Abstract
Background
In the Middle East and North Africa (MENA) the scarcity of local cost data is a key barrier to conducting health economic evaluations. We systematically reviewed reports of disease-related costs from MENA and analysed their transferability within the region.
Methods
We searched PubMed and included full text English papers that reported disease-related costs from the local populations of Algeria, Bahrain, Egypt, Iraq, Jordan, Saudi Arabia, Kuwait, Lebanon, Libya, Morocco, Oman, Palestine, Qatar, Syria, Tunisia, United Arab Emirates and Yemen between 1995 and 2019. Screening, study selection and data extraction were done in duplicate. Study-related variables, costing methods, all costs and their characteristics were extracted and analysed via descriptive methods. From multi-country studies of MENA employing homogenous costing methods, we estimated the ratio (cost transfer coefficient) between the relative differences in direct medical costs and macroeconomic indicators via robust regression. We predicted each cost via the estimated cost transfer formula and evaluated prediction error between true and predicted (transferred) costs.
Results
The search yielded 1646 records, 206 full text papers and 3525 costs from 84 diagnoses. Transferability was analysed involving 144 direct medical costs from eight multi-country studies. Adjusting the average of available foreign costs by 0.28 times the relative difference in GDP per capita provided the most accurate estimates. The correlation between true and predicted costs was 0.96; 68% of predicted costs fell in the true ± 50% range. Predictions were more accurate for costs from studies that involved the largest number of countries, for countries outside the Gulf region and for drug costs versus unit or disease costs.
Conclusion
The estimated cost transfer formula allows the prediction of missing costs in MENA if only GDP per capita is available for adjustment to the local setting. Input costs for the formula should be collected from multiple sources and match the decision situation.
Plain Language Summary
In the Middle East and North Africa (MENA) scarce local cost data hinder health economic evaluations. This systematic review summarized disease-related costs from 17 countries (Algeria, Bahrain, Egypt, Iraq, Jordan, Saudi Arabia, Kuwait, Lebanon, Libya, Morocco, Oman, Palestine, Qatar, Syria, Tunisia, United Arab Emirates and Yemen). Eight studies applied the same costing method across multiple countries. We used these data to estimate a formula for transferring costs between countries. We assumed that costs vary proportionally with gross domestic product per capita (GDP). Most accurate cost predictions were provided when relative cost differences were set to 0.28-times the relative differences in GDP per capita. The correlation between transferred and true costs was very high. Still, only 68% of transferred costs fell in the true ± 50% range. Cost estimates were more accurate if costs were transferred from multiple countries. Also, estimates were more accurate for countries outside the Gulf region and for drug costs when compared to unit- or disease costs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Between MENA countries, disease-related costs vary less than GDP per capita. Cost differences between countries were proportional to 0.28-times the differences in GDP per capita. When only GDP-based adjustments are feasible, for most accurate predictions, transferred costs should be adjusted by this factor. |
68% of such estimates fell in the true cost ± 50% range. Therefore, wide error margins should be applied in sensitivity analysis. |
Predictions were more accurate if costs were available from multiple countries, if predictions were made for non-Gulf countries and for drug costs versus unit or disease costs. |
1 Introduction
Depending on the definition, the Middle East and North Africa (MENA) region includes 19–35 countries, including some of the wealthiest and poorest in the world, comprising up to 6% of the global population and 4.5% of the global economy [1,2,3]. In the past decade, MENA countries have made substantial progress in improving their health systems and enhancing the health outcomes of their populations. However, the structure and financing of healthcare systems is rather heterogenous in the region. While high-income countries maintain state-of the art hospitals and universal coverage, lower income countries in the region are struggling to build their healthcare systems [4]. Overall, in most MENA countries, the proportion of GDP spent on healthcare is below the global average and the share of out-of-pocket spending within total health expenditure exceeds the global average [5].
Health technology assessment (HTA) is “a multidisciplinary process that uses explicit methods to determine the value of a health technology at different points in its lifecycle [6]”. As a means to inform decision making in order to promote equitable, efficient, and high-quality health systems [6], HTA has been recognized as an important tool in the pursuit of universal health coverage and sustainable healthcare financing worldwide [7]. In MENA, despite the growing interest from countries, the implementation of HTA is still in its early stage [8]. Health economic evaluations in MENA have been systematically reviewed in multiple studies [9,10,11,12,13]. In addition to limited funding as well as organizational and human resource barriers, a commonly cited constraint to the implementation of HTA in the region is the limited availability of relevant local data on costs and outcomes [9, 10, 12,13,14].
In the context of health economic evaluations, transferability generally refers to the feasibility of adjustments both for varying location/country-specific input parameters, and decision-maker-specific methodological requirements that provide valid estimates for a specific country using foreign studies when local studies are lacking [15,16,17]. Clinical outcomes are usually transferable between countries. However, the transferability of cost data is challenging due to the significant inter-country variability in demography, epidemiology, economic performance, healthcare systems, unit costs, financing mechanisms and healthcare practice patterns [15, 16, 18]. In general, the more detailed and transparent the reporting, the more likely that results of health economic evaluations can be transferred internationally [19, 20]. As such, several studies have explored the transferability of costs between jurisdictions [21,22,23,24,25]. Despite being a crucial aspect for the development of HTA in MENA, the transferability of costs within the region has not yet been systematically studied.
Therefore, this systematic review was undertaken to identify studies that report disease-related costs from MENA [26]. We describe the published costs and estimate a cost transfer formula that allows the prediction of missing direct medical costs using macroeconomic indicators. Finally, we analyse the prediction accuracy for transferred costs.
2 Methods
2.1 Systematic Review
A systematic review was conducted for the identification of publications reporting disease-related costs from the 17 selected countries, which were listed in at least six of seven MENA definitions[26]: Algeria, Bahrain, Egypt, Iraq, Jordan, Saudi Arabia, Kuwait, Lebanon, Libya, Morocco, Oman, Palestine, Qatar, Syria, Tunisia, United Arab Emirates (UAE) and Yemen. For the analysis of cost transferability, we selected the subset of articles that reported the same costs from multiple MENA countries as described below. The PRISMA guidelines were followed when reporting results [27] (Online Supplementary Material (OSM) File 1, Table S1). No ethics approvals were needed for the study.
