Abstract
Introduction
Immune checkpoint inhibitors improved survival of advanced stage non-small cell lung cancer patients, but the overall response rate remains low. A biomarker that identifies non-responders would be helpful to allow treatment decisions. Clearance of immune checkpoint inhibitors is related to treatment response, but its prognostic potential early in treatment remains unknown. Our primary aim was to investigate the prognostic potential of nivolumab clearance for overall survival early in treatment. Our secondary aim was to evaluate the performance of nivolumab clearance as prognostic biomarker.
Patients and Methods
Individual estimates of nivolumab clearances at first dose, 6 and 12 weeks after treatment initiation were obtained via nonlinear mixed-effects modelling. Prognostic value of nivolumab clearance was estimated using univariate Cox regression at first dose and for the ratios between 6 and 12 weeks to first dose. The performance of nivolumab clearance as biomarker was assessed by calculating sensitivity and specificity.
Results
During follow-up of 75 months, 69 patients were included and 865 died. Patients with a nivolumab clearance ≥ 7.3 mL/h at first dose were more likely to die compared to patients with a nivolumab clearance < 7.3 mL/h at first dose (hazard ratio [HR] = 3.55, 955 CI 1.75–7.20). The HRs of dose nivolumab clearance ratios showed similar results with a HR of 3.93 (955 CI 1.66–9.32) for 6 weeks to first-dose clearance ratio at a 0.953 cut-point and a HR of 2.96 (955 CI 1.32–6.64) for 12 weeks to first-dose clearance ratio at a cut-point of 0.814. For nivolumab clearance at all early time points, sensitivity was high (≥ 0.95) but specificity was low (0.11–0.29).
Conclusion
Nivolumab clearance is indicative of survival early in treatment. Our results encourage to further assess the prognostic potential of immunotherapy clearance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Early biomarkers are needed to predict response to immune checkpoint inhibitors. |
The prognostic value of early immune checkpoint inhibitor clearance is unknown. |
We show that nivolumab clearance is indicative of survival in the first 12 weeks. |
1 Background
The introduction of immune checkpoint inhibitors has significantly improved the prognosis of advanced stage non-small cell lung cancer (NSCLC). Although this treatment modality greatly improved survival, still “only” half of all patients respond to immune checkpoint inhibitors [1]. Identification of non-responders can be difficult early in treatment as it is hard at this timepoint to distinguish pseudo-progression and late-response from non-response [2]. Therefore, approximately half of all advanced stage NSCLC patients treated with immune checkpoint inhibitors, are exposed to a treatment they will not benefit from. To minimise unnecessary toxicity, morbidity and costs of ineffective treatment, early identification of immune checkpoint inhibitor non-responders is of urgent need.
There is accumulating evidence that (change in) clearance of immune checkpoint inhibitors (mainly aspecific degradation) may serve as an early monitoring biomarker for non-response to immune checkpoint inhibitors [3,4,5,6]. These studies all demonstrated that both higher immune checkpoint inhibitor clearance at first dose and smaller or no decrease in clearance after first dose are related to poor responses to therapy.
However, it remains unclear whether immune checkpoint inhibitor clearance could be used to identify non-responders early in treatment. Essential information, including the optimal immune checkpoint inhibitor clearance cut-point and the performance of clearance as biomarker in terms of sensitivity and specificity is missing for evaluating its clinical utility to assess survival. Therefore, our primary aim was to study the prognostic potential of immune checkpoint inhibitor clearance early in NSCLC treatment to assess overall survival (OS), considering optimal cut-points. Our secondary aim was to study the performance of immune checkpoint inhibitor clearance as prognostic biomarker. Samples and data were only available from patients who received treatment with nivolumab. This article therefore focuses on nivolumab as immune checkpoint inhibitor.
2 Methods
This study was conducted and reported in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines [7].
2.1 Study Population
Patients were not recruited for this study. Samples and data were obtained from patients included in a prospective fluid phase biopsy study (N13FPB). These patients were treated at the Netherlands Cancer Institute between 2015 and 2018. This study was approved by the Medical Ethics Committee of the Netherlands Cancer Institute. Informed consent was obtained from all individual participants included in the study. Patients were included in the N13FPB study using the following criteria: aged ≥ 18 years; cytologically/histologically confirmed advanced stage (IIIB and IV) NSCLC; Eastern Cooperative Oncology Group (ECOG) performance score 0–2 at baseline and written informed consent. Patients were included in our study using the following additional criterion: at least 2 nivolumab concentration measurements available in the first 4 months of nivolumab treatment.
