Abstract
Purpose
While radiotherapy (RT) for head and neck cancer (HNC) has made recent strides, RT-induced vasculitis continues to adversely affect long-term patient outcomes. Guidelines for managing this complication remain scarce, supporting the need for a sensitive imaging modality in post-treatment evaluations. In this review, we discuss the current literature regarding 18F-fluorodeoxyglucose positron emission tomography (FDG-PET) and 18F-sodium fluoride (NaF-PET) in evaluating RT-induced vasculitis in HNC patients, highlighting several arenas of evolving clinical significance: (1) early recognition and standardized evaluation of RT-induced vasculitis, and (2) potential for a multifaceted diagnostic tool to stratify cardiovascular risk in HNC patients.
Methods
Numerous databases, including, but not limited to, Google Scholar and PubMed, were utilized to compile a body of literature regarding PET imaging of RT-induced vasculitis in HNC and related malignancies.
Results
Multiple studies have established the clinical capabilities of FDG-PET/computed tomography (FDG-PET/CT) for detection and management of RT-induced vasculitis in HNC patients, while NaF-PET/CT remains under investigation. Inflammatory vascular stages may be best analyzed by FDG-PET/CT, while vascular microcalcification and atherosclerotic disease may be supplementally assessed by the unique properties of NaF-PET/CT. With these modalities detecting primary stages of more detrimental vascular complications, PET imaging may carry several advantages over conventional, structural techniques.
Conclusion
FDG-PET/CT and NaF-PET/CT hold significant potential as preliminary diagnostic tools in monitoring early inflammation and atherosclerotic plaque development, warranting further research and attention. Applying these techniques in this context may foster proactive and consistent assessments of RT-induced vasculitis in HNC patients, mitigating potential cardiovascular risks through better-informed treatment decisions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
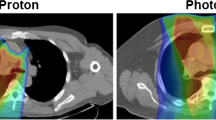
Head and neck cancers (HNC) exert an immense and devastating disease burden, with over 65,000 new Americans being affected annually [1]. Though this number is alarming, it is even more concerning that over half of post-treatment deaths are a result of complications, rather than caused by the cancer itself [2]. This group of malignancies includes tumors originating in the oral cavity, pharynx, larynx, paranasal sinuses or nasal cavity, and salivary glands, with head and neck squamous cell carcinoma (HNSCC) variants accounting for more than 90% of HNC tumors [1]. Photon radiotherapy (RT) along with combinations of chemotherapy or surgery are the recommended treatments for these patients, guided by disease site, stage, and pathologic reports [1, 3]. While intensity-modulated radiotherapy (IMRT) has made significant developments over the past few decades to better target radiation, properties of photon beams continue to include substantial exit doses, posing toxic effects to nearby healthy structures [4]. An alternative modality, proton RT, has demonstrated to deliver more focused, fewer, and lower doses of radiation, ultimately limiting the sequelae of inflammatory complications traditionally associated with photon RT [4, 5]. Although a detailed discussion on the merits of proton RT is beyond the focus of this review, this technique is quickly gaining clinical momentum and deserves further consideration as a treatment modality. In the realm of photon RT, the effects of head, neck, or mediastinal radiation often manifest as a heterogeneous group of cardiovascular complications, which include vasculitis, accelerated atherosclerosis of the irradiated arteries, as well as thrombolytic events, and can develop either acutely or delayed months to years after initial RT [3, 6,7,8,9,10]. Given the heterogeneity in clinical presentation, as well as the significant morbidity and mortality associated with these cardiovascular complications, there is an urgent need to improve management and refine guidelines pertaining to RT-induced vasculitis in HNC patients.
