Abstract
Purpose of review
Patient-centred care for people with osteoarthritis requires shared decision making. Understanding and considering patients’ preferences for osteoarthritis treatments is central to this. In this narrative review, we present an overview of existing research exploring patient preferences for osteoarthritis care, discuss clinical and research implications of existing knowledge and future research directions.
Recent findings
Stated preference studies have identified that patients place more importance on reducing or eliminating negative side effects rather than reducing pain, other clinical benefits or cost. Patients’ treatment preferences are influenced by characteristics such as age, symptom severity and beliefs about their osteoarthritis. Preferences appear to be largely stable over time and are not easily altered by single-point interventions.
Summary
Research exploring patient preferences for osteoarthritis treatments has increased in recent years. Treatment preferences appear to be primarily driven by patients’ wish to avoid adverse side effects and by symptom severity. Individualised, evidence-based information about potential treatments, delivered over the course of disease, is required.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
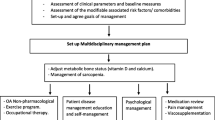
Osteoarthritis (OA) is one of the leading causes of disability worldwide [1]. As there is currently no cure for OA, treatments primarily aim to reduce joint pain and maintain mobility and quality of life. Evidence-based guidelines recommend non-pharmacological treatments (specifically therapeutic exercise, weight management and information and support) as core treatments, with pharmacological management alongside if required, at the lowest effective dose for the shortest possible time [2]. Referral for consideration of joint replacement is recommended if non-surgical management has not been effective and joint symptoms are substantially impacting the individual’s quality of life [2]. Given the increasing rates of hip and knee joint replacement for OA, finding ways to optimise the effectiveness of non-surgical treatments is urgently needed [3, 4].
Decisions about which OA treatments to use have historically been made by medical professionals, adopting an authoritative patient-practitioner relationship. More recently, the concept of shared decision making has been recognised as essential for patient-centred care. Shared decision making involves information exchange between patients and healthcare professionals. Healthcare professionals bring technical information about the disease and available treatments, while patients bring their personal experience, their concerns, expectations, and preferences about treatments, to together make treatment decisions [5].
Preferences are defined as “the expression of values for alternative options for action after informed deliberation of their risks and benefits” [6]. Considering patients’ preferences for OA treatments is central to shared decision making. Each treatment option for OA differs in terms of benefits and risks, so patients must frequently make decisions about what they need, what they prefer, and how they value the different aspects of each treatment. Patients’ preferences and beliefs about treatments are particularly important when there is a lack of certainty about treatment outcomes, or when there are multiple treatment options and patients need to balance the benefits and risks of each [2].
At an individual level, discussing and addressing patients’ concerns about treatments, and involving them in treatment decision making may improve treatment adherence and consequently treatment effectiveness [7••]. However, patient’s perspectives are becoming increasingly important in all aspects of OA care, from policy decisions to designing and evaluating healthcare programs and establishing treatment guidelines [8]. Improving our understanding of patients’ preferences for treatment is therefore critically important. Several different methods have been used to examine patients’ preferences for OA treatments. This narrative review presents an overview of existing research exploring patient preferences for osteoarthritis care, including patient use of, and satisfaction with, OA treatments as measured by survey studies; findings of studies using stated preference methods, results of qualitative studies (which offer an in-depth exploration of individual patient preferences, and patient preferences in trials and practice. Brief clinical and research implications of existing knowledge and future research directions are also discussed.
Use of, and satisfaction with, OA treatments
Several studies have used survey measures to explore patient use of and/or satisfaction with, treatments for OA. Findings highlight a mismatch between treatments most frequently used by patients with OA and those recommended in guidelines.
An Internet-based survey among people with knee OA in France, Germany, Spain, and the United Kingdom (UK) (n=2073) reported the most common treatments that respondents had used were non-prescription oral pain medication (74%), exercise (70%) and physical therapy (68%) [9]. Gökçe Kutsal et al. reported similar findings in a cross-sectional survey of OA patients in Turkey (n=305) [10•]. Most frequently reported treatments were oral drugs (80%), topical drugs (74%), a home-based exercise program (63%) and outpatient physical therapy (61%) [10•]. In the UK, Mitchell and Hurley surveyed 415 patients who had consulted a primary care physician for knee pain of more than 6-month duration. They also found that drugs (analgesic or NSAIDs) were the treatment most frequently received (83%), followed by physiotherapy (41%). All other therapies were used by less than 10% of respondents [11].