A literature search in PubMed database was carried out up to 15 December 2019 using the filter of English language and full-text journal articles and combining the countries as well as the list of keywords related to general descriptions, key methods and main outcomes of health economic analysis. The detailed search strategy is included in OSM File 1 (Table S2).
Abstracts and titles were screened for eligibility by two independent researchers, discrepancies were resolved by consensus. English language full-text articles of original research on humans were eligible for our review if the studies concerned the local population of the respective MENA countries, and costs were reported in monetary units between 1995 and 2019. In addition, we identified four systematic reviews of health economic studies from MENA and included eligible studies from their reference lists. Full text articles were checked against the predefined eligibility criteria by six pairs of four independent researchers, who made decisions upon mutual agreement in case of any arising differences.
2.2 Data Extraction
A Microsoft Excel spreadsheet was developed for data extraction according to predefined criteria. Data extraction was performed in parallel by six pairs of four independent researchers. All entries were cross-checked, and differences were resolved in a multi-phase process. First, each researcher extracted data from articles assigned to them, then results were cross-checked by a second reviewer and differences were resolved by consensus during regular group meetings under the supervision of two senior researchers. From each publication, the first author, publication year, and the target country and all costs were extracted. We recorded the type of economic analysis and the study perspective, based on the authors’ description or the best judgement of reviewers. For each cost, the disease area, intervention as well as the year of cost collection, currency, number of patients, and the discount rate were extracted. We assigned the International Classification of Diseases and Related Health Problems 10th Revision (ICD-10) chapter and diagnosis code to each cost [28]. We also mapped each diagnosis to disease categories of the Global Burden of Disease report for the region [29]. Furthermore, the healthcare setting, the main cost categories, the sources of cost data, the methods of primary studies and sources of secondary data were recorded. The predefined extraction sheet was piloted on a limited number of articles (five articles by each researcher pair; 30 in total) and refined thereafter. Detailed definitions of the variables are provided in OSM File 1 (Table S3).
2.3 Analysis of the Transferability of Costs in Multi-Country Studies
2.3.1 Assumptions
Although many factors influencing transferability have been identified [16, 17, 22], when imputing missing costs in a data-scarce setting, adjustments may only be feasible based on a limited number of available parameters. Motivated by the rapid de facto HTA assessments applied for Eastern Europe and other resource-limited settings [18, 30, 31], we assumed that missing costs can be imputed after adjusting only for a single macroeconomic indicator, such as gross domestic product per capita (GDPpc), total health expenditure per capita (THEpc) or governmental health expenditure per capita (GHEpc). To emphasize the use of per capita values, macroeconomic indicators are denoted as MIpc. We assumed that within the region, the relative differences of costs between countries (RDCost) are proportional to relative differences in macroeconomic indicators (RDMIpc) to a factor βMI, denoted as the cost transfer coefficient for a given macroeconomic indicator. This assumption is formally written as:
Eq. (1) can be expanded as follows:
where the left side of the equation is the relative difference of costs, and the right side is the relative difference in the macroeconomic indicators, multiplied by the cost transfer coefficient (i.e., the factor of proportionality). To eliminate the variability caused by different costing methods [32], we calculated relative differences of costs from studies, which measured the same cost in multiple MENA countries and applied the same costing methodology in the same costing year. Such costs are denoted as Costx. In Eq. (2) Costx,i denotes Costx measured in country i and \(\overline{Cost}_{x,j \ne i}\) denotes the mean of Costx for all countries where it was reported, except country i. With similar indexing, \(MIpc_{x,i}\) denotes the per-capita macroeconomic indicator measured in purchase-parity international dollars (PPP$) in country i in the costing year of Costx where MIpc can be replaced by GDPpc, THEpc and GHEpc. The error term is ε. The respective cost transfer coefficients are denoted by βGDP, βTHE and βGHE.
2.3.2 Assessing the Quality of Reporting
For the studies included in transferability analysis, one reviewer evaluated the transparency of reporting according to the transferability evaluation criteria proposed by Fukuda et al. [25]. Reporting transparency ensures that researchers can judge the potential applicability of a given cost for their own economic analysis. Level A denotes a full reporting of resource use and unit costs for all cost components. Level B denotes that all cost components are separately reported. Level C denotes that cost components are listed but not reported separately, and Level D describes the scope of costing but included cost components are not listed.
2.3.3 Input Variables
We included direct healthcare costs reported for a single patient if both costs and macroeconomic indicators were available from at least two countries. Population costs involving inputs from epidemiological data or treatment effects were excluded. By their level of aggregation, costs were categorised as drug, unit or disease costs [24]. All costs were reported in current US$ or PPP$ except one study, where local currency was transferred to US$ by the exchange rate of the costing year provided by the authors [33]. Following Eq. (2), we calculated the relative differences for each country-level cost versus the mean of the same cost measured in other countries. We also calculated the relative differences of GDPpc, THEpc and GHEpc using World Bank purchase power parity international dollars (PPP$) data, if available [2]. We applied the skewness-kurtosis test [34] to explore the distributional properties of the relative difference values.
2.3.4 Estimating Cost Transfer Coefficients
Following Eq. (1), we estimated the cost transfer coefficient from the relative differences of costs and macroeconomic indicators via simple regression without intercept. We used robust regression models, which are less sensitive to outliers than ordinary least squares (OLS) regression, providing more precise fit on the majority of data points while allowing greater errors for outliers [35]. First, we applied an M-estimator with iteratively reweighted least squares [35, 36]. Second, we used quantile regression, which estimates the conditional median of the dependent variable. Third, we applied interval regression, which estimates parameters by assuming that values of the dependent variable fall anywhere between a lower and an upper limit [37]. We estimated the cost transfer coefficient by setting the interval limits to true cost ± 30% (see below). We emphasize that cost transfer coefficient estimates apply only to situations where costs are collected with the same methods in the same costing year in multiple countries.
