Abstract
Individuals with obesity are at increased risk of developing infectious diseases. Timely administration of an effective dose of an antimicrobial agent is paramount to safeguard optimal therapy. For this purpose, special patient populations at risk for altered exposure such as renal or hepatic impairment are studied during drug development. Strikingly, there is no such evaluation in individuals with obesity despite a potential influence on exposure and a global obesity prevalence of 13 %. Optimal clinical decision making in patients with obesity is impossible without prior study of the drug of interest in this population. This statement is strengthened by an evaluation of 19 antimicrobial agents that showed tremendous variability in the influence of weight on clearance. In contrast to patient with renal or hepatic impairment who are mainly at risk of overexposure, individuals with obesity can be at risk of both under- and overexposure. Gaining knowledge on the influence of body weight on clearance during early phases of drug development may allow for optimisation of other phases of research, potentially increasing success rate of the drug, and can provide clinicians with vital information as soon as the drug reaches the market. Antimicrobial therapy should be tailored to obesity-related (patho)physiological changes and to reach this goal, obese individuals should be studied during drug development.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Individuals with obesity should be recognised as a special patient population during drug development of antibacterial and antifungal agents. Suboptimal exposure may be anticipated for 37 % of antimicrobial agents as dosing strategy does not match the influence of weight on clearance. |
1 Introduction
1.1 Clinical Problem
Patients with obesity (body mass index [BMI] ≥ 30 kg/m2) are at increased risk of nosocomial infections such as surgical-site infections, pneumonia and Clostridium difficile colitis and are also more likely to develop severe complications from infections [1]. Moreover, patients with obesity show increased length of stay in the intensive care unit, although mortality is not necessarily increased [1]. There is a great need to provide optimal care to patients with obesity with infectious diseases although clear guidance on how therapy should be individualised is often lacking. We are of the opinion that antimicrobial therapy should be tailored according to obesity-associated physiological changes that impact drug pharmacokinetics thereby assuring sufficient exposure and thus maximise efficacy and simultaneously minimising toxicity.
1.2 Obesity
Global obesity prevalence among adults was estimated at 650 million in 2016, 13 % of the world population, and has tripled since 1975 [2, 3]. Historically, prevalence was concentrated in high-income countries but is on the rise in low- and middle-income countries, especially in urban areas [3]. Although obesity is defined as a BMI > 30 kg/m2, the population of individuals with obesity is heterogeneous and could be viewed on a continuous scale as different classes of obesity are distinguished ranging from class I for BMI 30–35 kg/m2 to class III for BMI > 40 kg/m2 [2]. An overabundance of adipose tissue is the key characteristic of obesity, although physiological changes may simultaneously happen in various organ systems like the kidneys, liver and the cardiovascular system [3, 4].
Glomerular filtration rate increases at an early stage of obesity while it decreases in the long term. Additionally, tubular secretion is enhanced in individuals with obesity. Cardiac output increases, which leads to increased liver blood flow that is an important determinant for clearance of medium to high extraction ratio drugs. The intestinal and hepatic cytochrome P450 (CYP) 3A4- and 2C19-mediated metabolic capacity is reduced while CYP 2E1 and Phase II metabolism are enhanced while CYP 1A2 and 2C9 activity remains uninfluenced by obesity [4, 5]. Moreover, the expression of drug transporters like organic anion transporter, organic anion transporting polypeptides and multidrug resistance protein 2 and 3 may be either suppressed or increased by obesity [4].
Acute infection itself may simultaneously influence clearance as CYP 1A2, 2C19 and 3A activity is increased while 2B6 and 2C9 activity is decreased [5]. Fat disposition in individuals with obesity mainly takes place in the subcutis, abdominal visceral depot, heart, liver, pancreas and kidney. For the treatment of infections in these organs, increased systemic exposure in plasma may be needed to overcome impaired tissue penetration as was demonstrated for several antimicrobial agents using clinical micro-dialysis studies [3, 6,7,8]. Nevertheless, it remains unclear if higher plasma concentrations lead to improved clinical or microbiological cure.
