Abstract
The ethnic density thesis suggests a protective health benefit for ethnic minorities living in places with higher concentration of co-ethnic residents. This paper aims to make a step change in the examination of this thesis by proposing ethnic diversity rather than co-ethnic density will be more protective for mental health. The paper proposes ethnic diversity could be a community asset that benefits the health of all people in a neighbourhood regardless of their own ethnic group. Individual data is taken from the UK Household Longitudinal Study, 2009–2019 linked to aggregate data from the 2001 and 2011 Censuses to test the association between co-ethnic density, ethnic diversity and mental health using the General Health Questionnaire 12-item scale. The paper takes a novel approach by measuring pre-existing (in 2001) and change in (2001–2011) co-ethnic density and ethnic diversity. Moderating effects of individual ethnic group, neighbourhood deprivation and perceived social cohesion are tested. Results show lower pre-existing co-ethnic density is related to lower mental health amongst the White British ethnic group but not in most ethnic minority groups. Greater pre-existing ethnic diversity in more deprived neighbourhoods is associated with better mental health regardless of individual ethnic group. A point of contention in the findings is no association between change in ethnic diversity and mental health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ethnic group disparities in mental health within the UK have been reported, revealing inequalities in psychological distress and common mental disorders [4, 37]. Crude rates of psychological distress are as much as 13 percentage points higher for selected ethnic minority groups compared with the White British group [4]. Recognised stressors contributing to these disparities includes stigma and racism, and limited access to quality mental healthcare [5, 19, 24, 41, 51]. The effect of racial discrimination, as well as having a direct impact on mental health, extends beyond an individual’s belief and behaviours. Structural racial discrimination classifies ethnic groups into social hierarchies, subsequently disempowering them and unevenly allocating resources and opportunities [25]. This results in the unequal distribution of societal resources including, but not limited to, education, employment and housing for ethnic minority groups, consequently influencing individual outcomes in social status and health [52, 53]. Moreover, the settlement history of immigrants in more deprived neighbourhoods and the continued concentration of native-born ethnic minorities in these same places is an intertwined consequence of racism and a further potential cause of disparities in mental health [15, 28].
There is increasing research suggesting that living in neighbourhoods with a greater concentration of ethnic minorities could provide protective impacts on mental health for ethnic minority people, a phenomenon known as the ethnic density thesis [7]. Evidence supporting the ethnic density thesis is available in several contexts with a history of immigration settlement and maturity of native born ethnic minorities, including the UK, Norway, US and Australia [17, 20, 22, 27]. UK-based studies have demonstrated the positive impacts of higher ethnic density on common mental disorders in Bangladeshi, Irish, Indian and Caribbean groups [16, 26]. The findings in relation to psychological distress are mixed with no clear association between co-ethnic density and measures such as the Short-Form 12 Health Survey or the Clinical Interview schedule-revised [16, 44]. The mental health outcomes where the greater ethnic density tends to be more strongly negatively associated include acute disorders such as psychosis as well as suicide [6, 34, 47].
The theoretical underpinning for the ethnic density thesis is that ethnic minorities who live in neighbourhoods with a greater concentration of people who are similar in terms of their ethnic identity can benefit from enhanced social support networks, a stronger sense of community and belonging and reduced exposure to interpersonal discrimination and social stigma [8, 44]. This is thought to be achieved through shared cultural values, language and religion [3, 7, 11, 17]. Ethnic density is often measured using one’s own ethnic group concentration in a neighbourhood. This assumes a valid distinction in the meaning of ethnic groups. The protective shield that ethnic density is claimed to provide is, however, likely to transcend across ethnic groups in terms of ethnic minority concentration. This is because the processes through which the ethnic density thesis is thought to operate such as support from formal institutions (e.g. religious congregation) or informal contacts (e.g. friends and neighbours) are unlikely to be bound by ethnic group categories, at least not as defined in the UK context [2]. It therefore might be the case that the protective effect of co-ethnic density on mental health might be theoretically overstated and the broader effect of ethnic diversity empirically neglected.
For example, people in the largest religious minority in England and Wales, Muslim are not exclusive to one ethnic minority group [35, 42] and therefore the protective benefit from shared religious practices would almost certainly transcend across ethnic groups. Moreover, there were fewer than 1% of neighbourhoods in England and Wales where an ethnic minority group, as measured by the 2011 Census 18-group classification, is in the majority and less than 2.5% of neighbourhoods where an ethnic group accounts for a third of the population [40]. This demonstrates that it is rare for an ethnic minority individual to live in a place where they are surrounded by the benefits described by the ethnic density thesis. By contrast, more than one in ten neighbourhoods have more than 50% of their population who are not in the ethnic majority group and are therefore ethnically diverse places (ibid).
There is also a contention of an imperfect operationalisation of the concept of ethnicity. This is particularly problematic in the UK where census-based ethnic groups are routinely evolving as measurement categories and have been contested by researchers and the people that they intend to represent [12, 45, 46, 54]. It is more likely that support across broader groups (perhaps all non-white or all non-White British) can provide a form of protection against poor mental health. It is perhaps the case that if ethnic minorities live in neighbourhoods where there are relatively fewer people in the ethnic majority, they might expect fewer (and perhaps less likely to experience) interpersonal racist incidents compared with living in neighbourhoods where their specific ethnic group is more prevalent. For example, would a person of a particular ethnic group feel more protected from racism in a neighbourhood where 25% of the population are in the same ethnic group as them and everyone else is in the ethnic majority or in a neighbourhood where more than 50% of the population are from an ethnic minority group? It is interesting to note that studies that pool minority samples, often because of sample size rather than substantive justification, report more consistent ethnic density associations compared with studies that focus on specific ethnic groups [3]. This is most common in studies examining rare outcomes such as psychosis and suicide [7].
It could therefore be the case that rather than the concentration of a particular ethnic group, ethnic density more broadly or perhaps ethnic diversity is a protective force against discrimination that in turn improves or maintains mental health. It might also be the case that ethnic diversity’s positive effect on mental health is not mediated through racial discrimination but is a positive community asset that benefits the mental health of all people regardless of their own ethnicity. Empirical investigations of the ethnic density thesis have often neglected the exploration of whether the ethnic majority might benefit in terms of mental health from living in places where ethnic minority density, however measured, is greater. Negative effects of own group ethnic density of majority groups on their mental health are often not clearly reported or dismissed as artifact rather than tangible effects [3, 17]. Positive ethnic minority density associations have been shown for the White British ethnic group in a study that reveals better mental health for white adolescents living in neighbourhoods which are ethnically diverse and less deprived [33]. This might reflect the positive impact for younger people being exposed to more diverse friendships or something else about places where ethnic minorities are more concentrated that has a positive effect on mental health.
There is evidence to suggest that very high concentrations of minority groups can be detrimental to mental health. Shankley and Laurence [44] suggest too much concentration could be problematic because it limits social opportunities. This could also be due to a lack of ethnic diversity rather than concentration of a particular ethnic group. It might not be a concentration of minorities that causes poor mental health, rather concentration of any one ethnic group (including the ethnic majority) is damaging to mental health. Becares et al. [10] find that Black populations living in places with higher concentration of co-ethnic minorities (>85%) in the US have poorer mental health compared with those living in less concentrated places. Vervoort et al. [50] find that ethnic minorities living in neighbourhoods with a higher concentration of people in the same ethnic group have less social contact with other ethnic minority groups.
There might also be a lack of differentiation between effects on mental health caused by ethnic density and neighbourhood deprivation in some studies. As previously stated, ethnic minorities in the UK are concentrated in more deprived neighbourhoods [9, 28]. When deprivation is accounted for, the ethnic density association with mental health often persists [3, 10, 16, 17, 22, 44]. There is reason to expect ethnic density will have a stronger effect on mental health in more deprived neighbourhoods because theory proposes it will lessen the impact of other predictors of poor mental health such as contextual disadvantage [7]. One might therefore not expect ethnic density to protect ethnic minorities, and perhaps the ethnic majority, to the same extent in less deprived neighbourhoods.
The relationship between ethnic density and social cohesion has been hypothesised as complicated. High levels of social cohesion could increase the risk of poor mental health among ethnic minorities living in neighbourhoods where their minority peers are sparse because they may face increased likelihood of exclusion from the social networks that operate in these places [3]. Some studies have found the association between ethnic density and mental health is attenuated when neighbourhood social cohesion is accounted for [8, 27]. However, most studies neglect the role of social cohesion or social contacts. This is problematic because ethnic composition of a neighbourhood is an important determinant of social contacts with the same or different ethnic groups [50].
A striking limitation of the existing literature is no study to date has considered the association between change in ethnic density and mental health outcomes. This is especially important in contexts which are becoming more ethnically diverse such as the UK [14, 32].
This paper aims to make a step change in the empirical conceptualisation of how ethnic density is associated with mental health for ethnic minority as well as the ethnic majority in England and Wales. We ponder whether scientists have been looking at the ethnic density thesis from a distorted perspective. It could be the case that diversity is good for the mental health of all people and is neither limited to ethnic minorities and nor due to a protective effect from concentrations of their own group. The paper also aims to make a step change in the empirical investigation of the ethnic density thesis by assessing change in ethnic density and its association with mental health using the Household Longitudinal Study (UKHLS). This is compared to most of the existing literature that uses one-point in time measurements of ethnic density and will therefore have greater concerns in terms of residual confounding (i.e. a potential third effect that is associated with ethnic density that means places with greater ethnic minority concentration have fewer ethnic minorities in poorer mental health). The current paper also builds on the existing literature that has started to investigate these confounders including individual and neighbourhood factors, such as detailed ethnic group and neighbourhood deprivation and social cohesion.
The following hypotheses will be tested:
-
(1)
Increasing ethnic density is associated with better mental wellbeing irrespective of individual ethnic group and more so when measuring ethnic density according to ethnic diversity rather than co-ethnic density.
-
(2)
The positive association between change in neighbourhood ethnic diversity and mental health is stronger in more deprived neighbourhoods, especially for minority ethnic groups.
-
(3)
The positive association between change in neighbourhood ethnic diversity and mental health is weaker among people who feel better about their neighbourhood (i.e. in more social cohesive contexts) for majority and minority ethnic groups.
