Abstract
Literature has described treatment of flaccid neuromuscular scoliosis using different instrumentation; however, only one article has been published using posterior-only pedicle screw fixation. Complications using pedicle screws in paralytic neuromuscular scoliosis has not been described before. To present results and complications with posterior-only pedicle screws, a retrospective study was carried out in 27 consecutive patients with flaccid neuromuscular scoliosis (Duchenne muscular dystrophy and spinal muscular atrophy), who were operated between 2002 and 2006 using posterior-only pedicle screw instrumentation. Immediate postoperative and final follow-up results were compared using t test for Cobb angle, pelvic obliquity, thoracic kyphosis and lumbar lordosis. Perioperative and postoperative complications were noted from the hospital records of each patient. Complications, not described in literature, were discussed in detail. Average follow-up was 32.2 months. Preoperative, immediate postoperative and final follow-up Cobb angle were 79.8°, 30.2° (63.3% correction, p < 0.0001) and 31.9°, respectively; and pelvic obliquity was 18.3°, 8.9° (52% correction, p < 0.0001) and 8.9°. Postoperative thoracic kyphosis remained unchanged from 27.6° to 19.9° (p = 0.376); while lumbar lordosis improved significantly from +15.6° to −22.4° lordosis (p = 0.0002). Most patients had major to moderate improvement in postoperative functional and ambulatory status compared to the preoperative status. Thirteen (48.1%) perioperative complications were noted with five major complications (four respiratory in the form of hemothorax or respiratory failure that required ventilator support and one death) and eight minor complications (three UTI, two atelectasis, two neurological and one ileus). Postoperatively, we noted complications, such as coccygodynia with subluxation in 7, back sore on the convex side in 4 and dislodging of rod distally in 1 patient making a total of 12 (44.4%) postoperative complications. Of 12 postoperative complications, 6 (50%) required secondary procedure. We conclude that although flaccid neuromuscular scoliosis can be well corrected with posterior-only pedicle screw, there is a high rate of associated complications.
Similar content being viewed by others
Introduction
Treatment of neuromuscular scoliosis with posterior-only pedicle screw fixation has been recently introduced in clinical practice. There are two major categories of neuromuscular scoliosis that includes spastic (cerebral palsy and other upper motor neuron diseases) and flaccid (Duchenne muscular dystrophy, spinal muscular atrophy and other lower motor neuron diseases). Lung functions are usually compromised in flaccid neuromuscular scoliosis patients if they remain unoperated [18, 35, 44]. Using posterior-only procedure has the advantage of preventing further deterioration in compromised lung functions [25]. In flaccid neuromuscular scoliosis-like Duchenne muscular dystrophy (DMD) and spinal muscular atrophy (SMA), quality of bone is weak and often associated with osteoporosis [4, 39]. Hsu [23] reported long bones characterized by thin cortices and osteoporosis in 45 DMD and 81 SMA patients. In addition, pedicle screw can be inserted into osteoporotic spine with good purchase in the pedicle [36]. Hahn et al. [21] recently suggested 77% correction in Cobb angle and 65% correction in pelvic obliquity in 19 patients with DMD using pedicle screw fixation only. Usually, curves in flaccid neuromuscular scoliosis have higher flexibility and, therefore, we do not feel the necessity of anterior release procedure. As the pedicle is the strongest portion of the vertebral body, use of the pedicle screw can very well address the issue of correction.
However, in scoliosis, rotation and pelvic obliquity are hidden problems. Many authors have described rotational correction with various instrumentations and also with a number of complications related to the instrumentations and procedure [5, 21, 36, 37, 40]. Using pedicle screws is an effective method to correct the rotational component of the deformity. Some authors have advocated the use of pelvic fixation for pelvic obliquity, especially in neuromuscular scoliosis [1, 6, 8]; however, others have warned about the risk of complications with, it such as screw impingement and ulceration, pain and pressure sores, etc. [5, 36, 37, 40]. Recently, Phillips et al. [31] have noted 59% complications using iliac screw for pelvic fixation in 50 neuromuscualr scoliosis patients. Complications were deep wound infections, and screw-related and non-screw-related problems, which often required reoperation. Emami et al. [14] also prefer using iliac screw for pelvic fixation in spite of a higher rate of painful hardware, which often requires removal, mainly due to stronger purchase and correction, and less pseudarthrosis. With pedicle screws, literature also describes complications such as neurological injury, vascular injury, loosening of screws, screw pullout, breakage of rod or screw, etc. [7, 9, 13, 15, 17].
