1260419 (2015).
Dezso, Z. et al. A comprehensive functional analysis of tissue specificity of human gene expression. BMC Biol 6, 49, https://doi.org/10.1186/1741-7007-6-49 (2008).
Yang, L. et al. Comparative analysis of housekeeping and tissue-selective genes in human based on network topologies and biological properties. Mol Genet Genomics 291, 1227–1241 (2016).
Kumar, V., Sanseau, P., Simola, D. F., Hurle, M. R. & Agarwal, P. Systematic Analysis of Drug Targets Confirms Expression in Disease-Relevant Tissues. Sci Rep 6, 36205, https://doi.org/10.1038/srep36205 (2016).
Winter, E. E., Goodstadt, L. & Ponting, C. P. Elevated rates of protein secretion, evolution, and disease among tissue-specific genes. Genome Res 14, 54–61 (2004).
Nelson, M. R. et al. The support of human genetic evidence for approved drug indications. Nat Genet 47, 856–860 (2015).
King, E. A., Davis, J. W. & Degner, J. F. Are drug targets with genetic support twice as likely to be approved? Revised estimates of the impact of genetic support for drug mechanisms on the probability of drug approval. Preprint at, https://doi.org/10.1101/513945v1 (2019).
Rouillard, A. D., Hurle, M. R. & Agarwal, P. Systematic interrogation of diverse Omic data reveals interpretable, robust, and generalizable transcriptomic features of clinically successful therapeutic targets. PLoS Comput Biol 14, e1006142, https://doi.org/10.1371/journal.pcbi.1006142 (2018).
Liu, Y., Beyer, A. & Aebersold, R. On the Dependency of Cellular Protein Levels on mRNA Abundance. Cell 165, 535–550 (2016).
Edfors, F. et al. Gene-specific correlation of RNA and protein levels in human cells and tissues. Mol Syst Biol 12, 883, https://doi.org/10.15252/msb.20167144 (2016).
Schafer, S. et al. Translational regulation shapes the molecular landscape of complex disease phenotypes. Nat Commun 6, 7200, https://doi.org/10.1038/ncomms8200 (2015).
Lv, W. et al. The drug target genes show higher evolutionary conservation than non-target genes. Oncotarget 7, 4961–4971 (2016).
Hurst, L. D. The Ka/Ks ratio: diagnosing the form of sequence evolution. Trends Genet 18, 486 (2002).
van der Lee, R., Wiel, L., van Dam, T. J. P. & Huynen, M. A. Genome-scale detection of positive selection in nine primates predicts human-virus evolutionary conflicts. Nucleic Acids Res 45, 10634–10648 (2017).
Shultz, A. J. & Sackton, T. B. Immune genes are hotspots of shared positive selection across birds and mammals. Elife 8, https://doi.org/10.7554/eLife.41815 (2019).
Huang, B. H. & Liao, P. C. Tracing evolutionary relicts of positive selection on eight malaria-related immune genes in mammals. Innate Immun 21, 463–476 (2015).
Joshi, T. & Xu, D. Quantitative assessment of relationship between sequence similarity and function similarity. BMC Genomics 8, 222, https://doi.org/10.1186/1471-2164-8-222 (2007).
He, X. & Zhang, J. Rapid subfunctionalization accompanied by prolonged and substantial neofunctionalization in duplicate gene evolution. Genetics 169, 1157–1164 (2005).
Conant, G. C. & Wolfe, K. H. Turning a hobby into a job: how duplicated genes find new functions. Nat Rev Genet 9, 938–950 (2008).
Plenge, R. M., Scolnick, E. M. & Altshuler, D. Validating therapeutic targets through human genetics. Nat Rev Drug Discov 12, 581–594 (2013).
McKusick-Nathans Institute of Genetic Medicine & Johns Hopkins University (Baltimore, MD). Online Mendelian Inheritance in Man, OMIM®. World Wide Web URL, https://omim.org/ (2017).
Coban-Akdemir, Z. et al. Identifying Genes Whose Mutant Transcripts Cause Dominant Disease Traits by Potential Gain-of-Function Alleles. Am J Hum Genet 103, 171–187 (2018).