The extent of RT-induced vasculopathies is fundamentally dose-dependent, also being affected by tissue type and duration of radiation exposure [3, 7, 11]. The complex pathologic mechanism of RT-induced vascular injury involves the off-target damage of endothelial cells, disrupting vascular permeability and provoking oxidative damage of DNA through the formation of reactive oxygen species (ROS) [3, 6, 12]. This process is accompanied by a chronic inflammatory response involving macrophage infiltration and the release of proinflammatory cytokines such as interleukin (IL)-1, IL-6, tumor necrosis factor alpha (TNF-α), and interferon gamma (IFN-γ) [6, 7, 12]. An intricate network of interactions between these recruited cells ultimately leads to a prolonged state of inflammation and oxidative stress in the irradiated vessel, hindering endothelial healing and promoting further vulnerability to injury [13]. Through the subsequent aggregation of low-density lipoproteins (LDL) and the formation of lipid-laden macrophages (foam cells), atherosclerotic plaques are deposited and hold the capacity to enlarge or even rupture, giving rise to life-threatening cardiovascular complications [12, 13]. In light of this molecular mechanism, cellular inflammation and microcalcification are known to precede macroscopic vascular complications, which are commonly identified through the morphological extent of arterial stenosis and changes in arterial wall thickness (primarily intima media thickness) [14,15,16,17]. [Fig. 1—CT images denoting common carotid artery changes after RT]. However, at this point in the pathogenic process, the extent of vasculitis has already progressed considerably [14].
Measurements of pre- and postradiotherapy changes in the common carotid artery: vessel wall thickness, vessel area, and lumen area (A), calcification (B), and degree of stenosis (C) [18]
A systematic review by Gujral et al. exploring the effects of RT on the carotid arteries in HNC patients exemplifies the mechanistic link between RT-induced vascular injury and subsequent atherosclerotic plaque formation, reporting a significant and consistent increase in carotid intima media thickness and carotid artery stenosis when comparing irradiated and non-irradiated arteries [19]. Arterial stenosis, particularly of the carotid arteries, can lead to a range of debilitating effects, which may include fibrosis, necrosis, carotid blowout syndrome, and stroke with associated ischemic complications [2, 3, 8, 12, 20]. Several groups have highlighted the staggering risk of cerebrovascular events in HNC patients after receiving RT [9, 12, 21, 22]. A 2016 study analyzing 14,069 patients with HNSCC concluded that those treated with RT had a 70% increased risk of ischemic stroke, as compared to patients who received surgery alone [9]. [Fig. 2—Kaplan–Meier curve illustrating cerebrovascular mortality as a function of time]. A similar study examining 16,923 HNC survivors over 65 years of age also found a significantly elevated cerebrovascular mortality risk in cohorts receiving definitive RT alone, when compared to surgery and surgery/RT cohorts [21]. With these concerns in mind, there remains a dire need for proactive imaging of RT-induced vascular changes to limit subsequent complications and improve patient quality of life, as treatment of arterial stenosis can be difficult once progressed [2].
Stroke/stroke death cumulative incidence functions by radiation therapy alone and surgery alone [9]
Vasculopathies have been traditionally analyzed using a variety of non-invasive, structural imaging techniques, such as ultrasound, magnetic resonance (MR) imaging (MRI), MR angiography (MRA), computed tomography angiography (CTA), and conventional angiography [3, 8, 15, 16]. These techniques have their merits in distinguishing late-stage, morphologically visible changes (e.g., thickening of arterial walls, subsequent stenosis, and macrocalcifications), as well as evaluating the primary tumor site during pre-treatment imaging [1, 3, 5, 13, 15]. However, these modalities may fall short in detecting early microscopic and chemical evidence of vasculitis or atherosclerosis, as well as detecting vascular variations in smaller vessels [13,14,15,16,17, 23]. The use of these imaging techniques also proves to be challenging when differentiating between residual, chronic disease and RT-induced changes, due to difficulty delineating between normal and abnormal tissue structure [8, 20, 23]. While these anatomic imaging modalities may have a role during tumor staging and certain stages of HNC treatment progression, an in-depth discussion of their clinical capacities is beyond the scope of this review. Rather, we aim to review the recent literature on the use of 18F-fluorodeoxyglucose (FDG)-positron emission tomography (PET)/CT and 18F-sodium fluoride (NaF)-PET/CT in proactively evaluating RT-induced vasculitis in patients with HNC, focusing upon several areas with emerging clinical relevance: (1) early recognition and standardized evaluation of RT-induced vasculitis, and (2) potential for a multifaceted diagnostic tool to stratify cardiovascular risk in HNC patients.
