Abstract
Background
Sepsis-associated brain dysfunction (SABD) is frequent and is associated with poor outcome. Changes in brain hemodynamics remain poorly described in this setting. The aim of this study was to investigate the alterations of cerebral perfusion pressure and intracranial pressure in a cohort of septic patients.
Methods
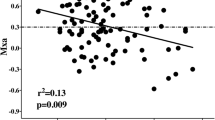
We conducted a retrospective analysis of prospectively collected data in septic adults admitted to our intensive care unit (ICU). We included patients in whom transcranial Doppler recording performed within 48 h from diagnosis of sepsis was available. Exclusion criteria were intracranial disease, known vascular stenosis, cardiac arrhythmias, pacemaker, mechanical cardiac support, severe hypotension, and severe hypocapnia or hypercapnia. SABD was clinically diagnosed by the attending physician, anytime during the ICU stay. Estimated cerebral perfusion pressure (eCPP) and estimated intracranial pressure (eICP) were calculated from the blood flow velocity of the middle cerebral artery and invasive arterial pressure using a previously validated formula. Normal eCPP was defined as eCPP ≥ 60 mm Hg, low eCPP was defined as eCPP < 60 mm Hg; normal eICP was defined as eICP ≤ 20 mm Hg, and high eICP was defined as eICP > 20 mm Hg.
Results
A total of 132 patients were included in the final analysis (71% male, median [interquartile range (IQR)] age was 64 [52–71] years, median [IQR] Acute Physiology and Chronic Health Evaluation II score on admission was 21 [15–28]). Sixty-nine (49%) patients developed SABD during the ICU stay, and 38 (29%) were dead at hospital discharge. Transcranial Doppler recording lasted 9 (IQR 7–12) min. Median (IQR) eCPP was 63 (58–71) mm Hg in the cohort; 44 of 132 (33%) patients had low eCPP. Median (IQR) eICP was 8 (4–13) mm Hg; five (4%) patients had high eICP. SABD occurrence and in-hospital mortality did not differ between patients with normal eCPP and patients with low eCPP or between patients with normal eICP and patients with high eICP. Eighty-six (65%) patients had normal eCPP and normal eICP, 41 (31%) patients had low eCPP and normal eICP, three (2%) patients had low eCPP and high eICP, and two (2%) patients had normal eCPP and high eICP; however, SABD occurrence and in-hospital mortality were not significantly different among these subgroups.
Conclusions
Brain hemodynamics, in particular CPP, were altered in one third of critically ill septic patients at a steady state of monitoring performed early during the course of sepsis. However, these alterations were equally common in patients who developed or did not develop SABD during the ICU stay and in patients with favorable or unfavorable outcome.



Similar content being viewed by others
Abbreviations
- ABG:
-
Arterial blood gases
- AP:
-
Arterial pressure
- APACHE II:
-
Acute physiology and chronic health evaluation II
- CPP:
-
Cerebral perfusion pressure
- eCPP:
-
Estimated cerebral perfusion pressure
- eICP:
-
Estimated intracranial pressure
- FiO2 :
-
Fraction of inspired oxygen
- FV:
-
Flow velocity
- FVd:
-
Diastolic flow velocity
- FVm:
-
Mean flow velocity
- hICP:
-
High intracranial pressure
- ICP:
-
Intracranial pressure
- ICU:
-
Intensive care unit
- lCPP:
-
Low cerebral perfusion pressure
- MAP:
-
Mean arterial pressure
- MCA:
-
Middle cerebral artery
- nCPP:
-
Normal cerebral perfusion pressure
- nICP:
-
Normal intracranial pressure
- PaCO2 :
-
Partial pressure of carbon dioxide
- PaO2 :
-
Partial pressure of oxygen
- PEEP:
-
Positive end-expiratory pressure
- SABD:
-
Sepsis-associated brain dysfunction
- ScvO2 :
-
Central venous oxygen saturation
- STROBE:
-
Strengthening the reporting of observational studies in epidemiology
- TCD:
-
Transcranial Doppler
References
Crippa IA, Taccone FS, Wittebole X, et al. The prognostic value of brain dysfunction in critically Ill patients with and without sepsis: A Post Hoc analysis of the ICON audit. Brain Sci. 2021;11(5):530. https://doi.org/10.3390/brainsci11050530.