By rewriting Eq. (1), the missing cost for a country can be predicted by the following cost transfer formula:
Where \(\widehat{{{\text{Cos}} t}}_{x,i}\) denotes the predicted cost. Equation (2) suggests that if β = 0 (i.e., costs do not vary with the macroeconomic indicator), then \(\widehat{{{\text{Cos}} t}}_{x,i} = \widehat{{{\text{Cos}} t}}_{x,j \ne i}\) and the missing cost could be imputed using the mean of available costs from other MENA countries (given that costs were measured by the same method in the same costing year). If β = 1, costs vary to the same extent as macroeconomic indicators. We formally tested both hypotheses, whether the estimated cost transfer coefficients are different from 0 (t-test) or from 1 (Wald-test).
2.3.5 Evaluation of the Prediction Accuracy for Transferred Costs
To evaluate the accuracy predictions that is unaffected by the magnitude of costs, we calculated Pearson correlation coefficients, and mean relative error (MRE) values between predicted and actual costs. For MRE we applied the following formula, where Costi represents the true value and \(\widehat{{Cost}_{i}}\) the predicted value of cost i.
Furthermore, we calculated the percentage of cost estimates falling in an acceptable tolerance range. Although we are not aware of established standards for the accuracy of cost estimates in healthcare, we applied standards used in industrial engineering and public planning. Class 5 and Class 4 estimates are rough cost estimates prepared from limited information during project initiation for purposes such as screening or the evaluation of economic or technical feasibility [38, 39]. Following these benchmarks, we evaluated the proportion of predicted costs falling in true cost ± 50% and ± 30% ranges.
2.3.6 Evaluation of the Determinants of Transferability
As robust regression methods are resistant to outliers, the prediction errors of robust regression are useful for the detection of outliers (i.e., costs that cannot be predicted with reasonable accuracy via the cost transfer formula) [40]. We used relative errors (REs) for each cost as a measure of transferability. From Eq. (3), the relative error for cost I is calculated by the following formula:
Greater RE values indicate less accurate cost estimates (and hence, less transferability). We used ordinary least squares (OLS) regression analysis on log transformed RE values to explore the determinants of transferability, such as the relative difference in macroeconomic indicators, country, study, and the level of aggregation of costs. All calculations were performed using Stata 17 statistical software [41].
3 Results
3.1 Literature Search
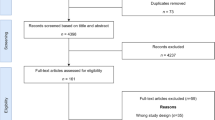
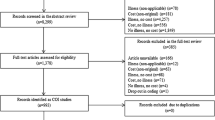
The results of the literature search are shown in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart (Fig. 1). From the 1,646 records, 198 full-text publications were assessed for eligibility. We identified additional 60 publications from the reference list of four systematic reviews [9,10,11, 42]. Altogether, we extracted 3525 costs from 206 publications for further analysis. Details of the included studies are summarized in OSM File 2 (Tables S4–S9). For the transferability analysis we identified eight reports [33, 43,44,45,46,47,48,49] including 144 eligible costs. Altogether 38 different costs were reported from at least two of the 17 countries. All studies and costs items included in the transferability analysis are detailed in OSM File 3 (Tables S10–S11).
3.2 Description of Disease-Related Costs Published in Middle East and North Africa (MENA) Countries
3.2.1 Distribution of Publications and Costs by Country
Most publications were from Saudi Arabia (52/206, 25.1%), Egypt (40/206, 19.4%) and Jordan (15/206, 7.3%). Fourteen of the 206 studies were multinational (6.8%), reporting either costs from multiple countries using uniform costing methods (8/206, 3.9%) or average costs for country groups (6/206, 2.9%). The fewest publications were from Yemen (3/206, 1.5%), Lebanon (3/206, 1.5%), Bahrain (3/206, 1.5%) and Syria (2/206, 1.0%). The detailed breakdown of publications and costs by country are provided in Fig. 2.
3.2.2 Distribution of Publications and Costs Over Time
We observed a marked increase of publication activity from 2012 with an average 2.8 (SD 1.9, range 0–15) years’ delay between the costing year and the publication year. Over half of the costs were published before 2012 (1,789/3,525, 50.7%). The distribution of publications and costs over time are detailed in OSM File 4 (Fig. S1).
3.2.3 Distribution of Publications and Costs Items by Disease Area and Diagnosis
Except for ICD-10 chapter XX (External causes of morbidity and mortality), we found publications from all disease areas. Most publications were reported in ICD-10 chapter I (Certain infectious and parasitic diseases; 41/206, 19.9%), followed by chapter IV (Endocrine, nutritional and metabolic diseases; 24/206, 11.7%) and chapter II (Neoplasms, 18/206, 8.7%). The disease area was not specified in 28/206 (13.6%) publications. These articles focused on a broad (not specified) patient population, a particular care setting, a lifestyle risk, subgroups of the general population or patients taking a particular therapy. Altogether 36/206 (17.5%) papers concerned paediatric populations. The breakdown of studies and costs by disease area is provided in OSM File 4 (Fig. S2).
We identified 84 conditions, out of which 16 were featured in at least three papers (Fig. 3) and a further 14 in at least two papers. Diabetes mellitus (18/206, 8.7%), hepatitis C (11/206, 5.3%) and rotavirus enteritis (10/206, 4.9%) were covered most frequently. The eight papers included in the transferability analysis covered seven conditions.
From the top 25 causes of DALYs in MENA, ten had more than three reports (Fig. 3), neonatal disorders, falls and injuries had 2–2 reports and low back pain, depression, diarrheal diseases and hypertensive heart disease were covered by one study each. We found no cost reports for ten conditions from the top 25 causes of disease burden in the region (e.g., congenital birth defects, iron deficiency, anxiety, chronic obstructive pulmonary disease (COPD), neonatal encephalopathy and sepsis, neck pain, drug use disorders, other musculoskeletal disorders and cardiomyopathy/myocarditis).