2.2 Data Collection
The following data were collected: gender, age at time of first administration, bodyweight, ECOG and albumin concentration at start of treatment, nivolumab dose and time of administration and survival data. Peak and trough nivolumab plasma concentrations were collected for the first 4 months of nivolumab treatment and quantified using a validated bioanalytical assay. As the extent of change of nivolumab clearance may be indicative of survival, the prognostic potential of change of nivolumab clearance from the first nivolumab dose to 6 and 12 weeks after the first nivolumab dose was calculated and compared. For these calculations, the 6 and 12 weeks to first-dose clearance ratios were calculated. These time points were chosen to align with RECIST evaluation version 1.1 at 6 and 12 weeks [8]. Empirical Bayesian estimates for individual nivolumab clearance were obtained by means of nonlinear mixed-effects modelling and a previously developed validated population pharmacokinetic model of nivolumab [9] using the software package NONMEM version V7.5 (ICON, Ireland).
2.3 Statistical Analyses
To investigate the prognostic potential of nivolumab clearance for OS as a primary endpoint, survival time differences were compared by means of log-rank tests using Kaplan-Meier analyses. These analyses were performed for the estimated nivolumab clearance at first dose as well as the ratio of the estimated nivolumab clearance from the first dose to 6 and 12 weeks. To adjust for multiple testing of the prognostic value of nivolumab clearance on these three time points on the same dataset, we performed a Bonferroni correction; a p-value of 0.0167 (0.05/3) was considered statistically significant. In order to divide the dataset into two groups for univariate analyses based on nivolumab clearance, optimal cut-points in nivolumab clearance were calculated using maximally selected rank statistics. This method aims to maximise the statistical significance between these groups based on differences in OS. We used the rank sum statistic, based on the Wilcoxon rank-sum test, to evaluate the association between nivolumab clearance and OS. The optimal cut-point was chosen as the one with the highest rank sum statistic, enabling us to analyse the relationship between nivolumab clearance and OS more effectively. Secondary, the performance of nivolumab clearance as prognostic biomarker was assessed by calculating sensitivity, specificity and accuracy for the outcome “non-response” with standardised formulas. For these calculations, patients were categorised as non-responder if they died (any cause) within 6 months from start of treatment with nivolumab, as this corresponds to the OS of patients who receive best supportive care (BSC) as 2nd line of treatment [10]. As the purpose of our analysis was to distinguish non-responders with high certainty, the aimed specificity for our analyses was > 0.95. All statistical analyses were performed using R, with Rstudio version 1.1.463 as interface and using packages “survminer”, “ggplot2” and “maxstat” [11,12,13].
3 Results
3.1 Patient Characteristics
In our cohort of 69 patients, the median age was 64 years and median bodyweight 74 kg. The majority of patients was male (615). The ECOG performance score was 0 or 1 before start of nivolumab treatment for 905 of the patients and median albumin was 42 mg/mL. Treatment with nivolumab was mainly (715) administered as 2nd line treatment. Because testing for programmed death-ligand 1 (PD-L1) expression was not standard-of-care during the study period, PD-L1 expression was partly unknown (N = 24 missing, 355). All patients were immunotherapy-naive and received nivolumab as monotherapy. No ROS1, ALK or classic EGFR mutations were found in our study population (Supplementary Material 1). Patients in our cohort had a median OS of 11 months and according to our definition, 705 of the patients responded to nivolumab therapy (i.e., did not die within 6 months). At the end of data collection in July 2022 and a follow-up of 75 months, 865 of all patients died. A summary of the study population characteristics is presented in Table 1. Information on observed nivolumab measurements versus time after last dose and the model code can be found in Supplementary Material 2 and 3, respectively.
3.2 Prognostic Potential of Nivolumab Clearance
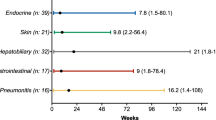
To predict OS, the optimal cut-point for nivolumab clearance at first dose was estimated to be 7.3 mL/h by maximally selected rank statistics. Patients with a nivolumab clearance ≥ 7.3 mL/h at first dose were more likely to die during the study compared to patients with a nivolumab clearance <7 .3 mL/h at first dose (HR = 3.55, 955 CI 1.75–7.20, p = 0.00045) (Fig. 1). Median OS was 10.6 months for patients with a nivolumab clearance ≥ 7.3 mL/h at first dose and 32.4 months for patients with a nivolumab clearance < 7.3 mL/h. Baseline albumin was not significantly lower in patients with high nivolumab clearance at first dose compared to patients with low nivolumab clearance at first dose (mean 42 vs 43 mg/mL, respectively, p = 0.1083). Sensitivity of clearance at first dose to distinguish non-responders was high (0.95), but accuracy was low (0.49) due to a high false-positive rate (635) (Table 2 and Supplementary Material 4).
