Abstract
Introduction
Several systemic therapies have been approved for the treatment of severe AD. In particular, Janus kinase inhibitors (JAKi), including abrocitinib, baricitinib, and upadacitinib, recently received approval for the treatment of patients with severe AD after being evaluated in several clinical trials. However, a few concerns have been raised regarding their long-term safety and the management of these drugs in real-world clinical practice. In this article we described the results of a Delphi consensus aimed at describing the knowledge on JAKi and focusing, in particular, on providing clinical recommendations for dermatologists in daily practice regarding the use of these drugs.
Methods
Twelve Italian dermatologists reviewed the most recent literature regarding the efficacy and safety profiles of JAKi and proposed 24 statements.
Results
Agreement was reached for statements focusing on three main topics: (1) place in therapy of JAKi in patients with moderate-to-severe AD; (2) effectiveness and safety of JAK inhibitors in different phenotypes; (3) different approaches to the management of patients treated with JAKi in clinical practice. The panel proposed several recommendations regarding all the statements.
Conclusion
Given the wide use of JAKi in clinical practice, it is crucial to establish a specific follow-up for each patient’s phenotype in order to achieve the best possible clinical outcome and minimize potential adverse events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
JAK inhibitors are very effective drugs approved for the treatment of severe atopic dermatitis. |
Given recent concerns emerging on the safety profile of JAK inhibitors, we carried out a Delphi consensus on the management of patients treated with these drugs in clinical practice. |
A detailed medical history should be obtained from each patient before starting the JAK inhibitor. |
JAK inhibitors could be prescribed to patients aged 65 years old or older in the absence of medical history or significant risk factors for cardiovascular disease and/or malignancies. |
Introduction
Atopic dermatitis (AD) is one of the most common inflammatory skin diseases worldwide [1]. AD usually presents with eczematous patches and intense itch that can significantly impair patients’ quality of life and productivity [1]. For decades, the management of AD has relied on topical emollients and corticosteroids for mild-to-moderate disease, while the systemic treatments approved in Europe were cyclosporine, methotrexate, azathioprine, and short courses of oral corticosteroids [2]. However, these treatments are unfeasible for the long-term management of this disease. During the last 5 years, several new drugs have been approved for severe AD. In particular, according to European guidelines, patients with severe AD should be treated with biological drugs (such as dupilumab and tralokinumab) or Janus kinase (JAK) inhibitors, such as abrocitinib, baricitinib, and upadacitinib [3]. JAK inhibitors have shown efficacy and safety in multiple phase III clinical trials and in a few initial real-world experiences [4,5,6,7,8,9]. However, a few concerns have been raised regarding their long-term safety and the management of these drugs in real-world clinical practice [7, 10]. Upadacitinib and abrocitinib are selective inhibitors of JAK-1, and they are each currently approved at two different dosages (30 mg and 15 mg for upadacitinib and 200 mg and 100 mg for abrocitinib). Baricitinib is an inhibitor of both JAK-1 and JAK-2, and it is approved for both AD and alopecia areata across two different dosages, 4 mg and 2 mg daily [11,12,13].
In this article, we describe the results of a Delphi consensus aimed at describing the knowledge on JAK inhibitors and focusing, in particular, on providing clinical recommendations for dermatologists in daily practice regarding the use of these drugs.
Methods
The use of JAK inhibitors for the treatment of severe AD is increasing constantly. However, current guidelines do not often give specific advice for the management of these patients, in particular regarding the place in therapy of JAK inhibitors and their role in difficult-to-treat subpopulations with multiple comorbidities and concomitant medications. We aimed to discuss current evidence on real-world data on JAK inhibitors, along with the clinical experience of a cohort of Italian dermatologists specialized in AD with at least 1 year of experience with JAK inhibitors. We performed a Delphi consensus on 24 statements in order to provide clinical guidance for dermatologists in routine practice. Delphi consensus represents a widely used method in medicine to generate consensus among experts when clinical guidelines are incomplete or lack enough clinical evidence.
