Abstract
Purpose
The purpose of this review is to discuss the development of Wixela™ Inhub™, a generic equivalent of Advair Diskus®, a fixed-dose combination of fluticasone propionate/salmeterol powder for oral inhalation for patients with asthma whose symptoms are not controlled with inhaled corticosteroids alone and for those with chronic obstructive pulmonary disease (COPD) who are at a high risk for exacerbations.
Summary
We provide an overview of the Inhub device and the bioequivalence studies that have been conducted to date. Briefly, the in vitro performance, improvements in forced expiratory volume in 1 s, and the fluticasone propionate/salmeterol dose strengths for Wixela Inhub and Advair Diskus were comparable.
Conclusion
The bioequivalence demonstrated by the totality of clinical and in vitro data supports the use of Wixela Inhub and provides a treatment option for patients with asthma or COPD.
Plain Language Summary
The Wixela™ Inhub™ device has been developed as a generic equivalent of Advair Diskus®, and provides a combination treatment for patients with asthma whose symptoms are not controlled with inhaled corticosteroids alone and for those with chronic obstructive pulmonary disease (COPD) who are at a high risk for exacerbations. We provide information about the Inhub device and studies conducted to show how Inhub and Diskus are comparable products. Based on the similar results between the two devices, Inhub can be used as a treatment option for patients with asthma or COPD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This review discusses Wixela™ Inhub™, a generic equivalent of Advair Diskus®, a fixed-dose combination of fluticasone propionate/salmeterol powder for oral inhalation for patients with asthma and chronic obstructive pulmonary disease (COPD). |
Wixela Inhub gave in vitro performance comparable to Advair Diskus for all strengths and flow rates for both single actuation content and impactor-sized mass. |
Compared with matched placebo, Wixela Inhub and Advair Diskus both demonstrated statistically significant improvements for forced expiratory volume in 1 s (FEV1). |
Fluticasone propionate/salmeterol dose strengths for Wixela Inhub and Advair Diskus are comparable. |
The bioequivalence demonstrated supports the use of Wixela Inhub and provides a treatment option for patients with asthma or COPD. |
Digital Features
This article is published with digital features, including a summary slide and plain language summary, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13252046.
Introduction
Asthma and chronic obstructive pulmonary disease (COPD) are prevalent respiratory diseases with an inflammatory component, the exacerbations of which can lead to poor outcomes. Inhaled corticosteroids (ICS) and long-acting beta-agonists (LABAs) are often prescribed for patients with asthma or COPD, with the Advair Diskus®, containing fluticasone propionate (FP)/salmeterol powder for oral inhalation, providing a common maintenance treatment option for patients [1,2,3]. Wixela™ Inhub™ was recently approved as a generic equivalent to Advair Diskus for patients with asthma whose symptoms are not controlled with ICS alone and for those with COPD who are at a high risk for exacerbations [4]. As a generic equivalent to Advair Diskus, Wixela Inhub provides a treatment option for patients that has a substantially lower list price [5, 6].
The purpose of this review is to provide an overview of the Inhub device and the bioequivalence studies that have been conducted to date. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Asthma
Asthma is a heterogeneous disease, usually characterized by chronic inflammation of the airways [1]. Asthma affects up to 18% of the population in different countries, including nearly 25 million Americans (7.7%), with 7.5% of children and 7.7% of adults aged over 18 years affected [1, 7]. Asthma is ultimately defined by respiratory symptoms (e.g., shortness of breath, wheeze, cough, and chest tightness) that vary over time and intensity, along with variable expiratory airflow limitation [1].
Asthma has five main clinical phenotypes, including allergic asthma, nonallergic asthma, adult/late-onset asthma, asthma with persistent airflow limitation, and asthma with obesity [1]. Allergic asthma is associated with a past and/or family history of allergic disease (e.g., eczema, allergic rhinitis, or food/drug allergy). Patients with allergic asthma usually respond well to ICS treatment. For nonallergic asthma, patients generally have a diminished short-term response to ICS [1]. Adult/late-onset asthma is more common in women and tends to be nonallergic [1]. Patients with adult/late-onset asthma often require higher ICS doses or are refractory to corticosteroid treatment.