For the 6 weeks to first-dose ratio of nivolumab clearance, the optimal cut-point was estimated to be 0.953 by maximally selected rank statistics. Patients with a 6 weeks to first-dose clearance ratio ≥ 0.953 were more likely to die during the study period compared to patients with a ratio < 0.953 (HR = 3.93, 955 CI 1.66–9.32, p = 0.00191) (Fig. 1). Median OS was 10.9 months for patients with a 6 weeks to first-dose ratio of nivolumab clearance ≥ 0.953 and 38.2 months for patients with a 6 weeks to first-dose ratio of nivolumab clearance < 0.953. Sensitivity of the change of nivolumab clearance from first dose to 6 weeks to distinguish non-responders was optimal (1), but accuracy was again low (0.43) due to a high false-positive rate (655) (Table 2 and Supplementary Material 4).
For the 12 weeks to first-dose ratio of nivolumab clearance, the optimal cut-point was estimated to be 0.814 by maximally selected rank statistics. Patients with a 12 weeks to first-dose clearance ratio ≥ 0.814 were more likely to die during the study period compared to patients with a ratio < 0.814 (HR = 2.96, 955 CI 1.32–6.64, p = 0.00823) (Fig. 1). Median OS was 10.9 months for patients with a 12 weeks to first-dose ratio of nivolumab clearance ≥ 0.814 and 35.0 months for patients with a 12 weeks to first-dose ratio of nivolumab clearance < 0.814. Again, sensitivity was optimal (1) but accuracy was low (0.43) due to the high false-positive rate (635) (Table 2 and Supplementary Material 4).
4 Discussion
This is the first study that explored the prognostic potential of nivolumab clearance on early time points. Our analyses revealed that nivolumab clearance at first dose, as well as the subsequent changes in nivolumab clearance over 6 and 12 weeks, hold significant prognostic potential for survival among NSCLC patients undergoing nivolumab treatment. Moreover, our findings suggest that changes in nivolumab clearance over 6 and 12 weeks do not confer superior prognostic potential when compared to nivolumab clearance at first dose.
Previous research has demonstrated that high nivolumab clearance is linked with shorter survival among lung cancer patients in contrast to those with low nivolumab clearance [3, 14, 15]. Our study supports these findings and provides valuable information regarding the sensitivity and specificity required for predicting non-response to treatment, which is critical for evaluating the clinical potential of prognostic biomarkers. The use of immune checkpoint inhibitor clearance as an early survival biomarker offers practical advantages, as quantitative assays for these monoclonal antibodies are widely available [16,17,18,19]. These biomarkers are determined through blood sampling, which can be easily combined with routinely performed blood sampling in daily clinical practice to minimise invasiveness.
Our study had some limitations. We aimed for high specificity (≥ 0.95) to enable physicians to stop immune checkpoint inhibitor treatment for non-responding patients. However, high specificity was not reached, which may be due to two decisions in our used method. Our definition of non-response (see Methods) was based on the OS of patients receiving BSC as second-line treatment who may have been unfit for systemic treatment [10]. Although the majority of our study population also consisted of patients who received nivolumab as second-line treatment, they were in a generally good condition, as reflected by their ECOG performance score of 0–1. Thus, our study participants had a median survival longer than 6 months, which resulted in a high false-positive rate (Supplementary Material 3) and low specificity. Additionally, our cut-points of nivolumab clearance were calculated by maximally selected rank statistics based on OS and not specifically on “non-response”, contributing to low specificity. However, high sensitivity may also be valuable for treatment decisions, as it indicates responders with high certainty, which enables the treating physician to reduce intensity of follow-up. The generalisability of our findings to the first-line setting with pembrolizumab remains to be investigated, but we expect similar potential to distinguish treatment non-response because the pharmacokinetic characteristics overlap. Furthermore, the retrospective study design may have resulted in missing data and smaller sample size, potentially contributing to selection bias and lower accuracy. Our dataset lacked complete information regarding PD-L1 expression and tumour histology for some participants, which may have contributed to variations in treatment response. However, we did not identify any genetic alterations that influence the response to nivolumab treatment. Therefore, we do not anticipate that the absence of tumour histology data compromises the validity of our results. The retrospective design of our study could also have contributed to the selection of subjects in a relatively good condition as their follow-up was more complete.