A scientific committee of 12 Italian dermatologists reviewed the most recent literature on the efficacy and safety profiles of JAK inhibitors and generated 24 statements focusing on three main topics: (1) place in therapy of JAK inhibitors in patients with moderate-to-severe AD; (2) effectiveness and safety of JAK inhibitors in different patient subgroups; (3) different approaches to the management of patients treated with JAK inhibitors in a real-world clinical setting (Table 1).
During the first meeting in July 2023, all the panel members produced their opinions on the three identified topics. Then, all the opinions were rewritten into statements and shared with all the members. Each panelist was asked to evaluate the statement using a Likert scale (1–5; 1 = total disagreement; 5 = total agreement). In accordance with the recommendations of the Italian Ministry of Health, the consensus on the agreement was reached when ≥ 75% of voters expressed a vote equal to 4 or 5 [14]. After the first round, a second round of voting was performed after reviewing the statements that did not reach agreement. After the second round, the list of approved statements was completed.
Data were analyzed using descriptive statistics.
Institutional review board approval was exempted for this study as its procedures did not include human subjects and did not deviate from good clinical practice. All the involved dermatologists gave their approval for the study to be published. All the dermatologists who were part of the consensus were involved in the writing and/or revision of the manuscript. All the dermatologists who participated in the consensus were aware of the objective of the study, and they all knew that the manuscript will be published. The participants gave written informed consent.
Results
Consensus on the agreement was obtained for 21 out of 24 statements during the first online meeting of the Delphi (Table 1). A consensus was not reached for three statements, two regarding the place in therapy of JAK inhibitors in some patient groups and one on the management of the treatment during concomitant infections. These three statements were modified according to the suggestions of the committee members and were re-presented during the second Delphi round. This time, consensus was obtained. Statements for each topic are discussed in the following sections.
Place in Therapy of JAK Inhibitors
European guidelines for the management of AD do not indicate which drug to prefer for different patient phenotypes (classic AD, predominant involvement of head and neck, hands AD, prurigo nodularis-like, generalized lichenoid, generalized inflammatory, erythroderma, and nummular eczema-like) as cyclosporine, interleukin (IL)-4/13 inhibitors, IL-13 inhibitors, and JAK inhibitors are equally recommended for the treatment of severe AD. During the last couple of years, several reports have evaluated the effectiveness of each treatment for different clinical phenotypes of AD [15,16,17,18]. In particular, Vittrup et al. [15] analyzed 347 adult patients treated with dupilumab, showing a lower effectiveness in those with predominant involvement of head/neck areas. Moreover, dupilumab showed lower effectiveness in patients with significant head, neck, and hand involvement, as recently described by Chiricozzi et al. [16]. On the other hand, baricitinib appears to be more effective in these areas, as described by Thyssen et al. [17]
During the first Delphi round, agreement was reached for the statement 1 regarding the use of JAK inhibitors as first-line treatments in patients with severe involvement of difficult-to-treat areas (face/neck, hands, genitalia). No agreement was obtained in the first round for statement 2, which concerned the preferable use of JAK inhibitors over biologics in patients with severe itch. This statement was rewritten according to the members’ suggestions, shifting the focus to the “itch-dominant” phenotype (patients with itch-NRS ≥ 7 and BSA up to 40%) [17], obtaining the agreement during the second Delphi round.
Consensus was also reached for statements 3 and 4 regarding the viable use of JAK inhibitors in patients with several AD phenotypes (including prurigo-like and nummular eczema-like AD) and those with concomitant AD and plaque psoriasis.
There was no agreement in the first round on statement 5, which suggested the possible use of JAK inhibitors as a first-line treatment in patients with atopic comorbidities (including asthma and allergic rhinitis). The statement was reconsidered after removing the words “first-line,” and it was approved during the second round.
Statement 6, regarding the preferable use of JAK inhibitors compared with dupilumab in patients with a medical history of conjunctivitis, was approved on the basis of the available literature on the different safety profiles of these drugs.