Lek, M. et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature 536, 285–291 (2016).
Karczewski, K. J. et al. Variation across 141,456 human exomes and genomes reveals the spectrum of loss-of-function intolerance across human protein-coding genes. Preprint at, https://doi.org/10.1101/531210v2 (2019).
Perez-Lopez, A. R. et al. Targets of drugs are generally, and targets of drugs having side effects are specifically good spreaders of human interactome perturbations. Sci Rep 5, 10182, https://doi.org/10.1038/srep10182 (2015).
Szklarczyk, D. et al. The STRING database in 2017: quality-controlled protein-protein association networks, made broadly accessible. Nucleic Acids Res 45, D362–D368, https://doi.org/10.1093/nar/gkw937 (2017).
Lopes, T. J. et al. Tissue-specific subnetworks and characteristics of publicly available human protein interaction databases. Bioinformatics 27, 2414–2421 (2011).
Blomen, V. A. et al. Gene essentiality and synthetic lethality in haploid human cells. Science 350, 1092–1096 (2015).
Narasimhan, V. M. et al. Health and population effects of rare gene knockouts in adult humans with related parents. Science 352, 474–477 (2016).
Sonawane, A. R. et al. Understanding Tissue-Specific Gene Regulation. Cell Rep 21, 1077–1088 (2017).
Nguyen, D. T. et al. Pharos: Collating protein information to shed light on the druggable genome. Nucleic Acids Res 45, D995–D1002, https://doi.org/10.1093/nar/gkw1072 (2017).
Liu, X., Yu, X., Zack, D. J., Zhu, H. & Qian, J. TiGER: a database for tissue-specific gene expression and regulation. BMC Bioinformatics 9, 271, https://doi.org/10.1186/1471-2105-9-271 (2008).
Xiao, S. J., Zhang, C., Zou, Q. & Ji, Z. L. TiSGeD: a database for tissue-specific genes. Bioinformatics 26, 1273–1275 (2010).
Yang, X. et al. VeryGene: linking tissue-specific genes to diseases, drugs, and beyond for knowledge discovery. Physiol Genomics 43, 457–460 (2011).
Kim, P. et al. TissGDB: tissue-specific gene database in cancer. Nucleic Acids Res 46, D1031–D1038, https://doi.org/10.1093/nar/gkx850 (2018).
Loring, H. S. & Flotte, T. R. Current status of gene therapy for alpha-1 antitrypsin deficiency. Expert Opin Biol Ther 15, 329–336 (2015).
Zhang, J. et al. Identification of human uroplakin II promoter and its use in the construction of CG8840, a urothelium-specific adenovirus variant that eliminates established bladder tumors in combination with docetaxel. Cancer Res 62, 3743–3750 (2002).
Tanowitz, M. et al. Asialoglycoprotein receptor 1 mediates productive uptake of N-acetylgalactosamine-conjugated and unconjugated phosphorothioate antisense oligonucleotides into liver hepatocytes. Nucleic Acids Res 45, 12388–12400 (2017).
GTEx Consortium. Human genomics. The Genotype-Tissue Expression (GTEx) pilot analysis: multitissue gene regulation in humans. Science 348, 648–660 (2015).
Yates, B. et al. Genenames.org: the HGNC and VGNC resources in 2017. Nucleic Acids Res 45, D619–D625, https://doi.org/10.1093/nar/gkw1033 (2017).
Gaulton, A. et al. The ChEMBL database in 2017. Nucleic Acids Res 45, D945–D954, https://doi.org/10.1093/nar/gkw1074 (2017).
Kibbe, W. A. et al. Disease Ontology 2015 update: an expanded and updated database of human diseases for linking biomedical knowledge through disease data. Nucleic Acids Res 43, D1071–1078, https://doi.org/10.1093/nar/gku1011 (2015).
Harrow, J. et al. GENCODE: the reference human genome annotation for The ENCODE Project. Genome Res 22, 1760–1774, https://doi.org/10.1101/gr.135350.111 (2012).
