Abstract
Objective
Our study aimed to investigate the predictive value of intracranial pressure (ICP) and cerebral oxygen metabolism monitoring in the postoperative prognosis of patients with spontaneous intracerebral hemorrhage (SICH).
Methods
The clinical data of 55 patients with SICH treated by neurosurgery were analyzed retrospectively. These patients were divided into two groups based on postoperative Glasgow Outcome Scale (GOS) scores, i.e., the poor prognosis group (GOS I-III) and the good prognosis group (GOS IV and V). Next, the ICP and cerebral oxygen metabolism indexes, such as brain temperature (BT), cerebral perfusion pressure (CPP), internal jugular venous oxygen saturation (SjvO2), and arterial partial pressure of carbon dioxide (PaCO2), were recorded after the operation. Further, the prognostic differences between the two groups were compared, and the predictive values were evaluated using the receiver operating characteristic curve (ROC) and area under the curve (AUC).
Results
The results showed that the average ICP and BT in the good prognosis group were lower than those in the poor prognosis group. However, the CPP and SjvO2 in the good prognosis group were higher than those in the poor prognosis group. Moreover, the incidence of low PaCO2 in the poor prognosis group was higher than that in the good prognosis group.
Conclusions
Our results demonstrated that the average ICP, BT, CPP, SjvO2, and arterial PaCO2 may reflect the changes in brain function and cerebral blood flow, which are significantly correlated with the prognosis of patients. Further, our findings indicated that the combined postoperative ICP levels with cerebral oxygen metabolism indexes could guide clinical treatments and predict prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spontaneous intracerebral hemorrhage (SICH) is a cerebral hemorrhage caused by arterial rupture and is characterized by high morbidity, mortality and disability rate. The incidence of SICH in patients in Europe and the US is 9–28% whereas in China, it is 19–48% [1, 2]. According to a report, the mortality rate of patients with SICH within 30 days is approximately 45% [3]. Although the mortality rate has been reduced owing to surgical intervention, the incidence of neurological function disorders in patients with SICH is still relatively high. Thus, SICH is considered to be one of the most challenging public health problems worldwide [4, 5]. A high intracranial pressure (ICP) was shown to be an independent risk factor for poor prognosis after SICH, and patients with long-term ICP > 22 mmHg require medical intervention to reduce ICP [6, 7]. However, many cerebral oxygen metabolic indexes vary, which eventually leads to ICP instability. In this study, we retrospectively analyzed a series of intracranial physiological and pathological indexes (ICP, brain temperature (BT), cerebral perfusion pressure (CPP), internal jugular venous oxygen saturation (SjvO2), and arterial partial pressure of carbon dioxide (PaCO2)) in patients with SICH. Further, the study explored the role of ICP in combination with cerebral oxygen metabolism indexes to predict the prognosis of patients with SICH.
Data and methods
Patient information and grouping
The clinical data of 55 patients with SICH, including 27 males and 28 females who underwent surgery at the Department of Neurosurgery of Shaanxi Provincial people’s Hospital from June 2020 to December 2021, were analyzed retrospectively. According to the guidelines [8], all patients were administered the basic treatment of hemostasis and intravenous antihypertensive therapy. Blood pressure was controlled under 140 mmHg to prevent hematoma expansion and nervous system deterioration, to promote functional recovery. The Glasgow Coma Scale (GCS) score of the patients was between 4 and 9. According to the Glasgow Outcome Scale (GOS) scores, patients were divided into two groups at 3 month postoperatively: the poor prognosis group (GOS I–III) and the good prognosis group (GOS IV–V). The study methods complied with the principles of the Helsinki Declaration. With the approval of the hospital ethics committee, family members of each patient provided signed informed consent for operation and placement of the ICP probe. The inclusion criteria of the study were as follows: (1) Brain CT scan indicating symptoms of intracranial hemorrhage, (2) patients with emergency surgical indications, including evacuation of intracranial hematoma, decompression of bone flap or minimally invasive neuroendoscopic surgery, and intraventricular ICP probe with brain temperature monitoring function placed after the operation, (3) central venous catheters placed in patients after the operation, and (4) intracranial pressure, cerebral oxygen metabolism, and arterial blood gas were monitored for 3 consecutive days after the operation. However, the exclusion criteria were as follows: (1) previous surgical history, (2) patients with multiple organ failures or other serious underlying diseases who cannot tolerate surgical treatment, (3) patients long-term anticoagulant or antiplatelet drug treatment, (4) recurrent stroke within 3 months.
