Abstract
Introduction
Osteoarthritis (OA) is a degenerative joint disease that impacts 3.3–3.6% of population globally with significant health and societal impact. The current study assessed the disease burden, treatment patterns, and healthcare resource utilisation (HCRU) and costs in patients with OA and subgroups of hip and/or knee OA, in Dubai, United Arab Emirates (UAE).
Methodology
This retrospective longitudinal case–control study collected OA-related data from January 1, 2014 to May 31, 2020 from the Dubai Real-World Claims Database (DRWD). Adults aged at least 18 years old with OA diagnosis and at least two claims and continuous enrolment during the study period were included in the study. The patients with OA were 1:1 matched with individuals without OA. The patients with OA were divided into four cohorts on the basis of an a priori algorithm: OA of the hip and/or knee (cohort 1) and (difficult-to-treat) subsets of patients with moderate-to-severe OA of the hip and/or knee (cohort 2), inadequate response or inability to tolerate at least three pain-related medications (cohort 3), and contraindications to nonsteroidal anti-inflammatory drugs (NSAIDs) (cohort 4).
Results
Disease burden of OA in Dubai and HCRU and treatment costs in patients with OA were evaluated from January 1, 2014 to May 31, 2021. Patients were compared with matched controls in 1:1 ratio. The overall cohort comprised 11,651 patients with a median age of 48 years and predominantly male population (61.6%). HCRU was calculated for each cohort and it was highest (United States dollar [USD] 11,354.39) in cohort 4 (patients with contraindication to NSAIDS); in cohort 3 (inability to respond to at least three pain-related medications), USD 495.30 and USD 765.14 were spent on medication and procedures, respectively. Highest cost burden was seen in cohort 4, USD 3120.49 on consumables and USD 228.18 on services.
Conclusion
Osteoarthritis imposes a substantial healthcare and economic burden in the UAE. The study findings elucidate the unmet need among patients with difficult-to-treat OA and inform development of new therapeutics to alleviate their burden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
OA is a chronic degenerative disease with significant impact on society and healthcare systems. There is a paucity of real-world data on burden and unmet needs due to OA in the UAE and the Middle East region. |
The current study assessed the disease burden, treatment patterns, and HCRU and costs in patients with OA and subgroups of hip and/or knee OA, in Dubai, UAE. |
HCRU was calculated for each cohort and it was highest (USD 11,354.39) in cohort 4 (patients with contraindication to NSAIDS); in cohort 3 (inability to respond to at least three pain-related medications), USD 495.30 and USD 765.14 were spent on medication and procedures, respectively. Highest cost burden was seen in cohort 4, USD 3120.49 on consumables and USD 228.18 on services. |
The findings would help understand the levels of unmet need among those with more severe forms and/or those for whom currently available pharmacological therapies may not provide adequate levels of analgesia and inform development of new therapeutics to alleviate their burden |
Introduction
Osteoarthritis (OA) is a chronic degenerative joint disease characterised by inflammation and major structural damage to one or more of the affected joints [1]. It is a highly prevalent disease and a leading cause of disability, with a significant health and societal impact [2, 3]. The course of OA disease differs among affected individuals in terms of number of joints involved (single or multiple) and also severity of symptoms [1]. Prevalence of OA is more common in women compared to men and increases with age [4,5,6].
A greater proportion of the burden of OA is contributed by OA of the hip and knee, often leading to significant disability requiring surgical intervention, particularly joint replacement surgeries [5, 7]. According to estimates, OA of the hip is ranked as the 11th leading cause for global disability, and knee OA as the 38th highest contributor for disability-adjusted life years (DALYs) [5]. Even in terms of life expectancy, OA inflicts a huge burden on the affected population. Evidence suggests that mortality is higher in patients with OA compared to the general population [8].
High prevalence of OA and associated morbidity and treatment expenses contribute to the large economic burden in terms of direct costs (hospital stay, elective orthopaedic surgery, medications, physician visits, other health professional visits, diagnostic procedures) and indirect costs incurred as a result of time lost from work, disease-related loss in productivity at work, early retirement due to disease) to both affected individuals and the healthcare sector [2].
Despite recent breakthroughs in understanding of disease pathogenesis, treatment of OA remains a major challenge for clinicians [9]. The current available treatment options in the management of patients with OA include non-pharmacological and pharmacological strategies, which predominantly focus on relieving symptoms such as pain and stiffness and minimising functional loss [9, 10]. Pharmacotherapeutic approaches for patients with OA include analgesics (topical and oral NSAIDs, opioids, and paracetamol), intra-articular (IA) corticosteroids and hyaluronic acid (HA). However, the pharmacological agents have certain limitations in terms of limited efficacy or increased adverse event profile in long-term or chronic use. With such limited therapeutic options, joint replacement with an artificial prosthesis remains the only option in patients with symptom-refractory disease.
Furthermore, OA, being a heterogeneous disease, is characterised by distinct clinical features, genetic characteristics, and treatment responses; therefore, stratification of the OA population into subsets and tailoring of treatments by individual subsets is required [11].
