Abstract
The timing of premenstrual syndrome (PMS) suggests that hormonal fluctuations are a key component in its pathogenesis. Unfortunately, women with PMS cannot be distinguished from asymptomatic women regarding biological markers. Research suggests that increased susceptibility to hormonal changes among women with PMS may be explained by the theory of cognitive vulnerability to affective disorders. The study group comprised 127 women (aged 19–35). The participants were divided into four groups: asymptomatic, nondepressed with PMS, depressed without PMS, and both depressed and with PMS. PMS was diagnosed by prospective daily reports, and depression by SCID-IV. All participants completed the Cognitive triad inventory (CTI), Metacognitive belief questionnaire (MCQ-30), and the self-referent information processing task (SRET) randomly either in the follicular or luteal phase. Findings indicated that only the asymptomatic women differed in cognitive processing from the depressed women. Those with PMS, despite demonstrating a slightly greater intensity of distorted cognitive processing, did not differ significantly from the asymptomatic participants; however, they differed from those with depression regarding in the cognitive triad. The phase of the cycle was not a significant factor in differentiating distorted cognitive processing. Depressed women have more distorted cognitive processes than non-depressed women. Women with PMS appear to be a group that lies between asymptomatic women and those who suffer from depression. Moreover, among women with depression, those with PMS have even more severe distorted cognitive processing than those without PMS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The etiology of PMS is poorly understood. Although all women experience hormonal changes during their menstrual cycle, few suffer from PMS, and although the symptoms correspond with biologically-based changes in the menstrual cycle, no biological factors differentiating women with and without PMS have been distinguished (Amiel Castro et al., 2019; Comasco & Sundström-Poromaa, 2015). Several biological mechanisms that underline PMS have been proposed, most of which focus on the interactions between gonadal hormones and serotonin and GABA. It has been suggested that more susceptible women may demonstrate increased sensitivity to changes in these systems (Halbreich, 2003). These findings provide support for the hypothesis that there is a subgroup of women who is more susceptible to physical, psychological, and sexual symptoms related to the hormonal shifts or abrupt hormonal fluctuations that occur throughout the reproductive lifespan (Pope et al., 2017). The factors leading to this vulnerability, however, are still unknown.
The observation that high rates of comorbidity and symptoms overlap between PMS and depression suggests that the two conditions share vulnerability factors (Craner et al., 2015); indeed, 11.3% of women with moderate PMS and 24.6% with severe PMS symptoms also had comorbid depressive disorder (Forrester-Knauss et al., 2011). Among women with prospectively-confirmed PMS and who are not in a current depressive episode, 30–70% had experienced a prior episode of major depression (Yonkers & McCunn, 2007). As a consequence, attempts have recently been made to examine the psychological constructs that may lead to increased vulnerability for PMS. Of these, the most promising paradigm is the theory of cognitive vulnerability to emotional disorders (Alloy & Riskind, 2006).
Cognitive vulnerability model postulated that individuals with maladaptive cognitive styles and attitudes are more likely to make dysfunctional interpretations of stressful events that increase vulnerability to emotional disorders (Riskind & Alloy, 2006). According to this theory, distal cognitive vulnerabilities develop during childhood. The negative schemata shaped in childhood are internal frameworks, constructed of attitudes, beliefs, and concepts used to interpret present, past, and future events. These distal vulnerabilities during stressful events lead to proximal cognitive processes: biased information processing. Furthermore, cognitive vulnerabilities and biological diatheses mutually moderate each other’s effect on the development of future emotional disorders. Thus, Riskind and Alloy (2006) postulated that despite the presence of biological factors in PMS, clinical experience shows that they are associated with maladaptive cognitive styles similar to those of people with depression. Bodily symptoms and hormonal changes may serve as “stresses” in cognitive vulnerability-stress interactions. The presence of negative cognitive styles will therefore differentiate whether PMS symptoms will appear after the onset of “stress” in the luteal phase.
Several studies have highlighted the risk factors shared by depression and PMS. Women with PMS report greater use of self-focused attention (SFA) in response to negative affect (Craner et al., 2015). SFA is defined as an excessive, sustained, and rigid focus on internally-generated information, such as physical symptoms or mood.
It has also been found that rumination predicted PMS and was associated with slower postmenstrual remission of PMS symptoms (Craner et al., 2014; Dawson et al., 2017). Rumination is an emotion-focused strategy for coping with distress, in which someone repetitively and passively focuses on the distress itself, as well as its possible causes and consequences. Many studies indicate that rumination occurring in response to sadness is a factor of cognitive vulnerability to depressive disorders (Nolen-Hoeksema et al., 2008). One such factor is the attributional style, which has been found to be significantly related to PMS (Kiesner et al., 2016).