Real-World Effectiveness and Safety of JAK Inhibitors
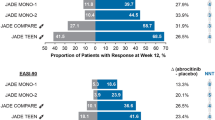
Ten statements were generated on this topic, and they all reached agreement during the first Delphi round. In particular, statements 7–10 highlighted the high effectiveness profiles of all the approved JAK inhibitors, according to data from both clinical trials and real-world experience in terms of both clinical improvement and patient-reported outcomes (PROs) [4,5,6,7,8,9]. In particular, upadacitinib and abrocitinib have demonstrated high rates of EASI 75 and EASI 90 (reduction of at least 75% and 90% of the Eczema Area and Severity Index compared to baseline), along with rapid decrease of the itch and improvement in the quality of life, across all patient groups (biological-naive versus biological-experienced, different phenotypes) [4, 19]. Also, baricitinib has shown significant results in terms of EASI 75 and reductions of itch, particularly in the post hoc analysis of BREEZE-AD7 on the itch-dominant profile, showing the importance of a personalized approach in AD therapies [17,20]
Regarding safety, agreement was reached in statements 11–15 concerning the low rates of treatment-emergent severe adverse events (AEs) and AEs leading to discontinuation in clinical trials and real-world studies. There was also agreement on the absence of absolute contraindication to the prescription of JAK inhibitors in women of childbearing potential. The panel also agreed that, according to existing literature, no increase in the thrombotic risk has been demonstrated during treatment with JAK inhibitors in patients with AD, including women who were taking oral contraceptives [21].
Management of Patients Treated with JAK Inhibitors in Real-World Clinical Practice
Eight statements were proposed to the panel concerning the management of patients in real-life clinical settings, and seven of the statements reached agreement after the first Delphi round. In particular, the panel agreed that it is not mandatory to prescribe contraceptives to women of childbearing potential before starting the treatment after appropriate counseling.
Also, there was agreement regarding the definition of patients with a higher risk of cancer (including those with a medical history and/or a family history of neoplasm diagnosis at young age in two first-degree family members) and higher cardiovascular risk for major adverse cardiovascular events (MACEs; including those with diabetes, smokers, dyslipidemia, hypertension, obesity). In those cases, the anamnesis is fundamental. If the patient presents an increased risk for thrombosis, MACEs, or neoplasm, multidisciplinary management is very important for modifying the variable risk factors inducing a risk reduction linked to the patient’s comorbidities and/or predisposition [22].
The members agreed that anti-herpes zoster vaccination should not be mandatory before starting the treatment. Concerning concomitant vaccinations (excluding live vaccines) and major surgeries occurring during the treatment, the panelists agreed that it is appropriate to interrupt the JAK inhibitor 1 week before and restart 1 week after the procedure (statements 21 and 23). Finally, after the first Delphi round, no agreement was reached on statement 22 suggesting that in the case of concurrent infections requiring systemic antibiotic therapy, suspending the JAK inhibitor until the resolution of the symptoms was recommended. The statement was modified as follows: “In case of concomitant infections, which do not require hospitalization, with fever and related symptoms (e.g., cough, dyspnea), it is advisable to suspend the JAK inhibitor until complete clinical resolution and, where applicable, until laboratory tests normalize.” In this form, this statement reached agreement during the second Delphi round.
Discussion
Abrocitinib, baricitinib, and upadacitinib currently represent three of the six recommended systemic treatments for adult patients with severe AD, according to European guidelines [3]. No specific recommendation is given regarding which treatment to prefer for different patient phenotypes. According to our group, JAK inhibitors could be preferred in those with a high itch-NRS and with significant involvement of sensitive areas (head, hands, genitalia). This is consistent with data from scientific literature since upadacitinib and abrocitinib have both shown more effectiveness and rapidity in treating both AD and subjective symptoms, compared with dupilumab in both head-to-head clinical trials and real-world experience [4,5,6, 19, 23]. Network meta-analyses, despite their limitations, have also shown better outcomes for abrocitinib and upadacitinib compared with anti-IL-13 monoclonal antibodies [24, 25]. Moreover, a recent post hoc analysis of the BREEZE-AD7 clinical trial, a phase III study that compared the efficacy of baricitinib 4 mg plus topical corticosteroids (TCS), with baricitinib 2 mg plus TCS and placebo plus TCS, has shown best results on signs (EASI 75) and symptoms (variations of itch-NRS of at least 4 points) in a clinical AD phenotype characterized by mild-to-moderate lesions (BSA up to 40%) and severe itch (itch-NRS > 7) [17,20]. As already mentioned, this phenotype is known as “itch-dominant” [26] and appears to respond better to baricitinib compared with all the intention-to-treat population of the clinical trials.