The first hypothesis tests whether pre-existing and change in co-ethnic density or ethnic diversity are associated with mental health. The expectation is that both, but more so ethnic diversity, will be related to better mental health in ethnic minorities based on the existing literature that, on balance, supports the ethnic density hypothesis. Analogously, the White British group is expected to have better health when pre-existing and change in their co-ethnic density is lower and pre-existing and change in ethnic diversity is higher based on the limited evidence that suggests ethnic mixing is positive for the group’s mental health. The second hypothesis tests whether the association between ethnic diversity and mental health depends on the level of neighbourhood deprivation. The association is expected to be stronger in more deprived neighbourhoods because these places are accustomed and prepared for integrating people into their communities based on the literature described above. The third hypothesis tests potential moderation of subjective social cohesion with an expectation that those who think their neighbourhood is more cohesive are more able to draw on social support from local friends and neighbours. It is therefore expected there will be a less strong association between ethnic diversity and mental health in neighbourhoods where people feel more connected.
Methods
Data
The data are taken for residents in England and Wales from waves 1 to 9 (2009 to 2019) of the UK Household Longitudinal Study (UKHLS) and the 2001 and 2011 Censuses. UKHLS is an annual household survey that started in 2009–2011 with over 40,000 UK households providing multidisciplinary data on health, socioeconomic circumstances and social life [49]. In wave 1, there were 53,344 eligible households from two separate samples across Great Britain: a general population sample (43,267 issued households with a response rate of 57.1%) and an ethnic minority boost sample (10,077 issued households with a response rate of 39.9%). The general population sample were selected through a clustered and stratified, probability sample and the ethnic minority boost sample were selected from areas of high ethnic minority concentration in 2009–2010 where at least one member was from an ethnic minority group. By wave 9, the responding general population was 12,454 households (50.4% of the responding sample from wave 1) and the ethnic minority boost sample was 1495 households (37.2% of the responding sample from wave 1).
This paper uses UKHLS data from 40,012 respondents living in England and Wales at wave 1 who completed a main interview (i.e. not a proxy interview) mostly conducted in-person in respondents’ homes by trained interviewers. In later waves increasing proportions of the issued sample completed the survey online to a maximum of 70% of the sample. Some of the data described below are taken from a self-completion questionnaire, available on paper in the first two waves and later completed independently by the respondent on a computer at the time of the main interview. At wave 1, 33,839 respondents completed a self-completion questionnaire (84.6% of those who completed a main interview).
A UK Data Service Special Licence request was approved for this paper to access neighbourhood identifiers for UKHLS households [43]. The neighbourhood identifiers were used to link 2001 Census and 2011 Census data on ethnic group and deprivation to the UKHLS respondents at the lower super output area (LSOA) level. LSOAs have been widely used in health research to represent neighbourhoods [29,30,31, 38]. There was a total of 34,917 LSOAs in England and Wales for which census data were available in either or both 2001 and 2011, each containing, on average, 1500 residents. The University of Essex Ethics Committee has approved all data collection on UKHLS, including asking consent for all data linkage except to health records.
Measures
The outcome variable is the 12-item General Health Questionnaire (GHQ-12) collected via the UKHLS self-completion questionnaire. GHQ-12 is a validated screening tool for minor psychiatric morbidity and a good proxy measure for depressive disorders in the general population and in non-clinical settings [23, 36]. The GHQ-12 questionnaire consists of self-administered questions comprising two major components: the inability to carry out normal functions and the appearance of new and distressing phenomena in the past 2 weeks [23]. All items are rated on a 4-scale point, then the single scale is recoded between 0 and 3. A summative score is used as an indicator of severity of mental distress, giving it from 0 (the least distressed) to 36 (the most distressed).
The main explanatory variables are co-ethnic density and ethnic diversity. Co-ethnic density is measured as the percentage of a UKHLS respondents’ own ethnic group in the neighbourhood they were living in at UKHLS wave 1 (baseline). The 16-group classification from the 2001 Census was used to collapse census data for 2011 and UKHLS respondents by combining White Gypsy and Irish Travellers groups into the White Irish group and the Arab group into the Other group. Change in co-ethnic density is measured as the point difference between 2001 and 2011 in the percentage of a UKHLS respondents’ own ethnic group in the neighbourhood they were living at baseline. Ethnic diversity is calculated using the Simpson’s reciprocal index which measures the evenness of the 16 ethnic groups across all groups in a neighbourhood [46]. The values lie between 0 and 100 where 0 indicates that all people in a neighbourhood are from the same ethnic group (i.e. no ethnic diversity) and 100 indicates all people in a neighbourhood are distributed evenly across all ethnic groups. Change in ethnic diversity is calculated as the point difference between 2001 and 2011 in the Simpson’s reciprocal index value.
There was a small degree of change (4.0%) in the boundaries of LSOAs in England and Wales between 2001 and 2011. Some LSOAs were split into two or more new areas and others were merged from more than one to one (3.5%). These changes were resolved by creating a new set of LSOAs from 2001 and 2011 that were aggregated to create consistent boundaries. A small number of changes to LSOA boundaries (<1%) were such that it was not possible to match to a harmonised boundary for the calculated measures of change between 2001 and 2011. These were linked to the closest matching LSOA they were split from or merged with.
Neighbourhood deprivation is measured using the Townsend deprivation index which is widely used in health research [31, 33]. The measure is calculated from the 2011 Census by calculating the mean values of four standardised indicators: unemployment, non-car ownership, non-home ownership and household overcrowding [39, 48]. The standardised z-score is calculated by subtracting the value from the mean of the values then divided by the standard deviation to provide a variable with a mean of 0 and a standard deviation of 1.
Social cohesion is measured by the Buckner’s neighbourhood cohesion instrument that comprises (1) attraction to the neighbourhood, (2) neighbouring and (3) the psychological sense of community [13]. It is measured at the respondent level collected via the UKHLS self-completion questionnaire. The measure has shown to have good internal consistency and has been adapted in the UKHLS [13]. The total score is the mean from 8 items encompassing social cohesion scaled between 1 (lowest cohesion) and 5 (highest cohesion).
Respondent-level covariates that predict GHQ-12 included are age at time of the UKHLS main interview: age in years, gender (male or female), ethnic group (reduced 2001 Census 9-group classification to reflect UKHLS sample sizes), country of birth (UK or overseas), highest qualification (degree, A-level/equivalent, GCSE/equivalent, other qualification or no qualification) and Government Office Region (10-group Census classification).
Statistical Analysis
Multilevel modelling is used to take account of the longitudinal nature of UKHLS data. Responses at each survey wave (level 1) are nested within respondents (level 2). There are 32,086 respondents spread across nine survey waves with an average of 4.3 waves per respondent with each respondent present at least at baseline. A complete case sample of 138,058 person-year level 1 units are used in the analysis. The complete case sample removes 4.7% of respondents from wave 1 who completed a self-completion questionnaire but who are missing either or both outcome and covariate data used in this paper. Most of the missing data is due to incomplete information for social cohesion, which was missing for 4.5% of respondents. GHQ-12 was missing for 2.0% of respondents. All other covariates were complete or were missing for less than 0.1% of respondents. Multiple imputation by chained equations to replace missing values for the social cohesion measure did not change the substantive conclusions of this paper (analysis not presented here).
Models of interest are fitted with random intercepts where GHQ-12 is the outcome and exposure variables are added in separate models for either co-ethnic density or ethnic diversity. The pre-existing value of co-ethnic density or ethnic diversity in 2001 is added to each constituent model to avoid the misclassification of neighbourhoods with the greatest change in co-ethnic density or ethnic diversity and conflate those that are already co-ethnically dense or ethnically diverse. The exposure variables are time constant as are neighbourhood deprivation and individual social cohesion and individual controls for sex, ethnic group, country of birth, highest qualification and region. Individual age is the only time-varying covariate measured at the time of each survey wave. Age is added to each model as a second order polynomial to take account of the non-linear relationship between age and mental health.
To aid interpretation, the effect of skew and ensure comparability between the White British group and ethnic minority groups measures of pre-existing and change in co-ethnic density and pre-existing and change in ethnic diversity are categorised into deciles according to the national distribution where a higher value indicates a more co-ethnically dense or ethnically diverse neighbourhood. The neighbourhood deprivation measure is categorised into quintiles where a higher value indicates a more deprived neighbourhood. The categorised values of co-ethnic density, ethnic diversity and neighbourhood deprivation are added to the models as continuous terms.
Interaction terms between individual ethnic group and four exposures (pre-existing and change in co-ethnic density and pre-existing and change in ethnic diversity), in separate models, are used the test hypotheses 1 and 2 that aim to determine whether there is a qualitatively different association for the ethnic majority group (White British) and ethnic minority groups (eight other groups). Interaction terms are added to separate models where ethnic diversity is the main exposure to test hypotheses 3 and 4. An interaction between pre-existing and change in ethnic diversity and neighbourhood deprivation is added first followed by a three-way interaction between ethnic group, ethnic diversity and neighbourhood deprivation. The same steps are followed for an interaction between pre-existing and change in ethnic diversity and social cohesion in separate models. These models test whether respondents living in neighbourhoods that are ethnically diverse that are also deprived or cohesive are more likely to report better mental health compared with neighbourhoods that are less deprived or less cohesive. The results from models containing interaction terms are presented if a likelihood ratio test compared with a nested main effects model is statistically significant (p <0.05).
Longitudinal survey weights for the self-completion questionnaire at each survey wave are added to the model at level 1 to take account of the unequal probability of response and survey design. All analysis were conducted via Stata 17 using mixed command to estimate multilevel models and margins to calculate predicted values. The code used in this report is available on request for assessment, reuse and replication.
Results
Table 1 presents survey weighted characteristics for the complete case sample aggregated over UKHLS waves 1 to 9. The mean GHQ-12 score was 11.0. The mean pre-existing co-ethnic density was 79.4, which means, on average, UKHLS respondents, notwithstanding their ethnic group, live in neighbourhoods with most people in the same ethnic group as them. The mean change in co-ethnic density was −3.9 suggesting, on average, UKHLS sample members lived in neighbourhoods becoming less co-ethnically dense. The mean ethnic diversity, whether pre-existing (2.8) or change (2.1), was the same, to one decimal place, as the national distribution of neighbourhoods. The mean value of 2.1 for change in ethnic diversity indicates UKHLS sample members lived in neighbourhoods becoming more ethnically diverse, on average. The mean neighbourhood deprivation score (−1.5) was marginally above the mean for the national distribution of neighbourhoods, which was −1.6. The mean social cohesion score was 3.6.