In another study, attributional style was found to be unrelated to the occurrence of PMS and PMDD (Premenstrual Dysphoric Disorder) (Śliwerski & Bielawska-Batorowicz, 2019). However, women with PMS demonstrated a worse cognitive triad and negatively self-referring information processing, but only in the luteal phase of the cycle. After failure induction, only women with PMS responded with increased sadness and irritation, and this mood change was associated with distorted cognitive processing.
The result of a study may be influenced by the fact of whether women with affective and anxiety disorders were included in the study. Only individual studies on SFA (Craner et al., 2015) and rumination (Dawson et al., 2017) excluded women with emotional disorders diagnosed by structured interview. However, no studies have compared whether women with PMS but without comorbidity differ from those with depression and PMS and those with depression alone in terms of the distorted cognitive processing.
The aim of the present study is to verify whether distorted cognitive processing differentiates women with PMS from those without PMS. It is hypothesized that the presence of distorted information processing will explain why only some women have PMS symptoms, even though all of them experience biological/hormonal changes. The second aim is to verify whether the elements of cognitive vulnerability to emotional disorders are a constant trait or occur only in the luteal phase of the cycle. According to the theory of cognitive vulnerability, biased information processing should be present only in the luteal phase, while negative beliefs about self, the world, and the future as a part of distal vulnerability should occur independently of the phase. Finally, the third aim of the study is to verify whether women with PMS alone differ in their cognitive processing from those with depression, and either with or without PMS. It is hypothesized that women with PMS will differ from both depressed and asymptomatic women.
Methods
Participants and Procedure
The entire study, along with its research plan, hypotheses, methods, and planned statistical analysis, has been pre-registered (Śliwerski, 2019). Approval for the study was obtained from the local ethics committee of the University of Lodz before it began and therefore the research was conducted in accordance with the 1964 Helsinki Declaration. A total of 127 women aged 19–35 participated in the study. Participants were recruited via Internet advertisement between June 2018 and April 2019. The invitation for the study contained information about the aim of the study, inclusion criteria, and remuneration for participation in the study. Those who were willing to participate were screened for eligibility criteria. The inclusion criteria for the study were as follows: age between 19 and 35 years old and regular menstrual cycle (20–34 days). This is a standard age range for participants in PMS research since PMS appears to be most severe between the age of 19 and 35 (Freeman, 2003). The exclusion criteria comprised a diagnosis of any hormonal problems (like hyperthyroidism, hypothyroidism, and hyperprolactinemia), endometriosis, amenorrhea, ongoing pregnancy, or fertility problems. The participants in the group of asymptomatic women or women with PMS without comorbidity could not take any psychiatric medications that could significantly reduce PMS symptoms.
In the first stage of the study, after filling in an informed consent form, the participants were screened using the Premenstrual symptoms screening tool (PSST; Steiner et al., 2003) and Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). As the study included women with and without PMS, as well as those with and without depression, the screening was aimed at preliminary verification of the division into groups, to keep the sizes relatively equal. None of the participants were excluded from the study due to the screening test results.
All participants who agreed to participate in the study were scheduled for a diagnostic interview to screen for psychiatric disorders (Structured Clinical Interview for DSM-IV-TR Axis I Disorders SCID-IV; First et al., 2014) and were asked to make daily ratings of their symptoms for a minimum of two consecutive menstrual cycles. SCID-IV was conducted by trained psychologists blinded to the results obtained in the screening test. Women were asked to make daily ratings of their symptoms for a minimum of two consecutive menstrual cycles and were instructed to log into a personal account on the custom-built website every day and rate their symptoms. If the participant forgot to complete the calendar, she received a reminder from the system. The participants were randomly assigned to groups in which the Cognitive triad inventory (CTI; Beckham et al., 1986), Metacognitions questionnaire (MCQ-30; Wells & Cartwright-Hatton, 2004), and the self-referent encoding task (SRET; Taylor & Ingram, 1999) were completed in either the follicular or luteal phase. Participation was remunerated upon completion of all stages of the study (100 PLN—the equivalent of 23 EUR).