3.2.4 Key Characteristics of Costs
Over one-third of costs (1295/3525, 36.7%) came from the outpatient setting, another third from the inpatient setting (1166/3525, 33.1%), 22.9% (808/3525) were from a mixed (outpatient and inpatient) setting, and for 7.4% of costs (259/3525) the outpatient/inpatient categories were not applicable (e.g., indirect costs/productivity losses, direct non-medical costs or communication/management costs of public health programs). The cost types and main sources of costs are shown in Fig. 4. The sources of costs in primary studies were most frequently a healthcare institution (957/2440, 39.2%), government database (726/2440, 29.8%), survey (294/2440, 12.1%), expert opinion (165/2440, 6.7%), chart review (144/2440, 5.9%), insurance database (56/2440, 2.3%), the author’s assumptions (52/2440, 2.1%), a supplier pricelist (25/2440, 1.0%) or a pharmacy (21/2440, 0.9%).
3.3 Transferability of Costs Within MENA
3.3.1 Description of Multi-Country Studies
For the eight eligible studies, the number of included countries (N) and costs (n) are provided below in parentheses. In a cost-effectiveness study of pneumococcal conjugate vaccines, Pugh et al. [33] reported the list prices of vaccines, and the treatment costs of pneumococcal bacteraemia, meningitis, pneumonia and otitis media from expert estimates in 2013 prices (N = 2, n = 16). Mustafa et al. [43] reported the economic burden of acute otitis media in children. Out-of-pocket medication expenses were collected from a survey of parents (N = 2, n = 2). Shafie et al. [44] studied the cost-effectiveness of biphasic insulin treatment in type 2 diabetes (N = 2, n = 16). Disease-costs were modelled on a 30-year timeframe using local unit costs of 2013, but the source of cost data was not reported. Mason et al. [45] compared the cost effectiveness of dietary salt-reduction policies to reduce coronary heart disease (N = 3, n = 21). Costs of seven conditions including acute myocardial infarction, unstable angina, chronic angina, chronic heart failure and hypertension were estimated via a standardized questionnaire completed by ministry of health officials in 2010. Boutayeb et al. [46] compared the direct costs of diabetes mellitus per year per patient in 2008 US$ (N = 16, n = 48). Identical assumptions on resource use and country specific prices for drugs, laboratory tests and physician visits were applied. The rationale for resource use assumptions was not reported. Acknowledging the intra-country variability of costs, the authors provided a low, medium and high price scenario for each country. Missing costs were imputed by the mean cost of respective country income groups, but details were not provided. Alkire et al. [47] reported the cost-effectiveness of caesarean section in obstructed labour (N = 6, n = 6). Unit costs per caesarean section were adopted from a WHO study covering 49 countries. The WHO study applied locally available unit costs on the same resource use structure. Unit costs were obtained from published and unpublished sources including econometric estimates [50]. Isma’eel et al. [48] reported the 2011 US$ costs of preventing a cardiovascular event using three statins (N = 7, n = 21). Costs were calculated using the same dosing and number needed to treat parameters across countries multiplied by local list prices. Aït-Khaled et al. [49] studied the affordability of inhalable corticosteroids for asthma (N = 2, n = 18). Drug costs and unit costs of physician consultations, diagnostic tests and hospitalisations were collected from local authorities in 1998. According to the transferability evaluation criteria of Fukuda et al. [25], the level of reporting transparency was generally low in the eight studies (level B: n = 1, level C: n = 3, level D: n = 4; OSM File 3, Table S10).
3.3.2 Estimates of Cost Transfer Coefficients
The relative differences of costs and macroeconomic indicators, which were used to estimate the cost transfer coefficients are summarized in OSM File 5, Fig. S3. The cost transfer coefficient estimates and the prediction accuracy statistics for transferred costs are displayed in Table 1. The cost transfer coefficient estimates and overall prediction accuracy for the three macroeconomic indicators were similar (OSM File 5, Fig. S4; Table 1). While THEpc and GHEpc data were not available for every country in every costing year, predictions using GDPpc were usually feasible. Therefore, based on the feasibility and accuracy of predictions, the robust regression model using GDPpc provided the optimal cost transfer coefficient (βGDP = 0.28, 95% confidence interval (95% CI): 0.17–0.40, p < 0.001, Table 1). The correlation between predicted and true costs was very high (r = 0.96). However, only 68% and 56% of predicted costs fell in the true ± 50% and ± 30% range, respectively (Fig. 5), which is mainly explained by the skewed distribution of costs. Large relative errors were observed mainly at smaller true costs (OSM File 5, Fig. S5). The non-zero cost transfer coefficient suggested that adjustment by GDPpc yields more accurate predictions than the unadjusted average of costs available from other countries (i.e., applying a cost transfer coefficient βGDP = 0). However, we also rejected the hypothesis of βGDP = 1 (Wald test F1,141 = 159.5, p < 0.001) suggesting that in the included studies actual costs varied less than GDPpc (Table 1).
3.3.3 Analysis of Transferability Using Relative Errors
The distributions of log transformed RE (logRE) values of each estimation model are depicted in OSM File 5 (Fig. S6). Some outlier costs differed up to two magnitudes from true costs, but the log-transformation resulted in reasonably symmetrical distributions. The regression models explained 51–67% of the variance in logRE. We found significant differences between countries, authors and the level of cost aggregation in terms of accuracy. When controlled for other variables, greatest logRE values (i.e., least transferable cost estimates) were found in Qatar and usually high-income countries from the Gulf region, except Oman. Costs from the study of Boutayeb et al. [46] were most accurately estimated. This study involved 16 countries from MENA, so its cost estimates could rely on information from the most countries among all included papers. We also found that estimates of drug costs were more accurate compared to unit costs or highly aggregated disease costs. The details of the transferability analysis are provided in OSM File 5 (Table S12).
4 Discussion
We performed a systematic scoping review of 206 studies presenting disease-related costs in 17 countries of MENA between 1995 and 2019. The number of published papers increased dynamically over the past 10 years, with nearly 3 years’ mean lag between the costing year and the time of publication. Most costs were published from Saudi Arabia and Egypt. The applied methods and data sources varied greatly. We analysed transferability using 144 direct medical costs from eight multi-country studies that applied the same costing methodology in multiple countries.
