Abstract
Introduction
The aim of this work is to compare the Corvis ST stress–strain index (SSI) and highest concavity (HC) parameters at baseline and 1 month after initiating monotherapy with prostaglandin analogues (PGs) in eyes showing visual field (VF) progression or stability.
Methods
In this prospective, single-center, observational study, newly diagnosed and treatment-naïve OAG patients were examined at baseline and 1 month after beginning monotherapy with topical PGs monotherapy. Goldmann applanation tonometry pressure readings, Corneal Hysteresis (ORA-CH), and the Corvis ST measurements were obtained at both visits. VF progression (Humphrey) was evaluated based on data from 6 years of follow-up after the baseline visit. Stress–strain index (SSI) and HC parameters in progressing (P) and non-progressing (NP) eyes were the main outcome measures.
Results
Sixty-three eyes were analyzed; mean age was 64.63 ± 11.26 years; 47 eyes were NP and 16 eyes were P according to the event analysis performed by the Humphrey device. There were no significant differences in IOP, CCT, or Corvis parameters between NP and P groups at baseline. Nevertheless, at 1 month, the SSI index was 1.60 ± 0.34 vs. 1.80 ± 0.34 (p = 0.003) in NP vs. P eyes, respectively. HC parameters were different between the groups at 1 month (p < 0.05) suggesting an increased scleral rigidity in the P group. There was no significant difference in IOP between groups at 1 month.
Conclusions
The Corvis ST provides a corneal rigidity index (SSI) that seems to be related to VF progression when measured 1 month after initiating PGs monotherapy. Differences in HC parameters, indicative of increased scleral stiffness, are also evident at 1 month on latanoprost in the P eyes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Biomechanical parameters of the eye have been proven clinically relevant, both in the measurement of intraocular pressure and in risk profiling of glaucoma patients. |
The purpose of the present study is to compare the dynamic corneal response parameters obtained with the Corvis ST in newly diagnosed and treatment-naïve patients at baseline and 1 month after initiating monotherapy with latanoprost in eyes showing visual field progression or stability after 6 years of follow-up. |
The stress–strain index (SSI) index and highest concavity (HC) parameters were different between the progressing and non-progressing groups at 1 month, suggesting an increased scleral rigidity in the eyes showing progression. |
SSI and HC parameters, measured with the Corvis ST represent biomarkers for future visual field progression when measured 1 month after initiating prostaglandin monotherapy. |
Introduction
Glaucoma is a progressive optic neuropathy characterized by a pattern of optic disc changes and associated irreversible visual field loss [1]. Glaucoma pathogenesis remains unclear, and several hypotheses have been proposed to explain the multitude of phenotypes, such as the mechanical damage theory. In this theory, intraocular pressure (IOP)-related stress (force/cross-sectional area) and strain (local deformation of the tissues) are thought to play a key role in the development of optic nerve head (ONH) changes, causing alterations in the lamina cribrosa, the peripapillary sclera, and their blood supply [2].
IOP is the main biomechanical risk factor for glaucoma. It is currently understood that material properties of the ocular wall and geometry of the eye are also important. A thin central corneal thickness (CCT) is recognized as a risk factor for glaucoma, both due to the noise it brings to the measurement of IOP, but also because it may act as a surrogate of the biomechanical susceptibility to suffer ONH damage in glaucomatous eyes [3,4,5,6]. However, other factors beyond CCT are also regarded as important, and cornea biomechanics seem to play a role in the pathogenesis of glaucoma subtypes [7].
The hypothesis relating corneal biomechanics to glaucoma progression is that the biomechanical properties of the cornea may be somehow related to those of the lamina cribrosa and/or the peripapillary sclera, which determine the response of the optic nerve to IOP. Assessment of corneal biomechanics may, therefore, offer an indirect measurement of the lamina cribrosa/posterior sclera rigidity, and thus behave as a surrogate for the optic nerve susceptibility to glaucomatous damage.
Corneal biomechanics can be currently evaluated in vivo with two devices; the Ocular Response Analyser (ORA) and the Corvis Scheimpflug tonometer (Corvis ST, OCULUS, Wetzlar, Germany). Corvis ST provides several biomechanical parameters, many of which are interrelated. It uses algorithms to analyze Scheimpflug images of the cornea reaction to an air pulse. It offers a unique clinical and experimental tool with good repeatability and reproducibility [8].
