Abstract
Introduction
Axial length (AL) elongation in myopia is considered irreversible. We aimed to systemically report unexpected AL shortening observed in a randomized clinical trial (RCT) after repeated low-level red-light (RLRL) therapy.
Methods
This is a post hoc analysis of a multicenter, single-masked RCT. Two hundred sixty-four myopic children aged 8–13 years allocated to RLRL treatment (intervention group) or a single vision spectacle (SVS, control group) were included. AL was measured using an IOL-master 500 at baseline, 1-, 3-, 6-, and 12-month follow-up visits. AL shortening was defined as AL reduction from baseline to follow-up visits at three cutoffs: > 0.05 mm, > 0.10 mm, and > 0.20 mm. Frequency of AL shortening at different cutoffs was calculated. Analysis was done with intent to treat (ITT).
Results
At 12-months follow up, frequency of AL shortening > 0.05 mm was 26/119 (21.85%) and 2/145 (1.38%) for the RLRL group versus the control group, respectively. The frequency was 18/119 (15.13%) versus 0/145 (0%) for AL shortening > 0.10 mm, and 7/119 (5.88%) versus 0/145 (0%), for AL shortening > 0.20 mm, respectively (p < 0.001). Mean AL shortening after 12 months (SD) was −0.156 (0.086) mm in the RLRL group and −0.06 mm in the control group. Age was significantly associated with AL shortening in the multivariable analysis. For the RLRL group that exhibited AL shortening (n = 56), choroidal thickness (ChT) thickening (0.056 mm) could only explain 28.3% of AL shortening (−0.20 mm).
Conclusion
Nearly a quarter of children had > 0.05 mm AL shortening following 12 months of RLRL therapy, whereas AL shortening rarely occurred among controls.
Trial Registration
ClinicalTrials.gov (NCT04073238).
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Why carry out this study? |
Myopia progression is characterized by axial elongation that is considered irreversible. |
No human studies to date have suggested any treatment for myopia control could result in axial shortening within a timeframe of months or years. |
What was learned from the study? |
In this post hoc analysis of a randomized controlled trial, repeated low-level red-light (RLRL) therapy was found to cause substantial reversal in elongation of axial length among nearly one-quarter of the participants. |
Introduction
Myopia is considered as a progressive, irreversible condition characterized by an excessive elongation of axial length (AL) [1]. Even in the fifth decades of life, AL elongation persists among some myopic adults [2, 3]. AL elongation is accompanied by a dramatically increased risk of vision-threatening complications such as macular hemorrhage, retinal detachment, and glaucoma [4]. Considering these adversities, preventing AL elongation is a primary focus for myopia control [5]. Current treatments for controlling myopia aim to slow AL elongation, but no treatments can reverse or cure AL elongation within a timeframe of months or years.
Repeated low-level red-light (RLRL) therapy is a novel therapeutic method for controlling myopia, with promising efficacy and safety. It was developed from the principle that adequate exposure to outdoor bright light is a strong protective factor against myopia development [6,7,8]. Our recent randomized controlled trial (RCT) demonstrated exposure to RLRL twice daily reduced myopic progression by 69.4% over a 1-year period [9]. In particular, when compliance of RLRL therapy increased from < 50% to 75%, the efficacy of reduction in AL elongation rose from 44.6% to 76.8%, and efficacy for spherical equivalent changes improved from 41.7% to 87.7% [9].
During the clinical trial, we observed clinically significant AL shortening among participants, which was greater than the level (> 0.05 mm) that could be attributed to measurement error. These findings challenge the view that myopia is an irreversible condition and provide new insights that may underlie the mechanisms of myopia development. In this post hoc analysis, we systematically report the frequency of AL shortening among treatment and control arms, and evaluate changes of AL and choroidal thickness (ChT) among those with significant AL shortening.
