Abstract
Design
Multicenter retrospective review.
Objective
To evaluate radiographic outcomes and complication rates of patients treated with distraction based implants and pelvic fixation with either screws (sacral-alar-iliac [SAI] screws or iliac screws) or hooks (S hook iliac fixation).
Summary of Background Data
Multiple options exist for pelvic fixation in distraction-based growing rod systems; however, limited comparative data are available.
Methods
Early-onset scoliosis (EOS) patients of all diagnoses with distraction-based implants that had pelvic fixation from 2000 to 2013 were reviewed from two EOS multicenter databases. Patients were divided into two groups by type of pelvic fixation: (1) screw group (SAI screws or iliac screws) or (2) S hooks. Exclusion criteria were as follows: index instrumentation ≥10 years old and follow up <2 years. A total of 153 patients met the inclusion criteria. Mean age at index surgery was 6.1 years (range 1.0-9.9 years) and mean follow-up was 4.9 years.
Results
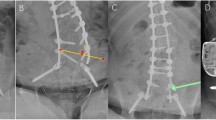
Pelvic fixation in the 153 patients was as follows: screw group = 42 and S hook group = 111. When comparing patients with >20° of initial pelvic obliquity, the screw group had significantly more correction; mean 26° ± 13° for the screw group versus mean 17° ± 7° in the S hook group (p = .039). There was no significant difference in change in T1–S1 length (40 vs. 39 mm, p = .89) or correction of Cobb angle (30° vs. 24°, p = .24). The total complication rate for the screw group was 14% (6/42) versus 25% (28/111) in the S hook group, though this did not achieve significance (p = .25). The most common complications were device migration (13), implant failure (8), and implant prominence (4) for S hooks and implant failure (3), implant prominence (2), and device migration (1) for the screw group.
Conclusion
In distraction-based growth-friendly constructs, pelvic fixation with screws achieved better correction of pelvic obliquity than S hooks. Complications were almost twice as common with S hooks than screws, though this did not reach statistical significance.
Similar content being viewed by others
References
Lenke LG, Kuklo TR. Sacropelvic fixation techniques in the treatment of pediatric spinal deformity. Semin Spine Surg 2004; 16:114–8.
Sponseller P, Yang JS, Thompson GH, et al. Pelvic fixation of growing rods: comparison of constructs. Spine 2009;34:1706–10.
Brooks JT, Jain A, Perez-Grueso FS, et al. Pelvic anchor outcomes in growing rod constructs: an analysis of patients with a minimum of 4 years of postoperative follow-up. Spine Deform 2014;2:512.
Dayer R, Ouellet JA, Saran N. Pelvic fixation for neuromuscular scoliosis deformity correction. Curr Rev Musculoskelet Med 2012;5:91–101.
Alman BA, Kim HK. Pelvic obliquity after fusion of the spine in Duchenne muscular dystrophy. J Bone Joint Surg Br 1999;81:821–4.
McCall RE, Hayes B. Long-term outcome in neuromuscular scoliosis fused only to lumbar 5. Spine 2005;30:2056–60.
Whitaker C, Burton DC, Asher M. Treatment of selected neuromuscular patients with posterior instrumentation and arthrodesis ending with lumbar pedicle screw anchorage. Spine 2000;25:2312–8.
Modi HN, Suh SW, Song H, et al. Evaluation of pelvic fixation in neuromuscular scoliosis: a retrospective study in 55 patients. Int Orthop 2010;34:89–96.
Broom MJ, Banta JV, Renshaw TS. Spinal fusion augmented by Luque-rod segmental instrumentation for neuromuscular scoliosis. J Bone Joint Surg Am 1989;71:32–44.
Mehta SS, Modi HN, Srinivasalu S. Pedicle screw-only constructs with lumbar or pelvic fixation for spinal stabilization in patients with Duchenne muscular dystrophy. J Spinal Disord Tech 2009;22:428–33.
Modi HN, Suh SW, Hong JY, et al. Treatment and complications in flaccid neuromuscular scoliosis (Duchenne muscular dystrophy and spinal muscular atrophy) with posterior-only pedicle screw instrumentation. Eur Spine J 2010;19:384–93.
Modi HN, Hong JY, Mehta SS, et al. Surgical correction and fusion using posterior-only pedicle screw construct for neuropathic scoliosis in patients with cerebral palsy: a three-year follow-up study. Spine 2009;34:1167–75.
Gitelman A, Joseph Jr SA, Carrion W, Stephen M. Results and morbidity in a consecutive series of patients undergoing spinal fusion with iliac screws for neuromuscular scoliosis. Orthopedics 2008;31.