Available evidence-based treatments are effective in patients with OA with mild symptoms, and also in elderly patients with advanced radiographic disease with severe pain for whom joint replacement remains an optimal option. Therefore, the unmet need for novel pharmacological agents arises in patients with OA whose symptoms have not responded adequately to existing pharmacological agents, or in whom these are contraindicated or not tolerated: younger patients with moderate-to-severe symptoms, and elderly patients with moderate radiographic disease only, or those who do not wish for surgery [12].
Therefore, an urgent need was felt to address this knowledge gap pertaining to disease burden, treatment patterns and healthcare resource utilisation (HCRU) of OA and levels of unmet need among selected OA subsets of patients. The aim of the current analyses was to evaluate the patient characteristics, disease prevalence, economic burden, and pharmacological treatment patterns in OA-diagnosed patients and selected difficult-to-treat subpopulations (patients with hip and/or knee OA, patients with moderate-to-severe hip and/or knee OA, patients with inadequate response or inability to tolerate at least three pain medications, patients with contraindications to NSAIDs) of OA in Dubai, UAE.
Methods
Study Design
This was a longitudinal case–control retrospective study. The data analyses covered the study period between January 1, 2014 and May 31, 2020. The index date for each patient was defined as the date on which the first diagnosis for OA (case group) or non-OA (control group) was identified during the patient identification period or the index period (between January 1, 2015 and May 31, 2019) within the database. The extracted data for the eligible population spanned two periods with respect to index date: pre-index or baseline period (12 months prior to the index date) and post-index or follow-up period (12 months following the index date). Incidental patients were excluded using continuous enrolment as surrogate, i.e. patients were required to be continuously eligible with at least one claim for any service for a period of two consecutive 6 months in pre-index period and two consecutive 6 months in post-index period. The intention of continuous enrolment was to exclude incidental patients or patients with only one claim during the index time period.
Data Source
The DRWD e-claims database is the largest claims database of private insurers in the Emirates of Dubai, and contains information pertaining to patients’ demographics, diagnoses, procedures (medical, surgical and diagnostic), prescriptions, and other related services [13].
All local, legal and regulatory guidelines were followed with no involvement of institutional review board (IRB) approval or informed consent form (ICF) signing, as this study used anonymised patient-level data.
Study Population
The International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes (M15-M19) were used to differentiate case and control groups (1:1 matching) from the database. The control group was selected on the basis of 1:1 matching with the OA case group for parameters of age, gender and comorbidities. The OA case group was matched with the OA control group for eight age categories, namely 18–24 years, 25–34 years, 35–44 years, 45–54 years, 55–64 years, 65–74 years, 75–84 years and 85+ years, and 41 comorbidities. Comorbidities considered for matching included other types of arthritis, pain-related conditions, pain-related neuropsychiatric conditions and other comorbidities (congestive heart failure, peripheral vascular disease, cerebrovascular disease, coronary heart disease, hypertension, chronic respiratory disease, rheumatologic disease, osteoporosis, peptic ulcer disease, mild liver disease, hemiplegia, diabetes without complication, diabetes with complications, renal disease, metastatic solid tumour, any malignancy, moderate-to-severe liver disease, fractures, obesity, human immunovirus deficiency disease, myocardial infarction, psychosis, dementia, constipation, gastro-oesophageal reflux disease, gastrointestinal bleeding, nausea) (Table 2).The ICD-10-CM codes are provided in the supplementary material (Table S1).
Patients at least 18 years of age (latest available age in DRWD at the time of extraction of data) with OA diagnosis, at least two claims for anytime and continuous enrolment during the study period (between January 1, 2014 and May 31, 2020) were included in this study. Other inclusion criteria included patients with first OA diagnosis and at least one pharmacy claim during the identification period. Patients with missing claims and those with ICD-10-CM codes corresponding to primary diagnosis of malignant cancer (C76–C80) were excluded from the study.
Case Selection Algorithms
A priori case selection algorithms [14] based on combinations of ICD-10 codes were used to identify four cohorts of patients with OA stratified as OA of the hip and/or knee (cohort 1) followed by its subsets of patients with moderate-to-severe OA of the hip and/or knee (cohort 2), inadequate response or inability to tolerate at least three pain-related medications (cohort 3) and contraindications to NSAIDs (cohort 4). These subgroups were not mutually exclusive (there was an overlap of 1324 patients between cohorts 2 and 3; 287 patients between cohorts 2 and 4 and 129 patients between cohorts 3 and 4). The algorithms are provided in the supplementary material (Table S2) and adapted on the basis of a targeted review of published literature, relevant treatment guidelines and professional organizations. The control group was selected on the basis of 1:1 matching with the OA case group for parameters of age, gender and comorbidities.
