Abstract
Introduction
Sepsis is characterized by a dysregulated host response to infection that leads to multiple organ dysfunction and often complicated with metabolic acidosis. However, the associations between serum total carbon dioxide level (TCO2) and long-term clinical outcomes in sepsis survivors remains unknown.
Methods
A total of 7212 sepsis survivors aged ≥ 20 years who were discharged from January 1, 2008 to December 31, 2018 were included in our analyses. The sepsis survivors were further divided into high TCO2 (≥ 18 mmol/L) and low TCO2 (< 18 mmol/L) groups, comprising 5023 and 2189 patients, respectively. The following outcomes of interest were included: all-cause mortality, myocardial infarction, ischemic stroke, hospitalization for heart failure, ventricular arrhythmia, and end-stage renal disease (ESRD).
Results
After propensity score matching, the low TCO2 group was at higher risks of all-cause mortality (hazard ratio [HR] 1.28, 95% confidence interval [95% CI] 1.18–1.39), myocardial infarction (HR 1.83, 95% CI 1.39–2.43), and ESRD (HR 1.38, 95% CI 1.16–1.64) than the high TCO2 group. The results remained similar after considering death as a competing risk.
Conclusion
Patients discharged from hospitalization for sepsis have higher risks of worse long-term clinical outcomes. Physicians may need to pay more attention to sepsis survivors whose TCO2 was low.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Metabolic acidosis is frequently found in patients with sepsis, and an understanding of serum total carbon dioxide levels (TCO2) in sepsis and their long-term clinical outcomes may give us an insight into the role of acid–base status in these patients. |
This cohort study assessed the long-term clinical outcomes among sepsis survivors with high and low TCO2 using propensity score matching to balance clinical characteristics at baseline. |
What was learned from this study? |
Our study assessed the relationship between serum TCO2 levels and the risk of all-cause mortality, major adverse cardiovascular events (MACEs), and end-stage renal disease (ESRD) in survivors of sepsis. |
In this cohort, sepsis survivors with low TCO2 levels were associated with increased risks of all-cause mortality, MACEs, and progression to ESRD. This result was consistently significant after considering death as a competing risk. |
Introduction
Sepsis is a major global healthcare concern characterized by a dysregulated host response to infection that can lead to life-threatening multiple organ dysfunction, and it has a high incidence and mortality rate [1,2,3]. Immune activation in sepsis may lead to systemic inflammation, endothelial barrier dysfunction, exaggerated coagulopathy, fibrin clot formation, myocardial depression, renal dysfunction, and the risk of future adverse events [1, 4,5,6]. About 37 million incident cases of sepsis and 11 million deaths attributable to this condition (20% of all global deaths) were recorded worldwide in 2017 [7]. In recent years, with the advancement of care technology, earlier recognition, and more effective protocolized treatment, sepsis has become a less life-threatening disorder [8, 9]. However, it remains associated with long-term critical consequences, including chronic inflammation, late immunosuppressive effects, tissue wasting, and organ sequalae [10,11,12,13]. Moreover, sepsis survivors (those discharged alive from hospitalization for sepsis) have a sustained increased risk of mortality and higher risks of major adverse cardiac events (MACEs) and long-term functional deficits [14,15,16].
Metabolic acidosis, a common acid–base disorder indicated by low serum bicarbonate levels, is frequently found in patients with severe sepsis and septic shock [17]. It may cause a reduction in cardiac contractility, release catecholamines, activate the sympathetic system, have a direct arteriolar vasodilatory effect due to increased nitric oxide production, and result in negative bone metabolism and protein balances [17, 18]. The serum bicarbonate and total carbon dioxide (TCO2) concentrations are both indicators of metabolic acidosis, and can be used interchangeably because bicarbonate ions make up about 95% of the plasma TCO2 [19]. As serum TCO2 measurement is usually included in routine chemistry analysis, these values are more available than values for other indicators of metabolic acidosis [20].