All patients were transferred to the ICU after the operation and the head CT scan was reexamined within 12 h postoperatively. Moreover, the ICP, BT, and mean arterial pressure (MAP) were collected per hour and SjvO2 and arterial PaCO2 were monitored every 8 h. Further, the average ICP, BT, CPP (CPP = MAP-ICP), SjvO2, and arterial PaCO2 were calculated.
No postoperative recurrent cerebral hemorrhage was observed in any patient. However, one patient died in the poor prognosis group, whereas no death or loss of mobility state was observed in the good prognosis group.
Some specific treatments were administered as follows:
-
1.
When the postoperative ICP was higher than 22 mmHg and lasted for more than 15 min, dehydration drugs were administered intravenously, and analgesic and sedative drugs were also administered intravenously.
-
2.
When the postoperative ICP was higher than 30 mmHg, intermittent and rapid administration of multiple dehydration drugs, cerebrospinal fluid drainage, analgesic and sedative therapy, and hyperventilation therapy was implemented.
-
3.
When the postoperative ICP was higher than 45 mmHg, the head CT scan was reexamined and reoperation was considered according to the situation.
-
4.
"Postoperative brain temperature management": the BT was controlled at 37℃. However, when the BT was above 37℃, an ice cap or ice blanket was used.
Data extraction
The ICP probe with BT monitor implanted into the ventricle of patients after the operation was removed after 3 days. The ICP and BT data stored on the intracranial pressure monitor were collected hourly, and the average value was calculated. The CPP obtained was the difference between the MAP and ICP. Besides, central venous catheterization was performed in patients, and the SjvO2 value was obtained every 8 h. Meanwhile, arterial blood gas analysis was performed to obtain PaCO2.
Statistical analysis
SPSS 22.0 software was used for statistical analysis. A Student’s t-test was used to compare the measurement data following normal distribution, and the data were expressed in terms of mean ± standard deviation. The Mann_Whitney U test was used to analyze the non-normal distribution of measurement data between groups, and the data were expressed using median (M) and quartile (IQR). Moreover, the classified variables were expressed by the number of cases and percentage or constituent ratio. The chi-square and Fisher’s exact probability tests were used for comparison. A P_value < 0.05 was considered statistically significant. The MedCalc software (version 19.0.2) was used to prepare the subject receiver operating characteristic curve (ROC), and the area under the ROC curve (AUC) was calculated to evaluate the significance of each index in predicting the prognosis of patients.
Results
Comparison of baseline and cerebral oxygen metabolism indexes between the two groups
No significant difference in age, sex, and GCS score was observed between the good prognosis group (n = 31) and the poor prognosis group (n = 24). However, the average ICP and BT in the good prognosis group (13.42 ± 3.62 vs 27.21 ± 7.87, P < 0.001) were significantly lower than those in the poor prognosis group (36.98 ± 0.54 vs 38.36 ± 0.65, P < 0.001). The CPP and SjvO2 of the good prognosis group (69.32 ± 4.94 vs 56.67 ± 10.09, P < 0.001) were higher than those of the poor prognosis group (65.58 ± 7.13 vs 48.92 ± 10.87, P < 0.001), with a statistically significant difference. The incidence of low PaCO2 in the poor prognosis group was significantly higher than that in the good prognosis group (χ2 = 16.897, P < 0.001), as shown in Table 1.
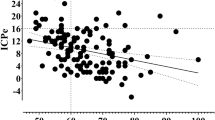
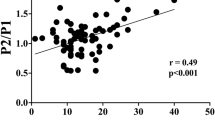
Comparison of different monitoring indexes for predicting poor prognosis of patients
To analyze the significance of different indexes on the poor prognosis of patients with SICH after operation, the average values of indexes were compared which were as follows: ICP (AUC = 0.933, 95% CI 0.832–0.983, P < 0.001), BT (AUC = 0.939, 95% CI 0.840–0.986, P < 0.001), CPP (AUC = 0.848, 95% CI 0.726–0.931, P < 0.001), SjvO2 (AUC = 0.890, 95% CI 0.776–0.958, P < 0.001) and low PaCO2 (AUC = 0.769, 95% CI 0.636–0.872, P < 0.001). The results revealed that the combination of ICP levels with cerebral oxygen metabolic indexes is of significant importance for predicting poor prognosis in patients with SICH, as shown in Table 2. Fig. 1.