Method
Study Design and Participants
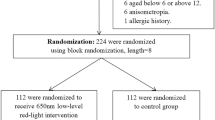
The current study is a post hoc analysis of a prospective 1-year RCT of children aged 8–13 years with myopia. Previous reports describe the methodology of the study in greater detail [9]. In brief, a parallel-group, single-masked, randomized controlled study was conducted across five study centers from four tertiary hospitals in China. The study aimed to determine the efficacy and safety of RLRL therapy for myopia control. Children aged 8–13 years with myopia of cycloplegic spherical equivalent refraction (SER) between −1.00 and −5.00 D, astigmatism 2.50 D or less, anisometropia 1.50 D or less, and best-corrected visual acuity (BCVA) 1.0 in either eye were recruited. Children were excluded if they had history or presence of strabismus, binocular visual function abnormalities, other ocular diseases, systemic diseases, or had received other myopia control treatment [including but not limited to atropine therapy, orthokeratology, or Defocus Incorporated Multiple Segments (DIMS) glasses]. A total of 400 random numbers were pregenerated, and all centers adopted the same centralized randomization list using the centralized web-based randomization service [Solomon electronic data capture (EDC) system, Vision Tech Medical Technology, Guangzhou, China]. A total of 264 eligible children were randomly allocated to an intervention group (RLRL group, n = 119) or control group (single vision spectacle, SVS group, n = 145) at the beginning of the study, with follow-up at 1, 3, 6, and 12 months.
The study was approved by the institutional ethics committee of Zhongshan Ophthalmic Centre (2019KYPH093) and adhered to the Declaration of Helsinki for study of human subjects. All participants and their guardians were informed of the study details and signed informed consent. The RCT protocol was registered at ClinicalTrials.gov (NCT04073238).
Intervention
As a routine treatment for myopia, all children including children in RLRL group wore SVS lenses throughout the study and updated their glasses if necessary. In addition to wearing SVS, children in the intervention group received RLRL therapy. The RLRL therapy was provided by a semi-conductor laser diode product (Eyerising, Suzhou Xuanjia Optoelectronics Technology, Jiangsu, China), which has been sold and widely used in China for amblyopia treatment for a decade. The device includes semiconductor laser diodes (LDs) and emits low-level red-light at a wavelength of 650 ± 10 nm. The light power going through a 4 mm pupil is 0.29 mW, which is considered as class 1 under the IEC 60825-1:2014 standard, and safe for direct ocular exposure, indicating there is no retinal thermal hazard. Children in the intervention group logged into the device with their unique accounts and passwords, and initiated the RLRL therapy twice a day, 3 min per session, with a minimum interval of 4 h. Data on the date and time of each login was automatically recorded in the device and transferred to an online database that monitored treatment compliance. The compliance of RLRL treatment was calculated as the percentage of actual number of treatments divided by the number of assigned treatment sessions (two times per day, 5 days per week) for the entire treatment period.
Due to the nature of the intervention in this study, the children and their parents were aware of the allocation. All outcome assessors were masked, including technicians, optometrists, and statisticians.
Measurements
The examination methods of this study are described elsewhere [9]. All variables for each participant were measured by the same device at baseline and follow-up. All participants received slit-lamp examination and were tested for uncorrected visual acuity (UCVA), best corrected visual acuity (BCVA), autorefractor, and ocular biometric parameters. The right eye was examined before the left eye. Measures of AL were conducted on each eye prior to cycloplegia using IOL-Master (Carl Zeiss 500, Meditec, Oberkochen, Germany). At least five measurements were performed with excellent precision (i.e., ≤ 0.05 mm) according to standard procedure, and the average value was used for analysis. Cycloplegia was achieved using two drops of 0.5% tropicamide 5 min apart for three times prior to autorefraction. Pupil light reflex and pupil diameter were checked to confirm full cycloplegia after an additional 15 min. A pupil size > 6 mm and/or an absent light reflex was considered successful dilation. Refraction was measured using Topcon KR-8800 (Topcon, Tokyo, Japan) three times with desired precision (i.e., ≤ 0.25 diopter), and the average of the three readings were used for analysis. Cycloplegic SER was calculated using the sum of the spherical power and half cylindrical power.
Choroidal thickness (ChT) was an optional measure in the RCT and was performed in centers with swept source optical coherence tomography (SS-OCT) equipment available. A total of 162 children in two study centers (Ouzhuang, Zhongshan Ophthalmic Center and Zhujiang New Town, Zhongshan Ophthalmic Center) underwent SS-OCT scanning (RLRL group, n = 72; SVS group, n = 90). After pupil dilatation, the children underwent SS-OCT imaging under standardized mesopic light conditions by the same technician masked to the study protocol, using the SS-OCT device (DRI-OCT Triton, Topcon, Tokyo, Japan) for choroidal imaging. This device uses a laser wavelength of 1050 nm, a scanning speed of 100,000 scans per second, and an axial and transverse resolution of 8 μm and 20 μm, respectively [10]. This study adopted 12.0 mm radial scans protocol (resolution, 1024 × 12) centered on the fovea. Eligible images had > 70 image quality scores (range 0–100) with no segmentation errors or artifacts. All eligible images were then verified by a masked technician. Data from built-in software that automatically segmented the choroidal layer and measured ChT parameters were used. Subfoveal ChT was defined as the distance between outer choroid-scleral margin and retinal pigment epithelium (RPE)–Bruch’s complex under the foveal region.