A low serum bicarbonate level is an independent risk factor for the progression of kidney disease and has been associated with all-cause mortality in people with chronic kidney disease (CKD) [21,22,23]. In the third National Health and Nutrition Examination Survey, low serum bicarbonate levels were associated with a 1.74-fold higher risk of all-cause mortality [21]. The Chronic Renal Insufficiency Cohort (CRIC) study, which enrolled 3939 patients with CKD, demonstrated that increased serum bicarbonate level associated with lower risk of end-stage renal disease (marked by the initiation of dialysis therapy or kidney transplantation) or a 50% reduction in the estimated glomerular filtration rate (eGFR) [22]. A recent retrospective cohort study showed that the serum TCO2 level was a prognostic factor for 28-day mortality among patients with sepsis [24]. However, that study was limited by the examination of the endpoint of short-term mortality; associations of the TCO2 concentration with long-term clinical outcomes in sepsis survivors remain unknown. Thus, we conducted a cohort study with a 10-year study period to determine whether the TCO2 level is associated with risks of long-term adverse outcomes (all-cause mortality, myocardial infarction, ischemic stroke, heart failure, ventricular arrhythmia, and adverse renal outcomes) in sepsis survivors.
Methods
Data Source
This retrospective cohort study was conducted with medical records data from the Big Data Center of Taipei Veterans General Hospital, which contains comprehensive medical records, pharmacy orders, laboratory results, and examination reports for all inpatients, outpatients, and emergency patients [25]. All patients were aged ≥ 20 years and had had their peripheral venous TCO2 levels measured within 1 week of discharge from hospitalization for sepsis (international classification of diseases [ICD] code 038, 995.91, A40, and A41), severe sepsis (ICD code 995.92 and R65.20), or septic shock (ICD code 785.52 and R65.21) between 1 January 2008 and 31 December 2018 [26, 27]. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. Ethical approval for this study was obtained from the Ethical Committee of Taipei Veterans General (2017-09-002BC), and the study was conducted under the relevant guidelines and regulations. Informed consent was waived because de-identified data were analyzed.
Study Cohort
On the basis of their post-discharge TCO2 levels, the sepsis survivors were divided into high TCO2 (≥ 18 mmol/L) and low TCO2 (< 18 mmol/L) groups. The following baseline variables were recorded: age, sex, eGFR, sources of infection, septic shock, intensive care unit admission, use of mechanical ventilation, use of inotropes, hypertension, coronary artery disease, diabetes mellitus, congestive heart failure, autoimmune disease, chronic obstructive pulmonary disease, obstructive sleep apnea syndrome, malignancy, Charlson comorbidity index (CCI) score, use of calcium channel blockers, alpha blockers, beta blockers, renin–angiotensin–aldosterone system inhibitors, diuretics, statins, non-steroidal anti-inflammatory drugs, proton pump inhibitors, antiplatelets, and anticoagulants.
Outcomes
The outcomes of interest were all-cause mortality, myocardial infarction, ischemic stroke, hospitalization for heart failure, ventricular arrhythmia, and end-stage renal disease (defined as eGFR < 15 mL/min/1.73 m2, initiation of long-term dialysis, or kidney transplantation). All sepsis survivors were followed until death or the end of the study period.