Initial interest in the study was expressed by 451 women. After becoming acquainted with the purpose and method of conducting the study, 185 resigned from further participation: In addition, a further 139 withdrew from participation during the course of the study: two became pregnant during the cycle monitoring, two refused to participate in the diagnostic interview, four women went abroad, and the remainder stopped filling out the calendar without giving any reason for their resignation. Women who withdrew from participation in the study did not differ from the final sample in terms of age, cycle length, depression, cognitive triad, metacognitive beliefs, and PMS.
Measures
The Premenstrual Symptoms Screening Tool (PSST) (Steiner et al., 2003) is a retrospective self-report questionnaire developed to screen for PMS and PMDD symptoms. The PSST was developed according to DSM diagnostic criteria. The tool is divided into two parts: one evaluating the intensity of 14 symptoms in the luteal phase of the cycle and the other assessing the degree to which these symptoms influence effectiveness at work, activity, and relations with people. Each item is rated on a four-point scale. A diagnosis of PMS requires at least five symptoms to be defined as moderate or severe. Moreover, it was required that the symptoms interfered with functioning, at least moderately. The internal consistency measured for the present study was high (Cronbach’s α = 0.90, CI95 [0.87,0.92]).
Calendar of Premenstrual Symptoms. All participants recorded their PMS symptoms every day for two consecutive menstrual cycles. The tool consisted of 11 items representing various symptoms of premenstrual distress: depressed mood or dysphoria, anxiety/tension, mood lability, irritability, decreased interest in usual activities, poor concentration, marked lack of energy, marked change in appetite, hypersomnia, or insomnia, feeling overwhelmed, and physical symptoms such as bloating. Finally, participants rated the extent to which these symptoms interfered with their work, activities, or relationships. Like the retrospective PSST, the items are rated based on a four-point scale. Calendar scores were summed across the daily symptom reports for three five-day periods: the last days of the luteal phase, the first days of the menstrual cycle, and the follicular phase (from 12–16 days after the last menses). For a diagnosis of PMS, the participants had to mark at least five symptoms as moderate or severe for at least 2 days in the luteal phase, without showing any symptoms in the middle of the cycle. Additionally, they had to note that their symptoms interfered with their functioning at least in a moderate way. Within this sample, high internal consistency was observed for the total score (beginning of the cycle α = 0.92, CI95 [0.89,0.94]; ovulation phase α = 0.93, CI95 [0.92,0.94]; luteal phase α = 0.95, CI95 [0.93,0.96]).
The Center for Epidemiologic Studies-Depression Scale (CES-D). CES-D (Radloff, 1977) is a self-report inventory consisting of 20 items, used to measure symptoms associated with depression experienced in the past week. The CES-D results allowed participants to be screened to identify the number who may have had depression. The internal consistency for the present study was high (Cronbach’s α = 0.91, CI95 [0.90,0.92]).
Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID-IV-I). The SCID-IV-I (First et al., 2014) is a semi-structured interview used to assess psychiatric disorders. The structural interview was used to diagnose the presence of current depressive disorders. During the interview, the participants were also asked about depressive symptoms occurring in the last 3 years. Interviewers were blind to screening test scores. Any participants diagnosed with depression and those who had experienced depression within the last 3 years were included in the depression group.
The Cognitive Triad Inventory (CTI). The CTI (Beckham et al., 1986) is a self-descriptive questionnaire used to asses thoughts about the self, the world, and the future. The scale consisted of 36 items scored on a seven-point Likert scale; these were divided into three subscales with high scores indicating a positive view, and low ones indicating a negative view. The division into three subscales (viz. view of the self, view of the world, and view of the future) is only theoretical: research shows that the CTI has a one-factor structure. The triad is believed to refer to the view of the self as a whole, and view of the self in the world, and the view of the self in the future (Haaga et al., 1991). Hence the single factor of the CTI is labeled as “self-relevant negative attitude” (McIntosh & Fischer, 2000). Internal consistency for the present study was high (Cronbach’s α = 0.90, CI95 [0.90,0.91]).
The Self-Referent Encoding Task (SRET). SRET (Taylor & Ingram, 1999) is used to measure biased information processing. It consists of 26 adjectives (10 had positive valence, 10 negative, and six neutral). Three neutral adjectives were included at the beginning and at the end of the whole list to prevent the effect of priority and novelty. The participants were asked to note whether a given adjective describes them by marking the answer “yes” or “no”. After all the answers were given, the participants were asked to recall as many words from the list as possible. The primary aim of the task was to count the number of recalled self-referent negative adjectives; in addition, the number of positive and negative adjectives used to describe the self was also calculated.