In addition, prostaglandin analogues (PGs) are commonly used as first-line therapy in glaucoma. Our group recently reported the biomechanical changes induced by latanoprost therapy [9]. Understanding the effects of PGs on the biomechanical behavior of the eye is important and it may confer information about the risk of future glaucoma progression [10].
The purpose of the present study is to compare the dynamic corneal response parameters (DCR) obtained with the Corvis ST in newly diagnosed and treatment-naïve patients at baseline and 1 month after initiating monotherapy with latanoprost in eyes showing visual field (VF) progression or stability after 6 years of follow-up.
Methods
Patients were prospectively enrolled from the Glaucoma Unit at the Hospital Universitario Príncipe de Asturias. This was a prospective, single-center, observational cohort study. Patients with ocular hypertension (OHT) or primary open-angle glaucoma (POAG) were recruited. The study protocol was explained to eligible patients and they were allowed to enter the study after signing an informed consent. The study followed the tenets of the Declaration of Helsinki and the protocol was approved by the Institutional Review Board (CEIM) Hospital Universitario Principe de Asturias with the number OE 15/2020. The study protocol has been previously published by our group [9].
Patients were examined at baseline, 1 month, 3 months, 6 months after initiation of prostaglandin analogue monotherapy and then every 6 months up to 6 years. The diagnosis of POAG was based on the typical glaucomatous optic neuropathy (GON) appearance and the corresponding visual field defects in the absence of signs of secondary open-angle glaucoma [1]. Only eyes with mild VF defects based on Hodapp–Parrish–Anderson criteria were included in the study. The diagnosis of ocular hypertension (OHT) was based on the finding of at least two GAT IOP measurements exceeding 24 mmHg performed on two separate days with normal findings in white-on-white 24–2 SITA standard visual field testing and without any signs of GON. Only patients with newly diagnosed POAG or OHT were included to ensure that no eye had been treated with antiglaucoma drugs before entry into the study.
A complete ocular examination was performed at the baseline visit, including measurement of best-corrected visual acuity, Goldmann applanation tonometry (GAT), intraocular pressure (IOP), ultrasound central corneal pachymetry (CCT), gonioscopy, dilated fundoscopy and OCT scanning of the retinal nerve fiber layer in the optic disc using the Cirrus OCT (Carl Zeiss Meditec, Oberkochen, Germany). Corvis ST (Oculus, Wetzlar, Germany) Dynamic corneal response parameters were recorded at baseline and at the 1-month follow-up visit after initiation of latanoprost monotherapy. Measurement of corneal hysteresis (CH) with the Ocular Response Analyzer (Reichert Ophthalmic Instruments, NY, USA) was also performed at baseline and at 1 month on latanoprost therapy. Visual field testing was performed with the Humphrey Visual Field Analyzer (Carl Zeiss Meditec, Oberkochen, Germany), using the white-on-white 24–2 Swedish Interactive Threshold Algorithm (SITA) standard strategy. Visual fields were performed at baseline and also at 6-month intervals up to 6 years to document progression.
Event-based analysis was used in this study to detect progression. The event-based pointwise changes on 24-2 tests in the validation cohort were determined using two progression criteria: at least three progressing VF locations on two or three consecutive tests were flagged as “possible” and “likely” progression respectively, and were considered both as progression (P group). When these assumptions were not fulfilled, the eye was grouped as non-progressing (NP).
Exclusion criteria included the presence of corneal disease, history of intraocular surgery or laser refractive surgery, IOP exceeding 35 mmHg without treatment, presence of moderate or severe visual field defects, systemic treatment with medications that could affect the IOP, including steroids, beta blockers, etc. Myopia higher than 6 diopters (sph equivalent), Hyperopia higher than 3 D or astigmatism higher than 3 D were also exclusion criteria.