Outcomes
The primary outcome for this analysis was the frequency of AL shortening, which was categorized into cutoffs of > 0.05 mm, > 0.10 mm, and > 0.20 mm. Secondary outcomes included the change in AL and subfoveal ChT per year among those with AL shortening. Baseline age was categorized into 8–10- and 11–13-year groups. Baseline SER was categorized into mild myopia (−3.0 < SER ≤ −1.0 D) and moderate myopia (−5.0 < SER ≤ −3.0 D).
Statistical Analysis
Data analysis was performed in accordance with the principle of intention-to-treat analysis (ITT) and included subjects who completed randomization. No imputation of missing data was performed. Given the strong correlation between right and left eyes, only data from right eyes were used for analysis. Continuous variables were presented as mean ± standard deviation (SD). Categorical variables were presented as number and percentage. Scatter plots with linear fit described the distribution of AL change per year between treatment groups, and were stratified for age, sex, and baseline SER. The Fisher’s exact test compared group differences in the frequency of AL shortening under the three cutoffs, and were stratified by age, sex, and baseline SER. Logistic regression models investigated the relationship between frequency of AL shortening in the three cutoffs and age, sex, AL at baseline, and SER at baseline. For the subset of children who underwent SS-OCT imaging, logistic regression models investigated the relationship between magnitude of AL shortening and baseline, and changes in ChT. The R2 of the regression quantified the variance in AL shortening, which were explained by changes in subfoveal ChT. We used Stata (StataCorp, Stata Statistical Software: Release 17; College Station, TX, USA) for statistical analyses. A p-value < 0.05 was considered statistically significant.
Results
All 264 randomized children (119 in RLRL group, 145 in SVS group) were included in the present analysis, with 57 males (47.9%) in the RLRL group and 73 males (50.3%) in the SVS group.
Frequency of Axial Length (AL) Shortening
Table 1 presents the frequency of AL shortening at each visit based on cutoffs of > 0.05 mm, > 0.10 mm, and > 0.20 mm. For > 0.05 mm cutoffs, 40.34% children achieved AL shortening at 1 month, followed by 28.57% at 3 months, 21.85% at 6 months, and 12 months in the RLRL group. AL shortening in the SVS cohort was 4.14% at 1 month, 0.69% at 3 months, 0% at 6 months, and 1.38% at 12 months. There were 26/119 (21.85%) in the RLRL group versus 2/145 (1.38%) in the SVS group who had observed AL shortening > 0.05 mm (p < 0.001) at the 12-month follow-up. For cutoffs of > 0.10 mm, AL shortening in RLRL group was recorded in 12.61% of participants at 1 month, 15.17% at 3 months, 10.08% at 6 months, and 15.13% at 12 months, while the AL shortening did not present in SVS group in any visits, except at 1 month (0.69%). For cutoffs of > 0.20 mm, AL shortening was only observed in the RLRL therapy arm but not in the control group, and the AL shortening in participants at 12 months was 7/119 (5.88%) (p < 0.001).
Figure 1 shows the associations of AL shortening (> 0.05 mm) at 12-months follow-up with age, AL, or SER at baseline in each group. Frequency of AL shortening was significantly associated with baseline age, AL, and SER (Fig. 1 and Table 2). Myopic children in the RLRL group had the highest frequency of AL shortening at 1 month follow-up, with new recorded AL shortening not as frequent at other follow-up time points. Boys had higher incidence of AL shortening at 3, 6, and 12 months compared with girls, although these sex differences were not statistically significant (Table 2). Sensitivity analyses at cutoffs > 0.10 mm (Supplementary Table S1) and > 0.20 mm (Supplementary Table S2) showed trends consistent with these sex differences.