Long-term goals of asthma management are to achieve control of symptoms and maintain normal activity levels, and to minimize the risk for asthma-related death, exacerbations, persistent airflow limitation, and side effects [1]. Currently, for adults and adolescents with asthma, Global Initiative for Asthma recommendations are to receive ICS-containing controller treatment, either as needed (in mild asthma) or daily, to reduce the risk for serious exacerbations and to control symptoms. For patients with frequent, troublesome asthma symptoms, the initial recommended treatment includes low-dose ICS-LABA as maintenance and reliever therapy with ICS-formoterol, or as conventional maintenance treatment of ICS/LABA, with a short-acting beta-agonist used as needed [1].
For patients whose initial asthma presentation is with severely uncontrolled asthma or with an acute exacerbation, initial treatment is a short course of oral corticosteroids and starting regular controller treatment with high-dose ICS or medium-dose ICS-LABA [1]. ICS are the primary choice of maintenance therapy for asthma [1]. Studies have shown improved symptoms and reduced asthma-related morbidity and mortality in patients treated with ICS [8, 9]. However, many patients treated according to guideline recommendations have symptoms that are difficult to control and experience frequent exacerbations and persistent symptoms [9]. Many patients experience a lack of asthma control with ICS alone; therefore, maintenance treatment with ICS and LABA, either separately or as a fixed-dose formulation, is recommended [1]. Fixed-dose combination therapy has been shown to increase persistence and adherence, which may be a result of the decreased required number of medications and/or the number of daily doses [10].
Chronic Obstructive Pulmonary Disease
A common, preventable, and treatable disease, COPD is characterized by persistent respiratory symptoms and airflow limitation resulting from airway and/or alveolar abnormalities generally caused by significant exposure to noxious particles or gases [2]. The prevalence of COPD is higher in smokers and ex-smokers compared with nonsmokers, in those aged 40 years or older compared with those aged younger than 40 years, and in men compared with women [11]. The number of COPD cases in 2010 was estimated to be 384 million, with a global prevalence of 11.7% and approximately 3 million deaths worldwide each year [2, 12]. Of importance, the prevalence is expected to increase over the next 30 years, with an estimate of more than 4.5 million deaths each year due to COPD and related conditions by the year 2060 [13].
Exacerbations are defined as an acute worsening of respiratory symptoms that result in additional therapy, and can be classified as mild (treated with short-acting bronchodilators), moderate (treated with short-acting bronchodilators plus antibiotics and/or oral corticosteroids), or severe (requiring hospitalization or visits to the emergency department) [2]. In a longitudinal study of 1105 subjects, 48.7% experienced at least one acute exacerbation during 3 years of follow-up, demonstrating a high rate of COPD exacerbations that can lead to poor patient outcomes [14].
Goals of treatment are to minimize the negative impact of the current exacerbation and prevent the development of subsequent events [2]. The choice of inhaler device must be individually tailored to the patient, and depends on variables including access, cost, prescriber, and the patient’s ability and preference. It is essential to provide instruction and demonstrate proper inhalation technique upon prescribing a device. Inhaler technique and adherence to therapy should be assessed before deciding to modify the current therapeutic regimen [2].
Bronchodilators, including LABAs and long-acting muscarinic antagonists, are indicated for individuals with suboptimal airflow through the lungs, including patients with COPD and asthma [15]. Beta-2 agonists are one of the primary treatments based on targeting of smooth muscles in lung bronchioles. The addition of an ICS to a LABA contributes to reduced inflammation and proinflammatory agents that constrict airways [15]. Inhaled bronchodilators are recommended over oral bronchodilators [2]. To prevent exacerbations, bronchodilation is considered the initial pharmacological step, with the initiation of dual bronchodilation following worsening of symptoms or the occurrence of exacerbations [16].