Table 2 shows mean and standard deviation values of the explanatory variables by individual ethnic group. On average, the White British group lived in neighbourhoods with more than nine in ten people in the same ethnic group. By contrast, all ethnic minority groups, apart from the White Other group lived in neighbourhoods with, on average, 1% or less of people in the same ethnic group as themselves. The White British group are the only ethnic minority group whose mean co-ethnic density in the neighbourhoods they were living in, decreased between 2001 and 2011. Co-ethnic density increased most for the White Other group (2.9 percentage points) and least for the Mixed group (0.8 percentage points).
On average, ethnic minority groups lived in more ethnically diverse neighbourhoods and neighbourhoods becoming more diverse compared with the White British group. The Caribbean group (14.7) lived in the most ethnically diverse neighbourhoods. The mean value was similar for the Indian, Pakistani, Bangladeshi and African groups at around 11 but lower for the Mixed (7.5), Other (7.1) and White Other (6.4) groups. All ethnic groups lived in neighbourhoods with a mean positive change in ethnic diversity, including the White British group. The mean change in ethnic diversity was greatest for the Caribbean (10.5) and African (9.1) groups.
Ethnic minority groups lived in neighbourhoods that were more deprived, on average, compared with the White British group. The mean neighbourhood deprivation score was highest for the African (2.5) and Bangladeshi (2.4) groups and lowest among ethnic minority groups for the White Other (−0.3) and Mixed (0.2) groups. The mean social cohesion score was similar across ethnic groups. The Pakistani (3.8) and Bangladeshi (3.7) groups had the highest perceived social cohesion, whereas the Mixed (3.4) and White Other (3.4) had the lowest perceived social cohesion.
Figure 1 shows the GHQ-12 scores by ethnic group and UKHLS survey wave. The mean GHQ-12 at wave 1 is similar across ethnic groups. The African (9.9) and the Indian (10.5) groups were exceptions with significantly lower mean GHQ-12 scores at wave 1 compared with the White British (11.0) group. The mean GHQ-12 score remains constant for most ethnic groups apart from the Caribbean and Other groups that had significantly higher scores by wave 9 and the Pakistani group that had significantly higher scores at waves 3 and 4 compared with wave 1.
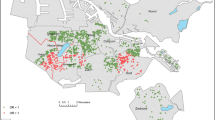
Figure 2 shows spatial variation in pre-existing neighbourhood ethnic density in 2001 across all neighbourhoods in England. It shows concentrations of the most ethnically diverse neighbourhoods in London and its surrounding urban areas as well as other selected urban areas including Birmingham, Manchester, Leicester, Coventry, Nottingham and Bradford. The least ethnically diverse neighbourhoods were concentrated in rural areas outside of the South East and selected towns in northern England. Figure 3 shows the spatial variation in the change in ethnic diversity between 2001 and 2011. There is a clear correlation between pre-existing and change in neighbourhood ethnic diversity (r = 0.66). The major urban areas containing concentrations of neighbourhoods that were already ethnically diverse in 2001 were the same places that increased their ethnic diversity most. However, there are neighbourhoods in these places that are in the lowest quintile for change in ethnic diversity (i.e. small increase or decrease in ethnic diversity). These are typically places already extremely diverse, such as selected neighbourhoods in Brent and Newham in London and neighbourhoods in Birmingham, Leicester and Bradford. The most notable difference in the spatial distributions between Fig. 2 and Fig. 3 is the rural areas and selected urban areas, which were not the same shade of red across the two maps. These places contain concentrations of the least ethnically diverse neighbourhoods in 2001 (i.e. darkest shade of red in Fig. 1) yet changes in ethnic diversity are at mid-points of the distribution (i.e. lighter shades of colour or white). These differences suggest that the change in ethnic diversity between 2001 and 2011 is less spatially concentrated than the level of ethnic diversity in 2001, and there is evidence of increased ethnic diversity in less diverse places.
-
Hypothesis 1: Greater ethnic density is associated with better mental health.
Figure 4 shows the results from a model predicting GHQ-12 score, including an interaction term between individual ethnic group and pre-existing (in 2001) co-ethnic density. The predicted values show for all ethnic groups, except for White British and Bangladeshi; there is an estimated lower GHQ-12 score at higher levels of pre-existing co-ethnic density. The differences across co-ethnic density deciles are significant only for the White British, White Other and Indian groups. The White Other group had a 1.3-point difference between the most and least co-ethnically concentrated deciles of neighbourhoods. There were no differences in predicted GHQ-12 scores for any ethnic group over change (2001–2011) in co-ethnic density level. The full model results for all regression analyses are available in the Appendix.
Figure 5 shows predicted values of GHQ-12 from a main effects model with a covariate for ethnic diversity rather than co-ethnic density. Respondents living in neighbourhoods with greater ethnic diversity in 2001 had lower predicted GHQ-12 scores, whereas those living in neighbourhoods that became more ethnically diverse during the 2000s had higher predicted GHQ-12 scores. The latter association is not significantly different between deciles of neighbourhoods by their change in ethnic diversity. The change in pre-existing ethnic diversity was associated with a 0.1 lower GHQ-12 score for each increase in the pre-existing decile of ethnic diversity. There were no ethnic group differences to these trends in models containing two-way interaction terms between individual ethnic group and either pre-existing ethnic diversity decile or change in ethnic diversity decile.
-
Hypothesis 2: ethnic diversity is more strongly associated with mental health in deprived neighbourhoods amongst minorities.
Figure 6 shows results from a model containing an interaction between pre-existing ethnic diversity and neighbourhood deprivation. There is a stronger association between pre-existing ethnic diversity and GHQ-12 score for those living in more deprived neighbourhoods. In the least deprived quintile of neighbourhoods, there is no significant difference across deciles of ethnic diversity. The slopes in Fig. 6 suggest that respondents living in more diverse neighbourhoods are predicted to have better mental wellbeing when also living in more deprived neighbourhoods. For example, respondents living in the most deprived quintile of neighbourhoods are predicted to have a 1.04-point difference in GHQ-12 when living in the most diverse deciles of neighbourhoods compared with the least diverse decile. Three-way interactions between ethnic diversity, neighbourhood deprivation and individual ethnic group showed the moderating association of neighbourhood deprivation was opposite for the Mixed ethnic groups compared with the White British group (see Model 10). For example, those living in the least deprived quintile of neighbourhoods that were also the least ethnically diverse are predicted to have a GHQ-12 score over four points higher than those living in the least deprived neighbourhood that are the most diverse. The predicted marginal difference was less than 0.2 between the Mixed ethnic group in the most deprived decile of neighbourhoods that were in the most and least diverse deciles. There were no significant moderating effects of neighbourhood deprivation on the change in ethnic diversity and GHQ-12 association.
There was no two-way moderating effect of the level of social cohesion on the ethnic diversity and mental health association. There is a moderating effect for the White Other ethnic group when adding a three-way interaction between ethnic diversity, social cohesion and individual ethnic group. Figure 7 shows that White Other respondents who felt their neighbourhood was less cohesive had a stronger association between ethnic diversity and mental health in the hypothesised direction. This is shown by the steeper slopes in Fig. 7 at the lower levels of cohesions, which suggests those who feel their neighbourhood is less cohesive have higher GHQ-12 scores when living in less diverse neighbourhoods compared with those who feel their neighbourhood is more cohesive whose GHQ-12 is more similar across deciles of ethnic diversity. There were no significant moderating effects of social cohesion on the change in ethnic diversity and GHQ-12 association.
-
Hypothesis 3: ethnic diversity is not as strongly related to mental health when social cohesion is greater.
Discussion
This paper has taken a novel approach to test the ethnic density hypothesis, which is ethnic minorities are better protected from deleterious determinants of health when living in places where there are more people from their ethnic background [11]. We have brought a challenge against how most of the existing literature empirically tests this hypothesis by proposing ethnic diversity rather than co-ethnic density of the neighbourhood in which a person lives could have a stronger protective effect on health. We suggest neighbourhood ethnic diversity’s protective effect will not be limited to ethnic minority groups but extends to the White British majority in England and Wales in what could be described as a community asset for all [33]. We have also aimed to forward the debate by analysing the association between change in co-ethnic density or ethnic diversity and mental health as well as the pre-existing level of co-ethnic density or ethnic diversity. We find support for our hypotheses in relation to pre-existing ethnic density but no support for an association between change in either co-ethnic density or ethnic diversity and mental health.
We find support for our first hypothesis that greater ethnic density is associated with better mental health and that this is not limited to ethnic minority groups. We find the association between ethnic diversity and mental health is the same across ethnic groups. Greater co-ethnic density is associated with worse mental health in the White British group. Against expectation, the only ethnic group estimated to have better mental wellbeing when living in neighbourhoods with greater concentrations of co-ethnic density is the White Other group. Many other studies find no evidence of a protective effect of co-ethnic density for some ethnic groups ([1, 16,17,18], p. 201; [20, 22]) or find that greater co-ethnic density is related to poorer mental health outcomes [8, 11].
Our second hypothesis suggested ethnic diversity is a community asset which is felt more strongly in deprived neighbourhoods because it is necessary to offset contextual disadvantage, especially for ethnic minority groups. We do not find support for ethnic minority groups reporting lower GHQ-12 when living in more ethnically diverse, deprived neighbourhoods relative to the White British group. We do, however, find that regardless of individual ethnic group, the association between ethnic diversity and mental wellbeing is stronger in more deprived neighbourhoods. This speaks to the sense that neighbourhood ethnic diversity is a community asset for all people regardless of ethnicity but is not as necessary when the neighbourhood is less deprived.