Scatter plots with line of best fit showing the associations between rate of AL change during follow-up with age, AL, and SER at baseline in each group. A Rate of AL change versus age at baseline; B rate of AL change versus AL at baseline; C rate of AL change versus SER at baseline. RLRL repeated low-level red-light, SVS single vision spectacle, AL axial length, SER spherical equivalent refraction, D diopter
Changes of Axial Length (AL) in Children with AL Shortening
For all participants, the RLRL group had consistent and significant AL progression from baseline to each visit compared with the SVS group (Supplementary Table S3). For children with AL shortening at each follow-up visit, the changes in AL of between intervention groups are summarized in Table 3. Over 12 months, mean changes in AL among children with AL shortening (SD) were −0.156 (0.086) mm in the RLRL group, while the two children in the control group with AL shortening had a mean of −0.06 mm. This was likely due to measurement error. Changes in AL among children with AL shortening was most pronounced in the first month of treatment (−0.095 mm) and subsequent reductions were less in magnitude but constant at 3, 6, and 12 months follow-up (Table 3). AL across follow-up visits stratified by the presence of AL shortening (> 0.05 mm and > 0.10 mm) at 1 month follow-up for RLRL participants is shown in Fig. 2. For those with AL shortening at 1 month, the AL remained stable at subsequent follow-up visits. As expected, the AL change was consistent and significant related to SER change [β = −0.0869 (95% CI −0.131, −0.0431), p < 0.0001) (Supplementary Fig. S1).
Trajectory of AL at each follow up visit for each child in RLRL group stratified by early responses to treatment. A AL shortening > 0.05 mm from baseline to 1 month. B AL shortening > 0.10 mm from baseline to 1 month. Each single line represents the trajectory of AL change in a year for each child in the RLRL group. The red line and blue line represent the children who had AL shortening or not at 1 month. To account for the measurement error (0.05 mm), AL shortening was defined as AL reduced by at least 0.05 mm, and a reference line of y = −0.05 mm is presented. RLRL repeated low-level red-light, SVS single vision spectacle, AL axial length. Red represents the children that achieved AL shortening at 1 month. Blue represents the children that did not have AL shortening at 1 month
Factors Associated with the Presence of Axial Length (AL) Shortening
Table 4 summarizes the baseline factors associated with frequency of AL shortening in multivariable models. After adjusting for other confounding factors, older age and female gender were significantly associated with a greater odds of AL shortening > 0.05 mm/year in model 1. For multivariate model 2, older baseline age was significantly associated with the presence of AL shortening after adjusting for other factors. Sensitivity analyses showed that older baseline age and lower SER were significantly associated with higher odds of AL shortening of > 0.10 mm/year (Supplementary Table S4). Table 5 summarizes the characteristics of the children with > 0.20 mm AL shortening across the 12-month period.
Choroidal Thickness in Relation to Axial Length (AL) Shortening
The subgroup of children with OCT data did not differ from those without OCT data with respect to age, sex, AL, and AL change (Supplementary Table S5). A total of 72 patients in the RLRL group underwent OCT measurement. Participants were included in the analysis if they had valid ChT at least at baseline and the 12-month visit (56 in the RLRL group). There were no significant differences in characteristics between included and excluded participants (Supplementary Table S6–7).
The change in AL and subfoveal ChT from 12-months follow-up to baseline were −0.20 mm and 0.056 mm of the right eye, and −0.23 mm and 0.083 mm of the left eye among children with AL shortening in the RLRL, respectively. After adjusting for other covariates, the presence of AL shortening was significantly associated with older age and greater ChT thickening (Supplementary Table S8). Figure 3 shows the associations of changes in AL with baseline parameters, and changes in ChT during the 12-month period among children with AL shortening in the RLRL group. Changes in AL of children with AL shortening was observed with increasing baseline ChT and changes in ChT at follow up. The ChT at baseline and ChT changes could only explain 5.4% and 28.3% of the AL changes, respectively.
Scatter plots showing the associations between rate of AL change with ChT at baseline and ChT changes during the 12-month period in each group. A total of 72 patients in the RLRL group and 90 patients in the SVS group underwent OCT measurement at baseline. Participants were included in the analysis if they provided valid choroidal thickness and had complete covariate data (56 in the RLRL group and 51 in the SVS group). RLRL repeated low-level red-light, SVS single vision spectacle, SS-OCT swept-source optical coherence tomography, ChT choroidal thickness
Sensitivity Analysis
Sensitivity analysis was performed by using the 1-month AL measurements as baseline. The results of the sensitivity analysis did not change the conclusions from the primary analysis (Table S9). Over 1/10 of children receiving RLRL therapy experienced AL shortening but this phenomenon was scare in the SVS control group at each visit (p < 0.05), indicating the consistency and robustness of the primary analysis.