We developed a cost transfer formula to predict missing costs. The average of available foreign costs adjusted by the relative difference in GDP per capita PPP$ multiplied by a cost transfer coefficient of 0.28 provided the most accurate estimates. A step-by step guide for using the formula is provided in OSM File 6. The correlation between true costs and predicted costs was 0.961. However, only 68% and 56% of the costs could be estimated within the true cost ± 50% and ± 50% tolerance ranges, respectively. Predictions were more accurate for costs from studies that involved the largest number of countries, for countries outside the Gulf region, and for drug costs versus unit or disease costs.
To the best of our knowledge, our study is the first systematic review of disease-related costs and their transferability within MENA. Health economic research has been systematically reviewed for Saudi Arabia by Al-Aqueel et al. [11] up to 2011 (n = 15 studies), for the Gulf cooperation by Eljilany et al. [9] up to 2017 (n = 49), for Egypt by Farid et al. [10] up to 2017 (n = 15), for the entire MENA region by Zrubka et al. [12] up to 2019 (n = 105) and most recently by AlAujan [13] for the Gulf region (n = 14) and Sharkawy et al. [51] including the entire WHO Eastern Mediterranean Region (n = 624). In general, the methodological and reporting quality of studies showed great variation and many shortcomings [9,10,11, 13].
We identified 3,525 costs reported in 84 conditions. Several conditions among the main causes of disease burden in MENA were covered by multiple studies [29]. However, we found no published costs concerning anxiety disorders and iron deficiency anaemia [29]. Multiple publications on cervical cancer and breast cancer reflected the rapidly increasing burden of neoplasms in the region [52]. Also, the large number of publications reflected that in several MENA countries the prevalence of diabetes [53] and in Egypt the prevalence of hepatitis C infection is among the highest in the world [54]. The potential transferability of these costs deserves further research.
Transferability issues have been widely studied for indirect costs of chronic diseases [55, 56], costs collected in various study settings [17, 23], different disease conditions [24, 25, 57] or within geographic regions [58, 59]. Numerous adjustment methods [17, 21, 22, 57], factors of transferability [16] as well as reporting guidelines [15, 20, 60] have been proposed for health economic evaluations. The analysis of patient-level data suggests that the variance of total costs is mainly attributable to individual patients [17, 21]. Studies in Central-Eastern Europe have demonstrated considerable differences in treatment practices involving the same condition, despite the rather similar economic profile of countries [61, 62]. When imputing missing costs, several methods have been proposed from using unadjusted averages of adjacent countries [23], using country-pair specific ratios based on the comparison of known baskets of healthcare goods or services [23, 57] or adjustments by GDP per capita [18, 30, 31]. Unit costs of in- and outpatient services have been estimated via econometric modelling for the WHO CHOICE project using input from 30 countries [63].
We assumed that the secondary usability of published costs in the region is low due to the general lack of data on patient- or location-specific transferability factors as well as the methodological and reporting heterogeneity of costing studies. Therefore, we aimed to develop a cost transfer formula that allows the prediction of missing costs if the same cost is reported from at least one country in the region.
The strength of our proposed approach is its simplicity and the universal availability of GDP per capita data for the adjustment of input costs. Furthermore, our transferability analysis was based on a comprehensive set of data reported from the region. We note that the cost transfer formula is applicable for predicting missing patient-level direct medical costs, given that input costs are measured with the same methodology in the same costing year. We also emphasize that the cost transfer formula is based on adjustment by a single macroeconomic indicator and should only be used if more comprehensive cost transfer methods are not feasible. Input costs should be carefully selected to ensure fit into the analysis. As a minimum requirement, researchers should ensure that the components of transferred costs are listed (transparency level C) so the match between the perspective and relevant components for the decision situation can be judged. Input costs, which are reported by components (transparency level B) or by separate resource use and unit cost elements (transparency level A), allow further adjustments to the decision situation [15, 25]. When selecting the appropriate input costs, the researcher needs to be aware of specific sources of cost variability such as differences between private versus public settings or tender versus list prices. Also, appropriate methods should be used to adjust time differences and currency exchange rates, which are not addressed by the cost transfer formula.
The transferability of costs between countries within the region remains an important research area. Despite the high correlation between the predicted costs and true costs, for nearly half the costs the relative error of prediction was greater than 30%, carrying the risk of flawed estimates of the cost-effectiveness of treatments. Therefore, the cost transfer formula should be used with prudence. To improve the accuracy of predictions, further research is needed on the explainable variability and transferability of costs within MENA involving specific diseases, sub-regions [64,65,66,67] or special cost categories such as productivity loss [56]. We hypothesize that if costs are reported by more countries and the reporting quality improves, more accurate imputations will be possible. We also hypothesize that cost transfer coefficients differ between high- and low- to middle-income countries as well as between different cost types and disease areas. Also, due to the specifics of health systems, the cost-transfer coefficient may be specific to geographic regions or even country-pairs. Furthermore, as more data become available for estimation or as health systems evolve over time, cost transfer coefficient estimates may also change.
Although some of these hypotheses can be studied from the cost database described in this paper, the methodological heterogeneity and varying reporting quality of costing studies in MENA may represent challenges for further studies. The association between reporting transparency and the accuracy of cost imputation warrants further research. While we promote the efficient secondary utilisation of published costs, we also encourage authors to report their primary costing research results with transferability in mind, following applicable international guidelines [15, 60].
Several limitations of our study should be noted. We limited our search to academic publications in peer-reviewed journals indexed in PubMed. Therefore, papers exclusive to other bibliographic databases have been omitted. Furthermore, although conference posters, government databases, HTA reports and other sources of the grey literature may be important sources of disease-related cost data, they were omitted from this review. Also, we limited our search to English language articles, so Arabic and French publications have been omitted [68]. Nevertheless, in a review of 27 months’ global health economic publications, Pitt et al. [69] did not identify Arabic or French articles from MENA. Therefore, we assume that English papers provide a good representation of health economic publications from the region. Furthermore, the database search was closed in December 2019, so further publications may have reported costs from the region. Although omitted from this study, recently published costs may prove useful in testing the external validity of our proposed imputation method. Finally, costs reported by Boutayeb et al. [46] and Alkire et al. [47] included components that were estimated from economic parameters of countries, which may have influenced the cost transfer coefficient estimates. While the exact proportion of these estimated components were not reported by the authors, according to the descriptions of their methods, the reported costs were mainly based on primary data.