The objectives of this study were to present the results of posterior-only pedicle screw in flaccid neuromuscular scoliosis (in DMD and SMA) and to address the rate and nature of complications with this procedure.
Materials and methods
We retrospectively reviewed the results of 27 flaccid neuromuscular scoliosis patients who were operated between 2002 and 2006. There were 18 patients with DMD and 9 patients with SMA: 20 males and 7 females. The average age of the study group was 14.7 ± 4.9 (range, 8–29 years) and average Cobb angle was 79.8° ± 28.3° (range, 40°–150°). Average follow-up was 32.2 ± 9.9 (range, 24–47 months).
Preoperatively, all patients were investigated: pulmonary function tests (spirometry, PFT) and cardiac functions tests (echo-cardiography, ejection fraction) for assessing the fitness for surgery. Patients with pulmonary functions less than 30% and ejection fraction (EF) less than 50% were not selected for the operation. All selected patients in the present study had PFT more than 30% and cardiac EF more than 50%. All were operated by posterior-only approach using pedicle screw fixation. The upper level of fixation was T2–T4 and lower level was L5 or sacrum (with/without pelvis) in all patients. Decisions for pelvic fixation were taken by the senior author (SWS) if the initial pelvic obliquity was more than 15° (18 patients; 11 DMD and 7 SMA). Pelvic fixation, if required, was achieved by bilateral iliac screw insertion (Fig. 1). All screws were fixed over 6-mm diameter titanium rods bilaterally. None of our patients in this study had undergone any other associated procedures such as thoracoplasty, osteotomy or posterior vertebral column resection (PVCR) to achieve the desired level of correction. Pedicle screws were inserted in the thoracic and lumbar level using free-hand technique. All the surgeries were done under hypotensive anesthesia keeping systolic blood pressure less than 100 mmHg and cell savers were used in each operation for collecting the blood lost. After the correction of the curve, posterior fusion was done by local bone grafts from the laminae mixed with the dried frozen allograft. To cut down the operative cost, intraoperative MEP monitoring was utilized only in patients with a curve of more than 90° (11 patients; 6 DMD and 5 SMA), while curves of less than 90° were not monitored by MEP. Postoperatively, in a routine manner, patients were monitored and extubated in the recovery ward by the anesthesiologist.
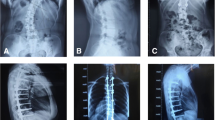
a Preoperative AP and lateral sitting radiogram of a 13-year-old boy with DMD with Cobb angle 50° operated by posterior-only pedicle screw fixation developed good correction. b Postoperative AP and lateral sitting radiogram; however, after 6 months he developed coccygodynia, which exhibited c coccyx subluxation on lateral coccyx radiogram
Preoperatively, patients had full-length AP and lateral spine X-rays in the sitting position and passive side-bending views in the supine position. Postoperatively and at follow-up, full-length AP and lateral radiographs in the sitting position were taken. Coronal angle was measured for the major curve using the Cobb method, while pelvic obliquity was measured as an angle between the line joining the highest points of two iliac crests and the horizontal line. In the sagittal plane, thoracic kyphosis and lumbar lordosis were measured between the maximum tilted vertebrae using the Cobb method. Analyses of the inserted pedicle screws were done on postoperative CT scan to observe any breach in the pedicle wall. Ambulatory status in each patient was evaluated using the modified Rancho classification [22]. Postoperatively, the functional status of each patient was evaluated for sitting balance, cosmetic improvement, transportation by relatives, functional freedom of the arm, improvement in nursing care by parents, overall quality of life (bathing, toilet), satisfaction with operation, and overall respiratory functions according to major, moderate, mild or no improvement compared to the preoperative functions [5].
We collected all the intraoperative record sheets, and postoperative indoor and follow-up sheets to observe perioperative (till discharge from the hospital including intraoperative) and postoperative (after discharge from the hospital) complications. In this study, we have presented all the complications with specific focus on its possible causes and prevention techniques.
Paired t test was used to observe the correction in Cobb angle, pelvic obliquity, thoracic kyphosis and lumbar lordosis between preoperative and postoperative correction, while the same was used to observe the maintenance of the correction between postoperative and final follow-up findings. Additionally, we also observed the postoperative CT scan in all patients to find out any misplacements of the pedicle screws. p Value less than 0.05 was considered as statistically significant. Complications were discussed in detail with previously reported literature to find out any correlation with the fixation method.