Discussion
This study systematically reported AL shortening over the course of months among the children on myopia control treatments. AL shortening > 0.05 mm occurred in a quarter of children using RLRL treatment across the 12-month duration of this study, and this was extremely rare among children in the control arm. AL shortening was also more common among older children. OCT examination confirmed that choroidal thickening only explained 28.3% of the AL shortening, indicating that scleral remodeling may involve the observed AL shortening as response to RLRL.
Axial Length (AL) Shortening in Previous Studies
Clinical reports specifically looking into AL shortening have been extremely rare to date. One study reported AL shortening in the children following orthokeratology treatment, but this was transient and only observed in the first week of treatment at a negligible level (average, 0.026 mm) [11]. In the present analysis, RLRL therapy achieved AL shortening of > 0.05 mm in 21.85% of children at the 12-month visit. A cutoff of 0.05 mm was selected because this was considered the range of measurement error of the IOL-Master.
Scleral Remodeling or Choroidal Thickening?
In the AL measurement, the optical biometric device (IOL-Master) measures the distance from the anterior surface of cornea to the retinal pigment epithelium (RPE). Therefore, the “observed” AL shortening could be due to choroidal thickening that would push the RPE forward. In our analysis, we confirmed significant choroidal thickening after RLRL treatment, but this could only explain 28.3% of AL shortening. This indicates the observed AL shortening might be related to true scleral remodeling or shortening, rather than an apparent shortening due to choroidal thickening.
Factors Associated with Axial Length (AL) Shortening
Age was strongly correlated with AL shortening from RLRL therapy and was more common in older children, indicating that the treatment response of RLRL therapy is weaker among young children. This phenomenon was also observed in other studies utilizing other myopia treatments, including the low-concentration atropine for myopia progression (LAMP) and Defocus Incorporated Multiple Segments (DIMS) studies [12, 13]. In general, young children tend to progress more rapidly than older children or adults, which often means children who are diagnosed earlier in childhood are likely to have worse visual prognosis. Approximately 80% of the DIMS lens wearers with rapid myopia progression were young children aged 8–9 years compared with 20% in children aged 10–13 years [13]. In children using 0.05%, 0.025%, and 0.01% atropine drops, for every 1 year younger, the AL elongation accelerated by −0.10, −0.11, and −0.12 mm/year, respectively [12]. Therefore, the effect of age on response to RLRL might be due to the different retinal profile or intuitive greater myopia progression in younger children. These treatments are likely fighting an uphill battle against factors that threaten concomitant AL elongation, so in future it would be of interest to determine if a bolus dose of RLRL is likely to curtail myopia progression further in children and change their course of disease.
Extent of Axial Length (AL) Shortening
The greatest AL shortening was observed in the 1-month visit, from there on, the extent of AL shortening gradually reduced and maintained at the same level until the end of the study, albeit in a reduced manner. From the inception of RLRL therapy to the 12-month follow-up visit, AL shortening ranged from −0.05 to −0.31 mm, with a mean (SD) of −0.156 ± 0.086 mm at the 12-month visit among children with AL shortening in the intervention group. These data suggest that AL shortening is more likely to be maintained at a certain level (−0.156 ± 0.086 mm) rather than to further increase over time. This implies that this AL shortening will unlikely fully recover a myopic eye to an emmetropia; however, longer follow-up durations are paramount to exploring the long-term response to RLRL therapy.
Insights into Mechanisms Underlying Eye Growth Regulation
It is unknown how RLRL therapy shortens AL, although animal models have observed ocular shape in infant rhesus monkeys recover, to some extent, from experimentally induced myopia once the myopic stimulus is removed [14]. After removal, the form deprivation or hyperopic defocus self-corrects and AL shortening can be achieved in chicks, guinea pigs, tree shrews, and nonhuman primates [14,15,16,17,18]. It was proposed that an altered scleral and choroidal mRNA expression was a possible mechanism underlying scleral remodeling, which led the shortening observed among these animals [19,20,21,22]. The nonhuman primate studies in response to imposed optical defocus suggested that the altered expressions of human myopia quantitative trait loci improved choroidal perfusion and choroidal vascular permeability, and dilated nonvascular smooth muscle, and may contribute to choroidal thickening [23,24,25,26,27]. In the chicken response during recovery from induced myopia, increased expression of the hyaluronan synthase-2 gene and avian thymic hormone were noted [28, 29]. In addition, choroidal changes coincide with a reduced synthesis of scleral glycosaminoglycan, and blocked human scleral fibroblast cell attachment to type I collagen may contribute to AL changes [30,31,32]. This leads to the idea that refractive development is influenced by both visual and nonvisual cues, which presumably interact with physiological mechanisms that alter eye length. By this principle, RLRL is a visual cue that alters the natural course of myopia. It is not clear whether red light interferes with any of these previously mentioned processes, but laboratory studies should seek to identify possible molecular sites of action.