Hinman and colleagues explored the use of American College of Rheumatology (ACR) recommended non-drug, nonoperative interventions by people with hip and/or knee OA (n=591) in Australia [12]. The most common interventions that respondents were currently using were making efforts to lose weight (50%) and shoe orthoses (30%). Strengthening (26%) and stretching exercises (23%) were the interventions that participants had most commonly previously used [12]. Of note, 12% of respondents had never used any of the interventions. Similarly, among 202 patients awaiting orthopaedic consultation for hip or knee OA in Australia, Haskins et al found that 22% of respondents had not previously used any form of non-pharmacological conservative management. When responses were compared to clinical guidelines 33% indicated that they had never used any of the non-pharmacological management strategies that were classified as core guideline recommendations [13].
Patient satisfaction with treatments for their OA has been found to be variable. Haskins et al. reported that only 20% of respondents felt that they had received sufficient education about the diagnosis, their treatment options and prognosis [13]. When asked to rank which of the treatments they had used was most beneficial, respondents in the survey by Gökçe Kutsal et al. found that physical therapy was ranked the highest, followed by oral drugs and home-based exercise programs [10•]. Similarly, physical therapy was the most preferred treatment (41%) by respondents in Mitchell and Hurley’s survey, while only 4% reported drugs as their most preferred option [11].
Surveys have also been used to examine patient preferences for delivery of OA treatments. Ackerman and colleagues explored preferences for, and use of, disease-related education and support by younger people with hip and knee OA via a cross-sectional postal questionnaire in Australia (n=147) [14]. In relation to obtaining OA information, social media had been used by only a small proportion of respondents (5%), as had group self-management programs (3%), or telephone helplines (2%). Information packs delivered by post and online education programs were rated as the most useful by respondents, while social media was rated as the least useful and accessible. Both mailed and online information the advantage that people can access information at a time that suits them [14].
Studies using stated preference methods
Stated preference studies originated in economics but are increasingly being used in healthcare to capture individual preferences related to services, treatments, and outcomes [15]. An important assumption of stated preference methods is that a treatment can be broken down into attributes (such as effectiveness in reducing pain, length of treatment required and risk of adverse side effects), and that the value of a treatment depends on the levels of the attributes [8]. The idea behind stated preference methods is that they resemble the many decisions that people make daily when choosing between potential options [7]. Several different stated preference methods can be used, including discrete choice experiments (DCE), conjoint analysis (CA), best-worst scaling, adaptive conjoint analysis (ACA) and adaptive choice-based conjoint (ACBC). All approaches require participants to compare between two or more hypothetical treatments with different levels of the attributes of interest and make trade-offs to select which treatment they prefer. Stated preference methods allow researchers to quantify the relative importance of the different attributes that make up a treatment by quantifying the trade-offs that respondents make [8].
A recent systematic review of studies using CA techniques to explore patients’ preferences for OA treatments included 16 studies, with sample sizes ranging from 11 to 3895 [7]. The majority of the included studies investigated the side effects and features of medications, specifically NSAIDs, disease-modifying drugs and supplements. Overall, patients placed more importance on eliminating or reducing negative side effects (both common and rare) than on reducing pain, time to benefit, costs, how the medication was administered or the medication label [7]. Where investigated, studies found that patient characteristics including age and severity of OA symptoms had a significant impact on preferences. Respondents who were older appeared to be more willing than younger respondents to accept a higher risk of negative side effects in exchange for improvement in OA symptoms. People who reported less OA symptoms were more influenced by the potential side effects associated with NSAID than those who reported more severe OA symptoms. Interestingly, when respondents were asked to choose between an exercise program and OA medications, the potential side effects were still more influential on their decision than the potential benefits [7]. When presented with surgical treatments compared to non-surgical treatments, respondents with the highest pain levels, those whose function was the most limited and those of younger age were more likely to opt for the surgical option [7••].