Discussion
SICH can cause a series of pathophysiological changes that are usually characterized by the rapid expansion of hematoma in the brain parenchyma, which extends to the ventricular system and subarachnoid space or dural space and leads to a high risk of recurrent cerebral hemorrhage, serious vascular events, epilepsy, dementia, and other neurological complications [9]. Acute hemorrhage is known to damage brain tissue and nerve system, leading to brain dysfunction. However, a large-sized hematoma oppresses the surrounding brain tissue and increases the pressure gradient between the hematoma area and the surrounding tissue, forcing the brain tissue to shift. The obstruction of peripheral vascular circulation, brain ischemia, and hypoxia result in brain edema, leading to a sharp increase in ICP, and eventually to brain hernia. Moreover, the acute and chronic toxic effects of hematoma decomposition lead to brain edema, degeneration, and necrosis, which further increases the ICP levels and aggravates neurological dysfunction. Therefore, it is necessary to remove intracerebral hematoma as early as possible to relieve compression and reduce the ICP levels and cytotoxicity of blood components, which preserves nerve function to the maximum extent and creates favorable conditions for the recovery of brain function [10]. At present, surgical treatments, including craniotomy, minimally invasive surgery, and bone flap decompression, are the main therapeutic strategies for SICH. Irrespective of the kind of surgical treatments, patients with SICH still have postoperative complications resulting in increased ICP levels, disturbance of cerebral oxygen metabolism and insufficient cerebral perfusion which affects the postoperative neurological functions and the quality of patients’ life. Therefore, during treatment after SICH, along with the fluctuation of ICP, the hemodynamic indexes reflecting the physiological and pathological of cerebrovascular should also be monitored. ICP, BT, CPP, SjvO2, and PaCO2 were found to be of great significance in predicting the prognosis of traumatic brain injury (TBI) [11]. Our study evaluated the significance of these parameters to predict the prognosis of patients with SICH.
Secondary brain injury caused by increased ICP levels is one of the main causes of poor prognosis in patients with SICH. High ICP levels increase the inhomogeneity of capillary permeability, which causes disorders of cerebral microcirculation, blood shunt, and suboptimal transport of energy substrates. The average ICP levels can indicate the occurrence and development of secondary damage and predict the optimal time point for intervention [12], which is very important for determining the time of surgery, standardizing the dose of dehydration drugs, and improving prognosis. For the prevention and treatment of secondary injuries in patients with SICH, the best CPP should be maintained while controlling the BP. The control of ICP levels alone without CPP may lead to insufficient perfusion, which increases the risk of cerebral ischemia, thus affecting the prognosis [13]. Besides, physiological cerebrovascular dysfunction is also an important factor in the pathogenesis of SICH. CPP levels indirectly reflect cerebral blood flow (CBF) and cerebral oxygen supply as well as the response of cerebrovascular autoregulation to blood pressure fluctuation, which can predict the deterioration of intracranial disease and suggest the outcome of the disease. Neurological dysfunction and secondary brain injury are attributed to the decrease in CBF and microcirculation perfusion, which further worsen brain edema and form a vicious circle. Therefore, clinical treatment under the guidance of CPP has been widely promoted [14]. At present, the CPP threshold has been determined to be 60–70 mmHg under TBI therapy, whereas the levels are not unified under the SICH treatment. The results of our study showed that the average CPP of the good prognosis group was significantly higher than that of the poor prognosis group, whereas the average ICP of the good prognosis group was lower than that of the poor prognosis group. This suggests that sufficient CPP should be ensured and specific CBF should be maintained to reduce secondary brain injury in patients with SICH [15].
BT is closely related to brain metabolism and the intracranial environment. An increase in BT may reflect the fluctuation in brain metabolism, hyperemia, or local inflammation. The increase in temperature leads to an increase in cerebral blood perfusion. This high cerebral blood volume may increase ICP [16]. Thus, an increase in BT results in the following aspects: (1) elevated levels of excitatory amino acids (such as glutamic acid and dopamine), free radicals, lactic acid, and pyruvate, (2) increased ischemic depolarization, (3) destruction of blood_brain barrier, (4) inhibition of protein kinase and activation of some matrix metalloproteinases, and (5) decreased cytoskeleton stability. Therefore, CBF and metabolism are thought to be the main factors in brain temperature regulation. During cerebral hypoperfusion or ischemia, a reduction in CBF may increase the brain temperature [17]. The increase in BT is related to diffused depolarization, which is similar to the active process of high metabolism. Neurons remain in a state of depolarization for a long time, and the cytotoxicity increases in severity, which eventually leads to necrosis or apoptosis and causes irreversible damage to neurons [18]. Our study revealed that the average BT of the good prognosis group was significantly lower than that of the poor prognosis group. Moreover, the ROC curve indicated that the prediction of prognosis by BT is highly significant.