Results
Proximal fixation was performed till the T2, T3 and T4 in 13, 6 and 8 patients, respectively; distal fixation level was to L5 in 11 patients and lumbosacral (with/without pelvis) in 16 patients. There were 8, 18 and 1 patient with lumbar, thoracolumbar and thoracic curves, respectively. There was 63.3% (p < 0.0001, paired t test) and 52% (p < 0.0001, paired t test) correction achieved postoperatively in Cobb angle and pelvic obliquity. At final follow-up, it was maintained at 63.1% and 50% of correction (Table 1). On lateral radiogram, the average thoracic kyphosis remained unchanged from preoperative 27.6° to postoperative 19.9° (p = 0.376, paired t test) and at final follow-up, 18.2° (p = 0.254, paired t test). The average lumbar lordosis improved from a preoperative 15.6° of kyphosis to a postoperative lordosis of −22.4° (p = 0.0002, paired t test), which was maintained at the final follow-up with lordosis of −20.9° (p = 0.0004, paired t test) (Table 1). On evaluating the functional status (Table 2), there were 20 patients confined to bed and 7 sitting with support. Postoperatively, all patients improved at least by one grade; 21 could sit without support, 4 improved to sitting with support from the bedridden position and 1 remained in bed (unchanged). One patient died perioperatively. Evaluation of the postoperative functional status of each patient showed that most of the patients had major to moderate improvement in sitting balance, cosmetic appearance, functional freedom of arms, nursing care by parents, overall satisfaction and overall respiratory functions as compared to the preoperative functional status (Table 3). None of the patients had worsening of the functional status.
There were 13 (48.1%) perioperative complications in the study (Table 4) and 1 patient with DMD died during the operation due to a sudden cardiac arrest. He was an 8-year-old boy with a Cobb angle of 50° and operated on with pedicle screw fixation from T2 to L5. The patient was known to have cardiomyopathy detected on preoperative echocardiogram with an EF of 50%. Intraoperatively, he had EBL of 4,800 ml and, after the rod derotation procedure, developed sudden cardiac arrest due to arrhythmia and reanimation attempts were unsuccessful. There were four (14.8%) major complications and all were respiratory complications in the form of hemothorax or respiratory failure that required ventilator support. They were all treated with insertion of chest tube and their symptoms were relieved immediately. Chest tubes were removed within 1 week in all of them. There were eight (29.6%) minor complications in the study. The most common minor complication was UTI in three (23%) patients, two (1.5%) had atelectasis as well as neurological complications and one (0.7%) patient had ileus. UTI was believed to result from postoperative catheterization, which was treated with appropriate antibiotics according to urine culture and sensitivity report. Atelectasis was treated with positive pressure oxygenation support and recovered was good. Ileus was treated with restricting fluids orally and intravenous fluid therapy. Neurologically, two patients had complications in the form of radicular pain or tingling sensations in the lower limbs. Thorough neurological examination with straight leg raising tests and motor and sensory system examination did not reveal any difference from preoperative neurological status. Postoperative radiogram and CT scan of the whole spine showed well-positioned screws within the pedicles and, therefore, no procedure was done further. These neurologic symptoms were believed to be related to stretching of the nerve roots and or the spinal cord and managed conservatively. Both the patients recovered within 6 weeks of operation. We performed CT scans in all patients postoperatively, which suggested that 93% (746/803) of the pedicle screws were within 2 mm of the medial and within 4 mm of the lateral pedicle wall and were considered safe. There were 172 (21.5%) screws that had breached either medial (56/803 = 6.9%) or lateral (117/803 = 14.4%) to the pedicle walls. Of the 56 pedicle screws that had violated the medial pedicle wall, 40 and 16 had penetration <2 mm and 2–4 mm, respectively. Of 117 pedicle screws that had violated the lateral pedicle wall, 41, 34 and 41 had penetration <2, 2–4 and 4–6 mm, respectively. None of the displaced screw caused any neurological complications in any patients. Similarly, there were no implant-related complications perioperatively. There were ten (37%) patients who required postoperative intensive care unit (ICU) support: 7 due to hypovolemia and 3 due to hemothorax. Out of them, three patients required ventilator support: 2 due to hemothorax and 1 due to hypovolemia. Ventilators were weaned off within 24 h in all patients. Rest of the patients were given oxygenation support overnight (Table 5). Average EBL (estimated blood loss, measured in the 100-ml range) in the study was 3,003 ± 1,634 ml (range, 800–7,800 ml), which was 123 ± 88% (range, 33–412%) of the total blood volume. There were 15 patients who had EBL more than 100% of total blood volume, while 8 had EBL between 50 and 100% of their blood volume. However, this increased EBL did not have any effect on the duration of hospital stay (p = 0.85, 20 days in patients who had EBL more than 100% versus 19.7 days in those who had EBL less than 100%) (Table 5).