Investigations on the plasma pharmacokinetics are of important relevance given the difficulties measuring exposure at the site of infection. Plasma exposure or area under the curve (AUC) in steady state is determined by the ratio of clearance and the maintenance dose. For patients with obesity both the influence of body weight on clearance and the dosing regimen, i.e., mg/kg body weight or fixed dose, determine whether an adjusted maintenance dosage is required. An increased volume of distribution would prolong the time to steady state conditions and reduce peak concentrations. A common assumption is that lipophilicity can be used to predict changes in volume of distribution for patients with obesity, however particularly for lipophilic drugs changes are unpredictable and there is high inter-drug variability. Obesity-associated changes in volume of distribution need to be considered for drugs with long half-life or drugs that depend on peak concentration [9]. For dose adjustments in individuals with obesity, clearance is the primary parameter of interest as changes directly influence exposure.
2 Influence of Obesity on Clearance of Antibacterial and Antifungal Agents
2.1 Non-infectious Individuals with Obesity
To motivate our position presented in this viewpoint, literature on the influence of body weight on clearance of commonly used antibiotic and antifungal agents in otherwise healthy, i.e., non-infectious, individuals with (morbid) obesity was reviewed [6, 7, 10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. Studies reporting on intravenously (iv) administered drugs were included and those only providing clearance for an obese and non-obese cohort without specifying an equation describing clearance over a large weight span were excluded. The fold increase in clearance between a 70 kg and 140 kg individual was calculated based on the equation for clearance reported in the respective studies. In line with typical criteria for bioequivalence a 1.0- to 1.25-fold increase in clearance may be considered a non-significant influence, a 1.25- to 1.5-fold increase a moderate influence and a ≥ 1.5-fold increase may be considered a strong influence of body weight on clearance. The 140 kg reference weight corresponds with the 95th percentile body weight of Americans in 2016 [27].
We identified 19 reports describing the influence of body weight on clearance of antimicrobial agents, i.e., 13 antibacterial agents and 6 antifungal agents. Either a non-significant, moderate or a strong influence of weight on clearance was identified for 7/19 (37 %), 8/19 (42 %) and 4/19 (21 %) antimicrobial agents, respectively [6, 7, 10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26].
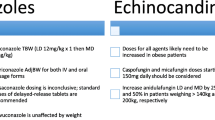
The results are visualised in Fig. 1, in which clearance for a typical 70-kg individual was set to 1.0. Each line represents the fold increase in clearance with increasing body weight for the respective antimicrobial agent. A large heterogeneity in influence of increasing body weight on clearance is shown. A 2-fold increase in clearance corresponds to a 50 % decrease in exposure (measured as AUC) for patients with a body weight of 140 versus 70 kg receiving an equal dose. The grey area in Fig. 1 represents a moderate influence of body weight on clearance, the area below and above represents non-significant and strong influence, respectively. If non–weight-based patient characteristics (age, height or serum creatinine) are predictive for clearance, the median value from the study population was fixed in order to visualise the influence of bodyweight on clearance. As a result, clearance may differ for patients with the same weight if difference in age, height or serum creatinine are present as is the case for cefazolin, ceftaroline, daptomycin, meropenem, piperacillin and tobramycin. From the figure it can be deduced that predicting the influence of body weight on clearance is challenging as even within the therapeutic classes of macrolides, cephalosporins, echinocandins and triazoles pronounced differences are observed, which cannot be explained by hepatic versus renal clearance or differences in lipophilicity, protein binding or molecular weight.