Baseline Variables and Outcomes
For the current analyses the following variables and outcomes were extracted from the DRWD:
-
Demographics and baseline clinical characteristics data for overall OA cohort was extracted from the pre-index period claim records. Assessment for presence of any pre-existing comorbidities was done from the pre-index period records, through identification of clinically relevant disease conditions using the ICD-10 CM codes. The comorbidities were quantified using the Quan–Charlson comorbidity index (CCI) score. The CCI is the most commonly used comorbidity index developed to predict 1-year mortality in patients with comorbid diseases. Each condition is assigned a score depending on the mortality risk associated with each comorbid condition, and consequently scores are summed to provide a total score to predict mortality. Quan et al. developed ICD-10 and ICD-9 comorbidity coding algorithms to define and estimate comorbidity prevalence in administrative data [15].
-
Data pertaining to consultation-based incident and prevalent cases of OA in the overall population was analysed during the 12-month pre-index period.
-
Treatment patterns in the overall cohort were determined on the basis of prescription pattern of pharmacological treatment. The prescription pattern was assessed by specialty and switching behaviour during the 12-month post-index period. Data pertaining to the time to index treatment from first diagnosis of OA and time to first surgery (hip and/or knee) from first diagnosis of OA and patient receiving hip and/or knee joint replacement surgery were analysed through the study period.
-
All-cause HCRU and OA-specific HCRU in the overall cohort were determined on the basis of visit type (number and types of claims [inpatient, outpatient and emergency claims] for healthcare visits) and activity type (number and types of claims [medications, procedures, consumables and services]) and associated healthcare costs (all-cause and OA-specific) for both visit type and activity-based claims and were analysed during the 12-month post-index period.
-
Baseline characteristics, comorbidities and HCRU claims and costs (all-cause) were compared and analysed between the case group (patients with OA) and control group (patients without) during the 12-month post-index period.
-
For the subset of four cohorts of OA hip and/or knee, all the aforementioned outcomes pertaining to demographics, clinical characteristics, comorbidities, treatment patterns and HCRU-related claims and costs were analysed. However, the matched cohort (non-OA) level analyses were not performed for the subset of OA cohorts.
Statistical Analysis
Descriptive statistics was used to analyse the study variables: patient characteristics and comorbidities in patients with OA and hip and/or knee OA during the pre-index period, consultation-based incident and prevalent OA and hip and/or knee OA during the study period, treatment patterns in patients with OA and hip and/or knee OA during the post-index period, all-cause and OA-specific HCRU and costs during post-index period. Continuous variables were calculated using mean, median, standard deviation, minimum and maximum, as appropriate. Categorical variables were calculated by frequency and percentages (n, %).
Results
Out of 361,806 ‘potentially eligible’ patients (diagnosed with OA anytime during the study period) identified from the database, 11,651 (3.22%) patients met all the inclusion criteria and none of the exclusion criteria and were included in the study for analyses.
Baseline Characteristics and Comorbidities of Patients with Osteoarthritis
The eligible patients in the overall OA cohort had a median age of 48.0 (range 18.0–98.0) years and the majority of them were male (61.6%). Nearly 94.1% of patients belonged to the 18–64 year age group. In the overall OA cohort 54.1% (n = 6301) of patients had a CCI score of 1 or more (higher CCI score indicates higher severity of condition and increased risk of mortality). The most common comorbidity in the overall OA cohort was other specified pain (68.8%). Other comorbidities in order of frequency included gastro-oesophageal reflux (45.5%), hypertension (35.8%), gastrointestinal (GI) bleeding (29.1%), diabetes without complications (24.1%), diabetes with complications (19.5%), chronic respiratory disease (19.7%), mild liver disease (13.4%) and coronary heart disease (9.0%) among others (> 10%). Details of key demographic and clinical characteristics of the overall OA cohort are summarised in Table 1.
The median age of patients with OA in the case group was 47.0 years and that in the matched control group was 46.5 years (range 18.0–80.0) years, and the majority of them were male (63.8%, both groups). The frequency of most of the baseline comorbidities was higher in the OA group compared to the control group (Table 2).
Incidence and Prevalence of Osteoarthritis
During the study period (January 1, 2014 to May 31, 2020), the incidence and prevalence of OA cases and patients with OA of the hip and/or knee were estimated using data available in the e-claims database. Overall, the average incidence of OA was 1.7% and average prevalence of OA was 2% during the study period, according to e-claims data (Fig. 1a). Average incidence of OA of the hip and/or knee was 1.2% and prevalence was 1.4% (Fig. 1b).
A marginal variation in incidence rates of OA cases and OA of the hip and/or knee cases was noted in Emiratis (local nationals) and expatriates or expats (foreign nationals) (Figs. 2 and 3, respectively). A similar trend in prevalence rates of OA and OA of the hip and/or knee cases was noted in locals and expats (see Table S3 in the supplementary material for details).
Identification of Selected Difficult-to-Treat Subgroups of Osteoarthritis
Of 11,651 patients with OA, records of 8879 (76.2%) patients with OA of the hip and/or knee were considered eligible for the subgroup cohort analysis; 2772 (23.8%) with diagnosis of OA of sites other than the hip and/or knee and other non-OA conditions were not eligible for subgroup cohort analysis.