Clinical Significance of Axial Shortening
The observed AL shortening among a quarter of children after RLRL treatment, at a mean of 0.156 mm, is clinically important for the future of myopia treatment. Myopia is expected to reach a population burden of 50% globally in the next 30 years, so the achievement of partial reversal in this study is a breakthrough that brings AL shortening treatments into the realm of possibility. In future, RLRL may reverse myopia in its early phases so the newly onset myopic children can be reverted to emmetropia, which would mean children might not ever require wearing glasses or specialist interventions. This study also observed higher magnitudes of AL shortening in moderate myopia children compared with mild myopia, which is promising because each diopter of reduction would reduce myopia-induced visual impairment by 40% [33]. Currently, existing RCT data on low-dose atropine drops and optical treatments (orthokeratology, bifocal spectacles, and multifocal spectacles) for myopia control are designed to delay AL progression rather than reverse or cure. This is the first treatment design to have a potentially curative future focus, and has unlocked potential to influence future clinical trials and laboratory studies.
Strengths and Limitations
The strengths of this study include its multicentered, randomized controlled design with 12-months follow-up, and standardized measurements at each study site. The data from the SVS group confirms that AL shortening is unlikely to occur among myopic children without treatment, leaving RLRL as the stimulus for the observed changes in AL. In addition, the measurements of both AL and ChT excludes choroidal thickening as the sole contributor to AL shortening, and invites new speculation for how the structure and shape of the eye may contribute to this phenomenon. Notably, SS-OCT imaging was following complete pupil mydriasis, which enables the obtainment of high-quality choroidal images and automatic ChT measurement.
Despite these breakthroughs, some limitations should also be acknowledged. First, all analyses were conducted in an RCT population with strict inclusion and exclusion criteria, which may not be representative of the general myopic population. Second, only 1-year AL shortening outcomes were reported for RLRL treatment compared with SVS. The frequency and extent of long-term AL shortening, including how AL changes after RLRL treatment needs further evaluation in future. Third, participants were limited to Chinese children, and studies with multiethnic populations are needed. In addition, understanding the long-term prospects for AL shortening over time and its contribution to myopia control will require a longer follow-up study to confirm. Fourth, given the fact that the right and left eyes were highly correlated and symmetrical (Supplementary Table S10), only data of the right eye were analyzed. The effect of RLRL on children with anisometropia needed further study. Fifth, OCT data were only available in a small subset of subjects. Further SS-OCT studies of large sample sizes are needed to clarify the correlations between AL, SER, and ChT, and their trends overtime. Sixth, the information of age of onset, progression rate before enrollment, and environmental factors such as near work and time outdoors were not collected in this study, which limited our ability to determine the potential impact of these factors on responses to the RLRL therapy. Future studies with sensors are needed to quantified theses myopia-genic factors. Lastly, biometry was performed without cycloplegia, which might be influenced by the accommodation, but it would not significantly change the conclusions.
Conclusions
Nearly a quarter of children presented with AL shortening following RLRL therapy, an effect that could not be attributed to measurement error and/or ChT. Age and baseline AL were related to the degree of benefit from RLRL therapy. This novel finding highlights the disease-modifying implications of RLRL and for the first time shows myopia, to some extent, may be reversible in humans in the year timeframe. Such findings present RLRL as a therapy which actively prevents sight-threatening complications associated with AL elongation due to myopia development. Further studies are needed to confirm the effect of RLRL on AL in non-Chinese populations and elucidate mechanisms underlying AL shortening.
References
Baird PN, Saw SM, Lanca C, et al. Myopia. Nat Rev Dis Primers. 2020;6(1):99.
Du R, Xie S, Igarashi-Yokoi T, et al. Continued increase of axial length and its risk factors in adults with high Myopia. Jama Ophthalmol. 2021;139(10):1096–103.
Lee MW, Lee SE, Lim HB, Kim JY. Longitudinal changes in axial length in high myopia: a 4-year prospective study. Br J Ophthalmol. 2020;104(5):600–3.