The Metacognition Questionnaire-30 (MCQ-30). MCQ-30 (Wells & Cartwright-Hatton, 2004) measures individual differences regarding a selection of metacognitive beliefs, judgments, and tendencies to overcontrol. The MCQ-30 has 30 items and a five-factor structure consisting of cognitive confidence, positive beliefs about worry, cognitive self-consciousness, negative beliefs about the uncontrollability of thoughts and danger, and beliefs about the need to control thoughts. The internal consistency was high for the total score scale in the present study (Cronbach’s α = 0.98, CI95 [0.98,0.98]) and for the five subscales (Cronbach’s α range 0.93–0.98).
Data Analysis
To compare the groups, the assumption of normality was first verified for the studied variables. It was found that almost none of the variables demonstrated a normal distribution. This is due to the fact that these variables do not typically have a normal distribution in the general population: both the prevalence of depressive symptoms and distorted cognitive processing have a skewed distribution.
Despite not being normally distributed, the data were analyzed with a parametric test as long as homogeneity of variance was maintained. In the case of any significant statistical difference, a parallel non-parametric test was applied. Unless otherwise indicated, both methods showed a significant difference. There were few missing data in the database due to the data collection method. Thus, every statistical analysis excluded all missing data with the na exclude = TRUE function.
To verify the hypothesis that negative cognitive styles differentiate women with PMS from those without PMS, a mixed-model ANOVA series was conducted (with the Kruskal–Wallis non-parametric test). The same two-way ANOVA was used to verify the hypothesis that negative cognitive styles differentiate PMS and non-PMS groups only during the luteal phase of the cycle, and the hypothesis that women with PMS differ in cognitive styles from depressed women with and without PMS. To make the description of the results clearer, the groups were assigned the following symbols: asymptomatic (PMS − , dep −); PMS without depression (PMS + , dep −); depressed without PMS (PMS − , dep +) and depressed with PMS (PMS + ,dep +). All calculations were performed in RStudio (RStudio Team, 2015) using the psych, effectsize, dplyr, ltm, and ggplot2 packages with a p-value of < . 05 considered significant.
Results
Participants Characteristics
The mean age of the participants (N = 127) was 24.39 years (SD = 3.32) and their mean length of education was 15.89 years (SD = 1.49). The four subgroups, divided on the basis of the occurrence of depression and PMS, differed significantly with regard to cycle length (F(3,123) = 3.700, p < 0.05, η2 = 0.08, CI90 [0.01,0.16]). Tukey’s HSD test found that asymptomatic women differ from both depressed groups, i.e., with and without PMS. In addition, the groups differed in the occurrence of depression symptoms measured with the CES-D (F(3,123) = 8.278, p < 0.001, η2 = 0.17, CI90 [0.07,0.26]); the Tukey’s HSD test found the asymptomatic group to differ from both depressed groups; however, no difference was observed between the asymptomatic group (PMS − , dep −) and the PMS without depression group (PMS + , dep −). In addition, PMS without depression (PMS + , dep −) differed significantly from PMS with depression (PMS + , dep +), but no differences were found with the depression without PMS group (PMS − , dep +). However, no differences were found between the study groups in terms of age or years of education (see Table 1). Also, 22% (n = 28) of participants reported using oral contraception (OC); however, no differences in use were found between groups (χ2(3) = 6.49, p > 0.05).
Distorted Cognitive Processing Among Women with and Without PMS According to Cycle Phase
In order to examine the differences in distorted cognitive processing between women with PMS and those without PMS, and whether the elements of cognitive vulnerability to emotional disorders are a constant trait or occur only in the luteal phase of the cycle, a mixed-model ANOVA analysis was conducted.
Results of a 4 (group) × 2 (cycle phase) ANOVA on cognitive triad total score indicated a significant effect for group (F(3,113) = 8.089, p < 0.001, η2 = 0.18 CI90 [0.07,0.27]) and cycle phase (F(1,113) = 3.926, p < 0.05, η2 = 0.03 CI90 [0.00,0.10]). The same effect was observed in the View of the Future scale: group (F(3,113) = 7.040, p < 0.001, η2 = 0.16 CI90 [0.06,0.25]) and cycle phase (F(1,113) = 5.154, p < 0.05, η2 = 0.04 CI90 [0.00,0.12]). The View of the self scale (F(3,113) = 6.100, p < 0.001, η2 = 0.14 CI90 [0.04,0.23]) and the View of the future scale (F(3,113) = 6.878, p < 0.001, η2 = 0.15 CI90 [0.05,0.25]) only demonstrated significant effects for group factor. No interaction effect between group × cycle phase was observed for the cognitive triad scale.