Parameters used from ORA were corneal hysteresis (CH) and corneal compensated IOP (IOPcc). For analysis of Corvis parameters the software version 1.6b2015 was used. Biomechanically corrected IOP (bIOP) was quantified. Stress–strain index (SSI), biomechanical glaucoma factor (BGF), and highest concavity (HC) parameters were measured at baseline and 1-month follow-up. HC parameters included the length of the arc at the highest concavity (HC dArc length), the time from the onset of the deformation to the maximum concavity (HC deflection time), and the length of the corneal deflection at the time of highest concavity (HC deflection length) and stiffness parameter at HC (SP HC).
Therefore, our study has three important timepoints; the baseline visit (when all baseline evaluations are performed as mentioned above), the month 1 visit (when IOP and biomechanical parameters are again tested, on latanoprost monotherapy) and the 6 years of follow-up timepoint, when eyes are grouped as P and NP, based on whether “possible” or “likely” progression has occurred until that timepoint.
Statistical analysis was performed with StatPlus software (AnalystSoft Inc.). Data are presented as mean ± standard deviation. Comparisons with the paired t test before and after, and the independent samples using the Mann–Whitney U test.
Results
Sixty-three eyes from 36 patients were analyzed. Sixteen eyes had OHT and 47 eyes had POAG. Mean age was 64.63 ± 11.26 years. There were 24 men’s eyes and 39 women’s eyes. Patients’ baseline characteristics are summarized in Table 1. All patients had 6 years of VF data.
When analyzing data from the whole cohort of patients, there is a statistically significant difference in variables of interest comparing baseline visit and month 1 visit. There is a decrease in IOP, a finding that is consistent when comparing either tonometry method, including GAT IOP, bIOP, IOPcc and IOPnct (see Table 2). There are also marked changes in a series of biomechanical parameters, including SSI, HC dARC length, HC time, HC deflection length, and SP HC at the 1-month visit.
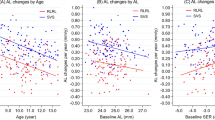
Event-based analysis marked 47 eyes as NP and 16 eyes as P during the 6 years of follow-up. The two groups differed in age, with the progressing group being older than the non-progressing group. A mean change in mean deviation (MD) of − 0.17 ± 4.43 db vs. − 5.87 ± 5.12 db (p < 0.001) was seen in the NP and P groups, respectively. No significant differences were observed in IOP or any other baseline parameter, including SSI, between the two groups (as shown in Table 3). The visual field index VFI decreased from − 0.76 ± 2.95% to − 2.68 ± 1.66% (p = 0.001) in the NP and P groups, respectively, during the period of 6 years.
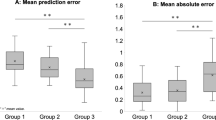
Nevertheless, in the 1 month follow-up exam, the SSI was found to be significantly lower in the NP compared to the P group (1.60 ± 0.34 vs 1.90 ± 0.34, p = 0.003), while CH (mmHg) was 10.26 ± 1.73 vs 9.34 ± 1.59 in the respective groups and failed to reach the level of significance (p = 0.06) (Table 4). Interestingly, no significant difference was found between groups in the amount of change of the SSI at 1 month from baseline. Therefore, it was only the difference in SSI at 1 month that was significant between the groups, not the initial (baseline) value or the change vs baseline. Furthermore, there was no difference between the P and NP groups in the IOP (measured with any tonometer) at 1 month.
At 1-month follow-up, HC parameters were also found to differ between the two groups. A higher value in the SP HC and in the HC deflection time is observed in patients who progress (see Table 4). These patients have higher scleral rigidity. On the other hand, lower values are observed in the HC length parameters, thus meaning that P eyes had a higher scleral rigidity. Finally, the BGF was similar in the P and NP groups both at baseline and at 1 month (see Tables 3 and 4).
Discussion
In the present study, we report that SSI and some HC parameters, measured at 1 month after initiation of latanoprost monotherapy, could be used as a biomarker for future visual field progression. This finding is clinically important since the estimated risk for progression can guide clinical decision-making, frequency of monitoring, as well as the threshold for more aggressive treatment. SSI measured at 1 month while on latanoprost treatment was higher in the eyes that progressed compared to the ones that remained stable over 6 years of follow-up, while SSI showed similar values between the two groups when measured at baseline. Therefore, it may represent an early biomarker for VF progression.