Almost 20 years ago, Ratcliffe and colleagues were among the first to use stated preference methods to explore patient preferences for attributes of a number of treatment options for OA [16]. Survey respondents (n=412) appeared to place greater importance on the risk of serious negative side effects (including rare side effects) than mild to moderate side effects. When the authors analysed preferences by subgroup, they identified significant variation. The level of importance respondents placed on relief of joint aches increased with increasing severity of the respondents OA symptoms. As was identified in the systematic review, increasing age was associated with increasing willingness to accept a higher risk of serious side- effects in exchange for improvement in OA symptoms. Respondents in lower income brackets appeared to place more importance on treatments easing joint aches and increasing their mobility compared to those in higher income brackets. Respondents who had experienced gastrointestinal side effects from treatments previously were more willing to accept a higher risk of them than those who had not [16].
In their 2008 paper titled “If you want patients with knee osteoarthritis to exercise tell them about NSAIDS,” Fraenkel and Fried reported that exercise was the most preferred and NSAIDs were the least preferred treatment options, and that the risk of negative side effects more strongly influenced patients’ preferences rather than the likelihood of benefits [17]. Similarly, Pinto et al. found that respondents were more likely to choose exercise rather than drug treatments [18]. They found that combined risk of indigestion and bleeding ulcer accounted for relative importance of 41.3% compared to 28.9% for decrease pain and improvement in strength combined [18]. An earlier study explored the maximum acceptable risk increments (MARI) that respondents were willing to accept for various potential adverse effects from OA medications, using a probabilistic threshold technique [19]. Heart attack/stroke had the lowest MARI (between 3 and 5%, depending on initial risk and the level of pain relief) and dyspepsia had the highest (23% to 35%). Higher initial-risk levels were associated with increased willingness to accept a higher level of risk if it was coupled with pain relief benefits [19].
Two recent stated preference studies have focused on the preferences of stakeholders from different parts of health systems. In a DCE conducted in the Netherlands patients with knee or hip OA, those who had previously had a joint replacement, healthcare providers, and insurance company employees evaluated six attributes of OA treatments: waiting times, out of pocket costs, travel distance, involved healthcare providers, duration of consultation and access to specialist equipment [20•]. Findings showed that patients and healthcare providers placed the most importance on lower out of pocket costs, while insurance company employees rated including a joint consultation by GP and orthopaedic consultant as the most important. The duration of consultation was less important to patients than it was to healthcare providers and insurance company employees [20•]. In multi-criteria decision analysis survey in New Zealand and Australia, Chua and colleagues compared stakeholders’ preferences for interventions to manage knee OA with existing guideline recommendations and published evidence [21•]. Fifteen guideline-recommended interventions were rated by patients with knee OA, indigenous health advocates, healthcare providers, policy informants and OA researchers. Land-based exercise, topical NSAIDs and total joint replacement were rated the highest. Concerningly, weight management and self-management education, both recommended core interventions, were ranked 11th and 15th out of the 15 interventions. Notably, preferences did not differ between the included stakeholder groups [21•].
Qualitative studies
Qualitative studies offer an in-depth exploration of patient preferences for OA care. While the nature of qualitative studies means that they include considerably smaller sample sizes, they allow a more nuanced examination of patient preferences, and can include insight from patients as to why they have such preferences and what might be done to improve management. A systematic review of qualitative studies exploring patient beliefs about exercise interventions identified several points that patients felt would improve the delivery and uptake of exercise interventions [22]. The identified points included: providing better information and recommendations about the safety and importance of exercise, providing individually tailored exercise and challenging unhelpful health beliefs [22].