Semmler A, Widmann CN, Okulla T, et al. Persistent cognitive impairment, hippocampal atrophy and EEG changes in sepsis survivors. J Neurol Neurosurg Psychiatry. 2013;84(1):62–9. https://doi.org/10.1136/jnnp-2012-302883.
Widmann CN, Heneka MT. Long-term cerebral consequences of sepsis. Lancet Neurol. 2014;13(6):630–6. https://doi.org/10.1016/S1474-4422(14)70017-1.
Heming N, Mazeraud A, Verdonk F, Bozza FA, Chrétien F, Sharshar T. Neuroanatomy of sepsis-associated encephalopathy. Crit Care. 2017;21(1):65. https://doi.org/10.1186/s13054-017-1643-z.
Czempik PF, Pluta MP, Krzych Ł. Sepsis-associated brain dysfunction: a review of current literature. Int J Environ Res Public Health. 2020;17(16):5852. https://doi.org/10.3390/ijerph17165852.
Mazeraud A, Righy C, Bouchereau E, Benghanem S, Bozza FA, Sharshar T. Septic-associated encephalopathy: a comprehensive review. Neurotherapeutics. 2020;17(2):392–403. https://doi.org/10.1007/s13311-020-00862-1.
Taccone FS, Su F, Pierrakos C, et al. Cerebral microcirculation is impaired during sepsis: an experimental study. Crit Care. 2010;14(4):R140. https://doi.org/10.1186/cc9205.
Cepinskas G, Wilson JX. Inflammatory response in microvascular endothelium in sepsis: role of oxidants. J Clin Biochem Nutr. 2008;42(3):175–84. https://doi.org/10.3164/jcbn.2008026.
Crippa IA, Subirà C, Vincent JL, et al. Impaired cerebral autoregulation is associated with brain dysfunction in patients with sepsis. Crit Care. 2018;22(1):327. https://doi.org/10.1186/s13054-018-2258-8.
Taccone FS, Castanares-Zapatero D, Peres-Bota D, Vincent JL, Berre’ J, Melot C. Cerebral autoregulation is influenced by carbon dioxide levels in patients with septic shock. Neurocrit Care. 2010;12(1):35–42. https://doi.org/10.1007/s12028-009-9289-6.
Bozza FA, Garteiser P, Oliveira MF, et al. Sepsis-associated encephalopathy: a magnetic resonance imaging and spectroscopy study. J Cereb Blood Flow Metab. 2010;30(2):440–8. https://doi.org/10.1038/jcbfm.2009.215.
Papadopoulos MC, Lamb FJ, Moss RF, Davies DC, Tighe D, Bennett ED. Faecal peritonitis causes oedema and neuronal injury in pig cerebral cortex. Clin Sci (Lond). 1999;96(5):461–6.
Gu M, Mei XL, Zhao YN. Sepsis and cerebral dysfunction: BBB damage, neuroinflammation, oxidative stress, apoptosis and autophagy as key mediators and the potential therapeutic approaches. Neurotox Res. 2021;39(2):489–503. https://doi.org/10.1007/s12640-020-00270-5.
Nyberg A, Gremo E, Blixt J, et al. Lung-protective ventilation increases cerebral metabolism and non-inflammatory brain injury in porcine experimental sepsis. BMC Neurosci. 2021;22(1):31. https://doi.org/10.1186/s12868-021-00629-0.
Pang D, Wu YL, Alcamo AM, et al. Early axonal injury and delayed cytotoxic cerebral edema are associated with microglial activation in a mouse model of sepsis. Shock. 2020;54(2):256–64. https://doi.org/10.1097/SHK.0000000000001446.