The artificial hyperventilation is used after craniocerebral surgery in addition to dehydration and diuresis to reduce ICP through cerebral vasoconstriction and cerebral perfusion. However, inappropriate hyperventilation can lead to a significant decrease in CBF and an imbalance between cerebral oxygen supply and demand, resulting in neurological complications and increased mortality and disability rates [19]. Therefore, it is essential to monitor CBF and oxygen metabolism after craniocerebral surgery. SjvO2 monitoring is a technique for estimating the overall balance between brain oxygen supply and metabolic needs. Nearly 80% of brain tissue reflux venous blood flows rapidly to the jugular bulb through the venous sinus with little extracerebral venous blood mixing [20]. Normally, the SjvO2 value is between 55 ~ 75%. A value less than 55% indicates that the patient has insufficient CBF owing to various reasons (hyperventilation, decreased CPP, and vasospasm) or increased metabolic oxygen demand (CMRO2). A value greater than 75% signifies hyperemia, reduced metabolic requirements of the brain (cell death or mitochondrial dysfunction), and microvascular shunts caused by disturbance of oxygen extraction and diffusion in the damaged brain tissue. These secondary lesions lead to poor neurological prognosis. Thus, SjvO2 monitoring helps determine the balance between CBF and CMRO2, monitor insufficient or excessive cerebral perfusion, and guide the treatment and prevention of secondary brain injury [21].
CBF is primarily regulated by arterial PaCO2. Hypocapnia (PaCO2 < 35 mmHg) may be a common and neglected cause of brain hypoxia after SICH, which is related to poor neurological prognosis and delayed cerebral ischemia [22]. Hypocapnia leads to cerebrospinal fluid alkalosis which affects the nervous system such as cerebrospinal fluid alkalosis reduces CBF through cerebral arterial vasoconstriction, and reduces cerebral blood volume to a lesser extent, resulting in reduced oxygen delivery as seen in patients with brain injury. CBF was observed to decrease approximately 3% as per change in 1 mmHg PaCO2 in patients with brain injury. Secondly, moreover, hypocapnia increases brain oxygen demand by increasing neuronal excitability or inducing seizures [23]. Hypocapnia is also associated with increased CMRO2. Thus, the decrease in oxygen delivery and the increase of CMRO2 lead to the imbalance of blood flow-metabolism, resulting in the transition to anaerobic metabolism or leading to cerebral ischemia, especially in the brain tissue with pre-existing CBF damage. Therefore, cerebrospinal fluid alkalosis can lead to neurotoxicity, especially through the production of excitatory amino acids, such as N-methyl-d-aspartic acid, which have severe cell cytotoxicity [24]. This suggests that hyperventilation should be carried out under the monitor of cerebral oxygenation indexes (partial pressure of brain oxygen or internal jugular venous oxygen saturation) to avoid cerebral hypoxia and increase the prognosis.
Craniotomy is the main surgical method for the treatment of SICH and the hematoma can be removed thoroughly. Although some shortcomings of craniotomy should be paid attention, including severe trauma, obvious brain tissue injury, high blood loss, long operation time, severe brain edema reaction, many complications, poor prognosis and curative effect [25]. SICH commonly occurs in deep brain tissue, such as the basal ganglia and thalamus and to remove the hematoma from the deeper areas, a large layer of brain tissue must be punctured during the operation, which may lead to iatrogenic damage to healthy brain tissue. In addition, postoperative complications under such clinical situations are common like rebleeding and infection which increases mortality, leading to poor prognosis [26]. In recent years, with the development of imaging technology, neuroendoscopy is combined with microneurosurgery, neuronavigation and intraoperative ultrasound, which makes it possible to fulfill the advantages of accurate location, less trauma and good curative effect in operations. During the endoscopic surgery of patients with SICH, the endoscope can be placed into the hematoma cavity which exposes the operation field in a panoramic manner and avoids the residual hematoma and further reduce the damage to healthy brain tissue and surgical trauma. Rapid removal of hematoma can reduce nerve damage, high-definition imaging can quickly identify active bleeding points, which is beneficial to hemostasis and reduces the risk of secondary bleeding', the process is crucial for improving the prognosis and living ability of patients [27]. The advantages of neuroendoscopic surgery have been recognized increasingly by neurosurgeons in the treatment of patients with SICH. In this study, six patients treated with neuroendoscope had good postoperative indexes and better prognosis. However, the sample size studied was too small and needs further validation.