Bunzli and colleagues interviewed patients with end stage knee OA awaiting total knee replacement (TKR) in Australia, to explore why patients may feel that nonsurgical interventions are not valuable for treating knee OA [23]. Participants who reported that they believed their knee joint to be “bone on bone,” or that the damage was caused by “wear and tear” which would be worsened by increased loading through the knee and would worsen over time tended to avoid physiotherapy and exercise interventions. These participants instead sought experimental or surgical treatments which they believed would replace lost cartilage and consequently cure their knee pain [23]. In a separate analysis of the same interviews, the researchers explored which patient factors impacted on the decision to progress to TKR [24]. Participants described the referral from GP or other health professional to see an orthopaedic surgeon as being simple, whereas non-surgical intervention pathways were described as complex and unknown. Participants’ commonly felt that non-surgical interventions were “Band-Aid fixes” that would not repair the damage in their knee. In contrast, surgery was viewed as the “only true-blue fix” and was felt by many participants to be “inevitable.” Participants who actively took part in exercise and saw this as the best way to manage their pain most commonly described themselves as having been very active in the past. Ease of referral pathway was highlighted as a determining factor for participants [24].
Yeh et al. specifically interviewed patients with knee OA who reported that they were undecided about whether to go ahead with a TKR which had been recommended by a surgeon [25]. They found that participants’ indecision was most related to four areas: concerns related to treatments, concerns related to their physical condition, concerns related to surgical outcomes, and concerns related to postsurgical care. Participants who felt that they had not had their concerns addressed during the decision-making process reported that they wished to have access to more information regarding preparation for surgery, care after surgery, medicines and rehabilitation [25].
Patient preferences in trials and practice
Given the perceived importance of patient preference, it would be useful to know whether outcomes from OA treatments are better if treatment allocation is based on choice or preference. To the authors knowledge, there are currently no published preference randomised controlled trials (RCTs) in the OA field. A small number of RCTs have completed exploratory secondary analyses to examine relationships between patient preferences and clinical outcomes from OA treatment. Foster et al., in a RCT comparing an exercise intervention to acupuncture among 352 patients with knee OA, assessed treatment preferences at baseline [26]. They found that 20% of participants reported a treatment preference; of these, 10% preferred advice and exercise, 13% preferred acupuncture and 44% reported that they would prefer combined treatment. No evidence was observed of a relationship between the patients’ baseline treatment preferences or expectations and pain reduction at 6 or 12 months [26].
Moreton and colleagues developed and tested the utility of a multicriteria patient decision aid for people who were in the process of deciding on treatments for their OA [27•]. A shorter (n=625 respondents) and a longer form (n=180 respondents) of the decision aid were tested. The most important treatment outcomes across both forms of the decision aid were serious side effects, pain and function. Strength training was the highest rated treatment option overall, and arthroscopy was the lowest rated. Only one-third of respondents reported that the decision aid had changed their view about treatment. Interestingly, almost half of respondents (48%) felt that the decision aid would improve their future decision making about OA treatments [27•].
In a retrospective cohort study in the USA, Hurley at al. explored whether including a decision aid in primary care consultations was associated with changes in patients’ treatment preferences compared to including a decision aid in orthopaedic consultations [28•]. Results showed that almost 20% of patients with knee OA and 17% of patients with hip OA reported that they were still uncertain about their treatment preferences after completing the decision aids. Subgroup analyses found that patients who reported higher pain levels and those who were older were more likely to express a strong preference for surgery. Older patients who complete the decision aids during primary care consultations were less likely to prefer surgery afterwards compared to those who completed the decision aids during an orthopaedic consultation. The authors concluded that patients’ treatment preferences were generally stable over time, and that a single point decision aid may not necessarily shift preferences [28•]. Findings also highlighted that initiating treatment conversations in primary care settings, rather than only during secondary care consultations, may have important implications for engaging patients with shared decision making, and with using decision aids.
In the first RCT to use a DCE as an intervention in the OA field, Dowsey et al. are evaluating the effect of administering a DCE containing information on risks of postoperative complications and health status to patients awaiting TKR, compared to a control survey on patient-reported pain and function and satisfaction following TKR [29]. Results of the trial are pending.