Influence of increasing body weight on clearance of antibacterial and antifungal agents expressed as fold increase compared to a typical 70 kg individual. Each line represents an antimicrobial agent visualising the fold increase in clearance from plasma with increasing body weight. *Amoxicillin, cefazolin, ciprofloxacin, liposomal amphotericin B, moxifloxacin and tigecycline show no influence of body weight on clearance and therefore overlap at fold increase in clearance = 1.0. The grey shaded area represents a moderate influence of body weight on clearance. A fold increase in clearance below the grey area represents no significant influence on clearance, a fold increase in clearance above the grey area represents a strong influence of body weight on clearance. For cefazolin, ceftaroline, daptomycin, meropenem, piperacillin and tobramycin drivers of clearance were identified that are not strictly weight based (age, height, serum creatinine); for these drugs values of the respective drivers were fixed at the median value in order to visualise the influence of body weight on clearance. The length of the line corresponds with the maximum total body weight in the study population, with a maximum of 210 kg
3 Optimising Exposure: Connecting Obesity and Dosing Strategy
3.1 Body Weight and Dosing Strategy
Exposure to antimicrobial agents in steady state across different body weights is determined by both the influence of body weight on clearance (as depicted in Fig. 1) and the employed dosing strategy, i.e., fixed dosing or mg/kg body weight. In individuals with obesity, it is particularly important that dose adjustments match the direction and magnitude of effect of weight on clearance. In Table 1 we show that applying the labelled dosing strategy (fixed dosing or mg/kg dosing) to individuals with obesity for the antimicrobial drugs from Fig. 1 would introduce a risk of underexposure for 7/19 (37 %) of antimicrobial agents and a risk of overexposure for 4/19 (21 %) of antimicrobial agents. Four different scenarios are distinguished in data presented in Table 1; fixed dosing regimen & body weight not associated with increased clearance, fixed dosing regimen & body weight associated with increased clearance, weight-based dose & body weight not associated with increased clearance and mg/kg dose & body weight associated with increased clearance. These scenarios are discussed below for the selected 19 antimicrobial agents.
3.1.1 Fixed Dosing Regimen and Body Weight Not Associated with Increased Clearance
The drugs amoxicillin, cefazolin, ciprofloxacin, moxifloxacin, piperacillin and tigecycline, are given in a fixed dose and their clearance is not influenced by body weight [6, 7, 11, 20, 22, 26]. Similar exposure in plasma is expected across all body weights.
3.1.2 Fixed Dosing Regimen and Body Weight Associated with Increased Clearance
The drugs anidulafungin, caspofungin, ceftaroline, fluconazole, meropenem, micafungin, posaconazole and tedizolid are also given at fixed dosages, yet their clearance is reported to be influenced by body weight and therefore individuals with obesity may be at risk of underexposure [10, 12, 15, 18, 19, 21, 24, 25]. These drugs may require higher maintenance dosages when the same exposure is aimed for, yet the need and magnitude of dose increase depends on the exact influence of body weight on clearance and the width of the therapeutic window.
3.1.3 Weight-Based Dosing Regimen and Body Weight Not Associated with Increased Clearance
Amphotericin B is dosed as mg/kg whereas no influence of body weight on clearance was identified in individuals up to 177 kg. As a result, individuals with obesity are at risk of overexposure if doses are not capped at a body weight of 100 kg [14].
3.1.4 Weight-Based Dosing Regimen and Body Weight Associated with Increased Clearance
For the drugs daptomycin, gentamicin, tobramycin and vancomycin a weight-based dosing regimen is employed and weight is of influence on clearance [13, 16, 17, 23]. An mg/kg-based dosing regimen provides a linear dose increase with body weight. Nevertheless, clearance may not necessarily increase linearly with body weight (Fig. 1). As such an mg/kg dose leads to overexposure for individuals with extreme body weights. In order to mitigate the risk of overexposure, alternative body size descriptors like adjusted body weight (ABW) or lean body weight (LBW) may be used to calculate dosing weights as these metrics also increase in a non-linear manner with body weight, similar to the non-linear increase of clearance with body weight. The heterogeneity in Fig. 1 illustrates that no single alternative body size descriptor is suited for use as a universal body size descriptor for predicting clearance in individuals with obesity. Moreover, care is to be taken when using LBW for this purpose, as the inclusion of gender in the calculation of LBW may introduce undesired differences in exposure between men and women [28,29,30, 32].