Tsirikos AI, Mains E. Surgical Correction of spinal deformity in patients with cerebral palsy using pedicle screw instrumentation. J Spinal Disord Tech 2012;25:401–8.
Phillips JH, Gutheil JP, Knapp Jr DR. Iliac screw fixation in neuromuscular scoliosis. Spine 2007;32:1566–70.
Hahn F, Hauser D, Espinosa N, et al. Scoliosis correction with pedicle screws in Duchenne muscular dystrophy. Eur Spine J 2008;17:255–61.
Sponseller PD, Zimmerman RM, Ko PS, et al. Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine 2010;35:1887–92.
McCarthy RE, Bruffett WL, McCullough FL. S rod fixation to the sacrum in patients with neuromuscular spinal deformities. Clin Orthop Relat Res 1999;364:26–31.
Shabtai L, Andras LM, Portman M, et al. Sacral alar iliac (SAI) screws fail 75% less frequently than iliac screws in neuromuscular scoliosis. J Pediatr Orthop 2017;37:e470–5.
Peelle M, Lenke L, Bridwell K, Sides B. Comparison of pelvic fixation techniques in neuromuscular spinal deformity correction: Galveston rob versus iliac and lumbosacral screws. Spine 2006;31:2392–8.
Carroll EA, Shilt JS, Jacks L. MW construct in fusion for NM scoliosis. Eur Spine J 2007;16:373–7.
Camp JF, Caudle R, Ashmun RD, Roach J. Immediate complications of Cotrel-Dubousset instrumentation to the sacro-pelvis. A clinical and biomechanical study. Spine 1990;15:932–41.
Sponseller PD, Shah SA, Abel MF, et al. Scoliosis surgery in cerebral palsy: differences between unit rod and custom rods. Spine 2009;34:840–4.
Yang JS, Sponseller PD, Thompson GH, et al. Growing Spine Study Group. Growing rod fractures: risk factors and opportunities for prevention. Spine 2011;36:1639–44.
Smith JT. Bilateral rib-to-pelvis technique for managing early-onset scoliosis. Clin Orthop Relat Res 2011;469:1349–55.
Yamaguchi KT, Skaggs DL, Mansour S, et al. Are rib versus spine anchors protective against breakage of growing rods. Spine Deform 2014;2:489–92.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Author disclosures: MS (none), LMA (personal fees from Biomet, Zimmer, Medtronic, NuVasive, and Orthobullets; other from Eli Lilly and the Journal of Pediatric Orthopedics; other from Pediatric Orthopaedic Society of North America [POSNA] and Scoliosis Research Society [SRS], outside the submitted work), RM (none), NRG (none), PDS (personal fees from DePuy Synthes Spine, Journal of Bone and Joint Surgery, and Globus, outside the submitted work), JBE (personal fees from Biomet and DePuy; other from the Journal of Pediatric Orthopedics; personal fees from Medtronic Sofamor Danek and Synthes, outside the submitted work), MGV (grants and personal fees from Biomet, grants and nonfinancial support from Children’s Spine Foundation, personal fees from East Coast Orthotics and Prosthetics, other from FOX, nonfinancial support from IPOS, grants from, OREF grants and nonfinancial support from POSNA, nonfinancial support from Project for Safety in Spine Surgery, grants from OSRF, grants from SRS, personal fees from Stryker, nonfinancial support from Wellinks, outside the submitted work), DLS (grants from POSNA and SRS, paid to Columbia University; Ellipse [co-PI, paid to Growing Spine Foundation (GSF)], personal fees from ZimmerBiomet, Medtronic, Zipline Medical, Inc., Orthobullets, Grand Rounds [a healthcare navigation company], Green Sun Medical, other from Zipline Medical, Inc; Green Sun Medical, other from Orthobullets, nonfinancial support from the Growing Spine Study Group [GSSG], SRS, and GSF; personal fees from ZimmerBiomet, Medtronic, Johnson & Johnson, other from Medtronic and ZimmerBiomet, other from Wolters Kluwer Health–Lippincott Williams & Wilkins, Biomet Spine; other from Orthobullets, co-editor in chief, outside the submitted work), Growing Spine Study Group (grants from DePuy Synthes Spine, grants from NuVasive, outside the submitted work), Children’s Spine Study Group (grants from DePuy Synthes Spine, grants from NuVasive, outside the submitted work).
IRB approval: This study has been carried out with approval from the Institutional Review Board at Children’s Hospital Los Angeles.
Rights and permissions
About this article
Cite this article
Schur, M., Andras, L.M., Murgai, R. et al. Pelvic Obliquity Correction in Distraction-Based Growth Friendly Implants. Spine Deform 7, 985–991 (2019). https://doi.org/10.1016/j.jspd.2019.03.003
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/j.jspd.2019.03.003