We find little support for our third hypothesis that the association between neighbourhood ethnic diversity and mental wellbeing is weaker for people who feel their neighbourhood is more cohesive. The White Other group was the only ethnic group who were predicted to report worse mental wellbeing when living in more ethnically diverse neighbourhoods if they felt their neighbourhood was less cohesive, whereas those who felt their neighbourhood was more cohesive did not report a difference in their mental wellbeing by ethnic diversity decile.
Our findings are important because they suggest ethnic minorities are potentially benefiting from a community asset (ethnic diversity) that is absent in neighbourhoods which most White British people in England live in, especially those living in deprived neighbourhoods. This is because White British people, on average, are living in neighbourhoods which are considerably less ethnically diverse than the typical neighbourhood in which ethnic minorities live (see Table 2). Although neighbourhood deprivation is lower for the White British group, those in this ethnic group living in deprived, ethnically homogenous neighbourhoods face a double disadvantage: poor neighbourhoods and lack of ethnic diversity. Ethnic diversity is becoming more evenly distributed spatially (see Figs. 2 and 3) and is increasing most in relative terms in places where diversity is currently low [32]. This suggests that if ethnic diversity is a community asset, there is a positive impact of it becoming increasingly available to more people, particularly the White British ethnic group. Figure 3 presents a clear pattern of increased diversity in less ethnically diverse neighbourhoods.
Our findings also point to a critical note of caution in making this causal inference. This is because we do not find that people living in neighbourhoods that are becoming more ethnically diverse have significant differences in their mental wellbeing when considering pre-existing neighbourhood diversity. Moreover, the point estimate suggests a direction of association opposite to our hypothesis. Unadjusted analysis (not shown here) suggests in neighbourhoods where ethnic diversity is increasing more, there is significantly higher levels of poor mental health. This presents a conundrum. It could be the case that too much diversity can be detrimental for health as suggested by [10, 44, 50]. Or it could be the case that there are unobserved characteristics about either the individuals living in places that are becoming more diverse or the neighbourhoods themselves that explains why the mental health of people living there is worse (or at least not better) compared with neighbourhoods that are not becoming as diverse.
Unobserved characteristics could include perceived or experienced racism. It could be the case that racism is felt more strongly in places where ethnic diversity is increasing most (i.e. neighbourhoods that are currently the least diverse), and that this is a strain on the mental health of individuals living there. These potential unobserved differences might also explain ethnic group inequalities in health that are not due to changes in ethnic diversity or other covariates included in the current analysis. For example, the Bangladeshi and Pakistani groups report considerably worse mental health compared with the White British group after considering pre-existing and change in ethnic diversity, neighbourhood deprivation, perceived cohesion, age, sex, foreign born status, qualifications and region. This finding is confirmed by Bamford et al. [4].
It is also important to consider the relative importance of factors such as neighbourhood deprivation and perceived neighbourhood cohesion which are both shown to be stronger determinants of mental health compared with ethnic diversity. This suggests that improvement in the equality of objective and subjective experience of place could help to reduce inequality in mental health and more so than fostering increased residential ethnic diversity, which, anyhow, is already taking place.
This paper has several strengths. We use a large nationally representative sample (UKHLS) that enables a more detailed classification of ethnic group compared with much of the ethnic density literature. Many existing studies evaluate the impacts for specific age or ethnic groups or places where ethnic minorities are densely populated (e.g. London) [17]. The longitudinal data analysis approach is a novel feature of the current paper as is the use of multiple measures of ethnic density to test whether co-ethnic density or ethnic diversity is the main driver of a protective effect of ethnic density. Differences between existing studies could be due to variant operationalisation of ethnic density, such as co-ethnic density, density of ethnic minorities and ethnic diversity. This is the first paper we are aware of that test both pre-existing ethnic density as well as change in ethnic density over a 10-year period prior to measurement of an outcome.
There are a number of limitations this paper should be set against. The categorisation of individual ethnicity is limited to nine groups due to the sample size restrictions of UKHLS. The longitudinal attrition of UKHLS study members is greater among ethnic minorities and therefore could add bias to the findings reported here. Missing data affected other variables used in the analysis, most notably the Buckner’s neighbourhood cohesion scale. The items that form the scale were collected as part of a self-completion questionnaire, itself not returned by all UKHLS study members. The definition of neighbourhood in this paper is operationalised using census LSOAs which were originally set by population threshold requirements and not intended to represent communities. The spatial scale of analysis of the effect of ethnic density varies substantially across studies from spaces containing hundreds of people to spaces containing millions of people. This makes it difficult to agree on how to conceptualise what is meant by ethnic density, but also limits comparison of the evidence between studies. The main premise of the ethnic density hypothesis is that minorities feel safer in areas where there are more people like them and are likely to experience less racist sentiment. This could be tested directly using measurements of racism using data such as the Evidence for Equality National Survey [21].
In summary, this paper finds greater ethnic diversity is associated with better mental health among those living in the most deprived areas. Our theoretical hypothesis and empirical testing support the notion that ethnic diversity is more strongly associated with mental health compared with co-ethnic density. It is unclear why increasing ethnic diversity is not associated with better mental health.
Data Availability
The UKHLS data that supports the findings of this manuscript was acquired under a special licence from the UK Data Service. The data was accessed and stored in secure conditions. The aggregate Censuses data were publicly available.
Code Availability
The authors declare that the code used in the development, analysis, and generation of results presented in this manuscript is available on request for assessment, reuse, and replication.
References
Arevalo SP, Tucker KL, Falcon LM. Beyond cultural factors to understand immigrant mental health: neighborhood ethnic density and the moderating role of pre-migration and post-migration factors. Soc Sci Med. 2015;138:91–100. https://doi.org/10.1016/j.socscimed.2015.05.040.
Aspinall PJ. The new 2001 census question set on cultural characteristics: is it useful for the monitoring of the health status of people from ethnic groups in Britain? Ethn Health. 2000;5(1):33–40. https://doi.org/10.1080/13557850050007329.
Baker SJ, Jackson M, Jongsma H, Saville CWN. The ethnic density effect in psychosis: a systematic review and multilevel meta-analysis. Br J Psychiatry. 2021;219(6):632–43. https://doi.org/10.1192/bjp.2021.96.
Bamford J, Klabbers G, Curran E, Rosato M, Leavey G. Social capital and mental health among black and minority ethnic groups in the UK. J Immigr Minor Health. 2021;23(3):502–10. https://doi.org/10.1007/s10903-020-01043-0.
Bansal N, Karlsen S, Sashidharan SP, Cohen R, Chew-Graham CA, Malpass A. Understanding ethnic inequalities in mental healthcare in the UK: a meta-ethnography. PLoS Med. 2022;19(12):e1004139. https://doi.org/10.1371/journal.pmed.1004139.
Bécares L, Das-Munshi J. Ethnic density, health care seeking behaviour and expected discrimination from health services among ethnic minority people in England. Health Place. 2013;22:48–55. https://doi.org/10.1016/j.healthplace.2013.03.005.
Becares L, Dewey ME, Das-Munshi J. Ethnic density effects for adult mental health: systematic review and meta-analysis of international studies. Psychol Med. 2018;48(12):2054–72. https://doi.org/10.1017/S0033291717003580.
Bécares L, Nazroo J. Chapter 14: Social capital, ethnic density and mental health among ethnic minority people in England: a mixed-methods study Handbook of Research Methods and Applications in Social Capital. Edward Elgar Publishing; 2015.
Bécares L, Nazroo J, Albor C, Chandola T, Stafford M. Examining the differential association between self-rated health and area deprivation among white British and ethnic minority people in England. Soc Sci Med. 2012;74(4):616–24. https://doi.org/10.1016/j.socscimed.2011.11.007.
Becares L, Nazroo J, Jackson J. Ethnic density and depressive symptoms among African Americans: threshold and differential effects across social and demographic subgroups. Am J Public Health. 2014;104(12):2334–41. https://doi.org/10.2105/AJPH.2014.302047.
Becares L, Nazroo J, Stafford M. The buffering effects of ethnic density on experienced racism and health. Health Place. 2009;15(3):670–8. https://doi.org/10.1016/j.healthplace.2008.10.008.
Berthoud R. Defining ethnic groups: origin or identify? Patterns Prejud. 1998;32(2):53–63. https://doi.org/10.1080/0031322X.1998.9970255.
Buckner JC. The development of an instrument to measure neighborhood cohesion. Am J Community Psychol. 1988;16(6):771–91. https://doi.org/10.1007/BF00930892.
Catney G, Lloyd CD, Ellis M, Wright R, Finney N, Jivraj S, Manley D. Ethnic diversification and neighbourhood mixing: a rapid response analysis of the 2021 Census of England and Wales. Geogr J. 2023;189(1):63–77. https://doi.org/10.1111/geoj.12507.
Darlington-Pollock F, Norman P. Examining ethnic inequalities in health and tenure in England: a repeated cross-sectional analysis. Health Place. 2017;46:82–90. https://doi.org/10.1016/j.healthplace.2017.04.011.
Das-Munshi J, Becares L, Dewey ME, Stansfeld SA, Prince MJ. Understanding the effect of ethnic density on mental health: multi-level investigation of survey data from England. Bmj. 2010;341:c5367. https://doi.org/10.1136/bmj.c5367.
Das-Munshi J, Schofield P, Bhavsar V, Chang C-K, Dewey ME, Morgan C, Stewart R, Thornicroft G, Prince MJ. Ethnic density and other neighbourhood associations for mortality in severe mental illness: a retrospective cohort study with multi-level analysis from an urbanised and ethnically diverse location in the UK. Lancet Psychiatry. 2019;6(6):506–17. https://doi.org/10.1016/s2215-0366(19)30126-9.
Emerson SD, Minh A, Guhn M. Ethnic density of regions and psychiatric disorders among ethnic minority individuals. Int J Soc Psychiatry. 2018;64(2):130–44. https://doi.org/10.1177/0020764017747909.
Eylem O, de Wit L, van Straten A, Steubl L, Melissourgaki Z, Danışman GT, de Vries R, Kerkhof AJFM, Bhui K, Cuijpers P. Stigma for common mental disorders in racial minorities and majorities a systematic review and meta-analysis. BMC Public Health. 2020;20(1):879. https://doi.org/10.1186/s12889-020-08964-3.