Discussion
Considering patients’ preferences for OA treatments is a core component of shared decision making and patient-centred care. Research exploring patient preferences for OA treatments has increased over recent years. Survey studies have highlighted a mismatch between the most commonly used OA treatments and those that are recommended in evidence-based guidelines. Satisfaction with OA treatment is also variable. Stated preference studies commonly identified that reducing or eliminating adverse side effects is the primary driving force behind patient preferences for treatments, rather than reducing pain, cost, or increasing other clinical benefits. Patient characteristics appear to significantly influence treatment preferences, and preferences appear to require sustained and tailored input to change. However, the role of patient preferences in determining outcome from OA treatments remains unknown.
Several reasons might explain the mismatch between the most used OA treatments and those that are recommended in evidence-based guidelines. These include lack of a robust evidence base, lack of awareness of guidance on the part of healthcare providers, beliefs of healthcare professionals, structure of healthcare systems, but also patient preferences. Patient preferences may also partially explain lack of satisfaction with care. In some studies medication was shown to be a least preferred treatment option, but one that is commonly provided. Qualitative studies suggest some people do not like analgesics for OA due to concern over side effects, and a belief that it is masking rather than curing the problem [30]. These beliefs could therefore reduce adherence and could be a contributing factor to the overall small treatment effects seen in RCTs and meta-analyses of simple pain killers such as paracetamol [31].
The identified importance of potential side effects in determining patient preferences for treatments highlights the need for patients to have access to clear evidence-based information about potential treatments. The impact of presenting information to patients focusing specifically on the associated risks of adverse side effects (or the minimal risk of such effects in the case of treatments such as exercise) alongside the expected benefit is worth further exploration. However, communicating risk is difficult to achieve well, and there is currently no best practice approach [32]. Careful consideration should be given to the commonly held fear of numbers and lack of understanding of statistical concepts among both clinicians and patients, loss framing versus gain framing, presenting more versus fewer data points and whether to present relative risk versus absolute risk [32].
Being guided by patient preferences in selecting treatment options theoretically offers great potential to increase engagement and adherence to OA treatments, which in turn could optimise outcomes. Existing exploratory secondary analysis of OA treatment RCT data suggests no association, but this is limited and underpowered. Beyond OA, a 2019 systematic review and meta-analysis of the effect of treatment preferences across all RCTs found that allowing patients to select which treatment they took part in resulted in better clinical outcomes for mental health and pain compared to assigning patients to their non-preferred treatment [33].
For patients to make informed decisions about which OA treatments they prefer, they need to fully understand the treatment options. As Haskins and colleagues identified, many patients may feel that they have not received enough education about their diagnosis, their treatment options and the short and long-term prognosis for their condition, highlighting the importance of evidence-based information provision [13]. Patient characteristics appear to significantly impact treatment preferences, suggesting individualised information is required.
Decision aids, which are commonly presented as a printed pamphlet, videos or as an online program, offer great potential for providing education to patients about their conditions and helping them to be active in decision making. However, the study by Hurley et al. found that up to 20% of participants remained uncertain after completing the decision aid [28•]. The authors acknowledged that this may have been due to the non-randomised nature of the study. When planning pragmatic implementation careful consideration needs to be given to organisational contexts, and specifically to factors such as cultural differences, competing demands and the presence of champions that may influence patient engagement with decision aids [28•]. An additional complexity is that treatment preferences seem stable over time, and difficult to change with a single timepoint intervention. Future research utilising tailored information interventions and decision aids provided over multiple timepoints is needed.
Over recent years, increasing studies have focused on using stated preference methods to explore patient preferences for OA treatments. These methods have several advantages including the ability to replicate real-life choices, the ability to gather data across large numbers of participants and the ability to adapt to participant responses as they complete the questionnaire. However, there are also disadvantages to these methods that should be considered. The usefulness of any stated preference method is reliant on appropriate design, in particular the selection of suitable attributes and levels. Stated preference methods are commonly conducted online, meaning that those without internet access, or those who are not able to use an online platform are excluded. Alternative methods such as questionnaires and qualitative studies continue to offer important insight into patient preferences alongside stated preference methods.