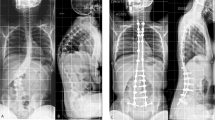
Complications that presented after the discharge from hospital were considered as postoperative complications (Table 4). Twelve (44.4%) patients had postoperative complications, which were ultimately solved. There were seven and five postoperative complications in patients with Cobb angle <90° and >90°, respectively, which did not establish any relationship between implant-related (postoperative) complications and severity of curve (p = 0.928, chi-square). Seven (25.9%) had coccygodynia, four (14.8%) had sore on the convex side at the apex and one (3.7%) had dislodging of rod from the distal end on the convex side. None of the patients had rod or screw breakage. All the patients who had coccygodynia complained of continuous pain, which interfered their moving ability with the wheelchair. Their coccyx radiogram showed mild subluxation. In these patients, CT scan did not show any pedicle screw displaced that could cause irritation to the nerve roots producing referred pain. Clinically there was significant tenderness on the coccyx. Patients were treated conservatively with modification in the sitting posture in the form of cushion having a central hole that avoided pressure on the coccyx while sitting. One patient with ccoccygodynia and coccyx subluxation was not relieved with conservative treatment and had to undergo a coccyx excision (Table 4; case 1; Fig. 1). After coccyx excision, his pain was relieved within 6 months. The treatment symptoms improved in all patients within 6 months of initiation of treatment. Two patients had DMD and SMA, respectively, who developed back sore on the convex side of the curve at the apex (Fig. 2) due to irritation by the screw head (Table 4; cases 10, 16, 19, 23). The screw head was palpable from the sore and they were treated with removal of at least four screws, including the causative screw, and reconstruction of the fixation. All symptoms resolved after this procedure. One 15-year-old DMD patient with preoperative Cobb angle of 102°, who was operated for T4–S1 fixation, had a dislodged rod from the S1 screw on the convex side and presented with a complaint of lower back pain 7 months after the operation (Table 4; case 20). The reason for dislodgment was found to be lack of tightening of cap over the screw. He was treated with revision operation, and re-fixation was done along with bone grafting.
a Preoperative AP and lateral radiogram of a 14-year-old boy with DMD and Cobb angle of 44° operated by posterior-only pedicle screw fixation. b Postoperative AP and lateral radiogram shows that there was lumbar kyphosis still persistent in spite of coronal correction. After one-and-half years he developed c back sore due to screw head irritation on the convex side, which was treated with removal of convex-sided prominent three screws and connected with domino. d AP and lateral radiogram after the procedure. Patient’s sore was cured after the procedure
Discussion
To our knowledge, all reports on the correction of scoliosis in patients with paralytic scoliosis deal with instrumentation of the spine using hooks, wires or hybrid instrumentation with pedicle screw in the spine [3, 20, 28, 38, 42, 45]. Recently, Hahn et al. [21] published their experiences with pedicle screws in DMD, which probably was the first report of using pedicle screws in paralytic scoliosis. Here, we presented our experiences of using posterior-only pedicle screws in paralytic scoliosis (DMD and SMA). Unlike previous reports, we specifically laid emphasis on perioperative and postoperative complications. To our knowledge, this is the first report especially about complications using posterior-only pedicle screws in paralytic scoliosis.