Donnelly J, Budohoski KP, Smielewski P, Czosnyka M. Regulation of the cerebral circulation: bedside assessment and clinical implications. Crit Care. 2016;20(1):129. https://doi.org/10.1186/s13054-016-1293-6.
Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–77. https://doi.org/10.1007/s00134-017-4683-6.
Pfister D, Schmidt B, Smielewski P, et al. Intracranial pressure in patients with sepsis. Acta Neurochir Suppl. 2008;102:71–5. https://doi.org/10.1007/978-3-211-85578-2_14.
Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury. Neurosurgery. 2017;80(1):6–15. https://doi.org/10.1227/NEU.0000000000001432.
Rasulo FA, Bertuetti R, Robba C, et al. The accuracy of transcranial Doppler in excluding intracranial hypertension following acute brain injury: a multicenter prospective pilot study. Crit Care. 2017;21(1):44. https://doi.org/10.1186/s13054-017-1632-2.
Lang EW, Lagopoulos J, Griffith J, et al. Noninvasive cerebrovascular autoregulation assessment in traumatic brain injury: validation and utility. J Neurotrauma. 2003;20(1):69–75. https://doi.org/10.1089/08977150360517191.
Czosnyka M, Matta BF, Smielewski P, Kirkpatrick PJ, Pickard JD. Cerebral perfusion pressure in head-injured patients: a noninvasive assessment using transcranial Doppler ultrasonography. J Neurosurg. 1998;88(5):802–8. https://doi.org/10.3171/jns.1998.88.5.0802.
Rasulo FA, Calza S, Robba C, et al. Transcranial Doppler as a screening test to exclude intracranial hypertension in brain-injured patients: the IMPRESSIT-2 prospective multicenter international study. Crit Care. 2022;26(1):110. https://doi.org/10.1186/s13054-022-03978-2.
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–10. https://doi.org/10.1001/jama.2016.0287.
Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med. 2003;31(4):1250–6. https://doi.org/10.1097/01.CCM.0000050454.01978.3B.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. https://doi.org/10.1016/j.ijsu.2014.07.013.
Czosnyka M, Brady K, Reinhard M, Smielewski P, Steiner LA. Monitoring of cerebrovascular autoregulation: facts, myths, and missing links. Neurocrit Care. 2009;10:373–86. https://doi.org/10.1007/s12028-008-9175-7.
Olsen MH, Riberholt CG, Plovsing RR, Møller K, Berg RMG. Reliability of the mean flow index (Mx) for assessing cerebral autoregulation in healthy volunteers. Physiol Rep. 2021;9:e14923. https://doi.org/10.14814/phy2.14923.
Hawryluk GWJ, Citerio G, Hutchinson P, et al. Intracranial pressure: current perspectives on physiology and monitoring. Intensive Care Med. 2022;48(10):1471–81. https://doi.org/10.1007/s00134-022-06786-y.
Rangel-Castilla L, Rangel-Castillo L, Gopinath S, Robertson CS. Management of intracranial hypertension. Neurol Clin. 2008;26(2):521–41. https://doi.org/10.1016/j.ncl.2008.02.003.
Polito A, Eischwald F, Maho AL, et al. Pattern of brain injury in the acute setting of human septic shock. Crit Care. 2013;17(5):R204. https://doi.org/10.1186/cc12899.
Meng L, Wang Y, Zhang L, McDonagh DL. Heterogeneity and variability in pressure autoregulation of organ blood flow: lessons learned over 100+ years. Crit Care Med. 2019;47(3):436–48. https://doi.org/10.1097/CCM.0000000000003569.
Brassard P, Labrecque L, Smirl JD, et al. Losing the dogmatic view of cerebral autoregulation. Physiol Rep. 2021;9(15):14982. https://doi.org/10.14814/phy2.14982.