For these antimicrobial agents, the width of the therapeutic window determines if dose adjustment is needed. Daptomycin has a relatively wide therapeutic window although doses beyond 500 mg are associated with creatinine phosphokinase elevation [31]. Gentamicin on the other hand has a narrow therapeutic window and is usually dosed on ABW in clinical practice. Interestingly this approach introduces a risk of underexposure in individuals with severe obesity and consequently may be dosed on a nomogram that ensures similar exposure across different body weights [17, 32].
3.2 (Critically) Ill Patients with Obesity
Real-world data from (critically) ill patients with obesity treated with amoxicillin, cefazolin, daptomycin, fluconazole, gentamicin, meropenem, micafungin, moxifloxacin, piperacillin and vancomycin show that, besides body weight, patient characteristics like renal function, renal replacement therapy, admission to ward or ICU, age and class of obesity may be associated with altered clearance [31,32,33,34,35,36,37,38,39,40,41,42,43,44].
The influence of body weight on clearance in (critically) ill patients with obesity was similar to the influence identified for their non-infectious counterparts for most antimicrobial agents. Nevertheless, for meropenem several studies in critically ill patients did not report an influence of weight on clearance; hence, dose modification solely based on body weight does not seem warranted [36, 37]. Fixed dosing of daptomycin in (critically) ill patients with obesity is associated with a lower incidence of creatinine phosphokinase elevation, despite a significant influence of weight on clearance [31]. For cefazolin it remains unclear if increased doses for surgical prophylaxis lead to improved outcome in individuals with obesity for procedures > 4 h despite impaired tissue penetration [34].
A major strength of studies in non-critically ill patients with obesity is the wide weight range compared with studies in (critically) ill patients. This allows for precise characterisation of the influence of body weight on clearance while minimising the influence of other potentially relevant influences on clearance like varying renal function. Nevertheless, findings from non-(critically) ill individuals with obesity need external validation in (critically) ill individuals as is illustrated by the need for fixed dosing of daptomycin in individuals with obesity and renal function-based dose optimisation for fluconazole, meropenem, piperacillin and vancomycin [31, 34, 41,42,43,44,45]. For gentamicin, dose optimisation may be based on both renal function and admission to the ward or ICU [32].
In conclusion, obesity-related changes in exposure to antimicrobial agents can be predicted using studies investigating the influence of body weight on clearance and volume of distribution together with the dosing strategy. Whether the resulting exposure is acceptable depends on the width of the therapeutic window, but also on the sensitivity of the causative pathogen towards the employed antimicrobial agent and penetration of the drug into the site of infection.
4 The Unpredictable Effect Size of Obesity on Clearance Necessitates Early Research, Similar to Renal and Hepatic Insufficiency
Nowadays, patients with renal and hepatic insufficiency are recognised as special patient populations as they are at increased risk of developing drug-related toxicity as a result of impaired clearance. Similarly, exposure may be altered in individuals with obesity and the lack of appropriate dose adjustment can put individuals with obesity at the same risk of toxicity. In contrast to individuals with renal or hepatic impairment, individuals with obesity may also be at risk of therapy failure as illustrated above.
To compare the effect size on clearance of increasing body weight versus renal and hepatic insufficiency, we summarised the dose adjustments required for individuals with obesity in order to achieve exposure in plasma that is similar to their normal-weight counterparts and dose adjustments proposed by the package inserts for renal and hepatic insufficiency for the aforementioned 19 antimicrobial agents (Table 2) [46]. Nevertheless, for some special patient populations additional data on dose adjustment may be available in the field.
For individuals with obesity, dose adjustments are required for 8/19 (42 %) antimicrobial agents. Of these eight agents, a dose increase of 25 %–100 % is proposed for four antimicrobial agents with a fixed-dose regimen while a dose reduction of up to 36 % is proposed for four antimicrobial agents with a weight-based dosing regimen. For individuals with renal impairment, dose reductions are proposed for 11/19 (58 %) of the identified antimicrobial agents. Typical dose adjustments range from 33–95 % of the daily dose. For only 2/19 (11 %) identified antimicrobial agents, a 50 % reduced daily maintenance dose is required depending on the severity of hepatic impairment. This low percentage may be explained by the large metabolic capacity of the liver implying that hepatic insufficiency (Child-Pugh class B/C) does not always require dose adjustment for drugs that are subject to hepatic metabolism.