FDG-PET/CT and NaF-PET/CT
PET is a robust, non-invasive imaging technique with the capacities to detect molecular and physiological changes. FDG, the most frequently employed tracer used in PET scanning, is a radiolabeled glucose analog taken up by cells with increased metabolic activity and glucose consumption [5, 13]. FDG-PET, commonly fused together with CT or MRI, has been traditionally used for staging and restaging of malignancy (due to the metabolic needs and higher rates of glucose uptake seen by many cancerous cells), as well as assessment of inflammation and infection [5, 8, 15, 24]. However, there is an overwhelming body of evidence that demonstrates the emerging clinical utility and accuracy of FDG-PET/CT in detecting areas of inflammation across multiple body systems [5, 7, 8, 13,14,15, 24,25,26]. In the framework of therapy-induced vasculitis, increased FDG uptake in the vessels of interest is analyzed using visual or semi-quantitative methods, commonly defined by standard uptake values (SUV) or target-to-background ratios (TBR), and has been demonstrated by several groups to correspond to the degree of macrophage infiltration and vascular inflammation [3, 7, 8, 13, 15, 25,26,27]. [Fig. 3—Illustrative figure of vascular FDG uptake].
Sagittal imaging of the left carotid artery before and during cisplatin-based CCRT. Images from left to right: co-registered computed tomography (CT), 18F-fluorodeoxyglucose (FDG) positron emission tomographic (PET), fused PET/CT, and focally magnified images of the left carotid artery (frames) from PET/CT fusion scan. a Indicates images before CCRT and b represents images during CCRT. Arrows indicate areas of inhomogenously increased vascular FDG uptake after concurrent chemo-radiotherapy (CCRT) [27]
Images from left to right: co-registered computed tomography (CT), 18F-fluorodeoxyglucose (FDG) positron emission tomographic (PET), fused PET/CT, and focally magnified images of the left carotid artery (frames) from PET/CT fusion scan. (A) Indicates images before CCRT and (B) represents images during CCRT. Arrows indicate areas of inhomogenously increased vascular FDG uptake after concurrent chemo-radiotherapy (CCRT) [27].
18F-sodium fluoride (NaF) is a more recently utilized and relatively unexplored tracer in the realm of PET cardiovascular imaging, traditionally used in the management of metastatic bone cancer [13]. Combined with CT, NaF-PET/CT may hold clinical potential from an alternative mechanism in managing treatment-related vascular complications in HNC patients. While FDG uptake denotes inflammatory processes, NaF uptake signifies areas of microcalcification and has the emerging potential to assess early atherosclerotic developments through visualization of active plaque deposition [13, 23, 28]. [Fig. 4—Demonstrative figure of NaF uptake in active calcification in carotid artery plaque]. These findings have been largely validated within animal studies, and multiple studies have demonstrated the correlation of NaF uptake with aging and various cardiovascular risk factors [13, 17, 23, 28]. Despite these hopeful outlooks, the clinical value of this tracer to evaluate RT-induced vascular complications has yet to be thoroughly defined.