Long-term ICS monotherapy is not recommended; however, long-term ICS treatment may be considered in association with LABAs for patients with a history of exacerbations despite appropriate treatment with LABAs and those with a peripheral eosinophil count > 300 [2]. An ICS combined with a LABA (e.g., FP/salmeterol in a dry powder inhaler) is more effective than either component alone in providing improved lung function and health status, as well as in reducing exacerbations in patients with moderate-to-very-severe COPD [2].
Wixela Inhub Development
Characteristics
Wixela Inhub is a handheld inhalation device that delivers FP/salmeterol in a dry powder formulation (Fig. 1) also containing lactose as an excipient. The device holds 60 pre-metered doses and includes a dose counter to indicate how many doses remain. The Inhub device was designed with a larger dose counter (twice the size of the Diskus inhaler) to improve readability. The Inhub device is operated by completing four key steps: open the mouthpiece, push down a lever, inhale, and close the mouthpiece. The usage of the Inhub inhaler is similar to the Diskus inhaler, with the main difference being that the Inhub is held vertically during operation [17], whereas the Diskus is held horizontally; therefore, a lever is pushed down on the (vertical) Inhub, whereas the lever is slid around the (horizontal) Diskus.
In Vitro Performance
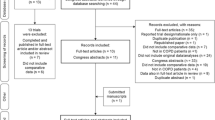
During in vitro testing, emitted dose (described as “single actuation content” in FDA product-specific guidance) [18] and impactor-sized mass were assessed at flow rates of 30 L min−1, 60 L min−1, and 90 L min−1 to determine in vitro equivalence between Wixela Inhub and Advair Diskus [19]. These flow rates are relevant to patients with asthma and COPD, as a flow-profiling study demonstrated that patients with asthma (adults and children) and COPD could all generate a flow rate of > 30 L min−1 through the Inhub device. Comparable performance was observed across the flow rates tested for both parameters, with a low degree of flow dependency observed for both products. When assessed statistically using the population bioequivalence test recommended in the FDA product-specific guidance [18], Wixela Inhub gave in vitro performance comparable to Advair Diskus for all strengths and flow rates for both single actuation content and impactor-sized mass, leading to the conclusion of in vitro bioequivalence for FP and salmeterol at all strengths [19]. Comparable aerodynamic particle size distribution (APSD) profiles were observed for the two products, with mass median aerodynamic diameter (MMAD) and geometric standard deviation (GSD) values for test and reference differing by ≤ 0.7 µm and ≤ 0.2 µm, respectively, across the 36 comparisons made in the in vitro studies [19].
The resistance of the Diskus and Inhub inhalers was measured in the course of the in vitro studies [19]. The resistance of Inhub at 0.034 kPa0.5 L min−1 was observed to be almost 30% higher than that of Diskus at 0.027 kPa0.5 L min−1, but this has no clinical consequence, and both inhalers are considered medium resistance. The resistance of Inhub was more consistent than that of Diskus, showing less than half the variability of Diskus when measured across batches. The flow rate at a 4-kPa pressure drop through the Diskus device ranged from 67 to 89 L min–1, whereas the Inhub device showed a much narrower flow-rate range, of 56–60 L min−1 [19].
The emitted dose and impactor-sized mass of Wixela Inhub and Advair Diskus were also shown to be comparable when tested at a fixed pressure drop of 4 kPa, reflecting the low flow dependency of performance in each product [19]. The mean flow rate for Inhub at 4 kPa was close to 60 L min−1 and the in vitro performance at 4 kPa was similar to that measured at 60 L min−1. For Diskus, the mean flow rate at 4 kPa was 75 L min−1. The in vitro performance was comparable to that measured at 60 L min−1 or 90 L min−1, with performance across this flow-rate range differing very little, as expected [19].