Patients with DMD and SMA have poor bone quality and so the correction rate using different instrumentation should be an important factor for comparison. Other studies have shown that an average correction of 40–64% in spinal curvature can be achieved, without much progression in the curve postoperatively [11, 32, 35]. Scoliosis in patients with flaccid neuromuscular pathology (DMD and SMA) is actually a kypho-scoliosis deformity, in comparison to other forms of neuromuscular scoliosis with spasticity where lumbar lordosis is usual [47]. Hahn et al. [21] showed an improvement in lumbar lordosis from 20° to 49°, while thoracic kyphosis remained unchanged. In their series, the mean Cobb angle was 44.2°, which was less compared to our series of 79.8° and probably could be one of the reasons for having difference in lumbar lordosis from our group. We have exhibited improvement in lumbar lordosis from kyphosis of 15.6° to lordosis of −22.4° (p = 0.0002); while thoracic kyphosis remained unchanged as in previous report from 27.6° to 19.9° (p = 0.376).
The literature regarding the surgical management of spinal deformity in flaccid neuromuscular disorders (SMA and DMD) suggests that bilateral instrumentation and fusion to either L5 or sacrum is the most effective [1, 6, 8, 12, 18, 29, 30, 33, 34, 42, 43] and multiple fixation points such as sublaminar wires are preferred. Marchesi et al. [26] selected the modified Galveston technique by inserting two diverging iliac rods over the S1 screw, which subsequently secured tightly with sublaminar wires. Subsequently, Arlet et al. [2] reported the use of MW (maximum width) construct to enhance the stronger and more firm lumbosacral fixation in patients with DMD. They believed that lumbosacral junctions can be fixed by a three-point fixation technique. Here, we have utilized posterior-only pedicle screw fixation from T2–T4 proximally to L5 or sacrum (and/or pelvis) distally. Patients who did not require pelvis fixation (eight patients) had preoperative pelvis obliquity of 9.6°, which was corrected to 4.5° postoperatively, showing 54% correction. It was maintained at 6.3° at final follow-up. Patients who required pelvis fixation (18 patients) had preoperative pelvis obliquity of 22.2°, which was corrected to 11.2° postoperatively, showing 51% correction. It was maintained at 13.4° at final follow-up. Comparison of the correction rate in both groups did not show any significant difference (p = 0.83, unpaired t test). Other reported benefits of scoliosis surgery include an improvement in sitting comfort [30, 32, 35] because the pelvic obliquity, which renders sitting uncomfortable (if not impossible), is corrected by surgery. Other benefits include improved sitting balance, [1, 20, 35] a stable spine [34] and trunk, [16] esthetic improvement, [20, 27] improvement in sitting height, [1, 30] relief from back pain [5] and greater ease with which patients could be transported by relatives [20]. The improved sitting balance resulted in greater functional freedom of the arms [1, 27, 32] as they could now be used for purposes other than supporting the trunk. Almost all the patients in other studies [20, 32, 35] were of the opinion that surgery had been worthwhile. Cervellati et al. [10] in their study of 20 patients with DMD treated surgically noted that the only important goal of spinal surgery in DMD was to improve the quality of life of these patients. We have experienced the same findings in the immediate postoperative period, as most of our patients had major to moderate improvement in sitting balance, greater functional freedom of the arms, better nursing care by their parents or caretakers, cosmetic appearance, overall functional status and satisfaction with surgical procedure as well as respiratory functions (Table 3). On evaluating the ambulatory status, there were 14 patients from class 5 and 7 patients from class 4, who improved to class 3 and became ambulatory in wheelchair without supporting themselves with their arms. Four patients from class 5 improved to class 4 and became ambulatory in wheelchair with the support of their arms (Table 2). Only one patient who had a Cobb angle of 150° (DMD) did not have improved functional ability, while one patient died perioperatively.
In spite of good results and benefits of surgery in flaccid neuromuscular scoliosis, complication rate is believed to be high with surgical treatment. Ramirez et al. [33] noted 27% major intraoperative or postoperative complications and 16% minor complications for an overall complication rate of 43% in their series of 22 DMD patients treated with Luque segmental instrumentation. The major complications involved one, or a combination, of three areas: cardiopulmonary compromise, infection and instrumentation failure. Aprin et al. [1], in their study on 22 patients with SMA using anterior Dwyer instrumentation, noted that the common immediate postoperative complications were pneumonitis and atelectasis, which nearly always occurred in patients who had anterior spine fusion and were not infrequent in those with posterior spine fusion. The major late complication was narrowing of the diameter of the chest, which was probably due to the pressure of the cast or progression of muscle weakness, or both. Complication rates between 32 and 61% have been reported previously but, within each study, have received little emphasis [37, 40, 41, 44–46].