Including individuals with obesity as a special patient population in drug labelling information seems justified as for the 19 evaluated drugs both the number of antimicrobial agents that require dose modification and the corresponding magnitude of the required dose modification are similar to those encountered in individuals with renal impairment and exceed those encountered in individuals with hepatic impairment.
5 Scenarios for Research in Individuals with Obesity
Regulating bodies recognise the importance of studying drug exposure in individuals with obesity and the current lack of guidance for industry. The Food and Drug Administration (FDA) already propagates enhancement of the diversity of clinical trial populations and the European Medicines Agency (EMA) published a reflection paper emphasising the importance of studying drug exposure in individuals with obesity [47, 48].
Individuals with obesity are currently often excluded from the early stages of drug research, which impedes detecting the influence body weight may or may not have on clearance. As a result, studies identifying the influence of weight on clearance are often conducted during Phase IV, after gaining market authorisation. In this process, unlocking access to vital information is postponed by several years, although this influence could be elucidated through small sample size pharmacokinetic studies. Model Informed Precision Dosing is an important tool for therapy optimisation and it has shown its value in many patient populations for various diseases [49]. In order for these models to provide valid predictions of exposure in individuals with obesity, it is of utmost importance to collect data in individuals over a wide weight range.
As a first step, admitting individuals with different classes of obesity to early stages of drug development will yield important information at a pivotal moment as findings can be carried over to later stages of pharmaceutical research. In case body weight shows a strong influence on clearance at an early stage, individualised doses may be administered during subsequent phases of research in order to achieve similar exposure in plasma across different body weights. In contrast, when no influence of body weight on the plasma pharmacokinetics is identified, fixed-dosing schedules can be applied in subsequent studies without limits for body weight at inclusion of the study.
The clinical population of individuals with obesity may still be heterogeneous with respect to additional factors that may influence clearance such as changes in renal or hepatic function, age or critical illness. As a second step, establishing a platform for sharing and bundling individual data from multi-morbid patients with obesity may potentiate therapy optimisation in this special population as collecting data from sufficient multi-morbid individuals may not be feasible in a single centre.
We propose to no longer exclude individuals with obesity at any phase of pharmaceutical research and specifically study individuals with (extreme) obesity during drug development. When the influence of weight on clearance is known the moment an antimicrobial agent reaches the market, clinicians are equipped with essential information for therapy optimisation.
6 Conclusion and Future Perspectives
From our overview, we conclude that obesity has a varying influence on exposure to antimicrobial agents with 7/19 (37 %) drugs indicating that clearance is not significantly increased with body weight. Dose adjustments, either an increase or a decrease, are required for 8/19 (42 %) antimicrobial agents, placing the population of over weight and patients with (morbid) obesity at increased risk of suboptimal exposure. While patients with renal or hepatic impairment are mostly at risk of overexposure, patients with increased body weight are at double jeopardy as both an increased risk of underexposure and overexposure should be anticipated depending on both the dosing strategy (fixed dose vs mg/kg). Also, the magnitude of the influence of body weight on clearance as the fold increase in clearance was found to vary between 1.0 and 1.7 for a 70 kg versus 140 kg individual. Furthermore, therapy optimisation is increasingly guided by model-informed decision making while individuals with obesity are not typically studied; hence, it remains uncertain whether models are fit for purpose in predicting exposure in individuals with obesity. In order to enable clinicians to individualise antimicrobial therapy in patients with obesity, determining the influence of body weight on exposure to antimicrobial agents should be done at an early stage, ideally from Phase I onwards, as it has proven to yield vital information for various antimicrobial agents.
We propose a call to action: patients with (extreme) obesity should be recognised as a special patient population during drug development, especially for antibacterial and antifungal agents given the strong exposure-response relationship.
References
Falagas ME. Obesity and infection. Lancet Infect Dis. 2006;6:438–46.