Regarding different clinical phenotypes, recent real-world case series have shown the effectiveness of JAK inhibitors, and upadacitinib in patients with overlapping psoriasis and AD features [27]. This could probably be explained by a broader spectrum of actions of JAK inhibitors, given the role of JAK-1 and JAK-2 in the signaling of different cytokines involved in AD and psoriasis pathogenesis. Regarding atopic comorbidities, limited data are available on the possible role of JAK inhibitors in patients with concomitant asthma or allergic rhinitis [28]. Few trials are ongoing with topical JAK-1 inhibitors in patients affected by asthma. As a matter of fact, JAK-1-selective inhibitors that could be used via dry powder inhalation in patients with asthma are currently under evaluation [28]. In this setting of Th2-mediated asthma, JAK-1 inhibition seems to be more efficacious than JAK-3 inhibition [28]. Thus, according to our panel, dupilumab should be preferred. Still, JAK inhibitors could also represent a possible option, especially in patients with mild-to-moderate asthma or rhinitis, as underlined in recent real-world experience [29].
Concerning the real-world effectiveness and safety of JAK inhibitors, data from scientific literature have confirmed data from clinical trials from all three drugs [5,6,7, 9]. In particular, abrocitinib and upadacitinib have shown very high rates of EASI 90 and EASI 100, comparable or superior to phase III clinical trials [4, 17]. Regarding the safety profile of these three drugs, no significant safety findings have emerged from real-life clinical practice compared with clinical trials [30]. To date, safety data for JAK inhibitors in patients with AD are available from clinical trials with a 3-year follow-up, while only limited long-term real-world experiences have been published. In particular, three studies have reached a 52-week observation period [7, 31, 32]. According to those studies, the vast majority of treatment-emergent AEs have been mild or moderate, and only a limited percentage of them have led to discontinuation [21, 33]. Also, currently, there is a consensus on the absence of absolute contraindication to the prescription of JAK inhibitors in women of childbearing potential after appropriate counseling on the importance of abstinence or the use of contraception [34].
Regarding oral contraceptives, it is worth mentioning that most of the women included in phase III clinical trials were taking them concomitantly as a result of the inclusion and exclusion criteria of these studies [4, 19]. According to a study on 22 healthy female subjects, upadacitinib showed no effects on the pharmacokinetics of levonorgestrel and ethinylestradiol [35]. No significant increase in thromboembolism has been reported to date. Moreover, a recent multicenter French real-world study on more than 200 patients confirmed the positive benefit–risk profile of JAK inhibitors, even in a population with cardiovascular comorbidities and multiple risk factors [30].
Regarding the recommendation for the use of JAK inhibitors in patients with AD, in 2022, under the Article 20 of Regulation (EC) No. 726/2004, the Pharmacovigilance Risk Assessment Committee (PRAC) of EMA developed a reassessment (EMA/PRAC/68283/2022) of the benefit–risk balance of oral JAK inhibitors [30, 36]. The final recommendations of the PRAC were released at the end of 2022, and the European Commission’s final decision was issued in March 2023. A recent report from Wollenberg et al. analyzed the PRAC recommendation, underlining that the JAK inhibitors maintain a favorable benefit–risk profile as a first-line therapy in patients under 65 years of age without cardiovascular or malignancy risk factors [36]. They assessed that the benefit–risk profiles of available treatments should be compared for patients with risk factors. Regarding this recommendation, our group reached a consensus on which category of patients should be defined as high risk, including those with recent cardiovascular events and concomitant malignancy. It should also be taken into account that the incidence rates of MACEs, thromboembolism, and malignancies in patients with AD not treated with JAKi and in those treated with JAK inhibitors are comparable in terms of events per 1000 patients-years, according to current literature [21, 30, 36, 37].