On reviewing surgical treatment in DMD, Swank et al. [43] reported a complication rate of 61% (eight of 13 patients) using Harrington instrumentation. Weimann et al. [46] reported 54% (13of 24 patients) using Harrigton instrumentation; Sussman [42] reported 36% (four of 11 patients) using segmental spinal instrumentation; Gibson et al. [19] reported 50% (five of 10 patients); LaPrade and Rowe [24] reported 33% (three of nine patients) using sublaminar wiring, and Mubarak et al. [29] reported 32% complications (seven out of twenty18 two patients) using Luque instrumentation. In the present study, we divided the complications into two groups: perioperative complications that presented during the hospital stay and postoperative complications that presented after discharge from hospital. We found 48.1% (13 out of 27 patients) perioperative complications: 30.7% major and 61.5% minor complications. Our complication rates appear to be similar with that of other instrumentation in literature; however, we feel that using pedicle screws, we could avoid further anterior procedure and get a strong purchase of implants. However, higher estimated blood loss (EBL) during the surgery could be related to the generalized osteoporotic quality of the bone and inserting pedicle screw at each level. Therefore, we feel that minimizing the number of pedicle screws in such patients would further decrease operative time as well as EBL. Though all patient were operated by posterior-only approach, major complications were respiratory (hemothorax or respiratory failure) that required chest tube insertion for drainage and/or ICU stay. Three patients with DMD developed hemothorax within 1 week of operation. Postoperative CT scan did not reveal any injury to the vessel or lung due to pedicle screws. We think that marked osteoporosis and breaching of the lateral wall of the pedicle and or the anterior vertebral body cortex, during pedicle screw probing or insertion, may be responsible for pneumo and or hemothorax. Minor complications were UTI, atelectasis, and neurological and paralytic ileus. UTI was caused due to catheterization and minor neurological symptoms were due to the stretching effect on the nerve root. None of the patients with minor complications had permanent sequel; all sequelae resolved within 6 weeks after operation. All major complications that required ventilator and ICU support improved within few days.
The overall rate of postoperative complications at the final follow-up was found to be 44.4% (12 out of 27), and a majority of these complications, such as coccygodynia and back sores, have not been described in literature. Additionally, 6 out of 12 patients (50%) with postoperative complications had to undergo a secondary procedure. On analyzing the coccygeal radiogram, we could find subluxation in most of the radiograms and the probable reason could be the vertical transfer of body weight after the correction of scoliosis and sagittal balance. Another possible cause could be that the patients had increased sitting ability after the correction, which could have increased the load over the coccyx. One coccygodynia could not resolve with conservative treatment and required coccygeal excision. Regarding coccygodynia, if we see mild subluxation of coccyx, there would be higher chances of developing postoperative coccygodynia. Such complications could be avoided by precautionary explanation to the patients, as well as cushion support for sitting purpose soon after the operation. Regarding the convex side back sore, retrospectively we feel if we had inserted low profile screws on the convex side near the apex, these complications could have been avoided. We think that on the convex side, there was constant irritation between the screw head and soft tissue (due to poor soft tissue coverage over the screw head), which resulted in back sore ultimately. Complications such as dislodging of rod from screw can be prevented by ensuring proper tightening of cap over the screw before the closure. In such cases, we feel that using a rod with a stopper at the distal end would solve this problem of dislodging of rod distally.
In conclusion, we can say that posterior-only pedicle screw fixation can correct the scoliosis in flaccid neuromuscular patients, such as DMD and SMA, with good maintenance over a period of time. However, after this critical review of our series, we feel that inserting less pedicle screw or even using some sublaminar wires at the apex in thin patients could further reduce the rate of pedicle screw complications. In addition, complications such as coccygodynia should always be kept in mind.