Statistical Analysis
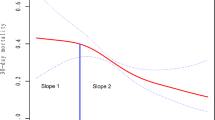
Among the baseline characteristics, categorical variables such as sex, underlying comorbidities, and medications were compared between groups using chi-squared tests. Continuous variables were compared using Student’s t test for normally distributed variables and the Mann–Whitney U test for non-normally distributed variables. We performed multivariate imputation by chained equations to impute missing values with five imputed data sets and 50 iterations [28, 29]. For matched cohort analysis, we used 1:2 propensity score matching of individuals from the low and high TCO2 groups [30, 31]. The covariates used in the propensity score were as follows: age, sex, eGFR, respiratory infection, bacteremia, endocarditis, central nervous system infection, skin infection, pelvic inflammatory disease, genitourinary tract infection, intra-abdominal infection, septic shock, intensive care unit admission, use of mechanical ventilation, inotropes use, hypertension, coronary artery disease, diabetes mellitus, congestive heart failure, autoimmune disease, chronic obstructive pulmonary disease, obstructive sleep apnea syndrome, malignancy, CCI score, calcium channel blockers, alpha blockers, beta blockers, renin–angiotensin–aldosterone system inhibitors, diuretics, statins, nonsteroidal anti-inflammatory drugs, proton-pump inhibitors, antiplatelets, anticoagulants, and follow-up period. In addition, we calculated propensity scores for the likelihood of sepsis survivors with high and low TCO2 by including clinical covariates in a multivariate logistic regression model (Table S1 in the supplementary material). The standardized mean difference was calculated to assess the balance between sepsis survivors with high and low TCO2 after matching, and a difference of less than 0.1 in the score was considered to be well balanced [32, 33]. Cox regression was used to obtain hazard ratios (HRs) for the evaluation of relative risks of outcomes in the two study groups. All analyses were performed using the SAS statistical software (version 9.4; SAS Institute, Cary, NC, USA) and R software (version 3.5.2 for Windows; R Foundation for Statistical Computing, Vienna, Austria. The significance level was set to p < 0.05.
Results
Baseline Characteristics of Study Population
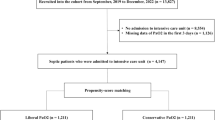
The study cohort comprised 7212 sepsis survivors allocated to the low (n = 2189) and high (n = 5023) TCO2 groups before propensity score matching. The baseline characteristics of the study subjects are provided in Table 1. Relative to those in the high TCO2 group, patients in the low TCO2 group were younger, and used more inotropes and proton pump inhibitors. Respiratory and genitourinary tract infections were less frequent, and intra-abdominal infection was more frequent, in the low TCO2 group than in the high TCO2 group. There was no missing data for age, sex, underlying comorbidities, and medications, but there were missing values in the eGFR (proportions of missing values 8.8%). Propensity score matching yielded a matched cohort of 3414 sepsis survivors (2276 patients in the high TCO2 group and 1138 patients in the low TCO2 group). Baseline characteristics did not differ significantly between these groups. After propensity score matching, the median age of matched-cohort was 80.8 (interquartile range [IQR] 67.7–87.1) years; 32.4% of patients were women, and the median eGFR was 63.1 (IQR 32.8–92.9) ml/min/1.73 m2, and the baseline characteristics were well balanced between these two groups (Fig. S1 in the supplementary material).
Long-Term Risks of Mortality, MACEs, and End-Stage Renal Disease According to TCO2 Levels
During the study period, the low TCO2 group had higher risks of all-cause mortality [HR 1.28; 95% confidence interval (CI) 1.18–1.39; p < 0.001], myocardial infarction (HR 1.83; 95% CI 1.39–2.43; p < 0.001), and end-stage renal disease (HR 1.38; 95% CI 1.16–1.64; p < 0.001; Table 2). No significant difference in the ischemic stroke, hospitalization for heart failure, or ventricular arrhythmia risk was observed between groups. The results remained similar after considering death as a competing risk. The cumulative incidences of all-cause mortality, myocardial infarction, ischemic stroke, and end-stage renal disease are illustrated in Fig. 1.
Subgroup Analyses for Risks of All-Cause Mortality and Clinical Outcomes Stratified by Septic Shock Status
In the subgroup analysis stratified by with and without septic shock, the effects of serum TCO2 on all-cause mortality (P for interaction = 0.122), myocardial infarction (P for interaction = 0.956), ischemic stroke (P for interaction = 0.753), hospitalization for heart failure (P for interaction = 0.941), ventricular arrhythmia (P for interaction = 0.638), and end-stage renal disease (P for interaction = 0.794) were consistent across patient subgroups (Table 3).
Discussion
In this study, we demonstrated that lower serum TCO2 levels were associated with greater risks of adverse long-term outcomes in sepsis survivors. Patients with low TCO2 levels were at greater risk of all-cause mortality, myocardial infarction, and end-stage renal disease than were those with high TCO2 levels over a 10-year study period.