The aim of our group was also to give practical recommendations for the management of patients receiving JAK inhibitors. On this topic, guidelines lack consistent evidence to date. In accordance with the summary of product characteristics of the three drugs, the panel agreed that the herpes zoster vaccination may be performed before starting the treatment. Still, it should not be mandatory, in agreement with local immunization guidelines [3, 36]. Similarly, according to the drugs’ SPC, we reached agreement regarding contraception, as women of reproductive potential should, of course, be advised to use effective contraception during treatment and for 1 month following the final dose of JAK inhibitor [11,12,13]. However, the oral contraception should not be mandatory. We also tried to advise patients undergoing medical procedures, including vaccines or surgeries. For both situations, we recommended withdrawing the drug 1 week before and 1 week after the procedure, based on the short half-lives of the three JAK inhibitors [38, 39].
Our study has a few limitations because of the limited number of clinicians included and because of the very limited real-world experience currently available, especially on abrocitinib and baricitinib. Moreover, a selection bias should be mentioned, as most of the panel’s dermatologists specialized in treating AD and were already familiar with JAK inhibitors. Another limitation is due to the intrinsic nature of a Delphi consensus, which is based on both clinical evidence and experts’ opinions.
Conclusion
This Delphi consensus produced 24 statements regarding the management of patients receiving JAK inhibitors in real-world clinical practice. Our suggestions aimed to fill a void in current guidelines in order to give clinicians some advice in this setting. It is crucial to critically update and revise current treatment guidelines in light of the most recent real-world data on new treatment options.
Data Availability
Additional data supporting the findings of this manuscript are available to the corresponding author upon reasonable request.
References
Ali F, Vyas J, Finlay AY. Counting the burden: atopic dermatitis and health-related quality of life. Acta Derm Venereol. 2020;100(12):00161. https://doi.org/10.2340/00015555-3511.
Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the management of atopic dermatitis: section 1. Diagnosis and assessment of atopic dermatitis. J Am Acad Dermatol. 2014;70(2):338–51. https://doi.org/10.1016/j.jaad.2013.10.010.
Wollenberg A, Kinberger M, Arents B, et al. European guideline (EuroGuiDerm) on atopic eczema: part I-systemic therapy. J Eur Acad Dermatol Venereol. 2022;36(9):1409–31. https://doi.org/10.1111/jdv.18345.
Blauvelt A, Teixeira HD, Simpson EL, et al. Efficacy and safety of upadacitinib vs dupilumab in adults with moderate-to-severe atopic dermatitis: a randomized clinical trial. JAMA Dermatol. 2021;157:1047–55.
Gargiulo L, Ibba L, Cortese A, et al. Real-life effectiveness and safety of upadacitinib in adults and adolescents with moderate-to-severe atopic dermatitis: a single-center 16-week study. Dermatol Ther (Heidelb). 2023;13:651–60.
Chiricozzi A, Gori N, Narcisi A, et al. Effectiveness and safety of upadacitinib in the treatment of moderate-severe atopic dermatitis: a multicentric, prospective, real-world, cohort study. Drugs R D. 2022;22:245–52.
Gargiulo L, Ibba L, Piscazzi F, et al. Effectiveness and safety of upadacitinib for moderate-to-severe atopic dermatitis in a real-world setting: a 52-week retrospective study. J Eur Acad Dermatol Venereol. 2023. https://doi.org/10.1111/jdv.19507.
Olydam JI, Schlösser AR, Custurone P, Nijsten TEC, Hijnen D. Real-world effectiveness of abrocitinib treatment in patients with difficult-to-treat atopic dermatitis. J Eur Acad Dermatol Venereol. 2023;37(12):2537–42. https://doi.org/10.1111/jdv.19378.
Napolitano M, Ferrucci SM, Foggia L, et al. Comparison of long-term effectiveness and safety of upadacitinib for atopic dermatitis between dupilumab-exposed and dupilumab-naïve patients. Clin Drug Investig. 2024;44(1):71–7. https://doi.org/10.1007/s40261-023-01336-w.