18 F-NaF uptake encompasses a greater region than calcific nodules within plaque (left) [29]
Although a variety of molecular tracers have been developed to support PET imaging capabilities, FDG-PET/CT shows favorable potential for use in cardiovascular risk management of HNC patients. In regards to NaF-PET/CT, given its success in detecting and characterizing atherosclerotic microcalcifications in other patient populations, it is anticipated to have similar utility in assessing atherosclerosis exacerbated by exposure to RT and warrants further investigation. Legitimate concerns of this imaging technique involve challenges distinguishing lesion versus background uptake (spillover) and decreased spatial resolution due to vascular wall motion, as well as cardiac and respiratory movements during imaging [14, 15, 17]. Recognizing these possible limitations, some have argued that utilizing global assessment methods may overcome some of these concerns, holding the potential to better characterize the extent of disease activity throughout the body [5, 8, 13, 30]. In this methodology, the uptake measurements include the whole region of interest (ROI), with ROIs along the entire length of an organ and lesion factored into a composite global disease score. Thus, the global disease measurement reflects the total disease burden [31]. Weighing these limitations with the potential advantages of this technique, we aim to summarize the current literature regarding RT-induced vascular injury and unpack the clinical utility of PET/CT in HNC management.
Early recognition and standardized evaluation of RT-induced vasculitis
While the use of FDG-PET/CT to monitor residual cancer at 3 months after RT completion is the current standard of care, the timely monitoring of vascular complications after photon RT completion remains largely undefined [1, 7, 11, 20, 26]. Considering the risks associated with late-stage vasculitis in HNC patients as discussed previously, early implementation of FDG-PET/CT to detect sub-acute vascular injury may hold the potential to mitigate further damage by allowing vigilant monitoring of injury progression and has been demonstrated to detect primary, molecular stages of inflammation [8, 14, 15, 25, 26]. With many of these studies noting an increase in vascular FDG uptake as early as three months post-RT, incorporation of FDG-PET/CT for vascular diagnostic purposes may seamlessly integrate into clinical evaluations of at-risk patients, fundamentally aligning with PET/CT imaging of cancer assessment itself.
Not only may early vascular monitoring allow for more effective treatment planning, but the quantifiable nature associated with FDG-PET/CT and NaF-PET/CT may prove valuable in refining HNC patient care across healthcare providers. RT-induced vasculitis continues to be a poorly recognized and managed complication, with treatment choices remaining a case-by-case, individualized decision [11]. The clinical usefulness of FDG-PET/CT has been widely established for other purposes, but FDG uptake analysis in regards to treatment-induced vasculopathies remains as relatively uncharted territory [7, 8]. Several pioneering groups have worked to demonstrate the use of FDG-PET/CT in quantifying intravascular inflammation after photon RT [8, 15, 25, 26]. A 2019 prospective study by Chen et al. that assessed carotid artery inflammation in 22 HNC patients pre-RT and 3 months post-RT demonstrated a significant increase in multiple FDG uptake parameters, including TBRmax (p = 0.0001), TBRmean (p = 0.0001), and partial volume corrected SUVmean (p = 0.002) [26]. Borja et al. assessed global FDG uptake in 30 HNC patients at these same time points and found a significant increase in average SUVmean in the left common carotid (p = 0.0004) and arch of aorta (p = 0.004) [8]. Another group that analyzed ten lymphoma survivors who had received unilateral RT 2–7 years earlier to either the carotid artery (eight patients) or internal iliac artery (two patients) found the highest FDG uptake in the artery of the irradiated side when compared to the non-irradiated side (p = 0.04) [15]. [Fig. 5—FDG-PET/CT image of non-irradiated and irradiated carotid artery].
Representative FDG-PET/CT from irradiated (arrow) and non-irradiated (arrowhead) carotid artery. The left panel shows the contrast enhanced CT and the right panel shows the FDG-PET fused with the CT [15]
This association between increased FDG uptake and inflammation within affected vasculature has been further validated in similar studies analyzing other cancer types in nearby mediastinal regions, as well as within additional tissues types of HNC patients. A 2019 study by Jahangiri et al. that examined the ascending aorta and aortic arch of 45 non-small cell lung carcinoma patients noted a statistically significant increase in intravascular average SUVmean when comparing FDG-PET/CT results from before and after photon radiotherapy [25]. Another group analyzing the parotid gland of 47 HNC patients before and 3 months after photon RT also found a significant increase in average SUVmean (p < 0.05), further highlighting the presence of treatment-induced inflammation [5].