Feng X, Astell-Burt T, Kolt GS. Do social interactions explain ethnic differences in psychological distress and the protective effect of local ethnic density? A cross-sectional study of 226 487 adults in Australia. BMJ Open. 2013;3(5) https://doi.org/10.1136/bmjopen-2013-002713.
Finney N, Nazroo J, Shlomo N, Kapadia D, Becares L, Byrne B. Evidence for equality national survey: a survey of ethnic minorities during the COVID-19 pandemic, 2021. UK Data Service; 2023.
Finnvold JE, Ugreninov E. Refugees’ admission to mental health institutions in Norway: is there an ethnic density effect? Soc Sci Med. 2018;209:43–50. https://doi.org/10.1016/j.socscimed.2018.05.029.
Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, Rutter C. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. 1997;27(1):191–7. https://doi.org/10.1017/S0033291796004242.
Grey T, Sewell H, Shapiro G, Ashraf F. Mental health inequalities facing U.K. minority ethnic populations. J. Psychol. Iss. Organiz. Cult. 2013;3(S1):146–57. https://doi.org/10.1002/jpoc.21080.
Hackett RA, Ronaldson A, Bhui K, Steptoe A, Jackson SE. Racial discrimination and health: a prospective study of ethnic minorities in the United Kingdom. BMC Public Health. 2020;20(1):1652. https://doi.org/10.1186/s12889-020-09792-1.
Halpern D, Nazroo J. The ethnic density effect: Results from a national community survey of England and wales. Int J Soc Psychiatry. 2000;46(1):34–46. https://doi.org/10.1177/002076400004600105.
Hong S, Zhang W, Walton E. Neighborhoods and mental health: exploring ethnic density, poverty, and social cohesion among Asian Americans and Latinos. Soc Sci Med. 2014;111:117–24. https://doi.org/10.1016/j.socscimed.2014.04.014.
Jivraj S, Khan O. Chapter 13: How likely are ethnic minorities to live in deprived neighbourhoods? In: Jivraj S, Simpson, editors. Ethnic identity and inequalities in Britain: The dynamics of diversity. 1st ed. Bristol University Press, Policy Press; 2015. pp. 199–214. https://doi.org/10.2307/j.ctt1t89504.
Jivraj S, Murray ET, Norman P, Nicholas O. The impact of life course exposures to neighbourhood deprivation on health and well-being: a review of the long-term neighbourhood effects literature. Eur J Pub Health. 2020;30(5). https://doi.org/10.1093/eurpub/ckz153.
Jivraj S, Nicholas O, Murray ET, Norman P. Life course neighbourhood deprivation and self-rated health: does it matter where you lived in adolescence and do neighbourhood effects build up over life? Int J Environ Res Public Health. 2021;18(19). https://doi.org/10.3390/ijerph181910311.
Jivraj S, Norman P, Nicholas O, Murray ET. Are there sensitive neighbourhood effect periods during the life course on midlife health and wellbeing? Health Place. 2019;57:147–56. https://doi.org/10.1016/j.healthplace.2019.03.009.
Jivraj, S., & Simpson, L. (2015). Ethnic identity and inequalities in Britain: the dynamics of diversity.
Jun J, Jivraj S, Taylor K. Mental health and ethnic density among adolescents in England: a cross-sectional study. Soc Sci Med. 2020;244:1125692–2. https://doi.org/10.1016/j.socscimed.2019.112569.
Kirkbride JB, et al. Social deprivation, inequality, and the neighborhood-level incidence of psychotic syndromes in East London. Schizophr Bull. 2012;40(1):169–80. https://doi.org/10.1093/schbul/sbs151.
Lindley J. Race or religion? The impact of religion on the employment and earnings of Britain’s ethnic communities. J Ethn Migr Stud. 2002;28(3):427–42. https://doi.org/10.1080/13691830220146536.
Lundin A, et al. Validity of the 12-item version of the general health questionnaire in detecting depression in the general population. Public Health. 2016;136:66–74. https://doi.org/10.1016/j.puhe.2016.03.005.
McManus, S., Bebbington, P. E., Jenkins, R., & Brugha, T. (2016). Mental health and wellbeing in England: the adult psychiatric morbidity survey 2014 (S. McManus, P. Bebbington, R. Jenkins, & T. Brugha, Eds.). NHS Digital. https://openaccess.city.ac.uk/id/eprint/23646/
Murray ET, Nicholas O, Norman P, Jivraj S. Life Course neighborhood deprivation effects on body mass index: quantifying the importance of selective migration. Int J Environ Res Public Health. 2021;18(16):8339.
Norman P. Identifying change over time in small area socio-economic deprivation. Appl Spat Anal Polic. 2010;3(2):107–38. https://doi.org/10.1007/s12061-009-9036-6.
Office for National Statistics - Nomis. Ethnic group by religion. 2013. Available at: https://www.nomisweb.co.uk/census/2011/dc2201ew. Accessed 28 June 2024
Paradies Y, Ben J, Denson N, Elias A, Priest N, Pieterse A, Gupta A, Kelaher M, Gee G. Racism as a determinant of health: a systematic review and meta-analysis. PLoS One. 2015;10(9):e0138511. https://doi.org/10.1371/journal.pone.0138511.
Peach C. Muslims in the 2001 census of England and Wales: gender and economic disadvantage. Ethn Racial Stud. 2006;29(4):629–55. https://doi.org/10.1080/01419870600665284.
University of Essex, Institute for Social and Economic Research. Understanding society: Waves 1-13, 2009-2022: Special licence access, census 2011 lower layer super output areas. [data collection]. 13th ed. 2023. https://doi.org/10.5255/UKDA-SN-7248-13.
Shankley W, Laurence J. Community ethnic density, ethnic segregation, and ethnic minorities’ common mental disorders in the UK. Health Place. 2022;73:102723. https://doi.org/10.1016/j.healthplace.2021.102723.
Simpson L, Jivraj S, Warren J. The stability of ethnic identity in England and Wales 2001–2011. J R Stat Soc Ser A Stat Soc. 2016;179(4):1025–49. https://doi.org/10.1111/rssa.12175.
Simpson L, Warren J, Jivraj S. Chapter 6: Do people change their ethnicity over time? In: Jivraj S, Simpson L, editors. Ethnic identity and inequalities in Britain: The dynamics of diversity. 1st ed. Bristol University Press, Policy Press; 2015. pp. 79–92. https://doi.org/10.2307/j.ctt1t89504
Termorshuizen F, Braam AW, van Ameijden EJC. Neighborhood ethnic density and suicide risk among different migrant groups in the four big cities in the Netherlands. Soc Psychiatry Psychiatr Epidemiol. 2015;50(6):951–62. https://doi.org/10.1007/s00127-014-0993-y.
Townsend P. Deprivation. J Soc Policy. 1987;16(2):125–46. https://doi.org/10.1017/S0047279400020341.
University of Essex, & Institute for Social and Economic Research. Understanding Society: Waves 1-11, 2009-2020 and Harmonised BHPS. Waves. 2022;1-18:1991–2009.
Vervoort M, Flap H, Dagevos J. The ethnic composition of the neighbourhood and ethnic minorities’ social contacts: three unresolved issues. Eur Sociol Rev. 2011;27(5):586–605. https://doi.org/10.1093/esr/jcq029.
Wallace S, Nazroo J, Bécares L. Cumulative effect of racial discrimination on the mental health of ethnic minorities in the United Kingdom. Am J Public Health. 2016;106(7):1294–300. https://doi.org/10.2105/AJPH.2016.303121.
Williams DR, Mohammed SA. Racism and health I: pathways and scientific evidence. Am Behav Sci. 2013;57(8):1152–73. https://doi.org/10.1177/0002764213487340.
Williams DR, Priest N, Anderson NB. Understanding associations among race, socioeconomic status, and health: patterns and prospects. Health Psychol. 2016;35(4):407–11.
Williams M, Husk K. Can we, should we, measure ethnicity? Int J Soc Res Methodol. 2013;16(4):285–300. https://doi.org/10.1080/13645579.2012.682794.
Author information
Authors and Affiliations
Contributions
All authors played integral roles in the study, contributing to its conception, design, material preparation, data collection, analysis and writing. The final manuscript was read and approved by all authors.
Corresponding author
Ethics declarations
Ethics Approval
This is a secondary analysis of an observational study. The University of Essex Ethics Committee has approved all data collection on Understanding Society main study, including asking consent for all data linkage except to health records.