Ertus C, Scailteux LM, Lescoat A, et al. Major adverse cardiovascular events in patients with atopic dermatitis treated with oral Janus kinase inhibitors: a systematic review and meta-analysis. Br J Dermatol. 2023;189(4):368–80. https://doi.org/10.1093/bjd/ljad229.
European Medicines Agency. Rinvoq (upadacitinib): summary of product characteristics. 2019. https://www.ema.europa.eu/en/medicines/human/EPAR/rinvoq. Accessed 2023 Dec 17.
European Medicines Agency. Cibinqo (abrocitinib): summary of product characteristics. 2021. https://www.ema.europa.eu/en/medicines/human/EPAR/cibinqo. Accessed 2023 Dec 17.
European Medicines Agency. Olumiant (baricitinib): summary of product characteristics. 2017. https://www.ema.europa.eu/en/medicines/human/EPAR/olumiant. Accessed 2023 Dec 17.
Diamond IR, Grant RC, Feldman BM, et al. Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol. 2014;67(4):401–9. https://doi.org/10.1016/j.jclinepi.2013.12.002.
Vittrup I, Krogh NS, Larsen HHP, et al. A nationwide 104 weeks real-world study of dupilumab in adults with atopic dermatitis: ineffectiveness in head-and-neck dermatitis. J Eur Acad Dermatol Venereol. 2023;37(5):1046–55. https://doi.org/10.1111/jdv.18849.
Chiricozzi A, Gori N, Di Nardo L, et al. Therapeutic impact and management of persistent head and neck atopic dermatitis in dupilumab-treated patients. Dermatology. 2022;238(4):717–24. https://doi.org/10.1159/000519361.
Thyssen JP, de Bruin-Weller M, Costanzo A, et al. Baseline body surface area and itch severity define response to baricitinib in patients with moderate-to-severe atopic dermatitis at week 16. Adv Ther. 2023;40(8):3574–87. https://doi.org/10.1007/s12325-023-02528-8.
Napolitano M, Fabbrocini G, Scalvenzi M, Nisticò SP, Dastoli S, Patruno C. Effectiveness of dupilumab for the treatment of generalized prurigo nodularis phenotype of adult atopic dermatitis. Dermatitis. 2020;31(1):81–4. https://doi.org/10.1097/DER.0000000000000517.
Bieber T, Simpson EL, Silverberg JI, et al. Abrocitinib versus placebo or dupilumab for atopic dermatitis. N Engl J Med. 2021;384(12):1101–12. https://doi.org/10.1056/NEJMoa2019380.
Silverberg JI, Simpson EL, Thyssen JP, et al. Long-term efficacy (up to 68 weeks) of baricitinib in combination with topical corticosteroids in adult patients with moderate-to-severe atopic dermatitis: analysis of treatment responders, partial responders and nonresponders originating from study BREEZE-AD7. J Eur Acad Dermatol Venereol. 2023;37(5):1036–45. https://doi.org/10.1111/jdv.18816.
Burmester GR, Cohen SB, Winthrop KL, et al. Safety profile of upadacitinib over 15 000 patient-years across rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis and atopic dermatitis. RMD Open. 2023;9(1):e002735. https://doi.org/10.1136/rmdopen-2022-002735.
Visseren FLJ, Mach F, Smulders YM, et al. ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2021;42(34):3227–337. https://doi.org/10.1093/eurheartj/ehab484.
Simpson EL, Silverberg JI, Thyssen JP, et al. Efficacy and safety of abrocitinib in patients with severe and/or difficult-to-treat atopic dermatitis: a post hoc analysis of the randomized phase 3 JADE COMPARE trial. Am J Clin Dermatol. 2023;24(4):609–21. https://doi.org/10.1007/s40257-023-00785-5.
Drucker AM, Morra DE, Prieto-Merino D, et al. Systemic immunomodulatory treatments for atopic dermatitis: update of a living systematic review and network meta-analysis. JAMA Dermatol. 2022;158(5):523–32. https://doi.org/10.1001/jamadermatol.2022.0455.
Drucker AM, Lam M, Elsawi R, et al. Comparing binary efficacy outcomes for systemic immunomodulatory treatments for atopic dermatitis in a living systematic review and network meta-analysis. Br J Dermatol. 2023. https://doi.org/10.1093/bjd/ljad393.