Cardiovascular events are considered to be important contributors to increased long-term mortality in sepsis survivors. Yende et al. [15] conducted a large retrospective cohort analysis with 4179 sepsis survivors and 819,283 control subjects, demonstrating that sepsis survivors had a 1.9-fold higher risk of the 1-year incidence of cardiovascular events (stroke, myocardial infarction, coronary revascularization, and transient ischemic attack) relative to matched-population control subjects.
Accumulating evidence identifies acidosis as a contributor to the progression of kidney disease in people with CKD [21, 22]. The multicenter prospective observational CRIC study, which included 3939 participants with CKD stages 2–4 followed for a median of 3.9 years, demonstrated that each 1-mEq/L increase in the serum bicarbonate level was associated with a 3% reduced risk of a composite renal outcome (eGFR decline ≥ 50% or eGFR < 15 mL/min/1.73 m2) [22]. However, the serum bicarbonate level was not associated significantly with all-cause mortality or atherosclerotic cardiovascular events (myocardial infarction, stroke, and peripheral arterial disease). Patients with diabetes were not excluded from the CRIC study, as has been done in other studies, and accounted for nearly half of the study population. Diabetes, a cardiovascular risk equivalent, may influence the interaction between the serum bicarbonate level and mortality. In a retrospective observational cohort study including 5422 patients, serum bicarbonate levels ≤ 22 mmol/L were associated with a 54% increased risk of kidney disease progression compared with serum bicarbonate levels of 25–26 mmol/L [21]. Nadir serum bicarbonate levels (< 18 mmol/L) in patients on hemodialysis were also associated with a greater mortality risk than were levels of 18–23 mmol/L [34]. Consistent with these findings, low serum TCO2 levels were associated with a higher mortality rate and worse renal outcomes among sepsis survivors in this study.
Kim et al. [24] concluded that serum TCO2 levels < 20 mEq/L correlated with 28-day mortality in patients with sepsis. However, that study was limited by the examination of short-term mortality as the endpoint. The use of 28-day outcomes in clinical studies may lead to the underestimation of morbidity and mortality, and the drawing of inaccurate inferences. The present study showed that the serum TCO2 level is a predictor of mortality in patients with sepsis over a longer follow-up period.
The pathophysiology underlying this association between low TCO2 level and long-term outcome in sepsis survivors remains unknown. Low TCO2 level commonly indicates metabolic acidosis and would be a surrogate of renal dysfunction, which had been shown to be associated with cardiovascular events and long-term mortality. Metabolic acidosis is associated with the development of cardiovascular disease due to its several detrimental effects on the cardiovascular system, such as induced inflammation, activation of the renin–angiotensin–aldosterone system, and insulin resistance. Inflammation associated with metabolic acidosis may result in endothelial dysfunction and an increased risk of cardiovascular events [35,36,37]. Metabolic acidosis is associated with elevated endothelin and aldosterone levels due to the activation of the renin–angiotensin–aldosterone system [38, 39]. Metabolic acidosis also increases insulin resistance, which may contribute to the pathogenesis of cardiovascular disease [40, 41]. However, further prospective studies are warranted to clarify the causality.
The strengths of the present study include the examination of a large cohort of sepsis survivors over a study period of 10 years. In addition, we investigated associations between the serum TCO2 level and not only all-cause mortality but also adverse cardiovascular outcomes in sepsis survivors. To our knowledge, this study is the first to examine serum TCO2 levels measured after discharge from hospitalization for sepsis, rather than those measured on admission. However, some limitations of this study must be considered. First, the study was observational, and thus may have been affected by selection bias and unmeasured confounding factors; in addition, no inference about causality could be made. Second, we did not have access to partial CO2 pressure or pH measurements for the study participants and cannot exclude the possibility that some of the variation in the bicarbonate levels represented respiratory effects. Additionally, we did not have information on the use of alkali therapy, which may influence the TCO2 level. Finally, long-term clinical outcomes were obtained using linkage to the hospital registry database of the Big Data Center. It is possible that some people may be lost to follow-up during the study period. However, sepsis survivors are a fragile population that requires continued access to medical resources for treatment and the study participants are old, leading to the relatively low possibility of those who do not continue to be followed up at a medical center like our hospital or move to another city.
