Abstract
Background and Objective
Metered-dose inhalers require patients to coordinate inhalation with actuation. The present albuterol multi-dose dry-powder inhaler (mDPI) does not require patients to coordinate inspiration with actuation, thereby simplifying delivery of albuterol to the lungs. The aim of the present study was to compare the efficacy, pharmacokinetics, pharmacodynamics, extrapulmonary pharmacodynamics, and safety of albuterol (salbuterol) delivered via a ProAir® hydrofluoroalkane (HFA) metered-dose inhaler and an mDPI.
Methods
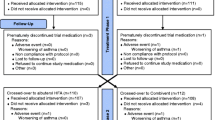
Two double-blind, randomized, double-dummy, crossover, multicenter, placebo-controlled studies in persistent asthma patients were conducted. Study 1: 47 adult patients were treated with cumulative doses of albuterol mDPI or ProAir HFA (90 µg/inhalation; 1 + 1 + 2 + 4 + 8 inhalations) or placebo. Study 2: 71 patients aged ≥12 years were randomly assigned to receive 90 or 180 μg of albuterol mDPI or ProAir HFA, or placebo. Primary efficacy endpoints were baseline-adjusted forced expiratory volume in 1 s (FEV1) at 30 min (30-min FEV1) after each cumulative dose (Study 1) and FEV1 area under the effect curve over 6 h (FEV1 AUEC0–6) after dosing (Study 2).
Results
Study 1: differences, with corresponding 90 % confidence intervals, between albuterol mDPI and ProAir HFA in FEV1 after each cumulative dose and in FEV1 AUEC0–6 after the final dose were within pre-established equivalence limits. The difference in FEV1 at high vs. low doses was significant for both active treatments (p < 0.0001). Active treatments were similar in systemic exposure, extrapulmonary pharmacodynamics, and safety. Study 2: mean FEV1 AUEC0–6 was significantly greater than for placebo for both doses of albuterol mDPI and ProAir HFA (p < 0.0001). Albuterol mDPI was comparable to ProAir HFA at 90 and 180 µg. Both study treatments were generally well tolerated.
Conclusion
The bronchodilatory efficacy and pharmacokinetic/pharmacodynamic profiles of albuterol mDPI and ProAir HFA are comparable, with a safety profile consistent with that of inhaled albuterol.




Similar content being viewed by others
References
Centers for Disease Control and Prevention. FastStats: asthma. Available at: http://www.cdc.gov/nchs/fastats/asthma.htm. Accessed 13 Aug 2015.
Fuhlbrigge AL, Adams RJ, Guilbert TW, et al. The burden of asthma in the United States: level and distribution are dependent on interpretation of the national asthma education and prevention program guidelines. Am J Respir Crit Care Med. 2002;166:1044–9.
Expert Panel Report 3 (EPR-3). Guidelines for the diagnosis and management of asthma: summary report 2007. J Allergy Clin Immunol. 2007;120:S94–138.
Proair HFA [package insert]. Horsham, PA: Teva Respiratory, LLC; 2012.
Bronsky E, Bucholtz GA, Busse WW, et al. Comparison of inhaled albuterol powder and aerosol in asthma. J Allergy Clin Immunol. 1987;79:741–7.
Kemp JP, Furukawa CT, Bronsky EA, et al. Albuterol treatment for children with asthma: a comparison of inhaled powder and aerosol. J Allergy Clin Immunol. 1989;83:697–702.
Dolovich MB, Ahrens RC, Hess DR, et al. Device selection and outcomes of aerosol therapy: evidence-based guidelines: American College of Chest Physicians/American College of Asthma, Allergy, and Immunology. Chest. 2005;127:335–71.
Given J, Taveras H, Iverson H, et al. Prospective, open-label assessment of albuterol sulfate hydrofluoroalkane metered-dose inhaler with new integrated dose counter. Allergy Asthma Proc. 2013;34:42–51.