There is evidence that PGs, being a first-line glaucoma therapy, alter the biomechanics of the cornea and the sclera. Latanoprost affects tonometric readings obtained with various methods, providing indirect support of the hypothesis for its effect on the viscoelastic properties of the cornea [11]. PGs use has been associated with changes in the anterior chamber volume and decrease in the anterior chamber depth, while they appear not to have an effect on the shape of the cornea [12]. Studies have already reported altered biomechanics of the eye attributed to PG therapy [12, 13]. In a recent report by our group, we found that SSI decreases significantly after 6 months of latanoprost use in POAG and OHT eyes [9]. It is imperative to mention that IOP level is an important confounding factor in many biomechanical parameters [14].
In the present study, we report that SSI, BGF, and HC parameters are significantly altered compared to baseline at 1 month of treatment. Therefore, latanoprost use seems to affect IOP and also a list of biomechanical parameters, some of which are known to be influenced by IOP, while others, such as the SSI, are regarded as non-IOP-correlated [15]. The changes induced in SSI and HC parameters provide an understanding that latanoprost induces a softening effect in the rigidity of both the cornea and the sclera, with changes in the material properties that could potentially even reach the peripapillary sclera. It is, however, unknown if the effects of PGs are reversed with PGs discontinuation and the timeframe within which this happens.
The SSI was introduced in fact recently as a novel metric that characterizes the material stiffness of the cornea, irrespective of the level of both IOP and CCT [15]. A higher SSI signifies a higher stiffness of the cornea. There is evidence from a cross-sectional study that treatment-naïve POAG eyes have a higher SSI when compared to control eyes [16]. There is no study in the literature to our knowledge to evaluate the role of SSI in the risk for glaucoma progression.
The ability to estimate the risk of progression using biomarkers at the beginning of glaucoma monitoring is crucial for the glaucoma patient, since risk profiling can aid the clinician to intensify treatment when needed and allocate resources more wisely. Being able to characterize the role of biomechanics may also help us understand why eyes with controlled IOP progress and others remain stable [17]. Our data show that the value of SSI and HC variables at 1 month, not at baseline, neither their change versus baseline, differs between those that progress and those that remain stable. Therefore, it is expected that those eyes that are less stiff at 1 month, irrespective of their starting point, are the ones less likely to progress. It is also understood that this difference is evident as quickly as 1 month after starting latanoprost drops, therefore it represents a fast response of the eye to the drug.
It is important to note that the two groups, those who progressed and those who did not, had similar IOPs at baseline and at subsequent follow-ups. The main difference between the two groups was in age; the P group was older. Interestingly, the SSI at baseline or the change in SSI between the first month and at baseline did not differ between the groups. It is possible that those who reach a low SSI at 1 month, either because they start from a lower SSI at baseline or because they demonstrate a larger decrease in SSI from baseline due to treatment, are more protected against VF progression.
Certain highest concavity parameters, including HC dARC length, HC time, and HC deflection length, were also different between the P and NP groups at 1 month on latanoprost. The data point to the direction that at 1 month, when we evaluate the hypotonic effect of the PG treatment is also a timepoint when we can also get an estimate of the risk for future progression. The value of the HC deflection length and the HC dARC length are significantly smaller in progressors. A higher value in the HC deflection time is observed in patients who progress. These differences point to a higher scleral rigidity in the P group. These parameters seem to better characterize the biomechanical properties of the sclera, rather than the cornea [18, 19]. Moreover, taking into account that bIOP was similar in both at baseline and also at the 1-month examinations between the two groups, it is inferred that the change is HC parameters represents in fact a difference in the scleral biomechanical properties.
There are only a few studies in the literature that have examined the relationship between the Corvis parameters and the risk of future glaucoma progression. In a large prospective study, Qassim et al. followed glaucoma-suspect eyes and investigated the value of stiffness parameter at 1st applanation (SP-A1) and SP HC as a risk factor for progression with VF or OCT [20]. They reported that eyes with corneas with higher stiffness parameters and thinner corneas present a greater risk of progression. It is also reported that both of these parameters are correlated with IOP and CCT. Nevertheless, we have to take into account that in that study, 23% of eyes were already under treatment at baseline. Aoki et al. have shown that the corneal concavity shape is closely related to VF progression in a cohort of myopic eyes that were under treatment [21]. Jung et al. showed that greater corneal deflection amplitude was related with faster progression [22]. Finally, Aoki showed that the biomechanical glaucoma factor is not useful in assessing the risk of progression or in discriminating between glaucoma and controls [23]. Future research may help us better understand the value of each of the above parameters.