Comprehensively, these studies emphasize the recurring capacity of FDG-PET/CT to objectively quantify RT-induced inflammation, supporting its potential role in fostering uniform clinical judgements. While these findings are beginning to show consistency in a growing body of literature, there continues to remain a gap in regards to the proper clinical management of RT-related vascular toxicities [7]. Utilization of FDG-PET/CT to guide screening and assessment of RT-induced vasculitis may provide an avenue for a more standardized methodology of HNC care, warranting further study and consideration by physicians [11].
Potential for a multifaceted diagnostic tool to stratify cardiovascular risk in HNC patients
While FDG-PET/CT and NaF-PET/CT may show promise as individual entities, the question arises as to whether the use of these two PET modalities together may serve value in overall cardiovascular risk assessment of HNC patients after RT completion. Recent literature has highlighted a wide gap in the arena of identifying patients at-risk of developing cardiovascular complications, which deserves clinical attention [2, 8, 32, 33]. A 2021 cross-sectional study of over 90,000 US Veterans with prostate cancer reported a staggeringly high incidence of underassessment and unmanaged comprehensive care concerning cardiovascular risk factors, highlighting the pre-existing vulnerability of cancer patient populations for cardiac events, prevalent even before potential post-treatment complications (such as those from RT) may arise [32]. Cancer shares many mechanistic pathways with the development of atherosclerosis, such as changes in integrin/cadherin activity and G1/S checkpoint [27, 34]. Recognizing this significant comorbidity, utilization of PET/CT to identify sub-acute microcalcification and atherosclerotic lesions in cancer patients may further inform and improve upon anti-atherosclerotic efforts [34].
A 2017 study on squamous cell carcinoma of HNC patients treated with RT or chemo-radiotherapy reported similar results, noting these patients were at high risk for cardiovascular disease, yet received poor preventative care to minimize these risks [2]. In the context of HNC, PET/CT may represent a powerful means to better inform proper cardiovascular risk assessment during RT treatment progression, ultimately improving long-term patient outcomes.
Many have specifically brought attention to the emerging role of NaF-PET/CT in illustrating the relationship between increased NaF vascular uptake and unfavorable cardiovascular risk profiles [7, 13, 17, 23, 28, 33, 35]. Castro et al. analyzed NaF uptake in the left common carotid artery of 128 patients and found a significant increase in average SUVmax in patients with increased cardiovascular and thromboembolic risk profiles, while noting a significant decrease in those with higher levels of physical activity [23]. Another study by Blomberg et al. found that cardiovascular disease risk was increased by 3.7 times in patients with elevated thoracic aorta NaF uptake, aligning with calcium scores denoted by CT [33]. These findings suggest that vascular microcalcification and atherosclerotic disease burden may be best assessed by the unique properties of NaF-PET/CT, while inflammatory vascular stages may be supplementally analyzed by FDG-PET/CT, as discussed previously [13, 17, 23, 28, 33, 35]. Noting the differing molecular targets of each of these tracers within vasculopathy progression, the use of FDG- and NaF-PET/CT as preliminary diagnostic tools may be well suited to delineate between vasculitis and vasculitis with superimposed atherosclerosis [13]. Although an in-depth comparison between these two techniques is beyond the scope of this review, the clinical relevance of NaF-PET is rapidly emerging. Acknowledging that the capabilities of NaF-PET/CT in detecting microcalcification have largely shown promise in other domains, it warrants the attention of larger prospective studies as to whether similar efficacy may be seen in the framework of RT-induced vascular complications in HNC patients. However, an approach that encompasses the strengths of both modalities may provide insight in monitoring early inflammation and atherosclerotic plaque progression in HNC patients, ultimately shedding light on cardiovascular risk planning as a whole [7].