Conclusions
The prognosis of patients with SICH is often poor and challenging. Our study assessed a variety of monitoring methods which are used to reflect different pathophysiological conditions in postoperative patients with SICH and explored their predictive values. It was suggested that the average ICP indicated intracranial space-occupying which guided dehydration and surgical treatment. Similarly, BT and CPP suggested hemodynamic changes, guided treatments and predicted prognosis. Moreover, the levels of SjvO2 and arterial PaCO2 suggested the changes of cerebral oxygen metabolism and CBF. Further, ROC curve determined that combined postopertaive ICP levels with cerebral oxygen metabolism indexes such as CPP, BT, SjvO2 and arterial PaCO2 could guide the clinical intervention and predict the prognosis of patients with SICH more effectively.
References
Zhou M, Wang H, Zeng X et al (2019) Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the global burden of disease study 2017 [published correction appears in lancet. 2020 Jul 4;396(10243):26]. Lancet 394(204):1145–1158. https://doi.org/10.1016/S0140-6736(19)30427-1
Hemphill JC 3rd, Greenberg SM, Anderson CS et al (2015) Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke 46(7):2032–2060. https://doi.org/10.1161/STR.0000000000000069
Rincon F, Mayer SA (2010) Intracerebral hemorrhage: getting ready for effective treatments. Curr Opin Neurol 23(1):59–64. https://doi.org/10.1097/WCO.0b013e3283352c01
Zhang K, Wei L, Zhou X, Yang B, Meng J, Wang P (2021) Risk factors for poor outcomes of spontaneous supratentorial cerebral hemorrhage after surgery [published online ahead of print, 2021 Nov 17]. J Neurol. https://doi.org/10.1007/s00415-021-10888-w
Peng WJ, Li Q, Tang JH et al (2019) The risk factors and prognosis of delayed perihematomal edema in patients with spontaneous intracerebral hemorrhage. CNS Neurosci Ther 25(10):1189–1194. https://doi.org/10.1111/cns.13219
de Manoel AL (2020) Surgery for spontaneous intracerebral hemorrhage. Crit Care 24(1):45. https://doi.org/10.1186/s13054-020-2749-2 (Published 2020 Feb 7)
Wilkinson DA, Pandey AS, Thompson BG, Keep RF, Hua Y, Xi G (2018) Injury mechanisms in acute intracerebral hemorrhage. Neuropharmacology 134(Pt B):240–248. https://doi.org/10.1016/j.neuropharm.2017.09.033
Lindner A, Rass V, Ianosi BA et al (2021) Individualized blood pressure targets in the postoperative care of patients with intracerebral hemorrhage [published online ahead of print, 2021 Apr 9]. J Neurosurg. https://doi.org/10.3171/2020.9.JNS201024
Al-Kawaz MN, Li Y, Thompson RE et al (2021) Intracranial pressure and cerebral perfusion pressure in large spontaneous intracranial hemorrhage and impact of minimally invasive surgery. Front Neurol 12:729831. https://doi.org/10.3389/fneur.2021.729831 (Published 2021 Aug 26)
Sun G, Fu T, Liu Z et al (2021) The rule of brain hematoma pressure gradient and its influence on hypertensive cerebral hemorrhage operation. Sci Rep 11(1):4599. https://doi.org/10.1038/s41598-021-84108-w (Published 2021 Feb 25)
Donnelly J, Czosnyka M, Adams H et al (2019) Twenty-five years of intracranial pressure monitoring after severe traumatic brain injury: a retrospective single-center analysis. Neurosurgery 85(1):E75–E82. https://doi.org/10.1093/neuros/nyy468
Kawoos U, McCarron RM, Auker CR, Chavko M (2015) Advances in intracranial pressure monitoring and its significance in managing traumatic brain injury. Int J Mol Sci 16(12):28979–97. https://doi.org/10.3390/ijms161226146
Ren J, Wu X, Huang J et al (2020) Intracranial pressure monitoring-aided management associated with favorable outcomes in patients with hypertension-related spontaneous intracerebral hemorrhage. Transl Stroke Res 11(6):1253–1263. https://doi.org/10.1007/s12975-020-00798-w
Riemann L, Beqiri E, Younsi A, Czosnyka M, Smielewski P (2020) Predictive and discriminative power of pressure reactivity indices in traumatic brain injury. Neurosurgery 87(4):655–663. https://doi.org/10.1093/neuros/nyaa039