Informed Consent
All authors provide consent for the publication of the manuscript, including any text, tables and figures contained within the manuscript.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Regression results for GHQ-12 and neighbourhood co-ethnic density (pre-existing and change)
Model 1 - main effects
Model 2 - main effects + interaction between pre-existing neighbourhood co-ethnic density and individual ethnic group
Model 3 - main effects + interaction between change in neighbourhood co-ethnic density and individual ethnic group
Regression results for GHQ-12 and neighbourhood ethnic diversity (pre-existing and change)
Model 4 - main effects
Model 5 - main effects + interaction between pre-existing neighbourhood ethnic diversity and individual ethnic group
Model 6 - main effects + interaction between change in neighbourhood ethnic diversity and individual ethnic group
Model 7 - main effects + interaction between pre-existing in neighbourhood ethnic diversity and neighbourhood deprivation
Model 8 - main effects + interaction between change in neighbourhood ethnic diversity and neighbourhood deprivation
Model 9 - main effects + interaction between pre-existing in neighbourhood ethnic diversity and neighbourhood deprivation and individual ethnic group
Model 10 - main effects + interaction between change in neighbourhood ethnic diversity and neighbourhood deprivation and individual ethnic group
Model 11 - main effects + interaction between pre-existing in neighbourhood ethnic diversity and neighbourhood cohesion
Model 12 - main effects + interaction between change in neighbourhood ethnic diversity and neighbourhood cohesion
Model 13 - main effects + interaction between pre-existing in neighbourhood ethnic diversity and neighbourhood cohesion and individual ethnic group
Model 14 - main effects + interaction between change in neighbourhood ethnic diversity and neighbourhood cohesion and individual ethnic group
Estimates (95% CI) | |||
|---|---|---|---|
Model 1 | Model 2 | Model 3 | |
Co-ethnic density 2001 | 0.012 (−0.01, 0.035) | 0.042 (0.015, 0.07) | 0.011 (−0.012, 0.034) |
Co-ethnic density 2001–2011 | 0.011 (−0.011, 0.033) | 0.005 (−0.017, 0.027) | 0.018 (−0.009, 0.045) |
Ethnic group (ref: White British) | |||
White Other | 0.33 (0.001, 0.66) | 1.616 (0.832, 2.399) | 0.82 (0.11, 1.529) |
Mixed | 0.335 (−0.084, 0.754) | 0.844 (−0.177, 1.864) | 0.807 (−0.054, 1.669) |
Indian | −0.114 (−0.426, 0.199) | 0.779 (0.038, 1.52) | −0.449 (−1.206, 0.308) |
Pakistani | 0.665 (0.251, 1.079) | 1.078 (0.17, 1.985) | 0.651 (−0.522, 1.824) |
Bangladeshi | 1.127 (0.623, 1.63) | 0.06 (−1.254, 1.373) | 0.744 (−0.606, 2.095) |
Caribbean | −0.161 (−0.587, 0.264) | 0.966 (−0.997, 2.929) | 0.971 (−0.25, 2.192) |
African | −0.967 (−1.381, −0.552) | −0.038 (−1.418, 1.343) | −1.309 (−2.233, −0.385) |
Other | 0.47 (0.099, 0.841) | 0.75 (−0.241, 1.742) | 0.373 (−0.487, 1.232) |
Co-ethnic density 2001*ethnic group | |||
White Other | - | −0.187 (−0.288, −0.085) | - |
Mixed | - | −0.082 (−0.211, 0.047) | - |
Indian | - | −0.134 (−0.228, −0.039) | - |
Pakistani | - | −0.069 (−0.185, 0.046) | - |
Bangladeshi | - | 0.117 (−0.038, 0.272) | - |
Caribbean | - | −0.154 (−0.377, 0.07) | - |
African | - | −0.132 (−0.292, 0.028) | - |
Other | - | −0.051 (−0.172, 0.069) | - |
Co-ethnic density 2001–2011*ethnic group | |||
White Other | − | − | −0.076 (−0.171, 0.019) |
Mixed | − | − | −0.074 (−0.192, 0.045) |
Indian | − | − | 0.039 (−0.053, 0.131) |
Pakistani | − | − | −0.002 (−0.141, 0.136) |
Bangladeshi | − | − | 0.045 (−0.119, 0.208) |
Caribbean | − | − | −0.14 (−0.283, 0.004) |
African | − | − | 0.039 (−0.074, 0.151) |
Other | − | − | 0.009 (−0.1, 0.119) |
Townsend deprivation | 0.286 (0.239, 0.334) | 0.305 (0.256, 0.353) | 0.293 (0.244, 0.342) |
Social cohesion | −0.827 (−0.905, −0.749) | −0.828 (−0.906, −0.75) | −0.829 (−0.907, −0.751) |
Age | 0.148 (0.133, 0.163) | 0.147 (0.132, 0.163) | 0.148 (0.132, 0.163) |
Age2 | −0.001 (−0.002, −0.001) | −0.001 (−0.002, −0.001) | −0.001 (−0.002, −0.001) |
Sex (ref: male) | |||
Female | 1.125 (1.028, 1.222) | 1.124 (1.028, 1.221) | 1.124 (1.028, 1.221) |
UK born (ref: born in the UK) | |||
Not born in the UK | −0.598 (−0.814, −0.383) | −0.6 (−0.815, −0.384) | −0.591 (−0.806, −0.376) |
Qualification (ref: degree) | |||
A level or equivalent | 0.384 (0.249, 0.52) | 0.371 (0.236, 0.507) | 0.382 (0.246, 0.517) |
GCSE or equivalent | 0.425 (0.292, 0.558) | 0.408 (0.275, 0.542) | 0.423 (0.29, 0.556) |
Other qualification | 0.659 (0.475, 0.842) | 0.639 (0.456, 0.822) | 0.657 (0.474, 0.841) |
No qualifications | 0.968 (0.786, 1.149) | 0.945 (0.763, 1.127) | 0.967 (0.785, 1.148) |
Government Office Region (ref: London) | |||
North East | 0.098 (−0.193, 0.39) | −0.095 (−0.402, 0.212) | 0.075 (−0.22, 0.37) |
North West | 0.322 (0.103, 0.541) | 0.171 (−0.061, 0.402) | 0.303 (0.079, 0.526) |
Yorkshire and Yhe Humber | 0.236 (0.002, 0.47) | 0.074 (−0.171, 0.32) | 0.219 (−0.017, 0.456) |
East Midlands | 0.192 (−0.038, 0.421) | 0.043 (−0.197, 0.283) | 0.174 (−0.058, 0.406) |
West Midlands | 0.394 (0.165, 0.623) | 0.266 (0.028, 0.504) | 0.379 (0.148, 0.61) |
East of England | 0.143 (−0.073, 0.359) | 0.031 (−0.192, 0.254) | 0.133 (−0.086, 0.352) |
South East | 0.025 (−0.181, 0.232) | −0.075 (−0.287, 0.136) | 0.013 (−0.195, 0.222) |
South West | 0.215 (−0.018, 0.447) | 0.061 (−0.183, 0.306) | 0.199 (−0.038, 0.435) |
Wales | 0.468 (0.19, 0.746) | 0.294 (0.003, 0.586) | 0.443 (0.16, 0.725) |
Intercept | 8.788 (8.28, 9.297) | 8.757 (8.248, 9.266) | 8.77 (8.259, 9.28) |
Estimates (95% CI) | |||
|---|---|---|---|
Model 4 | Model 5 | Model 6 | |
Ethnic diversity 2001 | −0.055 (−0.083, −0.028) | −0.052 (−0.08, −0.024) | −0.052 (−0.08, −0.024) |
Ethnic diversity 2001–2011 | 0.013 (−0.012, 0.039) | 0.012 (−0.013, 0.038) | 0.007 (−0.021, 0.035) |
Ethnic group (ref: White British) | |||
White Other | 0.416 (0.089, 0.742) | 1.087 (0.337, 1.837) | 0.608 (−0.077, 1.294) |
Mixed | 0.438 (0.021, 0.856) | −0.165 (−1.502, 1.171) | 0.435 (−0.762, 1.632) |
Indian | 0.051 (−0.259, 0.361) | 0.82 (−0.567, 2.206) | −0.484 (−1.313, 0.345) |
Pakistani | 0.89 (0.476, 1.304) | 1.192 (−1.47, 3.854) | 0.66 (−0.302, 1.622) |
Bangladeshi | 1.291 (0.793, 1.79) | 0.495 (−3.068, 4.059) | 1.166 (−0.19, 2.522) |
Caribbean | 0.006 (−0.41, 0.422) | 3.453 (−0.977, 7.884) | −0.247 (−2.069, 1.575) |
African | −0.824 (−1.231, −0.417) | −1.055 (−3.259, 1.15) | −0.947 (−2.37, 0.475) |
Other | 0.593 (0.226, 0.96) | 0.312 (−1.03, 1.654) | 0.141 (−1.028, 1.31) |
Ethnic diversity 2001*ethnic group | |||
White Other | - | −0.096 (−0.194, 0.003) | - |
Mixed | - | 0.072 (−0.092, 0.235) | - |
Indian | - | −0.089 (−0.245, 0.066) | - |
Pakistani | - | −0.035 (−0.322, 0.252) | - |
Bangladeshi | - | 0.083 (−0.29, 0.456) | - |
Caribbean | - | −0.375 (−0.846, 0.096) | - |
African | - | 0.023 (−0.22, 0.266) | - |
Other | - | 0.032 (−0.126, 0.191) | - |
Ethnic diversity 2001–2011*ethnic group | - | ||
White Other | − | −0.028 (−0.12, 0.065) | |
Mixed | − | − | 0.001 (−0.146, 0.149) |
Indian | − | − | 0.068 (−0.03, 0.166) |
Pakistani | − | − | 0.03 (−0.086, 0.146) |
Bangladeshi | − | − | 0.016 (−0.14, 0.171) |
Caribbean | − | − | 0.029 (−0.166, 0.224) |
African | − | − | 0.014 (−0.142, 0.171) |