The clinical results from the present study may be explained when taking into consideration the role of PGs at the molecular level. PGs upregulate the expression of matrix metalloproteinases (MMPs), therefore promoting the degradation of collagen of the extracellular matrix in the eye [24]. This finding has recently been shown again in an ex vivo human cornea model and it was also associated in the same corneas with an increase in measured CH [25]. Prostaglandin F2a analogs also decrease the expression of tissue inhibitors of metalloproteinases (TIMPs), which results in an increased turnover of collagen fibers and an increased outflow via the uveoscleral route. Therefore, apart from their effects on IOP, they are acting on the corneal biomechanics, thereby affecting tonometry readings more or less, depending on the tonometer used, and they can also be affecting the scleral biomechanics with a possible effect on the posterior sclera/optic nerve head biomechanics [26].
This softening of the eye wall (cornea and sclera) could in fact represent a new therapeutic target in the treatment of glaucoma. The optic nerve head is a complex biomechanical structure and ongoing research aims to characterize the series of events in the glaucomatous process [27]. In addition, a more compliant and less rigid eye wall may dampen pressure fluctuations and reduce the occurrence or magnitude of pressure spikes. The pressure–volume relationship in the living human eye is non-linear, both in normal and in open-angle glaucoma eyes [28]. Changes in the eye’s volume translate to changes in IOP, from the ocular pulse amplitude that occurs due to the ocular pulse to IOP spikes that can occur with eye rubbing or with changes in posture. There is evidence that the intraocular pressure–anterior chamber volume relationship changes with the use of prostaglandins [29]. Therefore, softening of the eye wall may in fact be protective for VF progression.
In the present study, CH failed to reach a level of significance, but there was a clear trend towards a lower CH in the P group. In a recent systematic review of the available evidence, Sit et al. concluded that lower CH is found in glaucoma, however it is at present unknown if the relationship is causal [30]. The authors also conclude that there are few studies that suggest that measurement of CH confers information on the risk in glaucoma suspects and patients, when appreciated together with structural and functional examinations, and that low CH may increase the risk of progression. However, the multifactorial associations between CH and other variables render the relationship complex.
Certain limitations should be considered when looking at results from this study. First, we enrolled only newly diagnosed patients with ocular hypertension or mild-to-moderate open-angle glaucoma. These were patients in whom initiation of prostaglandin monotherapy was decided clinically. Therefore, these results may not apply to previously treated glaucoma patients, patients with angle closure glaucoma, patients with advanced stage of the disease, and also patients with secondary glaucoma. Moreover, these were patients that were started on PG monotherapy with latanoprost. However, this is a pilot study that included a relatively small number of patients, and a larger dataset is necessary to confirm our results.
Conclusions
A higher value in the SSI index after 1 month of PG analogues is found in eyes that progress. The absolute value, not the change versus baseline, in SSI at 1 month of latanoprost treatment was the parameter able to predict the future risk of progression. Lower HC parameters (HC deflection length and HC dARC length), which suggest increased scleral stiffness, were also found in progressing eyes. To our knowledge, this is the first report on the association of these biomechanical parameters measured at 1 month on latanoprost monotherapy and the risk of progression. Our results provide evidence supporting the clinical relevance of measuring corneal biomechanics and the possible role of these parameters in assessing the risk of progression in newly diagnosed OHT and POAG. In addition, softening the eye wall may as well be proposed as a new glaucoma therapeutic target.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
European Glaucoma Society Terminology and Guidelines for Glaucoma. 5th Edition. Br J Ophthalmol. 2021;105(Suppl 1):1–169.
Boote C, Sigal IA, Grytz R, Hua Y, Nguyen TD, Girard MJA. Scleral structure and biomechanics. Prog Retin Eye Res. 2020;74: 100773.