Conclusion
Although radiotherapy has made meaningful advancements in the realm of oncology, the significant morbidity and mortality associated with post-treatment cardiovascular complications in head and neck cancer patients is a cause for concern. Numerous studies have confirmed the clinical capabilities of FDG-PET/CT for the detection and management of photon RT-induced vasculitis in HNC patients, while the role of NaF-PET/CT remains relatively unexplored in this domain. However, this technique does show potential based on data in neighboring clinical fields. Guidelines for managing RT-induced vascular injuries remain scarce, supporting the need for a sensitive imaging modality in post-treatment evaluations. On a molecular level, FDG-PET/CT may be useful in detecting primary stages of vascular inflammation, while NaF-PET/CT may be important in highlighting microcalcification and atherosclerotic plaque deposition. With these microscopic processes representing the primary stages of more detrimental vascular complications, the use of this technology may hold several advantages over traditional, structural techniques. Not only may FDG-PET/CT and NaF-PET/CT support the prompt discovery of RT-induced vasculitis, but they may also have the potential to foster consistent treatment decisions through the use of quantifiable measures. An approach emphasizing the strengths of both molecular tracers may hold clinical value in cardiovascular risk analysis, ultimately improving long-term outcomes in HNC patients. Though future studies are still needed to validate these clinical possibilities, we believe that FDG-PET/CT and NaF-PET/CT may show evolving potential for early and standardized assessment of RT-induced vasculitis in HNC patients, mitigating future cardiovascular risks through better-informed care and treatment planning improvements.
References
Pfister DG, Spencer S, Adelstein D, Adkins D, Anzai Y, Brizel DM et al (2020) Head and neck cancers, Version 2.2020, NCCN clinical practice guidelines in oncology. J Natl Comp Cancer Netw 18:873–898. https://doi.org/10.6004/jnccn.2020.0031
Okoye CC, Bucher J, Tatsuoka C, Parikh SA, Oliveira GH, Gibson MK et al (2017) Cardiovascular risk and prevention in patients with head and neck cancer treated with radiotherapy. Head Neck 39:527–532. https://doi.org/10.1002/hed.24646
Leboucher A, Sotton S, Gambin Flandrin I, Magné N (2022) Head and neck radiotherapy-induced carotid toxicity: pathophysiological concepts and clinical syndromes. Oral Oncol 129:105868. https://doi.org/10.1016/j.oraloncology.2022.105868
Mohamed N, Lee A, Lee NY (2022) Proton beam radiation therapy treatment for head and neck cancer. Precis Radiat Oncol 6:59–68. https://doi.org/10.1002/pro6.1135
Mouminah A, Borja AJ, Hancin EC, Chang YC, Werner TJ, Swisher-McClure S et al (2020) 18F-FDG-PET/CT in radiation therapy-induced parotid gland inflammation. Eur J Hybrid Imaging 4:22. https://doi.org/10.1186/s41824-020-00091-x
Donnellan E, Phelan D, Mccarthy CP, Collier P, Desai M, Griffin B (2016) Radiation-induced heart disease: a practical guide to diagnosis and management. Cleve Clin J Med 83:914–922. https://doi.org/10.3949/ccjm.83a.15104
Dreyfuss AD, Jahangiri P, Simone CB, Alavi A (2020) Evolving role of novel quantitative PET techniques to detect radiation-induced complications. PET Clin 15:89–100. https://doi.org/10.1016/j.cpet.2019.08.003