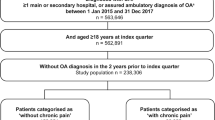
Specifically, 8879 (76.2%) patients with OA of the hip and/or knee were included for cohort 1 analysis; 3728 (32.0%) patients with moderate-to-severe hip and/or knee OA were included for cohort 2 analysis; 1612 (13.8%) patients with OA of the hip and/or knee with inadequate response or inability to tolerate at least three pain-related medications were included for cohort 3 analysis and 597 (5.1%) patients with OA of the hip and/or knee with NSAIDs contraindications were included for cohort 4 analysis (Fig. 4). Only 8556 patients out of 11,651 could be matched with a patient without OA in the control group.
Burden of baseline comorbid conditions was comparatively higher in cohort 4. Gout (including pseudogout) was reported in 11.6% patients in cohort 4, as compared to 9.9% in cohort 1, 10.9% in cohort 2, and 10% in cohort 3. Comorbid rheumatoid arthritis was noted in 6.4% patients in cohort 4 as compared to 4.9% in cohort 1, 5.7% in cohort 2, and 5.3% in cohort 3. Pain-related neuropsychiatric conditions (depression, anxiety, sleep disorders and drug or alcohol abuse) were reported in 4.8% of patients in cohort 4 as compared to 2.9% in cohort 1, 3.7% in cohort 2, and 2.4% in cohort 3. Details of key demographic and clinical characteristics including comorbidities of the four subgroup cohorts are summarised in Table 1.
Treatment Patterns in the Real World
Treatment Patterns by Drug Class in Overall and Subgroup OA Cohort During Study Period
Analgesics, anaesthetic nerve block, antidepressants, antiepileptics, HA, and IA corticosteroids were the common drug classes prescribed for the treatment of OA. Analgesics constituted the most commonly prescribed drug class compared to other medications. Among the analgesics, oral NSAIDs followed by topical NSAIDs were prescribed frequently at any time during the follow-up period in all study cohorts. This was followed by more targeted treatment like HA, IA steroids, antidepressants, antiepileptics and opioids. The prescription analysis showed that nearly 41.6% (n = 4852) patients in the overall cohort, 39.8% (n = 3532) patients in cohort 1, 53.4% (n = 1990) patients in cohort 2, 84.3% (n = 1359) patients in cohort 3 and 39.9% (n = 238) patients in cohort 4 were prescribed oral NSAIDs. The percentage of patients with opioid prescription was as follows: 1.6% (n = 192) in the overall cohort, 1.5% (n = 137) in cohort 1, 3% (n = 111) in cohort 2, 6.1% (n = 99) in cohort 3 and 2.3% (n = 14) in cohort 4. Also, in the overall cohort, 50.2% of opioids-related claims were for tramadol as compared to 48.5% in cohort 1, 45.1% in cohort 2, 47.7% in cohort 3 and 15.8% in cohort 4. Prescription patterns of analgesics and other pharmacological drug classes in the management of patients in the overall cohort and subgroup cohorts are described in Table 3.
Non-pharmacological treatments commonly prescribed in the study cohorts included therapeutic exercise, ultrasound therapy, electrical stimulation, heat or cold pack. Other non-pharmacological treatments less commonly prescribed were electric current therapy, massage therapy, knee arthroscopy, paraffin bath therapy, infrared therapy, total knee arthroplasty, treatment for ankylosing spondylitis, total hip arthroplasty and revision of knee. Study analyses showed that 14.2% (n = 1654) patients in the overall cohort, 15.7% (n = 1396) patients in cohort 1, 33.1% (n = 1235) patients in cohort 2, 26.2% (n = 423) in cohort 3 and 18.4% (n = 110) in cohort 4 were prescribed non-pharmacological treatment along with pharmacological treatment.
Orthopaedics, general medicine/family medicine, internal medicine and rheumatology were the specialties frequently visited by patients across all cohorts for treatment advice. Orthopaedics was the most commonly visited specialty for prescription treatment; 46.7% (n = 5441) in the overall cohort, 47.7% (n = 4231) in cohort 1, 68.9% (n = 2570) patients in cohort 2, 69.6% (n = 1122) in cohort 3 and 53.3% (n = 318) patients in cohort 4 (see Table S4 in the supplementary material for details).
Switch in Treatment Patterns in Overall Cohort and Subgroup Cohort Patients During Follow-Up Period
The maximum (most) number of switches in treatment pattern was noted in patients who were prescribed oral NSAIDs as first treatment and the majority of these patients switched to HA as second treatment, across all cohorts. In the overall cohort, approximately 51.8% (n = 218) patients on first treatment with oral NSAIDs switched to HA (Table 4). Similar switch pattern from oral NSAIDs as first treatment to HA as second treatment was observed across four subgroup cohorts of OA hip and/or knee. Specifically, 51.9% (n = 182) patients in cohort 1, 52.2% (n = 175) patients in cohort 2, 55.8% (n = 91) patients in cohort 3 and 63.0% (n = 17) in cohort 4 switched from NSAIDs to HA as second treatment.