Chovatiya R, Silverberg JI. DESCRIBE-AD: a novel classification framework for atopic dermatitis. J Am Acad Dermatol. 2022;87(3):541–50. https://doi.org/10.1016/j.jaad.2021.10.058.
Gargiulo L, Ibba L, Pavia G, et al. Upadacitinib for the treatment of concomitant psoriasis and atopic dermatitis: a case series. J Dermatolog Treat. 2023;34(1):2183729. https://doi.org/10.1080/09546634.2023.2183729.
Nilsson M, Berggren K, Berglund S, et al. Discovery of the potent and selective inhaled janus kinase 1 inhibitor AZD4604 and its preclinical characterization. J Med Chem. 2023;66(19):13400–15. https://doi.org/10.1021/acs.jmedchem.3c00554.
Gargiulo L, Ibba L, Piscazzi F, et al. Upadacitinib improves symptoms of concomitant allergic rhinitis or allergic asthma in patients with severe atopic dermatitis: a 16-week multicentre retrospective study. J Eur Acad Dermatol Venereol. 2024. https://doi.org/10.1111/jdv.19862.
Reguiai Z, Becherel PA, Fougerousse AC, et al. Janus kinase inhibitors for the treatment of atopic dermatitis: real-life data on efficacy and safety in light of the pharmacovigilance risk assessment committee recommended measures. J Eur Acad Dermatol Venereol. 2023;37(11):e1307–9. https://doi.org/10.1111/jdv.19302.
De Greef A, Ghislain PD, de Montjoye L, Baeck M. Real-life effectiveness and tolerance of upadacitinib for severe atopic dermatitis in adolescents and adults. Adv Ther. 2023;40(5):2509–14. https://doi.org/10.1007/s12325-023-02490-5.
Melgosa Ramos FJ, González-Delgado V, Motilla JMS, Marta GP, Mateu Puchades A, Sergio SA. Upadacitinib effectiveness in moderate-to-severe atopic dermatitis: a real-life multicentre and retrospective study. Australas J Dermatol. 2023;64(4):e361–4. https://doi.org/10.1111/ajd.14164.
Bieber T, Katoh N, Simpson EL, et al. Safety of baricitinib for the treatment of atopic dermatitis over a median of 1.6 years and up to 3.9 years of treatment: an updated integrated analysis of eight clinical trials. J Dermatol Treat. 2023;34:2161812.
Gargiulo L, Ibba L, Fiorillo G, et al. Pregnancy outcome of a patient treated with upadacitinib for severe atopic dermatitis. J Eur Acad Dermatol Venereol. 2023. https://doi.org/10.1111/jdv.19557.
Mohamed MF, Trueman S, Feng T, Friedman A, Othman AA. The JAK1 inhibitor upadacitinib has no effect on the pharmacokinetics of levonorgestrel and ethinylestradiol: a study in healthy female subjects. J Clin Pharmacol. 2019;59(4):510–6. https://doi.org/10.1002/jcph.1350.
Wollenberg A, Thyssen JP, Bieber T, Chan G, Kerkmann U. A detailed look at the European Medicines Agency’s recommendations for use of Janus kinase inhibitors in patients with atopic dermatitis. J Eur Acad Dermatol Venereol. 2023;37(10):2041–6. https://doi.org/10.1111/jdv.19255.
Piscazzi F, Gargiulo L, Ibba L, et al. Upadacitinib for the treatment of atopic dermatitis in the elderly: an Italian case series of seven patients. J Dermatol Treat. 2023;34(1):2245510. https://doi.org/10.1080/09546634.2023.2245510.
Goodman SM, Springer B, Guyatt G, et al. 2017 American College of Rheumatology/American Association of Hip and Knee surgeons guideline for the perioperative management of antirheumatic medication in patients with rheumatic diseases undergoing elective total hip or total knee arthroplasty. Arthritis Care Res (Hoboken). 2017;69(8):1111–24. https://doi.org/10.1002/acr.23274.