Toth P, Szarka N, Farkas E et al (2016) Traumatic brain injury-induced autoregulatory dysfunction and spreading depression-related neurovascular uncoupling: pathomechanisms, perspectives, and therapeutic implications. Am J Physiol Heart Circ Physiol 311(5):H1118–H1131. https://doi.org/10.1152/ajpheart.00267.2016
Mrozek S, Vardon F, Geeraerts T (2012) Brain temperature: physiology and pathophysiology after brain injury. Anesthesiol Res Pract 2012:989487. https://doi.org/10.1155/2012/989487
Wang H, Kim M, Normoyle KP, Llano D (2016) Thermal regulation of the brain-an anatomical and physiological review for clinical neuroscientists. Front Neurosci 9:528. https://doi.org/10.3389/fnins.2015.00528 (Published 2016 Jan 21)
Schiefecker AJ, Kofler M, Gaasch M et al (2018) Brain temperature but not core temperature increases during spreading depolarizations in patients with spontaneous intracerebral hemorrhage. J Cereb Blood Flow Metab 38(3):549–558. https://doi.org/10.1177/0271678X17703940
Kelly AM (2010) Review article: can venous blood gas analysis replace arterial in emergency medical care. Emerg Med Australas 22(6):493–498. https://doi.org/10.1111/j.1742-6723.2010.01344.x
Lu H, Gong Z, Song Y, Jiang R (2020) Application of P(jv-a) CO2 in monitoring cerebral oxygen supply-demand balance in injured brain. J Clin Neurosci 71:213–216. https://doi.org/10.1016/j.jocn.2019.11.028
Nordström CH, Koskinen LO, Olivecrona M (2017) Aspects on the physiological and biochemical foundations of neurocritical care. Front Neurol 8:274. https://doi.org/10.3389/fneur.2017.00274 (Published 2017 Jun 19)
Yokoyama S, Hifumi T, Okazaki T et al (2018) Association of abnormal carbon dioxide levels with poor neurological outcomes in aneurysmal subarachnoid hemorrhage: a retrospective observational study. J Intens Care 6:83. https://doi.org/10.1186/s40560-018-0353-1 (Published 2018 Dec 17)
Godoy DA, Seifi A, Garza D, Lubillo-Montenegro S, Murillo-Cabezas F (2017) Hyperventilation therapy for control of posttraumatic intracranial hypertension. Front Neurol 8:250. https://doi.org/10.3389/fneur.2017.00250 (Published 2017 Jul 17)
Esnault P, Roubin J, Cardinale M et al (2019) Spontaneous hyperventilation in severe traumatic brain injury: incidence and association with poor neurological outcome. Neurocrit Care 30(2):405–413. https://doi.org/10.1007/s12028-018-0639-0
Beynon C, Schiebel P, Bösel J, Unterberg AW, Orakcioglu B (2015) Minimally invasive endoscopic surgery for treatment of spontaneous intracerebral haematomas. Neurosurg Rev 38(3):421–428. https://doi.org/10.1007/s10143-015-0606-6
Zhu H, Wang Z, Shi W (2012) Keyhole endoscopic hematoma evacuation in patients. Turk Neurosurg 22(3):294–299. https://doi.org/10.5137/1019-5149.JTN.5136-11.1
Tang Y, Yin F, Fu D, Gao X, Lv Z, Li X (2018) Efficacy and safety of minimal invasive surgery treatment in hypertensive intracerebral hemorrhage: a systematic review and meta-analysis. BMC Neurol 18(1):136. https://doi.org/10.1186/s12883-018-1138-9 (Published 2018 Sep 3)
Funding
Systematic study of artificial intelligence technology in the diagnosis and treatment of patients with spontaneous cerebral hemorrhage, S2022-YF-YBSF-1399, Xingyu Miao.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Informed consent
Informed consent was obtained during hospitalization from the next of kin or by the patient after recovery at follow-up.
Ethics approval
This study is in line with the principles of the Helsinki Declaration and approved by the hospital ethics committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sun, Z., Liu, J., Dong, S. et al. Prognostic predictive value of intracranial pressure and cerebral oxygen metabolism monitoring in patients with spontaneous intracerebral hemorrhage. Acta Neurol Belg 123, 1815–1821 (2023). https://doi.org/10.1007/s13760-022-02037-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-022-02037-5