The maximum number of switches to third treatment was observed in patients prescribed HA as second treatment (Table 5). Approximately 50.7% (n = 76) patients in the overall cohort, 55.5% (n = 66) patients in cohort 1, 55.7% (n = 64) in cohort 2, 51.0% (n = 49) patients in cohort 3 and 45.5% (n = 5) in cohort 4 patients on HA switched to oral NSAIDs as third treatment (Table 5).
Time to Index Drug Treatment and First Surgery from First Diagnosis of OA in Overall and Subgroup Cohort During Study Period
The average time to treatment from first diagnosis of OA was 32 days in the overall cohort, 30 days in cohort 1, 37 days in cohort 2, 24 days in cohort 3 and 37 days in cohort 4 (Table 6). The average time to first surgery (hip and/or knee) was 227 days in the overall cohort, 202 days in cohort 1, 198 days in cohort 2, 264 days in cohort 3 and 192 days in cohort 4 (Table 7).
Healthcare Resource Utilisation and Costs of Osteoarthritis
All-Cause and OA-Specific HCRU Costs in Overall and Subgroup OA Cohorts During 12-Month Follow-Up Period
Data pertaining to the HCRU claims and the associated healthcare costs for the all-cause and the OA-cause was available from the 12-month post-index period for 11,651 and 8173 patients, respectively, in the overall cohort; 8877 and 6118 patients, respectively, in cohort 1; 3728 and 3229 patients, respectively, in cohort 2; 1612 and 1511 patients, respectively, in cohort 3 and 597 and 437 patients, respectively, in cohort 4 (Tables 8 and 9).
Costs incurred for inpatient, outpatient and emergency visit claims were higher in the overall cohort case group compared to the control group (see Table S5 in the supplementary material for details). Also, costs pertaining to medications, procedures, supplies and consumables and services were comparatively higher in the case group than control group (see Table S6 in the supplementary material for the details).
The mean number of all-cause HCRU claims and the associated costs for inpatient visits (mean HCRU claims = 1.7 per patient; mean cost = 7015.66 USD) and outpatient visits (mean HCRU claims = 36.3 per patient; mean cost = 4834.31 USD) were higher in cohort 4, as compared to the overall and other subgroup cohorts. For the emergency visits, the mean number of claims (mean HCRU claims = 3.1 per patient) was highest for cohort 3, while the associated cost (mean cost = 432.40 USD) was higher in cohort 4, compared to the overall and other subgroup cohorts (Table 8). Claims and costs pertaining to medications (mean HCRU claims = 15.1 per patient; mean cost = 1813.21 USD), procedures (mean HCRU claims = 16.2 per patient; mean cost = 3005.30 USD), consumables (mean HCRU claims = 2.1 per patient; mean cost = 1637.85 USD) and services (mean HCRU claims = 12.6 per patient; mean cost = 1104.97 USD) were higher in cohort 4 compared to the overall and other subgroup cohorts (see Table S7 in the supplementary material for the details).
The mean number of OA-specific inpatient claims did not vary across the study cohorts (mean number of claims, overall cohort = 1.2 per patient; cohorts 1–4 = 1.1 per patient), but the associated mean costs per patient for cohort 4 (11,354.39 USD) were higher compared to other cohorts (overall cohort = 6920.63 USD; cohort 1 = 7171.41 USD; cohort 2 = 8097.20 USD; cohort 3 = 10,661.13 USD). The mean number of OA-specific emergency claims was highest in cohort 2 (mean number of claims = 2.8 per patient) and in cohort 3 for outpatient claims (mean number of claims = 8.5 per patient). Associated costs for OA-specific inpatient claims were highest in cohort 4 and for both outpatient and emergency claims in cohort 3 (Table 9).
The claims for inpatient visits largely contributed to the mean annual all-cause and OA-related costs in overall and subgroup cohorts (Tables 8 and 9). A large proportion of all-cause HCRU costs was attributed to claims pertaining to procedures across all the cohorts (Table S7). The OA-related HCRU costs were mostly incurred from claims related to consumables (syringes, needles, sutures, gloves, masks, bandage rolls, etc. used in hospital) in the overall and subgroup cohorts (see Table S8 in the supplementary material for the details).
Discussion
The increasing burden of OA in the Middle East, particularly in the elderly, aged 60 years and above, is a cause of concern [16,17,18,19], and there is a paucity of data in the literature that analyse the demographic, clinical and economic burden of OA on the health sector of Middle Eastern countries. To our knowledge, the current study is the first of its kind to report incidence, treatment patterns and economic burden of OA among patients aged 18 years or older in Dubai, UAE. The data presented here, from a population of Emiratis and expatriates in Dubai, demonstrates that the patients with OA have higher prevalence of comorbidities characterised by a substantial clinical and cost burden relative to age- and gender-matched controls from the same geographical region.