The difference in negative self-referent information processing showed that the group × cycle phase effect was significant only for group (F(3,113) = 3.210, p < 0.05, η2 = 0.07 CI90 [0.01,0.15]). No effect was obtained for the phase of the cycle or for the group × phase interactions. It is worth noticing that the groups did not differ with regard to the number of negative adjectives recalled (F(3,113) = 0.840, p = 0.47) but they did differ regarding negative adjectives that had previously been used to describe themselves.
The same analysis was performed for metacognitive beliefs. The results of a 4 (group) × 2 (cycle phase) ANOVA indicated that there was significant effect for group (F(3,113) = 6.228, p < 0.001, η2 = 0.14 CI90 [0.04,0.23]) in negative belief about worry and uncontrollability and group effect (F(3,113) = 3.210, p < 0.001, η2 = 0.08 CI90 [0.01,0.15]) for the total MCQ-30 score. No phase or interaction effects were observed. Furthermore, positive beliefs about worry, cognitive confidence, self-consciousness, and need to control thoughts did not differentiate research groups nor cycle phases.
Distorted Cognitive Processing Between Women with PMS and Those with Depression
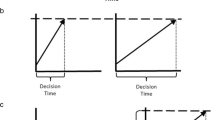
One-way ANOVA was performed to examine the third hypothesis, that women with PMS differ in cognitive styles from depressed women with and without PMS. Where the Bartlett test indicated a lack of homogeneity of variance, the Kruskal–Wallis test was also performed. Post hoc tests were performed with either the Tukey’s HSD or T3 Dunnett method. All differences are shown in Fig. 1.
Distorted cognitive processing between groups with and without depression and those with and without PMS. CTI, Cognitive Triad Inventory total score; SRET, mean number of encoded negative self-referent adjectives; Negative belief, MCQ-30 subscale; MCQ-30, total score of metacognitive functioning scale. *p < .05; **p < .01; ***p < .001
The comparison of the groups in terms of the cognitive triad showed that significant differences occurred mainly in asymptomatic women (PMS − , dep −) (Fig. 1a). They differed from both depressed groups, i.e., those with PMS (PMS + , dep + ; diff = − 26.48, p < 0.001) and without PMS (PMS − , dep + ; diff = − 25.03, p < 0.01). The group with PMS only (PMS + , dep −) differed significantly from the group with depression and PMS (PMS + , dep + ; diff = − 16.41, p < 0.05). No difference was found between women with PMS (PMS + , dep −) and women with depression (PMS − , dep +).
The same comparison for the self-referent encoding task found only asymptomatic women (PMS − , dep −) differed significantly from women with depression but without PMS (PMS − , dep + ; diff = 1.33, p < 0.05). No significant differences were observed between the PMS group (PMS + , dep −) and either group with depression (PMS − , dep + and PMS + , dep +) (Fig. 1b).
A similar relationship was observed regarding negative belief about worry and uncontrollability (Fig. 1c). The asymptomatic group (PMS − , dep −) significantly differed from the two depression groups: i.e., with PMS (PMS + , dep + ; diff = 4.22, p < 0.01) and without PMS (PMS − , dep + ; diff = 4.21, p < 0.01). The PMS only group (PMS + , dep −) did not show any significant differences with the other groups; only a slight trend was observed regarding the group of depressed women with PMS (PMS + , dep + ; diff = 2.76, p = 0.07).
For the MCQ-30 total score (Fig. 1d), the only significant difference was observed between asymptomatic subjects (PMS − , dep −) and women with depression and PMS (PMS + , dep + ; diff = 9.99, p < 0.05).
Discussion
The primary finding of this study was that the four groups of participants, divided according to the presence of depression and PMS, differ in distorted cognitive processing. However, post hoc analysis revealed that both depressive groups (with and without PMS) differ significantly only from the group of asymptomatic women, i.e., those without depression or PMS. The group of women with PMS (PMS + , dep −) had a greater severity of distorted cognitive processing than asymptomatic women (PMS − , dep −) and lower intensity than women with depression (PMS + / − , dep +), but the differences between the groups were too small to be statistically significant.
A methodologically-similar study indicated a difference between women with PMS and those without PMS, both in terms of the cognitive triad and biased information processing (Śliwerski & Bielawska-Batorowicz, 2019). However, in that study women with major depression were not excluded, and participants were only screened with a mood questionnaire. Thus, the biased information processing of depressed women may increase the difference between women with PMS and those without PMS. Both distinguishing women with depression and comparing them with the non-depressed group and with the PMS group in our study showed that these groups differ in cognitive processing.