Ward ZJ, Bleich SN, Cradock AL, Barrett JL, Giles CM, Flax C, et al. Projected U.S. State-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381:2440–50
González-Muniesa P, Mártinez-González M, Hu F, Després J, Matsuzawa Y, Loos R, et al. Obesity. Nat Rev Dis Prim. 2017;3(17034).
Smit C, De Hoogd S, Brüggemann RJM, Knibbe CAJ. Obesity and drug pharmacology: a review of the influence of obesity on pharmacokinetic and pharmacodynamic parameters. 2018;14:275–85.
Lenoir C, Daali Y, Rollason V, et al. Impact of acute inflammation on cytochromes P450 activity assessed by the geneva cocktail. Clin Pharmacol Ther. 2021;109:1668–76.
van Rhee KP, Smit C, Wasmann RE, et al. Ciprofloxacin pharmacokinetics after oral and intravenous administration in (morbidly) obese and non-obese individuals; a prospective clinical study. Clin Pharmacokinet. 2022;61:1167–75.
Brill MJE, Houwink API, Schmidt S, et al. Reduced subcutaneous tissue distribution of cefazolin in morbidly obese versus non-obese patients determined using clinical microdialysis. J Antimicrob Chemother. 2014;69:715–23.
Dorn C, Petroff D, Stoelzel M, et al. Perioperative administration of cefazolin and metronidazole in obese and non-obese patients: a pharmacokinetic study in plasma and interstitial fluid. J Antimicrob Chemother. 2021;76:2114–20.
Zhang T, Krekels EHJ, Smit C, Knibbe CAJ. Drug pharmacokinetics in the obese population: challenging common assumptions on predictors of obesity-related parameter changes. Expert Opin Drug Metab Toxicol. 2022;18:657–74.
Chen L, van Rhee KP, Wasmann RE, et al. Total bodyweight and sex both drive pharmacokinetic variability of fluconazole in obese adults. J Antimicrob Chemother. 2022;77:2217–26.
Mellon G, Hammas K, Burdet C, et al. Population pharmacokinetics and dosing simulations of amoxicillin in obese adults receiving co-amoxiclav. J Antimicrob Chemother. 2020;75:3611–8.
Wasmann RE, Smit C, van Donselaar MH, et al. Implications for IV posaconazole dosing in the era of obesity. J Antimicrob Chemother. 2020;75:1006–13.
Smit C, Wasmann RE, Goulooze SC, et al. Population pharmacokinetics of vancomycin in obesity: finding the optimal dose for (morbidly) obese individuals. Br J Clin Pharmacol. 2020;86:303–17.
Wasmann RE, Smit C, van Dongen EPH, et al. Fixed dosing of liposomal amphotericin B in morbidly obese individuals. Clin Infect Dis. 2020;70:2213–5.
Wasmann RE, Smit C, ter Heine R, et al. Pharmacokinetics and probability of target attainment for micafungin in normal-weight and morbidly obese adults. J Antimicrob Chemother. 2019;74:978–85.
Smit C, Wasmann RE, Goulooze SC, et al. A prospective clinical study characterizing the influence of morbid obesity on the pharmacokinetics of gentamicin: towards individualized dosing in obese patients. Clin Pharmacokinet. 2019;58:1333–43.
Smit C, Wasmann RE, Wiezer MJ, et al. Tobramycin clearance is best described by renal function estimates in obese and non-obese individuals: results of a prospective rich sampling pharmacokinetic study. Pharm Res. 2019;36:112.
Wasmann RE, Ter Heine R, van Dongen EP, et al. Pharmacokinetics of anidulafungin in obese and normal-weight adults. Antimicrob Agents Chemother. 2018;62.
Pai MP. Pharmacokinetics of tedizolid in morbidly obese and covariate-matched nonobese adults. Antimicrob Agents Chemother. 2016;60:4585–9.
Pai MP. Serum and urine pharmacokinetics of tigecycline in obese class III and normal weight adults. J Antimicrob Chemother. 2014;69:190–9.
Busse D, Simon P, Schmitt L, et al. Comparative plasma and interstitial tissue fluid pharmacokinetics of meropenem demonstrate the need for increasing dose and infusion duration in obese and non-obese patients. Clin Pharmacokinet. 2022;61:655–72.