Haarman A, Enthoven CA, Tideman J, et al. The complications of Myopia: a review and meta-analysis. Invest Ophthalmol Vis Sci. 2020;61(4):49.
Walline JJ. Myopia control: a review. Eye Contact Lens. 2016;42(1):3–8.
Wu PC, Chen CT, Chang LC, et al. Increased time outdoors is followed by reversal of the long-term trend to reduced visual acuity in Taiwan primary school students. Ophthalmology. 2020;127(11):1462–9.
He M, Xiang F, Zeng Y, et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314(11):1142–8.
Xiong F, Mao T, Liao H, et al. Orthokeratology and low-intensity laser therapy for slowing the progression of myopia in Children. Biomed Res Int. 2021;2021:8915867.
Jiang Y, Zhu Z, Tan X, et al. Effect of repeated low-level red-light therapy for myopia control in children: a multicenter randomized controlled trial. Ophthalmology. 2021. https://doi.org/10.1016/j.ophtha.2021.11.023.
Wang W, Liu S, Qiu Z, et al. Choroidal thickness in diabetes and diabetic retinopathy: a swept source OCT study. Invest Ophthalmol Vis Sci. 2020;61(4):29.
Lau JK, Wan K, Cheung SW, et al. Weekly changes in axial length and choroidal thickness in children during and following orthokeratology treatment with different compression factors. Transl Vis Sci Technol. 2019;8(4):9.
Li FF, Zhang Y, Zhang X, et al. Age effect on treatment responses to 0.05%, 0.025%, and 0.01% atropine: low-concentration atropine for myopia progression study. Ophthalmology. 2021;128(8):1180–7.
Lam C, Tang WC, Tse DY, et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. 2020;104(3):363–8.
Huang J, Hung LF, Smith ER. Recovery of peripheral refractive errors and ocular shape in rhesus monkeys (Macaca mulatta) with experimentally induced myopia. Vision Res. 2012;73:30–9.
Zhu X, McBrien NA, Smith ER, et al. Eyes in various species can shorten to compensate for myopic defocus. Invest Ophthalmol Vis Sci. 2013;54(4):2634–44.
Qiao-Grider Y, Hung LF, Kee CS, et al. Recovery from form-deprivation myopia in rhesus monkeys. Invest Ophthalmol Vis Sci. 2004;45(10):3361–72.
Lu F, Zhou X, Jiang L, et al. Axial myopia induced by hyperopic defocus in guinea pigs: a detailed assessment on susceptibility and recovery. Exp Eye Res. 2009;89(1):101–8.
Zhou X, Lu F, Xie R, et al. Recovery from axial myopia induced by a monocularly deprived facemask in adolescent (7-week-old) guinea pigs. Vision Res. 2007;47(8):1103–11.
McBrien NA, Lawlor P, Gentle A. Scleral remodeling during the development of and recovery from axial myopia in the tree shrew. Invest Ophthalmol Vis Sci. 2000;41(12):3713–9.
Guo L, Frost MR, Siegwart JJ, Norton TT. Gene expression signatures in tree shrew sclera during recovery from minus-lens wear and during plus-lens wear. Mol Vis. 2019;25:311–28.
Siegwart JJ, Norton TT. The time course of changes in mRNA levels in tree shrew sclera during induced myopia and recovery. Invest Ophthalmol Vis Sci. 2002;43(7):2067–75.
He L, Frost MR, Siegwart JJ, Norton TT. Gene expression signatures in tree shrew choroid during lens-induced myopia and recovery. Exp Eye Res. 2014;123:56–71.
Hung LF, Arumugam B, She Z, et al. Narrow-band, long-wavelength lighting promotes hyperopia and retards vision-induced myopia in infant rhesus monkeys. Exp Eye Res. 2018;176:147–60.
Smith ER, Hung LF, Arumugam B, et al. Effects of long-wavelength lighting on refractive development in infant rhesus monkeys. Invest Ophthalmol Vis Sci. 2015;56(11):6490–500.
Liu R, Hu M, He JC, et al. The effects of monochromatic illumination on early eye development in rhesus monkeys. Invest Ophthalmol Vis Sci. 2014;55(3):1901–9.
Smith ER, Hung LF, Arumugam B, Huang J. Negative lens-induced myopia in infant monkeys: effects of high ambient lighting. Invest Ophthalmol Vis Sci. 2013;54(4):2959–69.