Cochrane MG, Bala MV, Downs KE, et al. Inhaled corticosteroids for asthma therapy: patient compliance, devices, and inhalation technique. Chest. 2000;117:542–50.
Crompton GK, Barnes PJ, Broeders M, et al. The need to improve inhalation technique in Europe: a report from the Aerosol Drug Management Improvement Team. Respir Med. 2006;100:1479–94.
Lindgren S, Bake B, Larsson S. Clinical consequences of inadequate inhalation technique in asthma therapy. Eur J Respir Dis. 1987;70:93–8.
Chrystyn H, Price D. Not all asthma inhalers are the same: factors to consider when prescribing an inhaler. Prim Care Respir J. 2009;18:243–9.
Giraud V, Roche N. Misuse of corticosteroid metered-dose inhaler is associated with decreased asthma stability. Eur Respir J. 2002;19:246–51.
Scichilone N, Benfante A, Bocchino M, et al. Which factors affect the choice of the inhaler in chronic obstructive respiratory diseases? Pulm Pharmacol Ther. 2015;31:63–7.
Demoly P, Hagedoorn P, de Boer AH, et al. The clinical relevance of dry powder inhaler performance for drug delivery. Respir Med. 2014;108:1195–203.
Expert Panel Report 3 (EPR3). Guidelines for the diagnosis and management of asthma. Bethesda, MD: National Heart, Lung, and Blood Institute, US Department of Health and Human Services. 2007. Available at: http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm. Accessed on 19 Aug 2015.
Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–87.
Newman SP, Weisz AW, Talaee N, et al. Improvement of drug delivery with a breath actuated pressurised aerosol for patients with poor inhaler technique. Thorax. 1991;46:712–6.
Price DB, Pearce L, Powell SR, et al. Handling and acceptability of the Easi-Breathe device compared with a conventional metered dose inhaler by patients and practice nurses. Int J Clin Pract. 1999;53:31–6.
Acknowledgments
The authors acknowledge and thank the investigators from Study 1 and Study 2 and their respective teams for their valuable contributions during the conduct of this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was sponsored by Teva Branded Pharmaceutical Products R&D, Inc. Medical writing and editorial assistance during the preparation of this manuscript was provided by ApotheCom, with funding provided by Teva.
Conflicts of interest
Dr. Kerwin has served on advisory boards for Amphastar, AstraZeneca (Pearl), Mylan, Novartis, Sunovion, and Theravance; participated on speaker panels for Amphastar, AstraZeneca (Pearl), Boehringer Ingelheim, Forest, Mylan, Novartis, Sunovion, and Theravance; and has received travel reimbursement for presentations at meetings from Forest, Novartis, and Teva. He has conducted multicenter clinical research trials for approximately 40 pharmaceutical companies. Dr. Miller receives research funding from Teva and served as principal investigator for Teva through Northeast Medical Research Associates. Drs. Iverson, Shah, Taveras, and Wayne are employed by Teva Branded Pharmaceutical Products R&D and may hold stock or stock options in Teva. Dr. Lepore was employed by Teva Branded Pharmaceutical Products R&D at the time the study was conducted and holds stock or stock options in Lupin Inc.
Ethical approval
All procedures in both studies were conducted in accordance with the ethical principles based on the 1964 Declaration of Helsinki (and its amendments) and Good Clinical Practice. Both studies were approved by the institutional review board at each study site.
Informed consent
All patients from both studies provided written informed consent before screening.
Rights and permissions
About this article
Cite this article
Kerwin, E.M., Taveras, H., Iverson, H. et al. Pharmacokinetics, Pharmacodynamics, Efficacy, and Safety of Albuterol (Salbuterol) Multi-dose Dry-Powder Inhaler and ProAir® Hydrofluoroalkane for the Treatment of Persistent Asthma: Results of Two Randomized Double-Blind Studies. Clin Drug Investig 36, 55–65 (2016). https://doi.org/10.1007/s40261-015-0346-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-015-0346-y