5 Conclusion
The cost transfer formula estimated for MENA allows the imputation of missing direct medical costs if only GDP per capita is available to adjust transferred costs for the local setting. When using the formula, authors should collect costs from as many sources as possible that match the perspective and relevant components of the decision situation. Due to the limited accuracy of predictions, the cost transfer formula should be used with prudence. Further research is needed to improve the accuracy of transferred costs. To enable the secondary utilisation of data, primary costing research results should be reported according to applicable international guidelines.
References
Kiprop V. What Are The MENA Countries? 2019 Oct 30, 2020]; Available from: https://www.worldatlas.com/articles/what-are-the-mena-countries.html
World Bank. World Development Indicators. GDP per capita- Middle East & North Africa. 2020 October 30, 2020]; Available from: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=ZQ
World Bank. World Development Indicators. Population, total - Middle East & North Africa. 2020 October 30, 2020]; Available from: https://data.worldbank.org/indicator/SP.POP.TOTL?locations=ZQ
SHOPS Plus. Health Trends in the Middle East and North Africa: A Regional Overview of Health Financing and the Private Health Sector. Rockville, MD, USA: Abt Associates Inc.; 2018.
World Bank. World Development Indicators. Current health expenditure per capita (current US$) - Middle East & North Africa. 2020 October 30, 2020]; Available from: https://data.worldbank.org/indicator/SH.XPD.CHEX.PC.CD?locations=ZQ
O’Rourke B, Oortwijn W, Schuller T. Announcing the new definition of health technology assessment. Value Health. 2020;23(6):824–5.
Sixty Seventh World Health Assembly. Health intervention and technology assessment in support of universal health coverage. Geneva: WHO; 2014.
Kanavos P, Tzouma V, Fontrier A, Kamphuis B, Colville Parkin G, Saleh S. Pharmaceutical pricing and reimbursement in the Middle East and North Africa region. London: LSE Consulting, London School of Economics and Political Science; 2018.
Eljilany I, El-Dahiyat F, Curley LE, Babar ZU. Evaluating quantity and quality of literature focusing on health economics and pharmacoeconomics in Gulf Cooperation Council countries. Expert Rev Pharmacoecon Outcomes Res. 2018;18(4):403–14.
Farid S, Elmahdawy M, Baines D. A systematic review on the extent and quality of pharmacoeconomic publications in Egypt. Clin Drug Investig. 2019;39(2):157–68.
Al-Aqeel SA. State of health economic evaluation research in Saudi Arabia: a review. Clinicoecon Outcomes Res. 2012;4:177–84.
Zrubka Z, Rashdan O, Gulácsi L. Health economic publications from the middle east and North Africa region: a scoping review of the volume and methods of research. Glob J Qual Saf Healthcare. 2020;3(2):44–54.
AlAujan SS, Almazrou SH, Al-Aqeel SA. A systematic review of sources of outcomes and cost data utilized in economic evaluation research conducted in the Gulf cooperation council. Risk Manag Healthc Policy. 2021;14:209–20.
Al-Jazairi AS, Al-Qadheeb NS, Ajlan A. Pharmacoeconomic analysis in Saudi Arabia: an overdue agenda item for action. Ann Saudi Med. 2011;31(4):335–41.
Drummond M, Barbieri M, Cook J, Glick HA, Lis J, Malik F, et al. Transferability of economic evaluations across jurisdictions: ISPOR good research practices task force report. Value Health. 2009;12(4):409–18.
Welte R, Feenstra T, Jager H, Leidl R. A decision chart for assessing and improving the transferability of economic evaluation results between countries. Pharmacoeconomics. 2004;22(13):857–76.
Sculpher MJ, Pang FS, Manca A, Drummond MF, Golder S, Urdahl H, et al. Generalisability in economic evaluation studies in healthcare: a review and case studies. Health Technol Assess. 2004;8(49):1–192.
Gulacsi L, Rencz F, Pentek M, Brodszky V, Lopert R, Hever NV, et al. Transferability of results of cost utility analyses for biologicals in inflammatory conditions for Central and Eastern European countries. Eur J Health Econ. 2014;15(Suppl 1):S27-34.
Eldessouki R, Dix SM. Health care system information sharing: a step toward better health globally. Value Health Reg Issues. 2012;1(1):118–20.
Drummond M, Manca A, Sculpher M. Increasing the generalizability of economic evaluations: Recommendations for the design, analysis, and reporting of studies. Int J Technol Assess Health Care. 2005;21(2):165–71.
Grieve R, Nixon R, Thompson SG, Normand C. Using multilevel models for assessing the variability of multinational resource use and cost data. Health Econ. 2005;14(2):185–96.
Perrier L, Buja A, Mastrangelo G, Baron PS, Ducimetiere F, Pauwels PJ, et al. Transferability of health cost evaluation across locations in oncology: cluster and principal component analysis as an explorative tool. BMC Health Serv Res. 2014;18(14):537.
Oppong R, Jowett S, Roberts TE. Economic evaluation alongside multinational studies: a systematic review of empirical studies. PLoS ONE. 2015;10(6): e0131949.
Zwolsman S, Kastelein A, Daams J, Roovers JP, Opmeer BC, http://www.women-up.eu/consortium W-UC. Heterogeneity of cost estimates in health economic evaluation research. A systematic review of stress urinary incontinence studies. Int Urogynecol J. 2019;30(7):1045-59.
Fukuda H, Lee J, Imanaka Y. Costs of hospital-acquired infection and transferability of the estimates: a systematic review. Infection. 2011;39(3):185–99.
Wikipedia. MENA. 2021.10.15.]; Available from: https://en.wikipedia.org/wiki/MENA
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29(372): n71.