The results obtained by Craner et al. (2015) showed that women with PMS report greater use of self-focused attention (SFA) than women without PMS. In this study, participants were involved in two stress-inducing procedures: breathing through a straw and performing a task with an unpleasant sound for incorrect responses. The participants with PMS demonstrated higher levels of both emotional and somatic SFA in response to both the psychological and physiological laboratory stress tasks. Irrespective of PMS status, the stress tasks were found to increase the negative affect in a similar way; however, only the PMS group reacted to this negative affect as increased SFA. Thus, they found a difference in distorted cognitive processing between women with PMS and those without after stress induction. In contrary to Śliwerski and Bielawska-Batorowicz (2019), their study excluded women with depression.
Even so, if the biological changes in the luteal phase can trigger the activation of distorted cognitive processing, the question remains open as to why no significant differences in distorted cognitive processing exist between the phases. Previous studies showed differences in cognitive processing only after failure induction. Our study showed that the hormonal changes that occur in the luteal phase alone are not a sufficient stress inducer.
Another possible explanation may concern the current mood of the respondents. The groups were found to differ in their current mood, measured by CES-D, to the same extent as they differed with regard to distorted cognitive processing. In a prospective study, it is very hard to measure the elements of distal vulnerability factors which occurred prior to the appearance of mood changes (Segal & Ingram, 1994). Research on cognitive vulnerability indicates that distal components of this form of vulnerability precede the onset of the first visible symptoms of disorders (Alloy & Riskind, 2006). However, this does not change the fact that proximal factors may be present both just before and during the onset of the disorder. Therefore, both the distorted cognitive processing measured in the study and the methodology of the measurement itself have considerable influence on the research results.
The third hypothesis of this study assumed that the PMS group would differ from the depressed group in terms of distorted cognitive processing. Since we assume that PMS and depression are similar, but not the same, we assume that in terms of distorted cognitive processing, they should also function differently. The results showed that the PMS group (PMS + , dep −) only differed significantly with regard to cognitive triad to the group with PMS and comorbid depression (PMS + , dep +). No difference between groups was found with the other measured cognitive styles. Therefore, women with PMS appear to be a group that lies between asymptomatic women and those who suffer from depression. Moreover, among women with depression, those with PMS have even more severe distorted cognitive processing than those without PMS.
The study brings new elements to the general understanding of cognitive vulnerability to premenstrual disorders. First, using women with depression as one of the comparison groups gives a completely different point of view to previous studies. Differentiating women with PMS from both asymptomatic women, as well as those with depression, will provide an insight into whether the people with depression differ with regard to the examined cognitive processes, or whether they are of a lighter nature. Our findings show that the group with PMS does not function in the same way as those with depression or those without PMS.
The second new element in this study is that it measures three different types of distorted cognitive processing. While cognitive triad and self-referent information processing have already been used in research, metacognitive belief is a completely new element. This is because not only the vision of oneself and the way of processing information but also one’s own attitude to one’s thoughts, can have a huge impact on the phenomena studied.
The present study has implications for the cognitive vulnerability theory. First, it indicates that women with PMS have more severe negative cognitive styles, but not as much as women with depression. Second, the luteal phase alone without stress induction (failure, induction of sadness, etc.) is not sufficient to activate the proximal components of vulnerability. The results of this study also have implications for clinical practice, as the efficacy of SSRIs (Selective Serotonin Reuptake Inhibitors) and hormonal drugs in treating PMS are inconclusive (Hantsoo & Epperson, 2015). Understanding the vulnerability-stress paradigm allowed for better planning of PMS therapy. More importantly, the mere reduction of emotional reactivity by drugs in the cycle’s luteal phase may not be enough in the presence of negative cognitive styles. Finally, our results are consistent with studies presenting the effectiveness of cognitive-behavioral therapy (CBT). The meta-analysis showed that CBT has a better treatment effect at follow-up than SSRIs (Kleinstäuber et al., 2012).
There are several limitations of this study worth considering. The first concerns sample bias. A considerable percentage of women decided not to participate in the study lasting two cycles and this can have a huge impact on the results. The women who dropped out of the study might have shared certain characteristics, such as an overly low or overly high severity of symptoms. In addition, the level of engagement in such lengthy studies might be lower for those with mental health problems (Kannisto et al., 2017). Second, no measures of steroid levels or other biological processes were included. Including hormonal cyclicity changes would allow for richer and more informative analysis regarding activation of distorted cognitive processing. Thirdly, the current sample comprised a highly homogenous group of women at low social risk, living in urban areas. Due to the study design, all participating women were required to have direct access to a computer with an internet connection. There are also limitations for the type of data collected in this study: apart from the SRET method, measuring behavioral indicators, other tools are based on self-report questionnaires.