One could also argue that the underlying mechanism for differences in nivolumab clearance i.e., cachexia, could directly explain differences in non-response or survival. Cachexia, characterised by lower body weight, worse performance scores and hypoalbuminaemia due to increased catabolism [20, 21], among other symptoms, could theoretically account for differences in nivolumab clearance and possibly explain variations in non-response or survival. Although in our population albumin levels were not significantly different between patients with high and low nivolumab clearance at first dose, we cannot rule out that cachexia is an independent marker for survival. Moreover, the selection of subjects with a relatively good performance score in our study could result in relatively low nivolumab clearance, as cachexia is related to high nivolumab clearance via increased catabolism [22]. However, median nivolumab clearance estimated in our dataset of 9.4 mL/h is comparable to previously reported values (9.5 mL/h) [23]. The retrospective study design also forced to estimate nivolumab clearance largely (975) on trough concentrations. Even though trough concentrations provide better information regarding clearance than peak concentrations, richer sampling would help to estimate the individual nivolumab clearance.
Despite these limitations, multiple advantages of this study can be noted. First, OS as response measure is an objective endpoint, which facilitates straightforward interpretation and easy reproducibility for clinical validation, in contrast to endpoints like best overall response, which is based on imaging using RECIST version 1.1 [8]. Also, survival data were known for the majority of our subjects and a long-term date last known alive (3 months to 6 years after start nivolumab treatment) was known for the remainder, which resulted in thorough survival analyses.
Because a considerable number of NSCLC patients treated with immune checkpoint inhibitors do not respond to therapy, there is an urgent need for tools that can help us detect non-response early during treatment. Our results show that nivolumab clearance early in treatment is indicative of primary immunotherapy resistance in NSCLC patients. These results are promising for the prognostic potential of pembrolizumab clearance, which is currently used as first-line treatment of NSCLC.
Abbreviations
- BMI:
-
Body Mass Index
- ECOG:
-
Eastern Cooperative Oncology Group
- HR:
-
Hazard Ratio
- IQR:
-
Inter Quartile Range
- NSCLC:
-
Non-Small Cell Lung Cancer
- OS:
-
Overall Survival
- PD-L1:
-
Programmed death-ligand 1
- RECIST:
-
Response Evaluation Criteria In Solid Tumours
- TBW:
-
Total bodyweight
References
Miao K, Zhang X, Wang H, Si X, Ni J, Zhong W, et al. Real-world data of different immune checkpoint inhibitors for non-small cell lung cancer in China. Front Oncol. 2022;12:859938.
Humbert O, Chardin D. Dissociated response in metastatic cancer: an atypical pattern brought into the spotlight with immunotherapy. Front Oncol. 2020;10:566297.
Liu C, Yu J, Li H, Liu J, Xu Y, Song P, et al. Association of time-varying clearance of nivolumab with disease dynamics and its implications on exposure response analysis. Clin Pharmacol Ther. 2017;101(5):657–66.
Li H, Yu J, Liu C, Liu J, Subramaniam S, Zhao H, et al. Time dependent pharmacokinetics of pembrolizumab in patients with solid tumor and its correlation with best overall response. J Pharmacokinet Pharmacodyn. 2017;44(5):403–14.
Turner DC, Kondic AG, Anderson KM, Robinson AG, Garon EB, Riess JW, et al. Pembrolizumab exposure-response assessments challenged by association of cancer cachexia and catabolic clearance. Clin Cancer Res. 2018;24(23):5841–9.
Wilkins JJ, Brockhaus B, Dai H, Vugmeyster Y, White JT, Brar S, et al. Time-varying clearance and impact of disease state on the pharmacokinetics of avelumab in merkel cell carcinoma and urothelial carcinoma. CPT Pharmacomet Syst Pharmacol. 2019;8(6):415–27.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Zhang J, Sanghavi K, Shen J, Zhao X, Feng Y, Statkevich P, et al. Population pharmacokinetics of nivolumab in combination with ipilimumab in patients with advanced malignancies. CPT Pharmacometrics Syst Pharmacol. 2019;8(12):962–70.