Asfar P, Meziani F, Hamel JF, et al. High versus low blood-pressure target in patients with septic shock. N Engl J Med. 2014;370(17):1583–93. https://doi.org/10.1056/NEJMoa1312173.
Goodson CM, Rosenblatt K, Rivera-Lara L, Nyquist P, Hogue CW. Cerebral blood flow autoregulation in sepsis for the intensivist: why its monitoring may be the future of individualized care. J Intensive Care Med. 2018;33(2):63–73. https://doi.org/10.1177/0885066616673973.
Rosenblatt K, Walker KA, Goodson C, et al. Cerebral autoregulation-guided optimal blood pressure in sepsis-associated encephalopathy: a case series. J Intensive Care Med. 2020;35(12):1453–64. https://doi.org/10.1177/0885066619828293.
Raabe A, Kopetsch O, Woszczyk A, et al. Serum S-100B protein as a molecular marker in severe traumatic brain injury. Restor Neurol Neurosci. 2003;21(3–4):159–69.
Kanner AA, Marchi N, Fazio V, et al. Serum S100beta: a noninvasive marker of blood-brain barrier function and brain lesions. Cancer. 2003;97(11):2806–13. https://doi.org/10.1002/cncr.11409.
Dostal P, Cerny V, Parizkova R. Sepsis: cause of late deterioration of intracranial pressure in patients with severe traumatic brain injury? Crit Care. 1998;2:1–61.
Kim JA, Wahlster S, LaBuzetta JN, et al. Focused management of patients with severe acute brain injury and ARDS. Chest. 2022;161(1):140–51. https://doi.org/10.1016/j.chest.2021.08.066.
de Azevedo DS, Salinet ASM, de Lima OM, Teixeira MJ, Bor-Seng-Shu E, de Carvalho NR. Cerebral hemodynamics in sepsis assessed by transcranial Doppler: a systematic review and meta-analysis. J Clin Monit Comput. 2017;31(6):1123–32. https://doi.org/10.1007/s10877-016-9945-2.
Pfister D, Siegemund M, Dell-Kuster S, et al. Cerebral perfusion in sepsis-associated delirium. Crit Care. 2008;12(3):R63. https://doi.org/10.1186/cc6891.
Schramm P, Klein KU, Falkenberg L, et al. Impaired cerebrovascular autoregulation in patients with severe sepsis and sepsis-associated delirium. Crit Care. 2012;16(5):R181. https://doi.org/10.1186/cc11665.
Bowie RA, O’Connor PJ, Mahajan RP. Cerebrovascular reactivity to carbon dioxide in sepsis syndrome. Anaesthesia. 2003;58(3):261–5. https://doi.org/10.1046/j.1365-2044.2003.29671.x.
Terborg C, Schummer W, Albrecht M, Reinhart K, Weiller C, Röther J. Dysfunction of vasomotor reactivity in severe sepsis and septic shock. Intensive Care Med. 2001;27(7):1231–4. https://doi.org/10.1007/s001340101005.
Thees C, Kaiser M, Scholz M, et al. Cerebral haemodynamics and carbon dioxide reactivity during sepsis syndrome. Crit Care. 2007;11(6):R123. https://doi.org/10.1186/cc6185.
Berg RM, Plovsing RR. Effects of short-term mechanical hyperventilation on cerebral blood flow and dynamic cerebral autoregulation in critically ill patients with sepsis. Scand J Clin Lab Invest. 2016;76(3):226–33. https://doi.org/10.3109/00365513.2015.1137350.
Cardim D, Robba C, Bohdanowicz M, et al. Non-invasive monitoring of intracranial pressure using transcranial doppler ultrasonography: is it possible? Neurocrit Care. 2016;25(3):473–91. https://doi.org/10.1007/s12028-016-0258-6.