Conclusion
The sepsis survivors with low serum TCO2 level were associated with higher risks of mortality, myocardial infarction, and end-stage renal disease. Prospective studies are needed to confirm these relationships and to evaluate associations between the serum TCO2 level and adverse long-term outcomes.
References
Hotchkiss RS, Moldawer LL, Opal SM, Reinhart K, Turnbull IR, Vincent JL. Sepsis and septic shock. Nat Rev Dis Primers. 2016;2:16045. https://doi.org/10.1038/nrdp.2016.45.
Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–77. https://doi.org/10.1007/s00134-017-4683-6.
Blanco J, Muriel-Bombín A, Sagredo V, et al. Incidence, organ dysfunction and mortality in severe sepsis: a Spanish multicentre study. Crit Care. 2008;12(6):R158. https://doi.org/10.1186/cc7157.
Conway-Morris A, Wilson J, Shankar-Hari M. Immune activation in sepsis. Crit Care Clin. 2018;34(1):29–42. https://doi.org/10.1016/j.ccc.2017.08.002.
Boomer JS, Green JM, Hotchkiss RS. The changing immune system in sepsis: is individualized immuno-modulatory therapy the answer? Virulence. 2014;5(1):45–56. https://doi.org/10.4161/viru.26516.
Zarbock A, Gomez H, Kellum JA. Sepsis-induced acute kidney injury revisited: pathophysiology, prevention and future therapies. Curr Opin Crit Care. 2014;20(6):588–95. https://doi.org/10.1097/mcc.0000000000000153.
Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the global burden of disease study. Lancet. 2020;395(10219):200–11. https://doi.org/10.1016/s0140-6736(19)32989-7.
Kim HI, Park S. Sepsis: early recognition and optimized treatment. Tuberc Respir Dis. 2019;82(1):6–14. https://doi.org/10.4046/trd.2018.0041.
Yan MY, Gustad LT, Nytrø Ø. Sepsis prediction, early detection, and identification using clinical text for machine learning: a systematic review. J Am Med Inform Assoc. 2022;29(3):559–75. https://doi.org/10.1093/jamia/ocab236.
Shankar-Hari M, Rubenfeld GD. Understanding long-term outcomes following sepsis: implications and challenges. Curr Infect Dis Rep. 2016;18(11):37. https://doi.org/10.1007/s11908-016-0544-7.
Simpson A, Long D, Fleischmann-Struzek C, et al. Long-term functional outcomes after sepsis for adult and pediatric critical care patients-protocol for a systematic review. Front Pediatr. 2021;9:734205. https://doi.org/10.3389/fped.2021.734205.
Callahan LA, Supinski GS. Sepsis-induced myopathy. Crit Care Med. 2009;37(10 Suppl):S354–67. https://doi.org/10.1097/CCM.0b013e3181b6e439.
Rocheteau P, Chatre L, Briand D, et al. Sepsis induces long-term metabolic and mitochondrial muscle stem cell dysfunction amenable by mesenchymal stem cell therapy. Nat Commun. 2015;6:10145. https://doi.org/10.1038/ncomms10145.
Ou SM, Chu H, Chao PW, et al. Long-term mortality and major adverse cardiovascular events in sepsis survivors. A nationwide population-based study. Am J Respir Crit Care Med. 2016;194(2):209–17. https://doi.org/10.1164/rccm.201510-2023OC.
Yende S, Linde-Zwirble W, Mayr F, Weissfeld LA, Reis S, Angus DC. Risk of cardiovascular events in survivors of severe sepsis. Am J Respir Crit Care Med. 2014;189(9):1065–74. https://doi.org/10.1164/rccm.201307-1321OC.
Linder A, Guh D, Boyd JH, Walley KR, Anis AH, Russell JA. Long-term (10-year) mortality of younger previously healthy patients with severe sepsis/septic shock is worse than that of patients with nonseptic critical illness and of the general population. Crit Care Med. 2014;42(10):2211–8. https://doi.org/10.1097/ccm.0000000000000503.