Gaps in knowledge and future work
Whilst there has been an increasing focus on understanding patient preferences in the field of OA, gaps in knowledge remain around optimal content and delivery of core treatments including self-management, exercise and weight loss. Greater understanding of what people want to know to support self-management and weight loss might help these treatments to be perceived as more important. Greater knowledge about preferences around types of therapeutic exercise (e.g. strengthening, general aerobic and mind-body exercise) and mode of delivery (e.g. supervised versus unsupervised, exercise setting and exercise deliver) might facilitate design of exercise interventions that are most acceptable to patients. This could increase engagement and exercise adherence, thus improve effect sizes on pain and physical function from therapeutic exercise which currently, in comparison to non-exercise controls, are small and reduce over time [34]. This would need to be tested in a new clinical trial. Future research should also explore where outcomes from OA treatments are better if treatment allocation is based on patient preference.
Conclusions
Exploring and considering patient preferences are essential for shared decision making for OA treatments. Treatment preferences appear to be primarily driven by patients’ wish to avoid adverse side effects and by symptom severity. Individualised, evidence-based information about potential treatments, delivered over the course of disease, is required.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
GBD 2019 Diseases and Injuries Collaborators, et al. Lancet. 2020;396(10258):1204–22. https://doi.org/10.1016/s0140-6736(20)30925-9.
NICE. National Institute for Health and Care Excellence. Osteoarthritis in over 16s: diagnosis and management. London: National Institute for Health and Care Excellence (NICE); 2022.
Ackerman IN, Bohensky MA, de Steiger R, Brand CA, Eskelinen A, Fenstad AM, et al. Substantial rise in the lifetime risk of primary total knee replacement surgery for osteoarthritis from 2003 to 2013: an international, population-level analysis. Osteoarthr Cartil. 2017;25(4):455–61. https://doi.org/10.1016/j.joca.2016.11.005.
Ackerman IN, Bohensky MA, de Steiger R, Brand CA, Eskelinen A, Fenstad AM, et al. Lifetime risk of primary total hip replacement surgery for osteoarthritis from 2003 to 2013: a multinational analysis using National Registry Data. Arthritis Care Res. 2017;69(11):1659–67. https://doi.org/10.1002/acr.23197.
Rivero-Santana A, Perestelo-Perez L, Perez-Ramos J, Gonzalez-Lorenzo M, Serrano-Aguilar P. Treatment preferences in patients with knee or hip osteoarthritis: an overview. In: Qian C, editor. Osteoarthritis Diagnosis, Treatment and Surgery. Rijeka: IntechOpen; 2012. Ch. 12.
Bowling A, Ebrahim S. Measuring patients’ preferences for treatment and perceptions of risk. Qual Health Care. 2001;10(Suppl 1):i2–8. https://doi.org/10.1136/qhc.0100002.
•• Al-Omari B, McMeekin P, Bate A. Systematic review of studies using conjoint analysis techniques to investigate patients’ preferences regarding osteoarthritis treatment. Patient Prefer Adherence. 2021;15:197–211. https://doi.org/10.2147/ppa.S287322. The first systematic review of studies using conjoint analysis techniques to value patients’ preferences for OA treatments. Findings strongly indicate that patient preferences are driven by desire to avoid side effects, both common and rare
Hiligsmann M, Pinto D, Dennison E, Al-Daghri N, Beaudart C, Branco J, et al. Patients’ preferences for osteoarthritis treatment: the value of stated-preference studies. Aging Clin Exp Res. 2019;31(1):1–3. https://doi.org/10.1007/s40520-018-1098-3.
Posnett J, Dixit S, Oppenheimer B, Kili S, Mehin N. Patient preference and willingness to pay for knee osteoarthritis treatments. Patient Prefer Adherence. 2015;9:733–44. https://doi.org/10.2147/ppa.S84251.