Topcuoglu MA. Transcranial Doppler ultrasound in neurovascular diseases: diagnostic and therapeutic aspects. J Neurochem. 2012;123(Suppl 2):39–51. https://doi.org/10.1111/j.1471-4159.2012.07942.x.
Sheth KN, Stein DM, Aarabi B, et al. Intracranial pressure dose and outcome in traumatic brain injury. Neurocrit Care. 2013;18(1):26–32. https://doi.org/10.1007/s12028-012-9780-3.
Giller CA, Bowman G, Dyer H, Mootz L, Krippner W. Cerebral arterial diameters during changes in blood pressure and carbon dioxide during craniotomy. Neurosurgery. 1993;32(5):737–41.
Newell DW, Aaslid R, Lam A, Mayberg TS, Winn HR. Comparison of flow and velocity during dynamic autoregulation testing in humans. Stroke. 1994;25:793–7. https://doi.org/10.1161/01.str.25.4.793.
Serrador JM, Picot PA, Rutt BK, Shoemaker JK, Bondar RL. MRI measures of middle cerebral artery diameter in conscious humans during simulated orthostasis. Stroke. 2000;31(7):1672–8. https://doi.org/10.1161/01.str.31.7.1672.
Schreiber SJ, Gottschalk S, Weih M, Villringer A, Valdueza JM. Assessment of blood flow velocity and diameter of the middle cerebral artery during the acetazolamide provocation test by use of transcranial Doppler sonography and MR imaging. AJNR Am J Neuroradiol. 2000;21(7):1207–11.
Coverdale NS, Gati JS, Opalevych O, Perrotta A, Shoemaker JK. Cerebral blood flow velocity underestimates cerebral blood flow during modest hypercapnia and hypocapnia. J Appl Physiol. 2014;117(10):1090–6. https://doi.org/10.1152/japplphysiol.00285.2014.
Spilt A, Box FM, van der Geest RJ, et al. Reproducibility of total cerebral blood flow measurements using phase contrast magnetic resonance imaging. J Magn Reson Imaging. 2002;16(1):1–5. https://doi.org/10.1002/jmri.10133.
Valdueza JM, Balzer JO, Villringer A, Vogl TJ, Kutter R, Einhäupl KM. Changes in blood flow velocity and diameter of the middle cerebral artery during hyperventilation: assessment with MR and transcranial Doppler sonography. AJNR Am J Neuroradiol. 1997;18(10):1929–34.
Lindegaard KF, Lundar T, Wiberg J, Sjøberg D, Aaslid R, Nornes H. Variations in middle cerebral artery blood flow investigated with noninvasive transcranial blood velocity measurements. Stroke. 1987;18(6):1025–30. https://doi.org/10.1161/01.str.18.6.1025.
Bishop CC, Powell S, Rutt D, Browse NL. Transcranial Doppler measurement of middle cerebral artery blood flow velocity: a validation study. Stroke. 1986;17(5):913–5. https://doi.org/10.1161/01.str.17.5.913.
Liu Y, Yang X, Gong H, et al. Assessing the effects of norepinephrine on single cerebral microvessels using optical-resolution photoacoustic microscope. J Biomed Opt. 2013;18(7):76007. https://doi.org/10.1117/1.JBO.18.7.076007.
Carrara M, Ferrario M, Bollen Pinto B, Herpain A. The autonomic nervous system in septic shock and its role as a future therapeutic target: a narrative review. Ann Intensive Care. 2021;11:80. https://doi.org/10.1186/s13613-021-00869-7.
Pantzaris ND, Platanaki C, Tsiotsios K, Koniari I, Velissaris D. The use of electroencephalography in patients with sepsis: a review of The literature. J Transl Int Med. 2021;9(1):12–6. https://doi.org/10.2478/jtim-2021-0007.
Rosengarten B, Krekel D, Kuhnert S, Schulz R. Early neurovascular uncoupling in the brain during community acquired pneumonia. Crit Care. 2012;16(2):R64. https://doi.org/10.1186/cc11310.