Noritomi DT, Soriano FG, Kellum JA, et al. Metabolic acidosis in patients with severe sepsis and septic shock: a longitudinal quantitative study. Crit Care Med. 2009;37(10):2733–9. https://doi.org/10.1097/ccm.0b013e3181a59165.
Drosatos K, Lymperopoulos A, Kennel PJ, Pollak N, Schulze PC, Goldberg IJ. Pathophysiology of sepsis-related cardiac dysfunction: driven by inflammation, energy mismanagement, or both? Curr Heart Fail Rep. 2015;12(2):130–40. https://doi.org/10.1007/s11897-014-0247-z.
O’Leary TD, Langton SR. Calculated bicarbonate or total carbon dioxide? Clin Chem. 1989;35(8):1697–700.
Kim Y, Massie L, Murata GH, Tzamaloukas AH. Discrepancy between measured serum total carbon dioxide content and bicarbonate concentration calculated from arterial blood gases. Cureus. 2015;7(12):e398. https://doi.org/10.7759/cureus.398.
Shah SN, Abramowitz M, Hostetter TH, Melamed ML. Serum bicarbonate levels and the progression of kidney disease: a cohort study. Am J Kidney Dis. 2009;54(2):270–7. https://doi.org/10.1053/j.ajkd.2009.02.014.
Dobre M, Yang W, Chen J, et al. Association of serum bicarbonate with risk of renal and cardiovascular outcomes in CKD: a report from the chronic renal insufficiency cohort (CRIC) study. Am J Kidney Dis. 2013;62(4):670–8. https://doi.org/10.1053/j.ajkd.2013.01.017.
Raphael KL, Wei G, Baird BC, Greene T, Beddhu S. Higher serum bicarbonate levels within the normal range are associated with better survival and renal outcomes in African Americans. Kidney Int. 2011;79(3):356–62. https://doi.org/10.1038/ki.2010.388.
Kim JH, Jang DH, Jo YH, et al. Serum total carbon dioxide as a prognostic factor for 28-day mortality in patients with sepsis. Am J Emerg Med. 2021;44:277–83. https://doi.org/10.1016/j.ajem.2020.04.006.
Kuan AS, Chen TJ. Healthcare data research: the inception of the Taipei Veterans General Hospital Big Data Center. J Chin Med Assoc. 2019;82(9):679. https://doi.org/10.1097/jcma.0000000000000144.
Ou SM, Lee KH, Tsai MT, Tseng WC, Chu YC, Tarng DC. Sepsis and the risks of long-term renal adverse outcomes in patients with chronic kidney disease. Front Med. 2022;9:809292. https://doi.org/10.3389/fmed.2022.809292.
Lee KH, Chu YC, Tsai MT, et al. Artificial intelligence for risk prediction of end-stage renal disease in sepsis survivors with chronic kidney disease. Biomedicines. 2022. https://doi.org/10.3390/biomedicines10030546.
Zhang Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann Transl Med. 2016;4(2):30. https://doi.org/10.3978/j.issn.2305-5839.2015.12.63.
Donders AR, van der Heijden GJ, Stijnen T, Moons KG. Review: a gentle introduction to imputation of missing values. J Clin Epidemiol. 2006;59(10):1087–91. https://doi.org/10.1016/j.jclinepi.2006.01.014.
Kane LT, Fang T, Galetta MS, et al. Propensity score matching: a statistical method. Clin Spine Surg. 2020;33(3):120–2. https://doi.org/10.1097/bsd.0000000000000932.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46(3):399–424. https://doi.org/10.1080/00273171.2011.568786.
Zhang Z, Kim HJ, Lonjon G, Zhu Y. Balance diagnostics after propensity score matching. Ann Transl Med. 2019;7(1):16. https://doi.org/10.21037/atm.2018.12.10.
Stuart EA, Lee BK, Leacy FP. Prognostic score-based balance measures can be a useful diagnostic for propensity score methods in comparative effectiveness research. J Clin Epidemiol. 2013;66(8 Suppl):S84.e1-S90.e1. https://doi.org/10.1016/j.jclinepi.2013.01.013.