Conclusion
Our findings do not provide a univocal answer regarding the difference between asymptomatic women, women with PMS, and those with depression in terms of distorted cognitive processing. However, they nevertheless set the stage for future research that should address very basic but important questions. How does the functioning of women with PMS differ from that of women with depression? Can the difference in the studied variables be influenced by the induction or lack of induction of negative affect? In addition, will the measurement of distorted cognitive processing in the same person give different results if measured at different times, i.e., in the follicular and luteal phases of the cycle?
References
Alloy, L. B., & Riskind, J. H. (Eds.). (2006). Cognitive vulnerability to emotional disorders. Lawrence Erlbaum Associates.
Amiel Castro, R. T., Pataky, E. A., & Ehlert, U. (2019). Associations between premenstrual syndrome and postpartum depression: A systematic literature review. Biological Psychology, 147, 107612. https://doi.org/10.1016/j.biopsycho.2018.10.014
Beckham, E., Leber, W. R., Watkins, J. T., Boyer, J. L., & Cook, J. B. (1986). Development of an instrument to measure Beck’s cognitive triad: The Cognitive Triad Inventory. Journal of Consulting and Clinical Psychology, 54(4), 566–567. https://doi.org/10.1037/0022-006X.54.4.566
Comasco, E., & Sundström-Poromaa, I. (2015). Neuroimaging the menstrual cycle and premenstrual dysphoric disorder. Current Psychiatry Reports, 17(10), 77. https://doi.org/10.1007/s11920-015-0619-4
Craner, J. R., Sigmon, S. T., Martinson, A. A., & McGillicuddy, M. L. (2014). Premenstrual disorders and rumination. Journal of Clinical Psychology, 70(1), 32–47. https://doi.org/10.1002/jclp.22007
Craner, J. R., Sigmon, S. T., & Martinson, A. A. (2015). Self-focused attention in response to laboratory stressors among women with premenstrual disorders. Archives of Women’s Mental Health, 18(4), 595–606. https://doi.org/10.1007/s00737-015-0505-4
Dawson, D. N., Eisenlohr-Moul, T. A., Paulson, J. L., Peters, J. R., Rubinow, D. R., & Girdler, S. S. (2017). Emotion-related impulsivity and rumination predict the perimenstrual severity and trajectory of symptoms in women with a menstrually related mood disorder. Journal of Clinical Psychology, 74(4), 579–593. https://doi.org/10.1002/jclp.22522
First, M. B., Popiel, A., Zawadzki, B., Habrat-Pragłowska, E., & Lazarowicz, H. (2014). SCID-I. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version. Pracownia Testów Psychologicznych PTP.
Forrester-Knauss, C., Zemp Stutz, E., Weiss, C., & Tschudin, S. (2011). The interrelation between premenstrual syndrome and major depression: Results from a population-based sample. BMC Public Health, 11(795), 1–11. https://doi.org/10.1186/1471-2458-11-795
Freeman, E. W. (2003). Premenstrual syndrome and premenstrual dysphoric disorder: Definitions and diagnosis. Psychoneuroendocrinology, 28, 25–37. https://doi.org/10.1016/S0306-4530(03)00099-4
Haaga, D. A. F., Dyck, M. J., & Ernst, D. (1991). Empirical status of Cognitive Theory of depression. Psychological Bulletin, 110(2), 215–236. https://doi.org/10.1037/0033-2909.110.2.215
Halbreich, U. (2003). The etiology, biology, and evolving pathology of premenstrual syndromes. Psychoneuroendocrinology, 28, 55–99. https://doi.org/10.1016/S0306-4530(03)00097-0
Hantsoo, L., & Epperson, C. N. (2015). Premenstrual dysphoric disorder: Epidemiology and treatment. Current Psychiatry Reports, 17(11), 87. https://doi.org/10.1007/s11920-015-0628-3
Kannisto, K. A., Korhonen, J., Adams, C. E., Koivunen, M. H., Vahlberg, T., & Välimäki, M. A. (2017). Factors associated with dropout during recruitment and follow-up periods of a health-based randomized controlled trial for mobile net to encourage treatment adherence for people with serious mental health problems. Journal of Medical Internet Research, 19(2), e46. https://doi.org/10.2196/jmir.6417