Kees MG, Weber S, Frieder K, Horbach T. Pharmacokinetics of moxifloxacin in plasma and tissue of morbidly obese patients. J Antimicrob Chemother. 2011;66:2330–5.
Dvorchik BH, Damphousse D. The pharmacokinetics of daptomycin in moderately obese, morbidly obese, and matched nonobese subjects. J Clin Pharmacol. 2005;45:48–56.
Justo JA, Mayer SM, Pai MP. Pharmacokinetics of ceftaroline in normal body weight and obese (classes I, II, and III) healthy adult subjects. Antimicrob Agents Chemother. 2015;59:3956–65.
Hall RG, Swancutt MA, Meek C, Leff R, Gumbo T. Weight drives caspofungin pharmacokinetic variability in overweight and obese people: fractal power signatures beyond two-thirds or three-fourths. Antimicrob Agents Chemother. 2013;57:2259–64.
Busse D, Simon P, Petroff D, et al. Similar piperacillin/tazobactam target attainment in obese versus nonobese patients despite differences in interstitial tissue fluid pharmacokinetics. Pharmaceutics. 2021;12:1380.
National Health and Nutrition Examination Survey (NHANES) 2017–2018 data documentation, codebook, and frequencies
Janmahasatian S, Duffull S, Ash S, Ward L, Byrne N, Green B. Quantification of lean bodyweight. Clin Pharmacokinet. 2005;44:1051–65.
McCarron M, Devine B. Gentamicin therapy. Drug Intell Clin Pharm. 1974;8:650–5.
Bauer LA, Edwards WAD, Dellinger EP, Simonowitz DA. Influence of weight on aminoglycoside pharmacokinetics in normal weight and morbidly obese patients. Eur J Clin Pharmacol. 1983;24:643–7.
Gregoire N, Chauzy A, Buyck J, Rammaert B, Couet W, Marchand S. Clinical pharmacokinetics of daptomycin. Clin Pharmacokinet. 2021;60:271–81.
Smit C, van Schip AM, van Dongen EPA, Brüggemann RJM, Becker ML, Knibbe CAJ. Dose recommendations for gentamicin in the real-world obese population with varying body weight and renal (dys)function. J Antimicrob Chemother. 2020;75:3286–92.
Soares ALPPDP, Montanha MC, Alcantara CDS, Silva SRB, Kuroda CM, Yamada SS, Nicacio AE, Maldaner L, Visentainer JV, Simões CF, Locatelli JC, Lopes WA, Mazucheli J, Diniz A, Paixão PJPA, Kimura E. Pharmacokinetics of amoxicillin in obese and nonobese subjects. Br J Clin Pharmacol. 2021;87:3227–33
Coates M, Shield A, Peterson GM, Hussain Z. Prophylactic cefazolin dosing in obesity—a systematic review. Obes Surg. 2022;32:3138–49.
Alobaid AS, Wallis SC, Jarrett P, Starr T, Stuart J, Lassig-Smith M, Mejia JL, Roberts MS, Sinnollareddy MG, Roger C, Lipman J, Roberts JA. Effect of obesity on the population pharmacokinetics of fluconazole in critically ill patients. Antimicrob Agents Chemother. 2016;60:6550–7.
Chung EK, Cheatham SC, Fleming MR, Healy DP, Kays MB. Population pharmacokinetics and pharmacodynamics of meropenem in nonobese, obese, and morbidly obese patients. J Clin Pharmacol. 2017;57:356–68.
Wittau M, Scheele J, Kurlbaum M, et al. Population pharmacokinetics and target attainment of meropenem in plasma and tissue of morbidly obese patients after laparoscopic intraperitoneal surgery. Antimicrob Agents Chemother. 2015;59:6241–7.
Pai MP, Cojutti P, Pea F. Pharmacokinetics and pharmacodynamics of continuous infusion meropenem in overweight, obese, and morbidly obese patients with stable and unstable kidney function: a step toward dose optimization for the treatment of severe gram-negative bacterial infections. Clin Pharmacokinet. 2015;54:933–41.