John GF. Very low and high predialysis serum bicarbonate levels are risk factors for mortality: what are the appropriate interventions? Semin Dial. 2010;23(3):253–7. https://doi.org/10.1111/j.1525-139X.2010.00737.x.
Asai M, Takeuchi K, Saotome M, et al. Extracellular acidosis suppresses endothelial function by inhibiting store-operated Ca2+ entry via non-selective cation channels. Cardiovasc Res. 2009;83(1):97–105. https://doi.org/10.1093/cvr/cvp105.
Kendrick J, Shah P, Andrews E, et al. Effect of treatment of metabolic acidosis on vascular endothelial function in patients with CKD: a pilot randomized cross-over study. Clin J Am Soc Nephrol. 2018;13(10):1463–70. https://doi.org/10.2215/cjn.00380118.
Kraut JA, Madias NE. Adverse effects of the metabolic acidosis of chronic kidney disease. Adv Chronic Kidney Dis. 2017;24(5):289–97. https://doi.org/10.1053/j.ackd.2017.06.005.
Wesson DE, Simoni J. Acid retention during kidney failure induces endothelin and aldosterone production which lead to progressive GFR decline, a situation ameliorated by alkali diet. Kidney Int. 2010;78(11):1128–35. https://doi.org/10.1038/ki.2010.348.
Wesson DE, Simoni J, Broglio K, Sheather S. Acid retention accompanies reduced GFR in humans and increases plasma levels of endothelin and aldosterone. Am J Physiol Ren Physiol. 2011;300(4):F830–7. https://doi.org/10.1152/ajprenal.00587.2010.
Souto G, Donapetry C, Calviño J, Adeva MM. Metabolic acidosis-induced insulin resistance and cardiovascular risk. Metab Syndr Relat Disord. 2011;9(4):247–53. https://doi.org/10.1089/met.2010.0108.
Baldini N, Avnet S. The effects of systemic and local acidosis on insulin resistance and signaling. Int J Mol Sci. 2018. https://doi.org/10.3390/ijms20010126.
Acknowledgements
Funding
This work was supported in part by the Ministry of Science and Technology, Taiwan (MOST 107-2314-B-075-052, MOST 108-2314-B-075-008, MOST 109-2314-B-075-067-MY3, MOST 110-2634-F-A49-005); the Taipei Veterans General Hospital (V109B-022, V109D50-001-MY3-1, V109D50-001-MY3-2, V109D50-001-MY3-3, V109D50-002-MY3-3, V110C-152, V111C-171, V112C-175, V112D66-002-MY2-1). The funders did not play any roles in the study design, data collection or analysis, decision to publish, or preparation of the manuscript. The Rapid Service Fee was funded by the authors.
Author Contributions
Ching Han Yang, Yee-An Chen, Shuo-Ming Ou and Der-Cherng Tarng contributed in the conception and design of the study, and interpretation of data and drafting the article. Ching Han Yang, Pin-Jie Bin and Shuo-Ming Ou contributed in the acquisition of data and statistical analysis. Ching Han Yang, Yee-An Chen, Pin-Jie Bin, Shuo-Ming Ou and Der-Cherng Tarng contributed in the revision the article. All authors gave their final approval of the version to be submitted.
Disclosures
Ching Han Yang, Yee-An Chen, Pin-Jie Bin, Shuo-Ming Ou, Der-Cherng Tarng have no conflicts to declare.
Compliance with Ethics Guidelines
The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. Ethical approval for this study was obtained from the Ethical Committee of Taipei Veterans General (2017-09-002BC), and the study was conducted under the relevant guidelines and regulations. Informed consent was waived because de-identified data were analyzed.
Data Availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yang, C.H., Chen, YA., Bin, PJ. et al. Associations of the Serum Total Carbon Dioxide Level with Long-Term Clinical Outcomes in Sepsis Survivors. Infect Dis Ther 12, 687–701 (2023). https://doi.org/10.1007/s40121-023-00765-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00765-6