The incident and prevalent cases of OA increased numerically by year during the study period. The majority of patients with OA in overall and subgroup cohorts belonged to the age group of 45–54 years, similar to findings from the Prevalence of Rheumatic Diseases and Osteoporosis (PRO) Dubai Study (study conducted in the population of Emiratis attending primary healthcare clinics in Dubai). Key findings from the PRO Dubai study suggest that patients belonging to age group of 41–60 years were at increased risk for developing knee OA. However, the study did not observe any significant association between knee OA and gender [20]. In the current study, prevalence of OA was found to be higher in men compared to women across all the cohorts, unlike most of the published literature where women are most affected [4,5,6]. This observation could be attributed to social and cultural barriers to access and utilise the healthcare services in the female population of Middle Eastern countries [21]. However, the high frequency of comorbid conditions in patients with OA compared to patients without OA was consistent with other studies suggesting that patients with OA have high comorbidity burden that contributes to increased pain severity and thus reduced physical function [22, 23]. The most prevalent comorbid conditions noted across all cohorts in the study included gastro-oesophageal reflux disease (GERD), gastrointestinal (GI) bleeding, hypertension, diabetes mellitus and chronic respiratory disease. Gastro-oesophageal reflux (45.5%) and peptic ulcer disease (3.8%), which are common contraindications for NSAIDs, formed a major comorbid disease condition among patients with contraindications to NSAIDs (cohort 4). Presence of comorbidities in patients with OA contributes to the high treatment costs [24] and is associated with increased complexity (polypharmacy, complex medication regimens) of managing these patients [25]. In the current analyses, this complexity was manifested by increased medication burden and greater prescription frequency for pain medications, NSAIDs in particular. In subsets of the OA population for whom NSAIDs are contraindicated, this trend in prescription poses a great challenge and need for effective alternative pain relief approaches.
NSAIDs were the most frequently prescribed medication class in line with findings from other studies [26]. Treatment patterns of NSAIDs and other medications commonly prescribed in the study, including opioids, HA, IA steroids, antidepressants and antiepileptics, were similar across all the cohorts. Across all cohorts orthopaedics and internal medicine/family medicine were the common specialties prescribing drugs for OA.
During the 12-month follow-up period, as expected, a major switch pattern from first treatment with NSAIDs was observed across all cohorts. The most frequently prescribed second treatment was IA-HA, consistent with earlier studies [27]. However, the majority of switches from IA-HA (second treatment) back to NSAIDs (third treatment) during the follow-up period was quite intriguing. There were 29% more switches during second treatment from NSAIDs to IA-HA than IA-HA to NSAIDs indicating potential toxicities associated with NSAIDs. However, during the third treatment switch, 42% on IA-HA switched back to NSAIDs. This could be attributed to a large unmet need of effective treatment and standard of care in third-line settings, as clinicians are left with minimal options of pharmacological agents for treating patients with OA.
In the study, the time to first surgery from time of diagnosis varied across the cohorts. Surgical intervention was inevitable in cohort 4 patients because of limited effective therapeutic pharmacotherapeutic option and therefore average time to first surgery was shorter compared to other cohorts.
In the current analyses, patients with contraindication to NSAIDs (cohort 4) constituted only 5% of the study population and patients with inadequate response to or inability to tolerate at least three pain medications (cohort 3) constituted 13.8% of the study population. Despite representing a lower percentage of the study population, patients in cohorts 3 and 4 had the highest average burden across all the cohorts in terms of visits or claims, HCRU and associated costs. The average number of claim visits and associated costs were also higher for cohort 4 compared to the overall cohort. Likewise, for medications, procedures, consumables and services, cohorts 3 and 4 dominated the average number and cost claims, suggestive of increased morbidity and disease burden in these specific subsets of the OA population. When OA-specific HCRU was reviewed in comparison to all-cause diseases, patients belonging to cohort 3 carried the highest burden for outpatient visits and associated costs; cohort 2 for emergency visits and associated costs; inpatient visits and costs were similar across all cohorts. For medication, procedures and services, cohort 3 dominated the average number and cost claims compared to other cohorts and cohort 4 dominated for consumables-related claims and costs. The trend observed from this study suggests that patients with inadequate response to or inability to tolerate at least three pain medications had the highest cost burden in OA-specific claims while cohort 4 carried the cost burden for all-cause HCRU claims.
Patients with OA utilised greater outpatient resources compared to patients without OA, regardless of specialty. This HCRU was reflected by higher mean costs for these resource categories in the OA case group compared to the control group. This observation of outpatient costs being the primary driver of direct medical costs in patients with OA is consistent with the literature [28]. Similarly, average claims and associated costs for medications, procedures and services were found to be higher in the case group compared to the control group. The higher HCRU costs observed in patients with OA compared to the control group may in part be attributable to the management of comorbidities, factors related to overall health status including obesity (a significant risk factor for OA for which information is not available in claims databases), and cost due to physiotherapy or OA-related diagnostic procedures like radiography, ultrasound, magnetic resonance imaging (MRI) and optical coherence tomography.