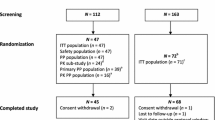
Local Therapeutic Equivalence Based on Clinical Endpoints
A multicenter study consisting of a 21- to 28-day single-blind, placebo run-in period followed by a 4-week placebo-controlled, double-blind, double-dummy treatment period was carried out to assess the local therapeutic equivalence of Wixela Inhub (test product) and Advair Diskus (reference product) using spirometry [20]. Patients were aged ≥ 18 years with an established diagnosis of asthma. A total of 1127 patients received Wixela or Advair at 100/50 μg or placebo in a 5:5:1 ratio. Spirometry assessments were conducted at screening; at run-in; at pre- and 0.5, 1, 2, 3, 4, 6, 8, 10, and 12 h post-dose on day 1 of treatment; prior to dosing on day 15; and on day 29 [20].
Compared with matched placebo, the test and reference products both demonstrated statistically significant improvements for forced expiratory volume in 1 s (FEV1), measured over the 12-h post-dose period on day-1 and day-29 trough FEV1 (Table 1) [20]. The geometric mean ratios of test/reference and corresponding 90% confidence intervals (CIs) for day-1 FEV1 area under the effect curve over 12 h and day-29 change from baseline in trough FEV1 were between 0.80 and 1.25 for both endpoints, demonstrating bioequivalence. A similar incidence of adverse events (AEs) was reported across the three treatment groups (Table 2). Asthma-related AEs and discontinuations were higher in the placebo group compared with both active treatment groups. No clinically significant changes to laboratory safety tests, vital signs, or electrocardiograms were reported [20].
Pharmacokinetic Bioequivalence Studies
Three studies examined the different dose strengths of FP/salmeterol Wixela Inhub and Advair Diskus (100/50 μg, 250/50 μg, and 500/50 μg), with one strength examined in each study [21].
Each study was an open-label, randomized, two-way crossover study at a single clinical center. In each study, 66 healthy male and female subjects were given single orally inhaled doses of Wixela (test product) and Advair (reference product), one per study period, with a minimum 7-day washout between them. Exclusion criteria included the use of any prescription or nonprescription drugs within 7 days of the study start, abnormal lung function (< 80% of predicted FEV1), or status as a current smoker or ex-smoker who had quit for < 6 months, and/or had a smoking history of ≥ 10 pack-years [21].
Each dose strength was administered as three inhalations, resulting in total FP/salmeterol doses of 300/150 μg (study 1), 750/150 μg (study 2), and 1500/150 μg (study 3) [20]. This was done to ensure FP and salmeterol were both detectable for at least three half-lives for each analyte after dosing [21]. The use of three inhalations was expected to reduce variability and was considered the “minimum number of inhalations that is sufficient to characterize a [pharmacokinetic] profile by using a sensitive analytical method,” in accordance with FDA guidance [18, 21]. Plasma samples were obtained prior to dosing and at 2, 5, 10, 15, 20, 30, and 45 min and 1, 1.5, 2, 3, 4, 6, 8, 12, 24, 36, and 48 h post-dose [21]. The early time points after dosing ensured the rapid absorption of salmeterol could be adequately characterized. Drug concentrations were analyzed using validated high-performance liquid chromatography tandem mass spectrometry [21].
In each study, plasma FP concentration versus time data for Wixela and Advair were comparable (Table 3) [21]. FP was rapidly absorbed, with time to maximum plasma concentration (Tmax) values ranging from 0.75 h (100/50 µg strength) to 1.5 h (250/50 µg strength). Across the studies, mean maximum plasma concentration (Cmax) values varied with dose, as would be expected given that the FP dose increases with strength and ranged from 109 pg/mL (100/50 µg strength) to 290 pg/mL (500/50 µg strength) [21].