Other | − | − | 0.057 (−0.082, 0.195) |
Townsend deprivation | 0.295 (0.246, 0.345) | 0.3 (0.249, 0.35) | 0.299 (0.249, 0.349) |
Social cohesion | −0.825 (−0.903, −0.747) | −0.824 (−0.903, −0.746) | −0.826 (−0.904, −0.748) |
Age | 0.148 (0.132, 0.163) | 0.147 (0.132, 0.163) | 0.148 (0.132, 0.163) |
Age2 | −0.001 (−0.002, −0.001) | −0.001 (−0.002, −0.001) | −0.001 (−0.002, −0.001) |
Sex (ref: male) | |||
Female | 1.122 (1.025, 1.219) | 1.122 (1.025, 1.218) | 1.121 (1.024, 1.218) |
UK born (ref: born in the UK) | |||
Not born in the UK | −0.599 (−0.815, −0.384) | −0.612 (−0.826, −0.397) | −0.596 (−0.811, −0.381) |
Qualification (ref: degree) | |||
A level or equivalent | 0.371 (0.236, 0.507) | 0.372 (0.236, 0.507) | 0.371 (0.236, 0.507) |
GCSE or equivalent | 0.406 (0.273, 0.539) | 0.409 (0.276, 0.543) | 0.406 (0.273, 0.539) |
Other qualification | 0.636 (0.452, 0.819) | 0.635 (0.452, 0.818) | 0.637 (0.454, 0.821) |
No qualifications | 0.942 (0.76, 1.124) | 0.944 (0.763, 1.126) | 0.945 (0.764, 1.127) |
Government Office Region (ref: London) | |||
North East | −0.06 (−0.369, 0.248) | −0.086 (−0.398, 0.225) | −0.055 (−0.365, 0.254) |
North West | 0.21 (−0.021, 0.44) | 0.177 (−0.06, 0.414) | 0.216 (−0.017, 0.45) |
Yorkshire and The Humber | 0.111 (−0.132, 0.354) | 0.08 (−0.168, 0.328) | 0.123 (−0.123, 0.368) |
East Midlands | 0.083 (−0.155, 0.32) | 0.05 (−0.191, 0.292) | 0.094 (−0.146, 0.333) |
West Midlands | 0.301 (0.067, 0.536) | 0.27 (0.031, 0.51) | 0.307 (0.071, 0.544) |
East of England | 0.065 (−0.154, 0.284) | 0.031 (−0.195, 0.256) | 0.075 (−0.147, 0.297) |
South East | −0.042 (−0.25, 0.166) | −0.077 (−0.292, 0.138) | −0.033 (−0.244, 0.178) |
South West | 0.094 (−0.15, 0.338) | 0.063 (−0.186, 0.312) | 0.101 (−0.145, 0.348) |
Wales | 0.333 (0.041, 0.626) | 0.303 (0.006, 0.6) | 0.336 (0.042, 0.63) |
Intercept | 9.228 (8.716, 9.74) | 9.234 (8.722, 9.747) | 9.23 (8.718, 9.742) |
Estimates (95% CI) | ||||
|---|---|---|---|---|
Model 7 | Model 8 | Model 9 | Model 10 | |
Ethnic diversity 2001 | 0.002 (−0.041, 0.045) | −0.055 (−0.083, −0.028) | −0.013 (−0.06, 0.033) | −0.048 (−0.077, −0.02) |
Ethnic diversity 2001–2011 | 0.011 (−0.015, 0.036) | 0.016 (−0.024, 0.057) | 0.007 (−0.019, 0.033) | −0.004 (−0.049, 0.042) |
Ethnic group (ref: White British) | ||||
White Other | 0.43 (0.104, 0.756) | 0.416 (0.09, 0.743) | 1.044 (−0.6, 2.689) | 1.07 (−0.271, 2.41) |
Mixed | 0.476 (0.058, 0.894) | 0.439 (0.022, 0.857) | −2.738 (−5.188, −0.287) | −0.991 (−2.982, 0.999) |
Indian | 0.085 (−0.226, 0.395) | 0.05 (−0.259, 0.36) | −0.287 (−3.213, 2.638) | 0.769 (−1.299, 2.838) |
Pakistani | 0.985 (0.566, 1.404) | 0.89 (0.476, 1.304) | −1.66 (−6.319, 2.999) | −1.909 (−6.946, 3.128) |
Bangladeshi | 1.396 (0.892, 1.9) | 1.293 (0.794, 1.792) | −2.972 (−8.947, 3.004) | −0.599 (−5.76, 4.562) |
Caribbean | 0.086 (−0.333, 0.505) | 0.009 (−0.409, 0.426) | 8.407 (−3.042, 19.856) | 4.611 (−1.014, 10.235) |
African | −0.748 (−1.158, −0.338) | −0.821 (−1.23, −0.412) | −0.202 (−5.606, 5.203) | 1.623 (−3.042, 6.288) |
Other | 0.626 (0.258, 0.993) | 0.594 (0.227, 0.961) | 0.207 (−2.59, 3.003) | −0.01 (−2.591, 2.571) |
Townsend deprivation | 0.433 (0.326, 0.541) | 0.302 (0.207, 0.398) | 0.412 (0.298, 0.525) | 0.34 (0.223, 0.456) |
Ethnic diversity 2001* Townsend deprivation | −0.023 (−0.039, −0.008) | − | −0.016 (−0.034, 0.001) | − |
Ethnic diversity 2001–2011* Townsend deprivation | − | −0.001 (−0.015, 0.013) | − | −0.001 (−0.018, 0.017) |
Ethnic diversity 2001*ethnic group | ||||
White Other | − | − | −0.082 (−0.322, 0.158) | − |
Mixed | − | − | 0.413 (0.037, 0.788) | − |
Indian | − | − | 0.132 (−0.226, 0.489) | − |
Pakistani | − | − | 0.316 (−0.256, 0.887) | − |
Bangladeshi | − | − | 0.471 (−0.209, 1.15) | − |
Caribbean | − | − | −1.002 (−2.348, 0.343) | − |
African | − | − | −0.053 (−0.718, 0.612) | − |
Other | − | − | 0.156 (−0.211, 0.522) | − |
Ethnic diversity 2001–2011*ethnic group | ||||
White Other | − | − | − | −0.027 (−0.234, 0.18) |
Mixed | − | − | − | 0.188 (−0.129, 0.505) |
Indian | − | − | − | 0.032 (−0.255, 0.319) |
Pakistani | − | − | − | 0.404 (−0.231, 1.039) |
Bangladeshi | − | − | − | 0.255 (−0.425, 0.936) |
Caribbean | − | − | − | −0.483 (−1.141, 0.174) |
African | − | − | − | −0.271 (−0.85, 0.308) |
Other | − | − | − | 0.207 (−0.149, 0.563) |
Townsend deprivation*ethnic group | ||||
White Other | − | − | −0.008 (−0.754, 0.738) | −0.352 (−0.996, 0.291) |
Mixed | − | − | 1.059 (0.039, 2.08) | 0.548 (−0.236, 1.332) |
Indian | − | − | 0.167 (−1.107, 1.441) | −0.437 (−1, 0.126) |
Pakistani | − | − | 0.962 (−0.903, 2.828) | 0.558 (−0.594, 1.71) |
Bangladeshi | − | − | 1.812 (−1.214, 4.838) | 0.377 (−0.705, 1.46) |
Caribbean | − | − | −1.818 (−5.049, 1.414) | −1.439 (−2.731, −0.146) |
African | − | − | −0.349 (−2.056, 1.358) | −0.743 (−2.046, 0.56) |
Other | − | − | −0.174 (−1.244, 0.896) | −0.117 (−0.918, 0.684) |
Ethnic diversity 2001* Townsend deprivation* ethnic group | ||||
White Other | − | − | −0.001 (−0.09, 0.088) | − |
Mixed | − | − | −0.128 (−0.251, −0.005) | − |
Indian | − | − | −0.045 (−0.185, 0.095) | − |
Pakistani | − | − | −0.111 (−0.313, 0.091) | − |
Bangladeshi | − | − | −0.192 (−0.499, 0.115) | − |
Caribbean | − | − | 0.215 (−0.148, 0.578) | − |
African | − | − | 0.034 (−0.157, 0.226) | − |
Other | − | − | −0.01 (−0.134, 0.114) | − |
Ethnic diversity 2001–2011* Townsend deprivation* ethnic group | ||||
White Other | − | − | − | 0.023 (−0.053, 0.1) |
Mixed | − | − | − | −0.068 (−0.168, 0.033) |
Indian | − | − | − | 0.018 (−0.058, 0.093) |
Pakistani | − | − | − | −0.085 (−0.231, 0.061) |
Bangladeshi | − | − | − | −0.053 (−0.197, 0.091) |
Caribbean | − | − | − | 0.149 (−0.001, 0.298) |
African | − | − | − | 0.08 (−0.073, 0.232) |
Other | − | − | − | −0.024 (−0.125, 0.077) |
Social cohesion | −0.825 (−0.903, −0.747) | −0.825 (−0.903, −0.747) | −0.825 (−0.903, −0.747) | −0.824 (−0.903, −0.746) |
Age | 0.147 (0.132, 0.162) | 0.148 (0.132, 0.163) | 0.147 (0.132, 0.162) | 0.147 (0.132, 0.162) |
Age2 | −0.001 (−0.002, −0.001) | −0.001 (−0.002, −0.001) | −0.001 (−0.002, −0.001) | −0.001 (−0.002, −0.001) |
Sex (ref: male) | ||||
Female | 1.12 (1.023, 1.217) | 1.122 (1.025, 1.219) | 1.119 (1.022, 1.216) | 1.119 (1.022, 1.216) |
UK born (ref: born in the UK) | ||||
Not born in the UK | −0.593 (−0.809, −0.378) | −0.599 (−0.815, −0.384) | −0.599 (−0.814, −0.384) | −0.593 (−0.808, −0.377) |
Qualification (ref: degree) | ||||
A level or equivalent | 0.37 (0.235, 0.506) | 0.371 (0.235, 0.506) | 0.368 (0.232, 0.503) | 0.369 (0.234, 0.505) |
GCSE or equivalent | 0.401 (0.268, 0.534) | 0.406 (0.272, 0.539) | 0.402 (0.269, 0.535) | 0.404 (0.271, 0.537) |
Other qualification | 0.633 (0.449, 0.816) | 0.635 (0.452, 0.819) | 0.627 (0.445, 0.81) | 0.638 (0.455, 0.822) |
No qualifications | 0.934 (0.752, 1.115) | 0.942 (0.76, 1.124) | 0.931 (0.749, 1.113) | 0.938 (0.756, 1.12) |
Government Office Region (ref: London) | ||||
North East | −0.169 (−0.486, 0.148) | −0.064 (−0.376, 0.248) | −0.178 (−0.496, 0.14) | −0.102 (−0.416, 0.212) |
North West | 0.138 (−0.098, 0.374) | 0.207 (−0.026, 0.44) | 0.121 (−0.12, 0.362) | 0.186 (−0.05, 0.421) |
Yorkshire and The Humber | 0.034 (−0.214, 0.282) | 0.108 (−0.137, 0.354) | 0.017 (−0.235, 0.269) | 0.084 (−0.164, 0.332) |