Borja AJ, Hancin EC, Dreyfuss AD, Zhang V, Mathew T, Rojulpote C et al (2020) F-FDG-PET/CT in the quantification of photon radiation therapy-induced vasculitis. Am J Nucl Med Mol Imaging 10:66–73
Arthurs E, Hanna TP, Zaza K, Peng Y, Hall SF (2016) Stroke after radiation therapy for head and neck cancer: what is the risk? Int J Radiat Oncol Biol Phys 96:589–596. https://doi.org/10.1016/j.ijrobp.2016.07.007
Kaghazchi F, Borja AJ, Hancin EC, Bhattaru A, Detchou DKE, Seraj SM et al (2021) Venous thromboembolism detected by FDG-PET/CT in cancer patients: a common, yet life-threatening observation. Am J Nucl Med Mol Imaging 11:99–106
Twitchell S, Karsy M, Guan J, Couldwell WT, Taussky P (2019) Sequelae and management of radiation vasculopathy in neurosurgical patients. J Neurosurg 130:1889–1897. https://doi.org/10.3171/2017.12.JNS172635
Venkatesulu BP, Mahadevan LS, Aliru ML, Yang X, Bodd MH, Singh PK et al (2018) Radiation-induced endothelial vascular injury. JACC Basic Transl Sci 3:563–572. https://doi.org/10.1016/j.jacbts.2018.01.014
McKenney-Drake ML, Moghbel MC, Paydary K, Alloosh M, Houshmand S, Moe S et al (2018) 18F-NaF and 18F-FDG as molecular probes in the evaluation of atherosclerosis. Eur J Nucl Med Mol Imaging 45:2190–2200. https://doi.org/10.1007/s00259-018-4078-0
Liddy S, Mallia A, Collins CD, Killeen RP, Skehan S, Dodd JD et al (2020) Vascular findings on FDG PET/CT. Br J Radiol. https://doi.org/10.1259/bjr.20200103
Ripa RS, Mette Hag A, Knudsen A, Loft A, Specht L, Kjaer A (2015) F-FDG PET imaging in detection of radiation-induced vascular disease in lymphoma survivors. Am J Nucl Med Mol Imaging 5:408–415
Agarwal A, Bathla G, Kanekar S (2020) Imaging of Non-atherosclerotic Vasculopathies. J Clin Imaging Sci 10:62. https://doi.org/10.25259/JCIS_91_2020
Moghbel M, Al-Zaghal A, Werner TJ, Constantinescu CM, Høilund-Carlsen PF, Alavi A (2018) The role of PET in evaluating atherosclerosis: a critical review. Semin Nucl Med 48:488–497. https://doi.org/10.1053/j.semnuclmed.2018.07.001
Kim BJ, Kang HG, Lee S, Jung J, Lee M-H, Kang D-W et al (2018) Changes in the common carotid artery after radiotherapy: wall thickness, calcification, and atherosclerosis. J Clin Neurol 14:35. https://doi.org/10.3988/jcn.2018.14.1.35
Gujral DM, Chahal N, Senior R, Harrington KJ, Nutting CM (2014) Radiation-induced carotid artery atherosclerosis. Radiother Oncol 110:31–38
Rohde M, Nielsen AL, Pareek M, Johansen J, Sørensen JA, Diaz A et al (2019) PET/CT versus standard imaging for prediction of survival in patients with recurrent head and neck squamous cell carcinoma. J Nucl Med 60:592–599. https://doi.org/10.2967/jnumed.118.217976
He Q-S, Wang Z-P, Li Z-J, Zhou P, Lian C-L, Wu S-G et al (2021) Increased risk of cerebrovascular mortality in head and neck cancer survivors aged ≥ 65 years treated with definitive radiotherapy: a population-based cohort study. Radiat Oncol 16:185. https://doi.org/10.1186/s13014-021-01913-3
Huang Y-S, Lee C-C, Chang T-S, Ho H-C, Su Y-C, Hung S-K et al (2011) Increased risk of stroke in young head and neck cancer patients treated with radiotherapy or chemotherapy. Oral Oncol 47:1092–1097. https://doi.org/10.1016/j.oraloncology.2011.07.024
Castro SA, Muser D, Lee H, Hancin EC, Borja AJ, Acosta O et al (2021) Carotid artery molecular calcification assessed by [18 F]fluoride PET/CT: correlation with cardiovascular and thromboembolic risk factors. Eur Radiol 31:8050–8059. https://doi.org/10.1007/s00330-021-07917-7