• Gökçe Kutsal Y, Eyigör S, Karahan S, Günaydın R, İrdesel J, Sarıdoğan M, et al. Incorporating patient preferences into osteoarthritis treatment. Arch Rheumatol. 2021;36(4):577–86. https://doi.org/10.46497/ArchRheumatol.2022.8291. Cross-sectional survey exploring patient preferences for treatments and reasons for these preferences. Findings showed that when offered physical therapy or pharmacologic treatments patients chose physical therapy because of the lower risk of side effects
Mitchell HL, Hurley MV. Management of chronic knee pain: a survey of patient preferences and treatment received. BMC Musculoskelet Disord. 2008;9:123. https://doi.org/10.1186/1471-2474-9-123.
Hinman RS, Nicolson PJ, Dobson FL, Bennell KL. Use of nondrug, nonoperative interventions by community-dwelling people with hip and knee osteoarthritis. Arthritis Care Res. 2015;67(2):305–9. https://doi.org/10.1002/acr.22395.
Haskins R, Henderson JM, Bogduk N. Health professional consultation and use of conservative management strategies in patients with knee or hip osteoarthritis awaiting orthopaedic consultation. Aust J Prim Health. 2014;20(3):305–10. https://doi.org/10.1071/py13064.
Ackerman IN, Bucknill A, Page RS, Broughton NS, Roberts C, Cavka B, et al. Preferences for disease-related education and support among younger people with hip or knee osteoarthritis. Arthritis Care Res. 2017;69(4):499–508. https://doi.org/10.1002/acr.22950.
Clark MD, Determann D, Petrou S, Moro D, de Bekker-Grob EW. Discrete choice experiments in health economics: a review of the literature. Pharmacoeconomics. 2014;32(9):883–902. https://doi.org/10.1007/s40273-014-0170-x.
Ratcliffe J, Buxton M, McGarry T, Sheldon R, Chancellor J. Patients’ preferences for characteristics associated with treatments for osteoarthritis. Rheumatology. 2004;43(3):337–45. https://doi.org/10.1093/rheumatology/keh038.
Fraenkel L, Fried T. If you want patients with knee osteoarthritis (OA) to exercise: tell them about NSAIDS. The Patient. 2008;1(1):21–6. https://doi.org/10.2165/01312067-200801010-00005.
Pinto D, Bockenholt U, Lee J, Chang RW, Sharma L, Finn DJ, et al. Preferences for physical activity: a conjoint analysis involving people with chronic knee pain. Osteoarthr Cartil. 2019;27(2):240–7. https://doi.org/10.1016/j.joca.2018.10.002.
Kopec JA, Richardson CG, Llewellyn-Thomas H, Klinkhoff A, Carswell A, Chalmers A. Probabilistic threshold technique showed that patients’ preferences for specific trade-offs between pain relief and each side effect of treatment in osteoarthritis varied. J Clin Epidemiol. 2007;60(9):929–38. https://doi.org/10.1016/j.jclinepi.2007.01.001.
• Arslan IG, Huls SPI, de Bekker-Grob EW, Rozendaal R, Persoons MCT, Spruijt-van Hell ME, et al. Patients’, healthcare providers’, and insurance company employees’ preferences for knee and hip osteoarthritis care: a discrete choice experiment. Osteoarthr Cartil. 2020;28(10):1316–24. https://doi.org/10.1016/j.joca.2020.07.002. A large discrete choice experiment that explored osteoarthritis treatment preferences of multiple stakeholders. Identified differences in preferences between the groups, highlighting the importance of actively including patients in decision making about treatments
• Chua J, Hansen P, Briggs AM, Wilson R, Gwynne-Jones D, Abbott JH. Stakeholders’ preferences for osteoarthritis interventions in health services: a cross-sectional study using multi-criteria decision analysis. Osteoarthr Cartil Open. 2020;2(4):100110. https://doi.org/10.1016/j.ocarto.2020.100110. A multiple-stakeholder preference study and comparison to guideline recommendations. Found that not all recommended core interventions are preferred by cross-sectoral stakeholders, which may be a barrier to their uptake
Hurley M, Dickson K, Hallett R, Grant R, Hauari H, Walsh N, et al. Exercise interventions and patient beliefs for people with hip, knee or hip and knee osteoarthritis: a mixed methods review. Cochrane Database Syst Rev. 2018;17(4):CD010842. https://doi.org/10.1002/14651858.CD010842.pub2.