Tkatchenko TV, Troilo D, Benavente-Perez A, Tkatchenko AV. Gene expression in response to optical defocus of opposite signs reveals bidirectional mechanism of visually guided eye growth. Plos Biol. 2018;16(10): e2006021.
Rada JA, Wiechmann AF, Hollaway LR, et al. Increased hyaluronan synthase-2 mRNA expression and hyaluronan accumulation with choroidal thickening: response during recovery from induced myopia. Invest Ophthalmol Vis Sci. 2010;51(12):6172–9.
Rada JA, Wiechmann AF. Ocular expression of avian thymic hormone: changes during the recovery from induced myopia. Mol Vis. 2009;15:778–92.
Rada JA, Palmer L. Choroidal regulation of scleral glycosaminoglycan synthesis during recovery from induced myopia. Invest Ophthalmol Vis Sci. 2007;48(7):2957–66.
Shelton L, Rada JA. Inhibition of human scleral fibroblast cell attachment to collagen type I by TGFBIp. Invest Ophthalmol Vis Sci. 2009;50(8):3542–52.
Rada JA, Shelton S, Norton TT. The sclera and myopia. Exp Eye Res. 2006;82(2):185–200.
Bullimore MA, Brennan NA. Myopia control: why each diopter matters. Optom Vis Sci. 2019;96(6):463–5.
Acknowledgements
We thank the participants of the study.
Funding
This research was supported in part by a grant from the Fundamental Research Funds of the State key Laboratory of 0phthalmology (3030901010058). The Rapid Service Fee was funded by the grant from the Fundamental Research Funds of the State key Laboratory of 0phthalmology (3030901010058).
Author Contributions
Mingguang He had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Wei Wang, Yu Jiang, Zhuoting Zhu, Meng Xuan, Jian Zhang, Ian G. Morgan and Mingguang He participated in study concept and design. Wei Wang, Yu Jiang, Zhuoting Zhu, Shiran Zhang, Jian Zhang, Junwen Zeng, Ian G. Morgan and Mingguang He were involved in acquisition, analysis, or interpretation of data. Wei Wang did the systematic review and image analysis. Wei Wang, Yu Jiang, Zhuoting Zhu, Shiran Zhang, Meng Xuan, Ian G. Morgan and Mingguang He drafted the report. All authors (Wei Wang, Yu Jiang, Zhuoting Zhu, Shiran Zhang, Meng Xuan, Xingping Tan, Xiangbin Kong, Hui Zhong, Gabriella Bulloch, Ruilin Xiong, Yixiong Yuan, Yanping Chen, Jian Zhang, Junwen Zeng, Ian G. Morgan, Mingguang He) provided critical revision of the manuscript for important intellectual content. Xingping Tan, Xiangbin Kong, Hui Zhong, Gabriella Bulloch, Ruilin Xiong, Yanping Chen, Jian Zhang, Junwen Zeng and Mingguang He coordinated the collection of clinical data and contributed to statistical analysis. Mingguang He raised the funding for the study. All authors provided administrative, technical, or material support. Ian G. Morgan and Mingguang He supervised the study.
Disclosures
Mingguang He and Zhuoting Zhu are inventors for the technology mentioned in the study patented as “A method to increase retinal blood flow and metabolism” (CN201910490186.6). Mingguang He is director and shareholder in Eyerising Ltd and Eyerising International Pty Ltd. Wei Wang, Yu Jiang, Shiran Zhang, Meng Xuan, Xingping Tan, Xiangbin Kong, Hui Zhong, Gabriella Bulloch, Ruilin Xiong, Yixiong Yuan, Yanping Chen, Jian Zhang, Junwen Zeng, Ian G. Morgan have nothing to declare.
Compliance with Ethics Guidelines
The study was approved by the institutional ethics committee of Zhongshan Ophthalmic Centre (2019KYPH093). The study was registered in ClinicalTrials.gov (NCT04073238). The study was conducted in accordance with the Declaration of Helsinki for study of human subjects. All participants and their guardians were informed of the study details and signed informed consent before entering the study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wang, W., Jiang, Y., Zhu, Z. et al. Axial Shortening in Myopic Children after Repeated Low-Level Red-Light Therapy: Post Hoc Analysis of a Randomized Trial. Ophthalmol Ther 12, 1223–1237 (2023). https://doi.org/10.1007/s40123-023-00671-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00671-7