East Midlands | 0.016 (−0.225, 0.258) | 0.08 (−0.159, 0.319) | 0.002 (−0.243, 0.247) | 0.072 (−0.169, 0.312) |
West Midlands | 0.239 (0, 0.477) | 0.299 (0.062, 0.535) | 0.226 (−0.016, 0.468) | 0.28 (0.042, 0.519) |
East of England | −0.018 (−0.245, 0.208) | 0.062 (−0.16, 0.284) | −0.031 (−0.262, 0.2) | 0.042 (−0.183, 0.267) |
South East | −0.133 (−0.35, 0.084) | −0.045 (−0.257, 0.167) | −0.142 (−0.365, 0.08) | −0.063 (−0.277, 0.151) |
South West | 0.028 (−0.221, 0.277) | 0.092 (−0.155, 0.338) | 0.013 (−0.24, 0.266) | 0.075 (−0.173, 0.323) |
Wales | 0.253 (−0.045, 0.552) | 0.331 (0.036, 0.626) | 0.237 (−0.065, 0.538) | 0.295 (−0.003, 0.593) |
Intercept | 9.014 (8.488, 9.539) | 9.216 (8.689, 9.742) | 9.09 (8.555, 9.626) | 9.221 (8.682, 9.759) |
Estimates (95% CI) | ||||
|---|---|---|---|---|
Model 11 | Model 12 | Model 13 | Model 14 | |
Ethnic diversity 2001 | −0.106 (−0.205, −0.006) | −0.055 (−0.083, −0.028) | −0.087 (−0.205, 0.031) | −0.052 (−0.08, −0.024) |
Ethnic diversity 2001–2011 | 0.013 (−0.012, 0.039) | −0.01 (−0.108, 0.087) | 0.012 (−0.013, 0.038) | 0.001 (−0.115, 0.116) |
Ethnic group (ref: White British) | ||||
White Other | 0.423 (0.096, 0.749) | 0.419 (0.092, 0.746) | 3.579 (−0.878, 8.036) | 1.928 (−1.901, 5.756) |
Mixed | 0.445 (0.028, 0.863) | 0.441 (0.023, 0.858) | 4.651 (−2.142, 11.444) | 3.641 (−3.047, 10.328) |
Indian | 0.049 (−0.261, 0.358) | 0.05 (−0.26, 0.36) | −0.434 (−9.701, 8.832) | 0.954 (−4.188, 6.096) |
Pakistani | 0.879 (0.465, 1.293) | 0.887 (0.473, 1.301) | −11.639 (−30.677, 7.399) | −1.543 (−7.224, 4.138) |
Bangladeshi | 1.278 (0.779, 1.777) | 1.287 (0.788, 1.787) | 5.895 (−19.909, 31.7) | −0.523 (−8.485, 7.44) |
Caribbean | 0.009 (−0.407, 0.426) | 0.007 (−0.409, 0.423) | 10.468 (−9.057, 29.993) | 8.722 (−3.475, 20.919) |
African | −0.819 (−1.226, −0.412) | −0.822 (−1.229, −0.415) | 1.902 (−7.551, 11.355) | 0.921 (−5.462, 7.303) |
Other | 0.598 (0.231, 0.965) | 0.595 (0.228, 0.962) | −2.962 (−10.885, 4.96) | −5.965 (−13.489, 1.559) |
Social cohesion | −0.902 (−1.07, −0.734) | −0.861 (−1.025, −0.698) | −0.882 (−1.062, −0.703) | −0.846 (−1.022, −0.669) |
Ethnic diversity 2001* social cohesion | 0.014 (−0.012, 0.04) | − | 0.01 (−0.021, 0.041) | − |
Ethnic diversity 2001-11* social cohesion | − | 0.007 (−0.019, 0.032) | − | 0.001 (−0.029, 0.032) |
Ethnic diversity 2001*ethnic group | ||||
White Other | − | − | −0.6 (−1.168, −0.031) | − |
Mixed | − | − | −0.271 (−1.058, 0.515) | − |
Indian | − | − | 0.07 (−0.951, 1.09) | − |
Pakistani | − | − | 1.301 (−0.744, 3.347) | − |
Bangladeshi | − | − | −0.343 (−3.018, 2.332) | − |
Caribbean | − | − | −0.954 (−3.019, 1.112) | − |
African | − | − | −0.305 (−1.351, 0.741) | − |
Other | − | − | 0.178 (−0.77, 1.126) | − |
Ethnic diversity 2001–11*ethnic group | ||||
White Other | − | − | − | −0.386 (−0.881, 0.109) |
Mixed | − | − | − | −0.154 (−0.935, 0.628) |
Indian | − | − | − | −0.117 (−0.718, 0.483) |
Pakistani | − | − | − | 0.238 (−0.452, 0.929) |
Bangladeshi | − | − | − | 0.373 (−0.553, 1.298) |
Caribbean | − | − | − | −0.807 (−2.108, 0.494) |
African | − | − | − | −0.206 (−0.928, 0.516) |
Other | − | − | − | 0.545 (−0.356, 1.446) |
Social cohesion*ethnic group | ||||
White Other | − | − | −0.724 (−1.925, 0.476) | −0.391 (−1.41, 0.628) |
Mixed | − | − | −1.364 (−3.154, 0.426) | −0.895 (−2.669, 0.879) |
Indian | − | − | 0.344 (−2.255, 2.944) | −0.395 (−1.767, 0.976) |
Pakistani | − | − | 3.384 (−1.597, 8.365) | 0.561 (−0.887, 2.01) |
Bangladeshi | − | − | −1.529 (−8.879, 5.821) | 0.454 (−1.686, 2.594) |
Caribbean | − | − | −1.993 (−7.235, 3.248) | −2.485 (−5.726, 0.756) |
African | − | − | −0.852 (−3.498, 1.795) | −0.542 (−2.248, 1.165) |
Other | − | − | 0.942 (−1.325, 3.21) | 1.723 (−0.414, 3.861) |
Ethnic diversity 2001* social cohesion * ethnic group | ||||
White Other | − | − | 0.148 (−0.009, 0.305) | − |
Mixed | − | − | 0.095 (−0.114, 0.303) | − |
Indian | − | − | −0.044 (−0.33, 0.242) | − |
Pakistani | − | − | −0.353 (−0.886, 0.181) | − |
Bangladeshi | − | − | 0.123 (−0.639, 0.884) | − |
Caribbean | − | − | 0.164 (−0.391, 0.719) | − |
African | − | − | 0.094 (−0.199, 0.388) | − |
Other | − | − | −0.042 (−0.314, 0.23) | − |
Ethnic diversity 2001–11* social cohesion * ethnic group | ||||
White Other | − | − | − | 0.107 (−0.029, 0.243) |
Mixed | − | − | − | 0.039 (−0.169, 0.248) |
Indian | − | − | − | 0.051 (−0.11, 0.212) |
Pakistani | − | − | − | −0.053 (−0.23, 0.124) |
Bangladeshi | − | − | − | −0.096 (−0.343, 0.152) |
Caribbean | − | − | − | 0.23 (−0.116, 0.577) |
African | − | − | − | 0.064 (−0.13, 0.258) |
Other | − | − | − | −0.136 (−0.393, 0.12) |
Townsend deprivation | 0.296 (0.246, 0.346) | 0.296 (0.246, 0.346) | 0.302 (0.252, 0.352) | 0.301 (0.251, 0.351) |
Age | 0.147 (0.132, 0.163) | 0.147 (0.132, 0.163) | 0.147 (0.132, 0.162) | 0.147 (0.132, 0.163) |
Age2 | −0.001 (−0.002, −0.001) | −0.001 (−0.002, −0.001) | −0.001 (−0.002, −0.001) | −0.001 (−0.002, −0.001) |
Sex (ref: male) | ||||
Female | 1.122 (1.025, 1.219) | 1.122 (1.025, 1.219) | 1.122 (1.025, 1.219) | 1.121 (1.024, 1.218) |
UK born (ref: born in the UK) | ||||
Not born in the UK | −0.604 (−0.82, −0.389) | −0.601 (−0.817, −0.386) | −0.604 (−0.819, −0.388) | −0.59 (−0.807, −0.374) |
Qualification (ref: degree) | ||||
A level or equivalent | 0.371 (0.236, 0.507) | 0.371 (0.235, 0.506) | 0.372 (0.236, 0.508) | 0.37 (0.235, 0.506) |
GCSE or equivalent | 0.405 (0.271, 0.538) | 0.405 (0.272, 0.539) | 0.406 (0.273, 0.539) | 0.404 (0.271, 0.537) |
Other qualification | 0.634 (0.451, 0.818) | 0.635 (0.451, 0.818) | 0.633 (0.45, 0.816) | 0.637 (0.454, 0.82) |
No qualifications | 0.942 (0.76, 1.124) | 0.942 (0.76, 1.124) | 0.945 (0.763, 1.126) | 0.947 (0.765, 1.129) |
Government Office Region (ref: London) | ||||
North East | −0.063 (−0.372, 0.245) | −0.062 (−0.371, 0.246) | −0.078 (−0.389, 0.233) | −0.046 (−0.356, 0.263) |
North West | 0.206 (−0.025, 0.437) | 0.209 (−0.022, 0.44) | 0.182 (−0.055, 0.419) | 0.226 (−0.007, 0.459) |
Yorkshire and The Humber | 0.108 (−0.136, 0.351) | 0.11 (−0.133, 0.353) | 0.086 (−0.162, 0.334) | 0.131 (−0.114, 0.377) |
East Midlands | 0.079 (−0.159, 0.316) | 0.082 (−0.155, 0.319) | 0.06 (−0.182, 0.302) | 0.11 (−0.13, 0.349) |
West Midlands | 0.298 (0.063, 0.532) | 0.3 (0.065, 0.534) | 0.272 (0.032, 0.511) | 0.315 (0.078, 0.552) |
East of England | 0.06 (−0.159, 0.28) | 0.064 (−0.155, 0.283) | 0.038 (−0.188, 0.263) | 0.085 (−0.137, 0.307) |
South East | −0.046 (−0.254, 0.163) | −0.043 (−0.251, 0.165) | −0.07 (−0.285, 0.144) | −0.021 (−0.232, 0.19) |
South West | 0.09 (−0.154, 0.335) | 0.093 (−0.151, 0.337) | 0.065 (−0.184, 0.314) | 0.11 (−0.136, 0.356) |
Wales | 0.335 (0.042, 0.627) | 0.334 (0.041, 0.627) | 0.316 (0.019, 0.612) | 0.349 (0.055, 0.643) |
Intercept | 9.511 (8.758, 10.264) | 9.361 (8.617, 10.106) | 9.442 (8.656, 10.228) | 9.294 (8.511, 10.078) |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Seo, J., Jivraj, S. Ethnic Density and Mental Health: Does it Matter Whether the Ethnic Density is Co-ethnic or Multi-ethnic and How Important is Change in Ethnic Density?. J. Racial and Ethnic Health Disparities (2024). https://doi.org/10.1007/s40615-024-02071-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-024-02071-4