Ferlini L, Su F, Creteur J, Taccone FS, Gaspard N. Cerebral autoregulation and neurovascular coupling are progressively impaired during septic shock: an experimental study. Intensive Care Med Exp. 2020;8(1):44. https://doi.org/10.1186/s40635-020-00332-0.
Heckelmann M, Shivapathasundram G, Cardim D, et al. Transcranial Doppler-derived indices of cerebrovascular haemodynamics are independent of depth and angle of insonation. J Clin Neurosci. 2020;82(Pt A):115–21. https://doi.org/10.1016/j.jocn.2020.10.037.
Hoskins PR. Accuracy of maximum velocity estimates made using Doppler ultrasound systems. Br J Radiol. 1996;69(818):172–7. https://doi.org/10.1259/0007-1285-69-818-172.
Lau VI, Arntfield RT. Point-of-care transcranial Doppler by intensivists. Crit Ultrasound J. 2017;9(1):21. https://doi.org/10.1186/s13089-017-0077-9.
Robba C, Crippa IA, Taccone FS. Septic encephalopathy. Curr Neurol Neurosci Rep. 2018;18(12):82. https://doi.org/10.1007/s11910-018-0895-6.
Boettger S, Nuñez DG, Meyer R, et al. Delirium in the intensive care setting: a reevaluation of the validity of the CAM-ICU and ICDSC versus the DSM-IV-TR in determining a diagnosis of delirium as part of the daily clinical routine. Palliat Support Care. 2017;15(6):675–83. https://doi.org/10.1017/S1478951516001176.
Reade MC, Eastwood GM, Peck L, Bellomo R, Baldwin I. Routine use of the confusion assessment method for the intensive care unit (CAM-ICU) by bedside nurses may underdiagnose delirium. Crit Care Resusc. 2011;13:217–24.
van Eijk MM, van den Boogaard M, van Marum RJ, et al. Routine use of the confusion assessment method for the intensive care unit: a multicenter study. Am J Respir Crit Care Med. 2011;184(3):340–4. https://doi.org/10.1164/rccm.201101-0065OC.
Zampieri FG, Park M, Machado FS, Azevedo LC. Sepsis-associated encephalopathy: not just delirium. Clinics (Sao Paulo). 2011;66(10):1825–31.
Sonneville R, de Montmollin E, Poujade J, et al. Potentially modifiable factors contributing to sepsis-associated encephalopathy. Intensive Care Med. 2017;43(8):1075–84. https://doi.org/10.1007/s00134-017-4807-z.
Skrobik Y, Duprey MS, Hill NS, Devlin JW. Low-dose nocturnal dexmedetomidine prevents ICU delirium. A randomized, placebo-controlled trial. Am J Respir Crit Care Med. 2018;197(9):1147–56. https://doi.org/10.1164/rccm.201710-1995OC.
Ely EW, Inouye SK, Bernard GR, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001;286(21):2703–10. https://doi.org/10.1001/jama.286.21.2703.
Funding
No funding was received for the present study. IAC, JC, NG, and FST are supported by the Fonds d’Excellence of Fondation Erasme (2015–2021).
Author information
Authors and Affiliations
Contributions
Conceptualization: FST, IAC; methodology: IAC, FST; investigation: IAC, FZC, SP, CM; analysis of data: IAC; writing original draft: IAC; review and editing: IAC, JLV, FZC, SP. NG, CM, JC, FST. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no competing interests.
Ethical Approval/Informed Consent
The study protocol was approved by the Ethics Committee of the Erasme Hospital (P2021/493), which waived the need for an informed consent because of the retrospective analysis of anonymized data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Crippa, I.A., Vincent, JL., Zama Cavicchi, F. et al. Estimated Cerebral Perfusion Pressure and Intracranial Pressure in Septic Patients. Neurocrit Care 40, 577–586 (2024). https://doi.org/10.1007/s12028-023-01783-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-023-01783-5