References
Aprin H, Bowen JR, MacEwen GD, Hall JE (1982) Spine fusion in patients with spinal muscular atrophy. J Bone Joint Surg Am 64:1179–1187
Arlet V, Marchesi D, Papin P, Aebi M (1999) The ‘MW’ sacropelvic construct: an enhanced fixation of the lumbosacral junction in neuromuscular pelvic obliquity. Eur Spine J 8:229–231
Basobas L, Mardjetko S, Hammerberg K, Lubicky J (2003) Selective anterior fusion and instrumentation for the treatment of neuromuscular scoliosis. Spine 28(20):S245–S248
Bianchi ML, Mazzanti A, Galbiati E, Saraifoger S, Dubini A, Cornelio F, Morandi L (2003) Bone mineral density and bone metabolism in Duchenne muscular dystrophy. Osteoporos Int 14(9):761–767
Bridwell KH, Baldus CL, Iffrig TM, Lenke LG, Blanke KR (1999) Process measures and patient/parent evaluation of surgical management of spinal deformities in patients with progressive flaccid neuromuscular scoliosis (Duchenne’s muscular dystrophy and spinal muscular atrophy). Spine 24(13):1300
Brook PD, Kennedy JD, Stern LM, Sutherland AD, Foster BK (1996) Spinal fusion in Duchenne’s muscular dystrophy. J Pediatr Orthop 16:324–331
Brown CA, Lenke LG, Bridwell KH, Geideman WM, Hasan SA, Blanke Kathy RN (1998) Complications of pediatric thoracolumbar and lumbar pedicle screws. Spine 23(14):1566–1571
Brown JC, Zeller JL, Swank SM, Furumasu J, Warath SL (1989) Surgical and functional results of spine fusion in spinal muscular atrophy. Spine 14:763–770
Castro WH, Halm H, Jerosch J, Malms J, Steinbeck J, Blasius S (1996) Accuracy of pedicle screw placement in lumbar vertebrae. Spine 21:1320–1324
Cervellati S, Bettini N, Moscato M, Gusella A, Dema E, Maresi R (2004) Surgical treatment of spinal deformities in Duchenne muscular dystrophy: a long-term follow-up study. Eur Spine J 13(5):441–448
Chng SY, Wong YQ, Hui JH, Wong HK, Ong HT, Goh DY (2003) Pulmonary function and scoliosis in children with spinal muscular atrophy types II and III. J Paediatr Child Health 39:673–676
Daher YH, Lonstein JE, Winter RB, Bradford DS (1985) Spinal surgery in spinal muscular atrophy. J Pediatr Orthop 5:391–395
Dvorak M, MacDonald S, Gurr KR, Bailey SI, Haddad RG (1993) An anatomic, radiographic and boimechanical assessment of extrapedicular screw fixaiton in thoracic spine. Spine 18:1689–1694
Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS (2002) Outcome and complications of long fusions to the sacrum in adult spine deformity: Luque–Galveston, combined iliac and sacral screws, and sacral fixation. Spine 27(7):776–786
Esses SI, Sachs BL, Dreyzin V (1993) Complications associated with the technique of pedicle screw fixation. A selected survey of ABS members. Spine 18:2231–2239
Evans GA, Drennan JC, Russman BS (1981) Functional classification and orthopaedic management of spinal muscular atrophy. J Bone Joint Surg Br 63:516–522
Faraj AA, Webb JK (1997) Early complications of spinal pedicle screw. Eur Spine J 6:324–326
Galasko CSB, Delaney C, Morris P (1992) Spinal stabilisation in Duchenne muscular dystrophy. J Bone Joint Surg Br 74:210–214
Gibson DA, Koreska J, Robertson D, Kahn A, Albisser AM (1978) The management of spinal deformity in Duchenne’s muscular dystrophy. Orthop Clin North Am 9:437–450
Granata C, Merlini L, Cervellati S, Ballestrassi A, Giannini S, Corbascio M, Lari S (1996) Long-term results of spine surgery in Duchenne muscular dystrophy. Neuromuscul Disord 6(1):61–68
Hahn F, Hauser D, Espinosa N, Blumenthal S, Min K (2008) Scoliosis correction with pedicle screws in Duchenne muscular dystrophy. Eur Spine J 17:255–261
Hoffer MM, Feiwell E, Perry R, Perry J, Bonnett C (1973) Functional ambulation in patients with myelomeningocele. J Bone Joint Surg Am 55(1):137–148
Hsu JD (1982) Skeletal changes in children with neuromuscular disorders. Prog Clin Biol Res 101:553–557
LaPrade RF, Rowe DE (1992) The operative treatment of scoliosis in Duchenne muscular dystrophy. Orthop Rev 21:39–45