WHO. International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10 Version:2019). 2019 5th Nov, 2020]; Available from: https://icd.who.int/browse10/2019/en
Institute for Health Metrics and Evaluation, Human Development Network TWB. The Global Burden of Disease: Generating Evidence, Guiding Policy – Middle East and North Africa Regional Edition. Seattle, WA: IHME, 2013. Seattle, WA: Institute for Health Metrics and Evaluation; 2013.
Lopert R, Ruiz F, Chalkidou K. Applying rapid “de-facto” HTA in resource-limited settings: experience from Romania. Health Policy. 2013;112(3):202–8.
Lopert R, Lang DL, Hill SR, Henry DA. Differential pricing of drugs: a role for cost-effectiveness analysis? The Lancet. 2002;359(9323):2105–7.
Franklin M, Lomas J, Walker S, Young T. An educational review about using cost data for the purpose of cost-effectiveness analysis. Pharmacoeconomics. 2019;37(5):631–43.
Pugh SJ, Fletcher MA, Charos A, Imekraz L, Wasserman M, Farkouh R. Cost-effectiveness of the pneumococcal conjugate vaccine (10- or 13-valent) versus no vaccination for a national immunization program in Tunisia or Algeria. Infect Dis Ther. 2019;8(1):63–74.
Royston P. sg3.5: Comment on sg3.4 and an improved D’Agostino test. Stata Tech bull. 1991;3:23–4.
Jann B. robreg: Stata module providing robust regression estimators. 2021 2021.10.28. ]; Available from: http://ideas.repec.org/c/boc/bocode/s458931.html
Huber PJ. Robust regression: Asymptotics, conjectures and Monte Carlo. Ann Stat. 1973;1(5):799–821.
StataCorp. Stata 17 Base Reference Manual. College Station, TX: Stata Press; 2021.
Christensen P, Dysert L, Bates J, Burton D, Creese R, Hollmann J, et al. AACE International Recommended Practice No. 18R-97. Cost Estimate Classification System – As Applied in Engineering, Procurement, and Construction for the Process Industries TCM Framework: 73 – Cost Estimating and Budgeting. Fairmont, WV: The Association for the Advancement for Cost Engineering; 2005.
Energy USDo. Cost Estimating Guide. Washington, DC2011.
Rousseew P, Leroy A. Robust regression and outlier detection. Toronto: John Wiley & Sons; 1987.
StataCorp. Stata Statistical Software: Release 17. . College Station, TX: StataCorp LP.; 2021.
Saleh S, El Harakeh A, Baroud M, Zeineddine N, Farah A, Sibai AM. Costs associated with management of non-communicable diseases in the Arab Region: a scoping review. J Glob Health. 2018;8(2): 020410.
Mustafa G, Al Aidaroos AY, Al Abaidani IS, Meszaros K, Gopala K, Ceyhan M, et al. Incidence and economic burden of acute otitis media in children aged up to 5years in three Middle Eastern countries and Pakistan: a multinational, retrospective, observational study. J Epidemiol Glob Health. 2017;7(2):123–30.
Shafie AA, Gupta V, Baabbad R, Hammerby E, Home P. An analysis of the short- and long-term cost-effectiveness of starting biphasic insulin aspart 30 in insulin-naive people with poorly controlled type 2 diabetes. Diabetes Res Clin Pract. 2014;106(2):319–27.
Mason H, Shoaibi A, Ghandour R, O’Flaherty M, Capewell S, Khatib R, et al. A cost effectiveness analysis of salt reduction policies to reduce coronary heart disease in four Eastern Mediterranean countries. PLoS ONE. 2014;9(1): e84445.
Boutayeb A, Boutayeb W, Lamlili MEN, Boutayeb S. Estimation of the direct cost of diabetes in the Arab region. Mediterr J Nutr Metab. 2014;7(1):21–32.
Alkire BC, Vincent JR, Burns CT, Metzler IS, Farmer PE, Meara JG. Obstructed labor and caesarean delivery: the cost and benefit of surgical intervention. PLoS ONE. 2012;7(4): e34595.
Isma’eel H, Mohanna Z, Hamadeh G, Alam E, Badr K, Alam S, et al. The public cost of 3 statins for primary prevention of cardiovascular events in 7 Middle East countries: not all of them can afford it. Int J Cardiol. 2012;155(2):316–8.
Ait-Khaled N, Auregan G, Bencharif N, Camara LM, Dagli E, Djankine K, et al. Affordability of inhaled corticosteroids as a potential barrier to treatment of asthma in some developing countries. Int J Tuberc Lung Dis. 2000;4(3):268–71.
Gibbons L, Belizán J, Lauer J, Betrán A, Merialdi M, Althabe F. The Global Numbers and Costs of Additionally Needed and Unnecessary Caesarean Sections Performed per Year: Overuse as a Barrier to Universal Coverage Geneva: WHO; 2010.
Sharkawy MN, Dastan I. A scoping review of health economic evaluation in the World Health Organization Eastern Mediterranean region. Expert Rev Pharmacoecon Outcomes Res. 2021.
Institute for Health Metrics and Evaluation. GBD Data Visualizations, GBD Compare, North Africa and Middle East Both sexes, All ages, DALYs per 100,000. June 13, 2021]; Available from: https://vizhub.healthdata.org/gbd-compare/
World Bank. Diabetes prevalence (% of population ages 20 to 79). [cited June 13, 2021; Available from: https://data.worldbank.org/indicator/SH.STA.DIAB.ZS
Blach S, Zeuzem S, Manns M, Altraif I, Duberg A-S, Muljono DH, et al. Global prevalence and genotype distribution of hepatitis C virus infection in 2015: a modelling study. Lancet Gastroenterol Hepatol. 2017;2(3):161–76.
Zhao FL, Xie F, Hu H, Li SC. Transferability of indirect cost of chronic disease: a systematic review and meta-analysis. Pharmacoeconomics. 2013;31(6):501–8.
Rashdan O, Brodszky V, Péntek M, Gulácsi L, Zrubka Z. PNS32 Towards a Healthcare Cost Catalogue for Middle EAST and North Africa: A Systematic Review of Productivity Loss Costs Reported in Health Economic Publications between 1989-2019. Value in Health. 2020;23.