Mahne A, El-Haddad G, Alavi A, Houseni M, Moonis G, Mong A et al (2007) Assessment of age-related morphological and functional changes of selected structures of the head and neck by computed tomography, magnetic resonance imaging, and positron emission tomography. Semin Nucl Med 37:88–102. https://doi.org/10.1053/j.semnuclmed.2006.10.003
Jahangiri P, Kalboush E, Pournazari K, Seraj SM, Neamaalla S, Werner T et al (2019) The Utility of FDG-PET/CT for quantifying radiation-induced vasculitis. J Nucl Med 60:1345
Chen X, Zheng Y, Tatsuoka C, Muzic RF, Okoye CC, O’Donnell JK et al (2019) Chemoradiotherapy-related carotid artery inflammation in head and neck cancer patients quantified by [18F]FDG PET/CT. Oral Oncol 93:101–106. https://doi.org/10.1016/j.oraloncology.2019.04.008
Wang Y-C, Hsieh T-C, Chen S-W, Yen K-Y, Kao C-H, Chang K-C (2013) Concurrent CHEMO-RADIOTHERAPY POTENTIATES VASCULAR Inflammation. JACC Cardiovasc Imaging 6:512–514. https://doi.org/10.1016/j.jcmg.2012.06.017
Castro S, Muser D, Acosta-Montenegro O, Emamzadehfard S, Pourhassan Shamchi S, Desjardins B et al (2017) Common carotid artery molecular calcification assessed by F-NaF PET/CT is associated with increased cardiovascular disease risk: results from the CAMONA study. J Nucl Med 58:34
Cocker MS, Spence JD, Hammond R, Wells G, deKemp RA, Lum C et al (2017) [18 F]-NaF PET/CT identifies active calcification in carotid plaque. JACC Cardiovasc Imaging 10:486–488. https://doi.org/10.1016/j.jcmg.2016.03.005
Høilund-Carlsen PF, Edenbrandt L, Alavi A (2019) Global disease score (GDS) is the name of the game! Eur J Nucl Med Mol Imaging 46:1768–1772. https://doi.org/10.1007/s00259-019-04383-8
Høilund-Carlsen PF, Piri R, Gerke O, Edenbrandt L, Alavi A (2021) Assessment of total-body atherosclerosis by PET/computed tomography. PET Clin 16:119–128. https://doi.org/10.1016/j.cpet.2020.09.013
Sun L, Parikh RB, Hubbard RA, Cashy J, Takvorian SU, Vaughn DJ et al (2021) Assessment and management of cardiovascular risk factors among US veterans with prostate cancer. JAMA Netw Open. https://doi.org/10.1001/jamanetworkopen.2021.0070
Blomberg BA, de Jong PA, Thomassen A, Lam MGE, Vach W, Olsen MH et al (2017) Thoracic aorta calcification but not inflammation is associated with increased cardiovascular disease risk: results of the CAMONA study. Eur J Nucl Med Mol Imaging 44:249–258. https://doi.org/10.1007/s00259-016-3552-9
Raynor WY, Borja AJ, Zhang V, Kothekar E, Lau HC, Ng SJ et al (2022) Assessing coronary artery and aortic calcification in patients with prostate cancer using 18F-Sodium Fluoride PET/computed tomography. PET Clin 17:653–659. https://doi.org/10.1016/j.cpet.2022.07.009
Borja AJ, Rojulpote C, Hancin EC, Høilund-Carlsen PF, Alavi A (2020) An update on the role of total-body PET imaging in the evaluation of atherosclerosis. PET Clin 15:477–485. https://doi.org/10.1016/j.cpet.2020.06.006
Funding
Open access funding provided by University of Oslo (incl Oslo University Hospital).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Ethics approval
This articles does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Delman, A., Griffin, M.T., Werner, T.J. et al. The emerging role of positron emission tomography (PET) in the management of photon radiotherapy-induced vasculitis in head and neck cancer patients. Clin Transl Imaging 11, 157–164 (2023). https://doi.org/10.1007/s40336-023-00541-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40336-023-00541-z