Maseda E, Grau S, Luque S, Castillo-Mafla MP, Suárez-de-la-Rica A, Montero-Feijoo A, Salgado P, Gimenez MJ, García-Bernedo CA, Gilsanz F, Roberts JA. Population pharmacokinetics/pharmacodynamics of micafungin against Candida species in obese, critically ill, and morbidly obese critically ill patients. Crit Care. 2018;22:94.
Wicha SG, Haak T, Zink K, Kees F, Kloft C, Kees MG. Population pharmacokinetics and target attainment analysis of moxifloxacin in patients with diabetic foot infections. J Clin Pharmacol. 2015;55:639–46.
Veillette JJ, Winans SA, Maskiewicz VK, Truong J, Jones RN, Forland SC. Pharmacokinetics and pharmacodynamics of high-dose piperacillin-tazobactam in obese patients. Eur J Drug Metab Pharmacokinet. 2021;46(3):385–94. https://doi.org/10.1007/s13318-021-00677-1. (Epub 2021 Mar 20).
Chung EK, Cheatham SC, Fleming MR, Healy DP, Shea KM, Kays MB. Population pharmacokinetics and pharmacodynamics of piperacillin and tazobactam administered by prolonged infusion in obese and nonobese patients. J Clin Pharmacol. 2015;55:899–908.
Alobaid AS, Wallis SC, Jarrett P, Starr T, Stuart J, Lassig-Smith M, Mejia JL, Roberts MS, Roger C, Udy AA, Lipman J, Roberts JA. Population pharmacokinetics of piperacillin in nonobese, obese, and morbidly obese critically ill patients. Antimicrob Agents Chemother. 2017;61:e01276-e1316.
Busse D, Simon P, Petroff D, Dorn C, Schmitt L, Bindellini D, Kratzer A, Dietrich A, Zeitlinger M, Huisinga W, Michelet R, Wrigge H, Kloft C. Similar piperacillin/tazobactam target attainment in obese versus nonobese patients despite differences in interstitial tissue fluid pharmacokinetics. Pharmaceutics. 2021;13:1380.
Wong S, Reuter SE, Jones GR, Stocker SL. Review and evaluation of vancomycin dosing guidelines for obese individuals. Expert Opin Drug Metab Toxicol. 2022;18:323–35.
EMA—summary of product characterisitics. https://www.ema.europa.eu/en/medicines. Accessed 26 Oct 2022.
FDA. Enhancing the diversity of clinical trial populations—eligibility criteria, enrollment practices, and trial designs guidance for industry. 2020.
European Medicines Agency. Reflection paper on investigation of pharmacokinetics and pharmacodynamics in the obese population. 2018 EMA/CHMP/535116/2016.
Wicha SG, Märtson AG, Nielsen EI, et al. From therapeutic drug monitoring to model-informed precision dosing for antibiotics. Clin Pharmacol Ther. 2021;109:928–41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Not applicable.
Conflict of interest
RB declares no interest with regard to this work. Outside of this work, he has served as consultant to and has received unrestricted research grants from Astellas Pharma Inc., F2G, Gilead sciences, Merck Sharpe and Dohme Corp., Mundipharma Inc., and Pfizer Inc. All payments were invoiced by the Radboud University Medical Center. PvdL declares membership of the compliance committee of STIZON and is treasurer of the Dutch Working party on Antibiotic Policy (SWAB). The remaining authors have no conflict of interest to declare.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Author contribution
KR, CK, PvdL, RB helped with conceptualisation of this personal view. KR helped with the original draft and visualisation. KR, CK and RB conducted data curation and formal analysis. CK, PvdL, RB helped with review and editing of the draft.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
van Rhee, K.P., Knibbe, C.A.J., van der Linden, P.D. et al. Patients with Obesity Should be Recognised as a Special Patient Population During Drug Development of Antibacterial and Antifungal Agents; A Call to Action. Clin Pharmacokinet 63, 1–12 (2024). https://doi.org/10.1007/s40262-023-01332-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-023-01332-5