Schulman K, Burke J, Drummond M, Davies L, Carlsson P, Gruger J, et al. Resource costing for multinational neurologic clinical trials: methods and results. Health Econ. 1998;7(7):629–38.
Mandrik O, Knies S, Kalo Z, Severens JL. Reviewing transferability in economic evaluations originating from eastern Europe. Int J Technol Assess Health Care. 2015;31(6):434–41.
Augustovski F, Iglesias C, Manca A, Drummond M, Rubinstein A, Marti SG. Barriers to generalizability of health economic evaluations in Latin America and the Caribbean region. Pharmacoeconomics. 2009;27(11):919–29.
Husereau D, Drummond M, Petrou S, Carswell C, Moher D, Greenberg D, et al. Consolidated Health Economic Evaluation Reporting Standards (CHEERS)–explanation and elaboration: a report of the ISPOR Health Economic Evaluation Publication Guidelines Good Reporting Practices Task Force. Value Health. 2013;16(2):231–50.
Gulacsi L, Rencz F, Poor G, Szekanecz Z, Brodszky V, Baji P, et al. Patients’ access to biological therapy in chronic inflammatory conditions; per capita GDP does not explain the intercountry differences. Ann Rheum Dis. 2016;75(5):942–3.
Pentek M, Poor G, Wiland P, Olejarova M, Brzosko M, Codreanu C, et al. Biological therapy in inflammatory rheumatic diseases: issues in Central and Eastern European countries. Eur J Health Econ. 2014;15(Suppl 1):S35-43.
Stenberg K, Lauer JA, Gkountouras G, Fitzpatrick C, Stanciole A. Econometric estimation of WHO-CHOICE country-specific costs for inpatient and outpatient health service delivery. Cost Eff Resour Alloc. 2018;16:11.
Zrubka Z, Alabdulkarim HAA, Péntek M, Gulácsi L. PNS34 Towards a Healthcare Cost Catalogue for Middle EAST and North Africa: A Systematic Review of Costs Reported in Health Economic Publications from the GULF Region 1995-2019. Value in Health. 2020;23.
Zrubka Z, Mhanna L, Bassem Chmaissani M, Péntek M, Gulácsi L. PNS20 Towards a Healthcare Cost Catalogue for Middle EAST and North Africa: A Systematic Review of Costs Reported in Health Economic Publications from Egypt 1995-2019. Value in Health. 2020;23.
Zrubka Z, Abu-Zahra T, Almaaytah A, Péntek M, Gulácsi L. PNS38 Towards a Healthcare Cost Catalogue for Middle EAST and North Africa: A Systematic Review of Costs Reported in Health Economic Publications from Jordan, Lebanon Palestine and Syria 1995-2019. Value in Health. 2020;23.
Zrubka Z, Fgaier M, Atitallah A, Mahdi Abid M, Péntek M, Gulácsi L. PNS19 Towards a Healthcare Cost Catalogue for Middle EAST and North Africa: A Systematic Review of Costs Reported in Health Economic Publications from Algeria, Libya, Morocco and Tunisia 1995-2019. Value in Health. 2020;23.
Ballais J, Al Amrawy M, Al Dbiyat M, Charbel L, Geyer B, Mezedjri L. The Place of the French Language in Arabic-Speaking Mediterranean. In: Brunn S, Kehrein R, editors. Handbook of the Changing World Language Map. Chambridge: Springer; 2018.
Pitt C, Goodman C, Hanson K. Economic evaluation in global perspective: a bibliometric analysis of the recent literature. Health Econ. 2016;25(Suppl 1):9–28.
Acknowledgements
The authors thank Bassem Chmaissani for his valuable contribution to this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author contributions
Conceptualisation and design: ZZ, LG. Acquisition of data: ZZ, LM, TA-Z, MM-A, MF, HA, LG. Statistical analysis: ZZ, LM, TA-Z. Analysis and interpretation of data: ZZ, MP, FE-D, MD, LG. Writing—original draft preparation: ZZ. Writing—review and edition: ZZ, MP, FE-D, MD, LG. Funding acquisition: LG. Supervision: ZZ, LG.
Funding
Open access funding provided by Óbuda University. This work was supported by the National Research, Development and Innovation Fund of Hungary, under the Tématerületi Kiválósági Program funding scheme (Project no. TKP2020-NKA-02).
Data availability
Data are provided in the Online Supplementary Materials. Further details are available from the authors upon a reasonable request.
Conflicts of interest
For conducting this research, MP, LM, TAZ, MMA, MF and MD received funding from Project no. TKP2020-NKA-02, implemented with the support provided from the National Research, Development and Innovation Fund of Hungary, financed under the Tématerületi Kiválósági Program funding scheme. During this research, MP received funding from project No. 2019-1.3.1-KK-2019-00007, implemented with the support provided from the National Research, Development and Innovation Fund of Hungary, financed under the 2019-1.3.1-KK funding scheme. During this research, LG received funding from Project no. TKP2020-NKA-02, implemented with the support provided from the National Research, Development and Innovation Fund of Hungary, financed under the Tématerületi Kiválósági Program funding scheme. During this research, ZZS received funding from Project no. TKP2020-NKA-02, implemented with the support provided from the National Research, Development and Innovation Fund of Hungary, financed under the Tématerületi Kiválósági Program funding scheme, from the European Research Council under the European Union’s Horizon 2020 research and innovation program (grant 679681) and from project No. 2019-1.3.1-KK-2019-00007, implemented with the support provided from the National Research, Development and Innovation Fund of Hungary, financed under the 2019-1.3.1-KK funding scheme.
Compliance with ethical standards
No ethics approval was necessary for this research.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zrubka, Z., Péntek, M., Mhanna, L. et al. Disease-Related Costs Published in The Middle East and North Africa Region: Systematic Review and Analysis of Transferability. PharmacoEconomics 40, 587–599 (2022). https://doi.org/10.1007/s40273-022-01146-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-022-01146-6