The UniProt Consortium. UniProt: the universal protein knowledgebase. Nucleic Acids Res 46, 2699, https://doi.org/10.1093/nar/gky092 (2018).
NCBI Resource Coordinators. Database resources of the National Center for Biotechnology Information. Nucleic Acids Res 46, D8–D13, https://doi.org/10.1093/nar/gkx1095 (2018).
Herrero, J. et al. Ensembl comparative genomics resources. Database (Oxford) 2016, https://doi.org/10.1093/database/bav096 (2016).
Lambert, S. A. et al. The Human Transcription Factors. Cell 172, 650–665 (2018).
O’Leary, N. A. et al. Reference sequence (RefSeq) database at NCBI: current status, taxonomic expansion, and functional annotation. Nucleic Acids Res 44, D733–745, https://doi.org/10.1093/nar/gkv1189 (2016).
Csardi, G. & Nepusz, T. The igraph software package for complex network research. InterJournal, Complex Systems 1695, 1–9 (2006).
Garas, A., Schweitzer, F. & Havlin, S. A k-shell decomposition method for weighted networks. New Journal of Physics 14, 083030 (2012).
Hothorn, T. & Hornik, K. exactRankTests: Exact Distributions for Rank and Permutation Tests, https://CRAN.R-project.org/package=exactRankTests (2017).
Wickham, H. ggplot2: elegant graphics for data analysis. (Springer, 2016).
Garnier, S., Ross, N., Rudis, B., Sciaini, M. & Scherer, C. viridis: Default Color Maps from ‘matplotlib’, https://CRAN.R-project.org/package=viridis (2018).
Conway, J. R., Lex, A. & Gehlenborg, N. UpSetR: an R package for the visualization of intersecting sets and their properties. Bioinformatics 33, 2938–2940, https://doi.org/10.1093/bioinformatics/btx364 (2017).
R Core Team. R: A language and environment for statistical computing. (R Foundation for Statistical Computing, Vienna, Austria., 2018).
Acknowledgements
Authors would like to thank the anonymous reviewers for comments and constructive feedback that helped to substantially improve the manuscript. Authors would like to thank the Exome Aggregation Consortium (ExAC) and Genome Aggregation Database (gnomAD) and the groups that provided exome and genome variant data to these resources. A full list of contributing groups can be found at http://exac.broadinstitute.org/about and https://gnomad.broadinstitute.org/about. Authors would like to thank the The Genotype-Tissue Expression (GTEx) Project. The GTEx Project was supported by the Common Fund of the Office of the Director of the National Institutes of Health, and by NCI, NHGRI, NHLBI, NIDA, NIMH, and NINDS. The data used for the analyses described in this study were obtained from the GTEx Portal release 6 (https://gtexportal.org/home/).
Author information
Authors and Affiliations
Contributions
Conceptualization: M.R., M.H. Formal data analysis: M.R. Writing: M.R., M.H.
Corresponding author
Ethics declarations
Competing Interests
M.R. is a contractor to AstraZeneca. M.H. is employed by AstraZeneca. AstraZeneca provided support to the authors in form of salaries, but had no role in conceptualization of the study, data collection, analysis, interpretation and writing. The authors receive no financial or non-financial reward for publication.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ryaboshapkina, M., Hammar, M. Tissue-specific genes as an underutilized resource in drug discovery. Sci Rep 9, 7233 (2019). https://doi.org/10.1038/s41598-019-43829-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-43829-9
- Springer Nature Limited
This article is cited by
-
Comparative proteomic profiling of the ovine and human PBMC inflammatory response
Scientific Reports (2024)
-
Transcriptomic analysis reveals a tissue-specific loss of identity during ageing and cancer
BMC Genomics (2023)
-
Considerations and challenges for sex-aware drug repurposing
Biology of Sex Differences (2022)
-
CoMI: consensus mutual information for tissue-specific gene signatures
BMC Bioinformatics (2021)
-
Modelling human liver fibrosis in the context of non-alcoholic steatohepatitis using a microphysiological system
Communications Biology (2021)