Kiesner, J., Mendle, J., Eisenlohr-Moul, T. A., & Pastore, M. (2016). Cyclical symptom change across the menstrual cycle: Attributional, affective, and physical symptoms. Clinical Psychological Science, 4(5), 882–894. https://doi.org/10.1177/2167702616635031
Kleinstäuber, M., Witthöft, M., & Hiller, W. (2012). Cognitive-behavioral and pharmacological interventions for premenstrual syndrome or premenstrual dysphoric disorder: A meta-analysis. Journal of Clinical Psychology in Medical Settings, 19(3), 308–319. https://doi.org/10.1007/s10880-012-9299-y
McIntosh, C. N., & Fischer, D. G. (2000). Beck’s cognitive triad: One versus three factors. Canadian Journal of Behavioural Science/revue Canadienne Des Sciences Du Comportement, 32(3), 153–157. https://doi.org/10.1037/h0087110
Nolen-Hoeksema, S., Wisco, B. E., & Lyubomirsky, S. (2008). Rethinking rumination. Perspectives on Psychological Science, 3(5), 400–424. https://doi.org/10.1111/j.1745-6924.2008.00088.x
Pope, C. J., Oinonen, K., Mazmanian, D., & Stone, S. (2017). The hormonal sensitivity hypothesis: A review and new findings. Medical Hypotheses, 102, 69–77. https://doi.org/10.1016/j.mehy.2017.03.012
Radloff, L. S. (1977). The CES-D scale: A self report depression scale for research in the general population. Applied Psychological Measurement, 1, 385–401. https://doi.org/10.1177/014662167700100306
Riskind, J. H., & Alloy, L. B. (2006). Cognitive vulnerability to emotional disorders: Theory and research design/methodology. In L. B. Alloy & J. H. Riskind (Eds.), Cognitive Vulnerability to Emotional Disorders (pp. 1–32). Lawrence Erlbaum Associates.
RStudio Team. (2015). RStudio: Integrated Development for R. [English; MacOs]. RStudio, Inc.
Segal, Z. V., & Ingram, R. E. (1994). Mood priming and construct activation in tests of cognitive vulnerability to unipolar depression. Clinical Psychology Review, 14(7), 663–695. https://doi.org/10.1016/0272-7358(94)90003-5
Śliwerski, A. (2019). Negative cognitive styles and depression as a risk factors for the occurrence of PMDD. OSF Registries. https://doi.org/10.17605/OSF.IO/4MZDB
Śliwerski, A., & Bielawska-Batorowicz, E. (2019). Negative cognitive styles as risk factors for the occurrence of PMS and PMDD. Journal of Reproductive and Infant Psychology, 37(3), 322–337. https://doi.org/10.1080/02646838.2018.1543943
Steiner, M., Macdougall, M., & Brown, E. (2003). The premenstrual symptoms screening tool (PSST) for clinicians. Archives of Women’s Mental Health, 6(3), 203–209. https://doi.org/10.1007/s00737-003-0018-4
Taylor, L., & Ingram, R. E. (1999). Cognitive reactivity and depressotypic information processing in children of depressed mothers. Journal of Abnormal Psychology, 108(2), 202–210. https://doi.org/10.1037/0021-843X.108.2.202
Wells, A., & Cartwright-Hatton, S. (2004). A short form of the metacognitions questionnaire: Properties of the MCQ-30. Behaviour Research and Therapy, 42(4), 385–396. https://doi.org/10.1016/S0005-7967(03)00147-5
Yonkers, K. A., & McCunn, K. L. (2007). Comorbidity of premenstrual syndrome and premenstrual dysphoric disorder with other psychiatric conditions. In P. M. S. O’Brien, A. J. Rapkin, & P. J. Schmidt (Eds.), The Premenstrual Syndromes: PMS and PMDD (pp. 49–54). Informa UK Ltd.
Funding
This research was funded by Narodowe Centrum Nauki, grant number 2017/01/X/HS6/01890.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
This study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the University of Łódź (protocol code 3/KBBN-UŁ/I/2018; 9 April 2018).
Informed Consent
All participants provided written informed consent for participation, use of the collected data, and publication.
Conflicts of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Śliwerski, A., Koszałkowska, K., Mrowicka, A. et al. Differences in Cognitive Triad, Biased Information Processing, and Metacognitive Beliefs Between Women with Depression and Premenstrual Syndrome. J Cogn Ther 16, 26–39 (2023). https://doi.org/10.1007/s41811-022-00151-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41811-022-00151-z