Curtis JR, Johnson SR, Anthony DD, et al. American College of Rheumatology Guidance for COVID-19 vaccination in patients with rheumatic and musculoskeletal diseases: version 1. Arthritis Rheumatol. 2021;73(7):1093–107. https://doi.org/10.1002/art.41734.
Acknowledgements
This work was partially supported by “Ricerca Corrente” funding from Italian Ministry of Health to IRCCS Humanitas Research Hospital.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Conceptualization: Antonio Costanzo and Alessandra Narcisi. Methodology: Luigi Gargiulo and Luciano Ibba. Validation: Antonio Costanzo and Alessandra Narcisi. Formal analysis: Luigi Gargiulo and Luciano Ibba. Investigation: Luigi Gargiulo and Luciano Ibba. Data curation: Luigi Gargiulo and Luciano Ibba. Writing original draft: Luigi Gargiulo. Writing/reviewing and editing: Luigi Gargiulo, Luciano Ibba, Piergiorgio Malagoli, Anna G. Burroni, Andrea Chiricozzi, Paolo Dapavo, Silvia M. Ferrucci, Massimo Gola, Maddalena Napolitano, Michela Ortoncelli, Maria T. Rossi, Claudio Sciarrone, Antonio Costanzo, Alessandra Narcisi. Visualization: Luigi Gargiulo. Supervision: Alessandra Narcisi. Project administration: Antonio Costanzo and Alessandra Narcisi. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
Luigi Gargiulo has been a consultant for Almirall. Luciano Ibba has been a consultant for Almirall. Piergiorgio Malagoli has been a speaker for AbbVie, Lilly, Novartis, Janssen-Cilag, Celgene, Leopharma, and Almirall. Andrea Chiricozzi has served as advisory board member and consultant and has received fees and speaker’s honoraria or has participated in clinical trials for AbbVie, Almirall, Bristol Myers Squibb, Leo Pharma, Lilly, Janssen, Novartis, Pfzer and Sanof Genzyme. Paolo Dapavo has been a speaker for Novartis, Abbvie, Sanofi, UCB, Janssen, Lilly, and LeoPharma. Silvia M. Ferrucci has been principal investigator in clinical trials for ABBVIE, Almirall, Galderma, Leo Pharma, Sanofi, Amgen, Novartis, Bayer and received honoraria for lectures for Novartis and Menarini. Maddalena Napolitano acted as speaker, consultant and/or advisory board member for Abbvie, Eli Lilly, Leo Pharma, Novartis, and Sanofi. Michela Ortoncelli has served as a consultant and/or speaker for AbbVie, LEO Pharma, Novartis and Sanofi. Maria T. Rossi has received personal fee for advisory board meeting from Sanofi, Abbvie, Novartis, and Cantabria. Antonio Costanzo has served as an advisory board member, consultant and has received fees and speaker’s honoraria or has participated in clinical trials for Abbvie, Almirall, Biogen, LEO Pharma, Lilly, Janssen, Novartis, Pfizer, Sanofi Genzyme, and UCB-Pharma. Alessandra Narcisi has served on advisory boards, received honoraria for lectures and research grants from Almirall, Abbvie, Leo Pharma, Celgene, Eli Lilly, Janssen, Novartis, Sanofi-Genzyme, Amgen and Boehringer Ingelheim. Anna G. Burroni, Massimo Gola and Claudio Sciarrone have nothing to declare.
Ethical Approval
Institutional review board approval was exempted for this study as its procedures did not include human subjects and did not deviate from good clinical practice. All the involved dermatologists gave their approval for the study to be published. All the dermatologists who were part of the consensus were involved in the writing and/or revision of the manuscript. All the dermatologists who participated in the consensus were aware of the objective of the study, and they all knew that the manuscript will be published. The participants gave written informed consent.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gargiulo, L., Ibba, L., Malagoli, P. et al. Management of Patients Affected by Moderate-to-Severe Atopic Dermatitis with JAK Inhibitors in Real-World Clinical Practice: An Italian Delphi Consensus. Dermatol Ther (Heidelb) 14, 919–932 (2024). https://doi.org/10.1007/s13555-024-01135-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13555-024-01135-x