Bunzli S, O’Brien P, Ayton D, Dowsey M, Gunn J, Choong P, et al. Misconceptions and the acceptance of evidence-based nonsurgical interventions for knee osteoarthritis. a qualitative study. Clin Orthop Relat Res. 2019;477(9):1975–83. https://doi.org/10.1097/corr.0000000000000784.
O’Brien P, Bunzli S, Ayton D, Dowsey MM, Gunn J, Manski-Nankervis JA. What are the patient factors that impact on decisions to progress to total knee replacement? A qualitative study involving patients with knee osteoarthritis. BMJ Open. 2019;9(9):e031310. https://doi.org/10.1136/bmjopen-2019-031310.
Yeh WL, Tsai YF, Hsu KY, Chen DW, Chen CY. Factors related to the indecision of older adults with knee osteoarthritis about receiving physician-recommended total knee arthroplasty. Disabil Rehabil. 2017;39(22):2302–7. https://doi.org/10.1080/09638288.2016.1226407.
Foster NE, Thomas E, Hill JC, Hay EM. The relationship between patient and practitioner expectations and preferences and clinical outcomes in a trial of exercise and acupuncture for knee osteoarthritis. Eur J Pain. 2010;14(4):402–9. https://doi.org/10.1016/j.ejpain.2009.06.010.
• Moreton SG, Salkeld G, Wortley S, Jeon YH, Urban H, Hunter DJ. The development and utility of a multicriteria patient decision aid for people contemplating treatment for osteoarthritis. Health Expect. 2022;25(6):2775–85. https://doi.org/10.1111/hex.13505. Describes the multi-stage development and testing of a decision aid for patients. Most respondents reported a positive experience using the tool, and >1/3 reported that the tool had changed their treatment preferences
• Hurley VB, Wang Y, Rodriguez HP, Shortell SM, Kearing S, Savitz LA. Decision aid implementation and patients’ preferences for hip and knee osteoarthritis treatment: insights from the high value healthcare collaborative. Patient Prefer Adherence. 2020;14:23–32. https://doi.org/10.2147/ppa.S227207. An implementation study of a decision aid in clinical practice in the USA. Found that patient preferences were stable over time and not easily shited by a single point intervention
Dowsey MM, Scott A, Nelson EA, Li J, Sundararajan V, Nikpour M, et al. Using discrete choice experiments as a decision aid in total knee arthroplasty: study protocol for a randomised controlled trial. Trials. 2016;17(1):416. https://doi.org/10.1186/s13063-016-1536-5.
Milder TY, Lipworth WL, Williams KM, Ritchie JE, Day RO. “It looks after me”: how older patients make decisions about analgesics for osteoarthritis. Arthritis Care Res. 2011;63(9):1280–6. https://doi.org/10.1002/acr.20514.
Machado GC, Maher CG, Ferreira PH, Pinheiro MB, Lin CW, Day RO, et al. Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ. 2015;350:h1225. https://doi.org/10.1136/bmj.h1225.
Naik G, Ahmed H, Edwards AG. Communicating risk to patients and the public. Br J Gen Pract. 2012;62(597):213–6. https://doi.org/10.3399/bjgp12X636236.
Delevry D, Le QA. Effect of treatment preference in randomized controlled trials: systematic review of the literature and meta-analysis. The Patient. 2019;12(6):593–609. https://doi.org/10.1007/s40271-019-00379-6.
Holden M, Hattle M, Runhaar J, Riley R, Healey E, Quicke J, et al. Moderators of the effect of therapeutic exercise for knee and/or hip osteoarthritis: a systematic review and individual participant data meta-analysis with the OA trial bank. Lancet Rheumatology. 2023; in press
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Philippa Nicolson declares that she has no conflict of interest. Melanie Holden declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nicolson, P.J.A., Holden, M.A. Patient Preferences and Osteoarthritis Care: What Do We Know About What Patients Want from Osteoarthritis Treatment?. Curr Treat Options in Rheum 9, 120–131 (2023). https://doi.org/10.1007/s40674-023-00208-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40674-023-00208-w