Gordon MO. The Ocular Hypertension Treatment Study: Baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):714.
Leske MC, Heijl A, Hyman L, Bengtsson B, Dong L, Yang Z. Predictors of long-term progression in the Early Manifest Glaucoma Trial. Ophthalmology. 2007;114(11):1965–72.
Leske MC, Wu SY, Hennis A, Honkanen R, Nemesure B. Risk factors for incident open-angle glaucoma. Ophthalmology. 2008;115(1):85–93.
Francis BA, Varma R, Chopra V, Lai MY, Shtir C, Azen SP. Intraocular pressure, central corneal thickness, and prevalence of open-angle glaucoma: The Los Angeles Latino Eye Study. Am J Ophthalmol. 2008;146(5):741–6.
Liu MX, Zhou M, Li DL, Dong XX, Liang G, Pan CW. Corneal biomechanics in primary open angle glaucoma and ocular hypertension: A systematic review and meta-analysis. J Glaucoma. 2023;32(3):e24-32.
Lopes BT, Roberts CJ, Elsheikh A, Vinciguerra R, Vinciguerra P, Reisdorf S, et al. Repeatability and reproducibility of intraocular pressure and dynamic corneal response parameters assessed by the Corvis ST. J Ophthalmol. 2017;2017:1–4.
Martínez-Sánchez MI, Bolívar G, Sideroudi H, Teus MA. Effect of prostaglandin analogues on the biomechanical corneal properties in patients with open-angle glaucoma and ocular hypertension measured with dynamic Scheimpflug analyzer. Graefes Arch Clin Exp Ophthalmol. 2022;260(12):3927–33.
Shen SR, Fleming GP, Jain SG, Roberts CJ. A review of corneal biomechanics and scleral stiffness in topical prostaglandin analog therapy for glaucoma. Curr Eye Res. 2023;48(2):172–81.
Sánchez‐Barahona C, Bolívar G, Katsanos A, Teus MA. Latanoprost treatment differentially affects intraocular pressure readings obtained with three different tonometers. Acta Ophthalmol (Copenh) [Internet]. 2019 Dec [cited 2023 Jun 1];97(8). Available from: https://doi.org/10.1111/aos.14170
Amano S, Nejima R, Inoue K, Miyata K. Effect of topical prostaglandins on the biomechanics and shape of the cornea. Graefes Arch Clin Exp Ophthalmol. 2019;257(10):2213–9.
Wu N, Chen Y, Yang Y, Sun X. The changes of corneal biomechanical properties with long-term treatment of prostaglandin analogue measured by Corvis ST. BMC Ophthalmol. 2020;20(1):422.
Vinciguerra R, Rehman S, Vallabh NA, Batterbury M, Czanner G, Choudhary A, et al. Corneal biomechanics and biomechanically corrected intraocular pressure in primary open-angle glaucoma, ocular hypertension and controls. Br J Ophthalmol. 2020;104(1):121–6.
Eliasy A, Chen KJ, Vinciguerra R, Lopes BT, Abass A, Vinciguerra P, et al. Determination of corneal biomechanical behavior in-vivo for healthy eyes using CorVis ST tonometry: Stress-strain index. Front Bioeng Biotechnol. 2019;16(7):105.
Aoki S, Asaoka R, Fujino Y, Nakakura S, Murata H, Kiuchi Y. Comparison of two analyzer measurements focusing on material stiffness among normal, treatment-naïve, and treated glaucoma eyes. Sci Rep. 2023;13(1):96.
Susanna BN, Ogata NG, Jammal AA, Susanna CN, Berchuck SI, Medeiros FA. Corneal biomechanics and visual field progression in eyes with seemingly well-controlled intraocular pressure. Ophthalmology. 2019;126(12):1640–6.
Nguyen BA, Reilly MA, Roberts CJ. Biomechanical contribution of the sclera to dynamic corneal response in air-puff induced deformation in human donor eyes. Exp Eye Res. 2020;191: 107904.
Roberts CJ, Mahmoud AM, Bons JP, Hossain A, Elsheikh A, Vinciguerra R, et al. Introduction of two novel stiffness parameters and interpretation of air puff-induced biomechanical deformation parameters with a dynamic Scheimpflug analyzer. J Refract Surg. 2017;33(4):266–73.