Wao H, Mhaskar R, Kumar A, Miladinovic B, Djulbegovic B. Survival of patients with non-small cell lung cancer without treatment: a systematic review and meta-analysis. Syst Rev. 2013;2(1):10.
Kassambara A, Kosinski M, Biecek P. Survminer: Drawing Survival Curves using 'ggplot2'. R package version 0.4.9. 2021. https://CRAN.R-project.org/package=survminer.
Wickham H. ggplot2: Elegant Graphics for Data Analysis: Springer-Verlag New York; 2016. https://ggplot2.tidyverse.org.
Hothorn T. maxstat: Maximally Selected Rank Statistics. 2017. R package version 0.7-25. https://CRAN.R-project.org/package=maxstat.
Hurkmans DP, Basak EA, van Dijk T, Mercieca D, Schreurs MWJ, Wijkhuijs AJM, et al. A prospective cohort study on the pharmacokinetics of nivolumab in metastatic non-small cell lung cancer, melanoma, and renal cell cancer patients. J Immunother Cancer. 2019;7(1):192.
Feng Y, Wang X, Bajaj G, Agrawal S, Bello A, Lestini B, et al. Nivolumab exposure-response analyses of efficacy and safety in previously treated squamous or nonsquamous non-small cell lung cancer. Clin Cancer Res. 2017;23(18):5394–405.
Millet A, Khoudour N, Guitton J, Lebert D, Goldwasser F, Blanchet B, et al. Analysis of pembrolizumab in human plasma by LC-MS/HRMS. Method validation and comparison with elisa. Biomedicines. 2021;9(6):621.
Basak EA, Wijkhuijs AJM, Mathijssen RHJ, Koolen SLW, Schreurs MWJ. Development of an enzyme-linked immune sorbent assay to measure nivolumab and pembrolizumab serum concentrations. Ther Drug Monit. 2018;40(5):596–601.
Pluim D, Ros W, van Bussel MTJ, Brandsma D, Beijnen JH, Schellens JHM. Enzyme linked immunosorbent assay for the quantification of nivolumab and pembrolizumab in human serum and cerebrospinal fluid. J Pharm Biomed Anal. 2019;164:128–34.
Chiu HH, Liao HW, Shao YY, Lu YS, Lin CH, Tsai IL, et al. Development of a general method for quantifying IgG-based therapeutic monoclonal antibodies in human plasma using protein G purification coupled with a two internal standard calibration strategy using LC-MS/MS. Anal Chim Acta. 2018;1019:93–102.
Evans WJ, Morley JE, Argilés J, Bales C, Baracos V, Guttridge D, et al. Cachexia: a new definition. Clin Nutr. 2008;27(6):793–9.
Fearon KC, Voss AC, Hustead DS. Definition of cancer cachexia: effect of weight loss, reduced food intake, and systemic inflammation on functional status and prognosis2. Am J Clin Nutr. 2006;83(6):1345–50.
Puszkiel APBR, Arrondeau J, Wislez M, Fabre-Guillevin E, Bianconi G, Declèves X, Jouinot A, De Percin S, Alexandre J, Goldwasser F, Blanchet B. 1073P - Relationship between basal metabolism, nivolumab clearance and survival in metastatic non-small cell lung cancer patients of the ELY study. Ann Oncol. 2022;33:S448–554.
U.S. Food and Drug Administration (FDA). Center for Drug Evaluation and Research. Clinical Pharmacology and Biopharmaceutics Review OPDIVO (Nivolumab). 2014. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/125554orig1s000clinpharmr.pdf.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
Ethics Approval and Consent to Participate
The study (N13FPB) in which the subjects participated was approved by the Medical Ethics Committee of the Netherlands Cancer Institute.
Consent for Publication
Not applicable.
Availability of Data and Material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Authors' Contributions
RtH, MvdH, SAB, BP and LSO conceived of the presented research idea RS, DvdH, SB and LSO collected data and samples. LSO, DvdH and EB took the lead in designing the analysis, LSO performed the analysis. MS, RtH, BP, MvdH and EB contributed to the interpretation of the results: LSO wrote the manuscript with input from all authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Otten, L.S., Piet, B., van den Haak, D. et al. Prognostic Value of Nivolumab Clearance in Non-Small Cell Lung Cancer Patients for Survival Early in Treatment. Clin Pharmacokinet 62, 1749–1754 (2023). https://doi.org/10.1007/s40262-023-01316-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-023-01316-5