The strengths of our study are that we used data from DRWD which is the largest source of secondary data on OA in Dubai. In Dubai, approximately 80% of the population is covered by private insurance and 20% by public insurance. The DRWD captures information for almost the entire population covered by Dubai private health insurance, predominantly comprising the multi-ethnic expatriate population. Therefore, the results of this study would have a good level of generalizability and reflect the real-world patterns in OA prevalence and its related burden on the healthcare system and financial infrastructure in Dubai. Further, since claims data was used there is a lower possibility of selection bias and the data are inclusive of all treatment modalities performed by all healthcare providers and medical specialties.
Since the retrospective insurance e-claims database was used in this study, it is important to consider the limitations associated with such a study design, including potential errors in coding and recording. The study sample covered only the privately insured population of Dubai, UAE. There is only approximately 30–40% coverage of demographics in DRWD. Data on patients’ weight were not available in the e-claims database; hence, assessment of the treatment patterns based on body mass index (BMI) was not performed, which could have resulted in confounding bias in this study. Since publicly insured patients were not covered, the socioeconomic status would have influenced the treatment and cost utilisation outcome, thereby contributing to selection bias. Certain information not readily available in the e-claims database could have influenced study outcomes, such as certain clinical and disease-specific parameters. It is acknowledged that this limitation may significantly result in loss of initial sample of patients with OA of the hip and /or knee during the identification period. Another limitation is with regards to cost estimation in the study. Since insurance companies often set reimbursement limits for physicians, inpatient and outpatient services, it is not only possible but very likely that our study underestimates the true costs of OA from both societal and patient perspectives. Further, indirect costs due to absenteeism and presenteeism on the job (lost wages and productivity loss) that contribute substantially to the economic burden of OA are also not reflected in our study.
Conclusions
Despite the aforementioned limitations, the analyses from this claims data extend our knowledge of the clinical and economic burden and treatment landscape among the adult population in Dubai, UAE. The analyses presented here characterise patients with OA with respect to the significantly greater frequency of comorbid conditions that are present relative to those without OA, as well as to the higher use of resource utilisation. The analyses identify the increased burden of disease in patients with OA with inadequate response to or inability to tolerate more than three pain medications and patients with OA with contraindications to NSAIDs and emphasises the unmet need for effective pain relief in third-line settings among these subsets of patients with OA. Overall, our findings would help clinicians and insurance policymakers to make informed decisions, to improvise treatment strategies pertaining to effective pain relief for OA of the hip and/or knee patients in Dubai, UAE.
References
Thysen S, Luyten FP, Lories RJ. Targets, models and challenges in osteoarthritis research. Dis Model Mech. 2015;8(1):17–30.
Hunter DJ, Schofield D, Callander E. The individual and socioeconomic impact of osteoarthritis. Nat Rev Rheumatol. 2014;10(7):437–41.
Mahendira LJC, Papachristos A, Waddell J. Comparative clinical and cost analysis between surgical and non-surgical intervention for knee osteoarthritis. Int Orthop. 2020;44:77–83.
Vina ER, Kwoh CK. Epidemiology of osteoarthritis: literature update. Curr Opin Rheumatol. 2018;30(2):160–7.
Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–30.
Shane Anderson A, Loeser RF. Why is osteoarthritis an age-related disease? Best Pract Res Clin Rheumatol. 2010;24(1):15–26.
Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185–99.
Nuesch E, Dieppe P, Reichenbach S, Williams S, Iff S, Juni P. All cause and disease specific mortality in patients with knee or hip osteoarthritis: population based cohort study. BMJ. 2011;342:d1165.
Hermann W, Lambova S, Muller-Ladner U. Current treatment options for osteoarthritis. Curr Rheumatol Rev. 2018;14(2):108–16.
Ghouri A, Conaghan PG. Update on novel pharmacological therapies for osteoarthritis. Ther Adv Musculoskelet Dis. 2019. https://doi.org/10.1177/1759720X19864492.
Driban JBSM, Barbe MF, Balasubramanian E. Is osteoarthritis a heterogeneous disease that can be stratified into subsets? Clin Rheumatol. 2010;29(2):123–31.
Watt FE, Gulati M. New drug treatments for osteoarthritis: what is on the horizon? Eur Med J Rheumatol. 2017;2(1):50–8.
Mahagaonkar SB. Drug safety assessment using Dubai Real World Claims Database (DRWD). Joint International Conference and Expo on Industrial Pharmacy & 5th Global Pharmacovigilance Summit. J Develop Drugs. 2016;5(2):49.
Berger ARR, Lu Y, Zagar A, et al. Creation and validation of algorithms to identify patients with moderate-to-severe osteoarthritis of the hip and/or knee and inadequate/intolerable response to multiple pain medications. Postgrad Med. 2020;132:58–9.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Ahmed A, Rigi A, Kokash FE, Samad OA, Sebae IA, Shaikh RB. Arthritis among patients attending GMC hospital, Ajman, UAE: a cross sectional survey. Proceedings of the 6th Annual Scientific Meeting of Gulf Medical University, 2014 [cited 2021 November 8]. Available from: https://applications.emro.who.int/imemrf/Gulf_Med_Univ_Proc/Gulf_Med_Univ_Proc_2014_5-6_52_59.pdf.