Qassim A, Mullany S, Abedi F, Marshall H, Hassall MM, Kolovos A, et al. Corneal stiffness parameters are predictive of structural and functional progression in glaucoma suspect eyes. Ophthalmology. 2021;128(7):993–1004.
Aoki S, Murata H, Nakakura S, Nakao Y, Matsuura M, Fujino Y, et al. Development of a novel corneal concavity shape parameter and its association with glaucomatous visual field progression. Ophthalmol Glaucoma. 2019;2(1):47–54.
Jung Y, Chun H, Moon JI. Corneal deflection amplitude and visual field progression in primary open-angle glaucoma. Oddone F (ed). PLOS ONE. 2019;14(8):e0220655.
Aoki S, Miki A, Omoto T, Fujino Y, Matsuura M, Murata H, et al. Biomechanical glaucoma factor and corneal hysteresis in treated primary open-angle glaucoma and their associations with visual field progression. Investig Opthalmology Vis Sci. 2021;62(7):4.
Weinreb RN, Robinson MR, Dibas M, Stamer WD. Matrix metalloproteinases and glaucoma treatment. J Ocul Pharmacol Ther. 2020;36(4):208–28.
Weber C, Buerger A, Priglinger S, Mercieca K, Liegl R. Influence of a prostaglandin F2α analogue on corneal hysteresis and expression of extracellular matrix metalloproteinases 3 and 9. Transl Vis Sci Technol. 2023;12(5):28.
Weinreb RN. Enhancement of scleral macromolecular permeability with prostaglandins. Trans Am Ophthalmol Soc 2001;99:319–43 [Internet]. Available from: https://pubmed.ncbi.nlm.nih.gov/11797317/. Accessed 1 May 2023.
Burgoyne CF, Crawford Downs J, Bellezza AJ, Francis Suh JK, Hart RT. The optic nerve head as a biomechanical structure: A new paradigm for understanding the role of IOP-related stress and strain in the pathophysiology of glaucomatous optic nerve head damage. Prog Retin Eye Res. 2005;24(1):39–73.
Dastiridou AI, Tsironi EE, Tsilimbaris MK, Ginis H, Karyotakis N, Cholevas P, et al. Ocular rigidity, outflow facility, ocular pulse amplitude, and pulsatile ocular blood flow in open-angle glaucoma: A manometric study. Investig Opthalmology Vis Sci. 2013;54(7):4571.
Scott JA, Roberts CJ, Mahmoud AM, Jain SG. Evaluating the relationship of intraocular pressure and anterior chamber volume with use of prostaglandin analogues. J Glaucoma. 2021;30(5):421–7.
Sit AJ, Chen TC, Takusagawa HL, Rosdahl JA, Hoguet A, Chopra V, et al. Corneal hysteresis for the diagnosis of glaucoma and assessment of progression risk. Ophthalmology. 2023;130(4):433–42.
Funding
No funding or sponsorship was received for the study or publication of this article.
Author information
Authors and Affiliations
Contributions
All authors meet the ICMJE criteria for authorship. Marta I Martinez-Sánchez: data acquisition, manuscript revision. Gema Bolívar: data acquisition, manuscript revision. Anna Dastiridou: original draft preparation. Purificación Escámez: data acquisition, manuscript revision. Miguel A Teus: concept and design, statistical analysis, critical revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
There are no competing interests for any of the authors.
Ethical Approval
The study followed the tenets of the Declaration of Helsinki and the protocol was approved by the Institutional Review Board (CEIM) Hospital Universitario Principe de Asturias with the number OE 15/2020.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Martinez-Sánchez, M.I., Bolívar, G., Dastiridou, A. et al. Predictive Value of Dynamic Corneal Response Parameters Evaluated with Scheimpflug High-Speed Video (Corvis ST) on the Visual Field Progression in Prostaglandin Treated Ocular Hypertension and Open-Angle Glaucoma Patients. Ophthalmol Ther 12, 3177–3186 (2023). https://doi.org/10.1007/s40123-023-00810-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00810-0