Lin LC, Jong YJ (2004) Pulmonary function assessment in patients with spinal muscular atrophy type II and type III. Acta Paediatr Taiwan 45(1):15–18
Marchesi D, Arlet V, Stricker U, Aebi M (1997) Modification of Luque technique in the treatment of Duchenne’s muscular dystrophy. J Pediatr Orthop 17:743–749
Merlini L, Granata C, Bonfiglioli S, Marini ML, Cervellati S, Savini R (1983) Scoliosis in spinal muscular atrophy: natural history and management. Dev Med Respir Dis 128:1002–1007
Mohamad F, Parent S, Pawelek J, Marks M, Bastrom T, Faro F, Newton P (2007) Perioperative complications after surgical correction in neuromuscular scoliosis. J Pediatr Orthop 27(4):392–397
Mubarak ST, Morin WD, Leach J (1993) Spinal fusion in Duchenne muscular dystrophy: fixation and fusion to the sacropelvis? J Pediatr Orthop 13:752–757
Phillips DP, Roye DP, Farcy JC, Leet A, Shelton YA (1990) Surgical treatment of scoliosis in a spinal muscular atrophy population. Spine 15:942–945
Phillips JH, Gutheil JP, Knapp DR Jr (2007) Iliac screw fixation in neuromuscular scoliosis. Spine 32(14):1566–1570
Piasecki JO, Mahinpour S, Levine DB (1986) Long-term follow-up of spinal fusion in spinal muscular atrophy. Clin Orthop 207:44–54
Ramirez N, Richards BS, Warren PD, Williams GR (1997) Complications after posterior spinal fusion in Duchenne’s muscular dystrophy. J Pediatr Orthop 17:109–114
Riddick MF, Winter RB, Lutter LD (1982) Spinal deformities in patients with spinal muscular atrophy: a review of 36 patients. Spine 7:476–483
Robinson D, Galasko CSB, Delaney C, Williamson JB, Barrie JL (1995) Scoliosis and lung function in spinal muscular atrophy. Eur Spine J 4:268–273
Sarwark J, Sarwahi V (2007) New strategies and decision-making in the management of neuromuscular scoliosis. Orthop Clin North Am 38:485–496
Schuffelbarger HL, Neustadt JB, Cammisa FP (1992) Spinal fusions to the pelvis augmented by Cotrel–Dubousset instrumentation for neuromuscular scoliosis. J Pediatr Orthop 12:465–469
Sengupta DK, Mehdian SH, McConnell JR, Eisenstein SM, Webb JK (2002) Pelvic or lumbar fixation for the surgical management of scoliosis in Duchenne muscular dystrophy. Spine 27(18):2072–2079
Söderpalm AC, Magnusson P, Ahlander AC, Karlsson J, Kroksmark AK, Tulinius M, Swolin-Eide D (2007) Low bone mineral density and decreased bone turnover in Duchenne muscular dystrophy. Neuromuscul Disord 17(11–12):919–928
Steib JP, Ducrocq X, Averous C, Bogorin J (1999) Surgical correction of lumbar scoliosis: a comparison of different techniques. Results. Eur J Orthop Surg Traumatol 9:151–156
Sussman M (1985) Treatment of scoliosis in Duchenne muscular dystrophy. Dev Med Child Neurol 27:522–524
Sussman MD (1984) Advantage of early spinal stabilization and fusion in patients with Duchenne muscular dystrophy. J Pediatr Orthop 4:532–537
Swank SM, Brown JC, Perry RE (1982) Spinal fusion in Duchenne’s muscular dystrophy. Spine 7:484–491
Tangsrud SE, Petersen IL, Carlsen KCL, Carlsen KH (2001) Lung function in children with Duchenne’s muscular dystrophy. Resp Med 95:898–903
Thacker M, Hui JH, Wong HK, Chatterjee A, Lee EH (2002) Spinal fusion and instrumentation for paediatric neuromuscular scoliosis: retrospective review. J Orthop Surg (Hong Kong) 10(2):144–151
Weimann R, Gibson DA, Moseley C, Jones D (1983) Surgical stabilization of the spine in Duchenne muscular dystrophy. Spine 8:776–780
Wilkins K, Gibson DA (1976) The pattern of spinal deformity in Duchenne’s muscular dystrophy. J Bone Joint Surg Am 58:24–32
Acknowledgment
None of the authors or their family members has received financial benefits from any commercial party for this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Modi, H.N., Suh, SW., Hong, JY. et al. Treatment and complications in flaccid neuromuscular scoliosis (Duchenne muscular dystrophy and spinal muscular atrophy) with posterior-only pedicle screw instrumentation. Eur Spine J 19, 384–393 (2010). https://doi.org/10.1007/s00586-009-1198-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-009-1198-z