Salmeterol concentration versus time data for Wixela and Advair were also comparable (Table 3); salmeterol was very rapidly absorbed (Tmax, 5 min) in all studies [21]. Mean Cmax, area under the concentration–time curve from time 0 to the last measurable concentration (AUC0–t), and terminal elimination half-life values were also consistent across studies, as would be expected, considering the same dose of salmeterol is contained in all three strengths of the products [21].
For each of the FP/salmeterol dose strengths, the geometric mean test/reference ratios and 90% CIs were between 0.80 and 1.25 for both the FP and salmeterol AUC0–t and Cmax, indicating Wixela and Advair were bioequivalent for both FP and salmeterol (Table 4) [21].
No clinically significant changes occurred in electrocardiograms, vital signs (blood pressure/pulse), cardiac telemetry, or laboratory safety tests [21]. AEs were mild and were reported in similar frequencies among treatment groups in all studies. The most commonly reported AE was headache [21].
A study of 110 subjects demonstrated usability success of the Wixela Inhub device, with 100 subjects holding the inhaler properly; of the ten who did not, nine achieved successful peak inhalation flow rates and total inhaled volume [22]. In a second study, 111 subjects with asthma or COPD, ranging from pediatric to elderly, used the Inhub inhaler for approximately 3 weeks in the outpatient setting. In vitro testing demonstrated preserved pharmaceutical performance of FP and salmeterol, illustrating the robustness of the Inhub inhaler [22].
Conclusions
Wixela Inhub represents a generic equivalent FP/salmeterol treatment option to Advair Diskus for patients with asthma whose symptoms are not controlled with ICS alone and for patients with COPD who are at a high risk for exacerbations. The package of clinical and in vitro data described met the requirements of FDA guidance, and therefore supports the use of Wixela Inhub in patients with both asthma and COPD, providing a treatment option for patients with either indication.
References
Global Initiative for Asthma. Global strategy for asthma management and prevention. https://ginasthma.org/wp-content/uploads/2020/04/GINA-2020-full-report_-final-_wms.pdf (2020). Accessed 12 June 2020.
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2020 report. https://goldcopd.org/wp-content/uploads/2019/11/GOLD-2020-REPORT-ver1.1wms.pdf (2020). Accessed 12 June 2020.
Allan R, Haughie S, Ahrens R, et al. A dose-response study examining the use of methacholine challenge to demonstrate local therapeutic equivalence of the salmeterol component of generic inhaled fluticasone propionate/salmeterol combination products. J Aerosol Med Pulm Drug Deliv. 2019;32:352–63.
Mylan announces FDA approval of Wixela™ Inhub™ (fluticasone propionate and salmeterol inhalation powder, USP), first generic of Advair Diskus® (fluticasone propionate and salmeterol inhalation powder. Hertfordshire, England and Pittsburgh, PA. 31 Jan 2019.
Advair Diskus prices, coupons and patient assistance programs. Updated November 2, 2020. https://www.drugs.com/price-guide/advair-diskus. Accessed 11 Nov 2020.
Wixela Inhub prices, coupons and patient assistance programs. Updated November 2, 2020. https://www.drugs.com/price-guide/wixela-inhub. Accessed 11 Nov 2020.
Centers for Disease Control and Prevention. Most recent national asthma data (March 24, 2020). http://www.cdc.gov/asthma/most_recent_national_asthma_data.htm. Accessed 2 July 2020.
Barnes CB, Ulrik CS. Asthma and adherence to inhaled corticosteroids: current status and future perspectives. Respir Care. 2015;60:455–68.
Barnes PJ. Efficacy of inhaled corticosteroids in asthma. J Allergy Clin Immunol. 1998;102(4 Pt 1):531–8.
Marceau C, Lemière C, Berbiche D, et al. Persistence, adherence, and effectiveness of combination therapy among adult patients with asthma. J Allergy Clin Immunol. 2006;118:574–81.
Halbert RJ, Natoli JL, Gano A, et al. Global burden of COPD: systematic review and meta-analysis. Eur Respir J. 2006;28:523–32.
GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age–sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–71.
World Health Organization. Global summary projections. http://www.who.int/healthinfo/global_burden_disease/projections/en (2020). Accessed 8 July 2020.
Han MK, Quibrera PM, Carretta EE, et al. Frequency of exacerbations in with COPD: an analysis of the SPIROMICS cohort. Lancet Respir Med. 2017;5:619–26.
Almadhoun K, Sharma S. Bronchodilators. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020.
Miravitlles M, Anzueto A, Jardim JR. Optimizing bronchodilation in the prevention of COPD exacerbations. Respir Res. 2017;18:125.
Advair Diskus [prescribing information]. Research Triangle Park, NC: GlaxoSmithKline. http://www.gsksource.com/pharma/content/dam/GlaxoSmithKline/US/en/Prescribing_Information/Advair_Diskus/pdf/ADVAIR-DISKUS-PI-PIL-IFU.PDF (2019). Accessed 4 Nov 2020.
Draft guidance on fluticasone propionate; salmeterol xinafoate (powder/inhalation). http://www.accessdata.fda.gov/drugsatfda_docs/psg/Fluticasone%20Proprionate_Salmeterol%20Xinafoate_21077_RC09-13.pdf (2013). Accessed 28 June 2019.
Cooper A, Parker J, Berry M, et al. Wixela Inhub: dosing performance in vitro and inhaled flow rates in healthy subjects and patients compared with Advair Diskus. J Aerosol Med Pulm Drug Deliv. 2020. https://doi.org/10.1089/jamp.2019.1584 (Published online 19 May 2020).
Ng D, Kerwin EM, White MV, et al. Clinical bioequivalence of Wixela Inhub and Advair Diskus in adults with asthma. J Aerosol Med Pulm Drug Deliv. 2020;33:99–107.
Haughie S, Allan R, Wood N, et al. Equivalent systemic exposure to fluticasone propionate/salmeterol following single inhaled doses from Advair Diskus and Wixela Inhub: results of three pharmacokinetic bioequivalence studies. J Aerosol Med Pulm Drug Deliv. 2020;33:34–42.
Allan R, Canham K, Wallace R, Singh D, Ward J, Cooper A, Newcomb C. Usability and robustness of the Wixela Inhub dry powder inhaler. J Aerosol Med Pulm Drug Deliv. 2020. https://doi.org/10.1089/jamp.2020.1603 (Published online 31 Aug 2020).
Acknowledgements
We would like to thank the participants in these studies.
Funding
No funding or sponsorship was received for this study or publication of this article. The journal’s Rapid Service Fee was provided by Mylan Inc.
Medical Writing and Other Assistance
Technical, editorial, and medical writing assistance were provided under the direction of the authors by Erin Burns, PhD, and Strategix, an affiliate of The Lynx Group LLC. Funding for this assistance was provided by Mylan Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
James F. Donohue reports consultant fees from AZ, Mylan, Teva, BI, GSK and Theravance, outside the submitted work; Douglas S. Burgoyne reports he is on the advisory boards for Celgene, RB, and Sunovion; Jonathan K. Ward reports he is an employee and stockholder of Mylan Inc., during the conduct of the study; Richard Allan reports he is an employee of Mylan and has stock ownership in Mylan, Inc.; Arkady Koltun reports he is an employee of Mylan Inc.; Andrew Cooper reports he is an employee of Mylan Inc. Jonathan K. Ward, Richard Allan, Arkady Koltun, and Andrew Cooper are now employees of Viatris (a result of the merger between Mylan and Upjohn, a legacy division of Pfizer).
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Donohue, J.F., Burgoyne, D.S., Ward, J.K. et al. Wixela Inhub: A Generic Equivalent Treatment Option for Patients with Asthma or COPD. Pulm Ther 7, 47–57 (2021). https://doi.org/10.1007/s41030-020-00142-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41030-020-00142-5