Al-Shaali A, Al-Jaziri A. Health profile of elderly patients registered in the elderly home based primary care Dubai, UAE. Middle East J Age Aging. 2015;12:13–9.
Al-Modeer MA, Hassanien NS, Jabloun CM. Profile of morbidity among elderly at home health care service in Southern Saudi Arabia. J Family Community Med. 2013;20(1):53–7.
Naeem SMJF, Siddiqui MA, Khan MM. Pattern of morbidity among elders attending general practice: health needs assessment of geriatric patients in Oman. Geriatric Care. 2018. https://doi.org/10.4081/gc.2018.7774.
Cui ALH, Wang D. Global, regional prevalence, incidence and risk factors of knee osteoarthritis in population-based studies. EClinicalMedicine. 2020. https://doi.org/10.1016/j.eclinm.2020.100587.
Kronfol NM. Access and barriers to health care delivery in Arab countries: a review. East Mediterr Health J. 2012;18(12):1239–46.
Swain S, Sarmanova A, Coupland C, Doherty M, Zhang W. Comorbidities in osteoarthritis: a systematic review and meta-analysis of observational studies. Arthritis Care Res (Hoboken). 2020;72(7):991–1000.
Muckelt PE, Roos EM, Stokes M, et al. Comorbidities and their link with individual health status: a cross-sectional analysis of 23,892 people with knee and hip osteoarthritis from primary care. J Comorb. 2020. https://doi.org/10.1177/2235042X20920456.
Gore M, Tai KS, Sadosky A, Leslie D, Stacey BR. Clinical comorbidities, treatment patterns, and direct medical costs of patients with osteoarthritis in usual care: a retrospective claims database analysis. J Med Econ. 2011;14(4):497–507.
Manias E, Claydon-Platt K, McColl GJ, Bucknall TK, Brand CA. Managing complex medication regimens: perspectives of consumers with osteoarthritis and healthcare professionals. Ann Pharmacother. 2007;41(5):764–71.
Crofford LJ. Use of NSAIDs in treating patients with arthritis. Arthritis Res Ther. 2013;15(Suppl 3):S2.
Ishijima M, Nakamura T, Shimizu K, et al. Intra-articular hyaluronic acid injection versus oral non-steroidal anti-inflammatory drug for the treatment of knee osteoarthritis: a multi-center, randomized, open-label, non-inferiority trial. Arthritis Res Ther. 2014;16(1):R18.
Dunn JD, Pill MW. A claims-based view of health care charges and utilization for commercially insured patients with osteoarthritis. Manag Care. 2009;18(12):44–50.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Sponsorship for this study and Rapid Service Fee were funded by Pfizer Gulf FZ LLC.
Medical Writing, Editorial, and Other Assistance
Medical writing support was provided by Dr Kavitha Ganesha and assistance with data analyses was provided by Radhika Nijhawan, at Real-World Solutions, IQVIA. Support for this assistance was funded by Pfizer Gulf FZ LLC.
Authorship
All named authors meet the International Committee of Medical Journal Editors criteria for authorship of this article, take responsibility for the integrity of work as a whole, and have given their approval for this version to be published.
Author Contributions
JAA-S, AAA, AAS and MF, JGJ and AMG contributed for the concept and design of the final paper. SL, BCR and AN contributed for the concept, design and statistical analysis of the final paper. BCR helped revise the article in response to the reviewer’s comments.
Disclosures
Jean George Joury and Ahmed Mohamed Ghorab are Pfizer employees and may hold stock or stock options. Dr. Jamal Ali Al-Saleh, Dr. Ali Abbas Albelooshi, Dr. Ammar Amine Salti, Dr. Mohamed Farghaly, Sreenivasulu Linga, Badarinath Chickballapur Ramachandrachar, and Ashok Natarajan have nothing to disclose.
Compliance with Ethics Guidelines
All local, legal and regulatory guidelines were followed with no involvement of IRB approval or ICF signing, as this study used anonymised patient-level data.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available. Data for this study were made available to the authors through IQVIA (third-party license). The de-identified data of this study were handled by IQVIA Dubai FTE. There is a prior agreement with the Dubai Health Authority that de-identified data set will be kept confidential as there may be legal and ethical restriction with patient sensitive data. We have included all relevant data for this study in the manuscript. We have provided the aggregated data set as a Excel file containing all the analysis outputs for this study, which should consist the “minimal data set”.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Al-Saleh, J.A., Albelooshi, A.A., Salti, A.A. et al. Burden, Treatment Patterns and Unmet Needs of Osteoarthritis in Dubai: a Retrospective Analysis of the Dubai Real-World Claims Database. Rheumatol Ther 9, 151–174 (2022). https://doi.org/10.1007/s40744-021-00391-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-021-00391-z