Abstract
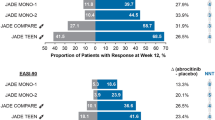
Therapeutic options for people with moderate or severe atopic dermatitis refractory to topical therapy have rapidly expanded in recent years. These new targeted immunomodulatory agents—biologics and Janus kinase (JAK) inhibitors—have each demonstrated high levels of efficacy and acceptable safety in mostly placebo-controlled clinical trials for atopic dermatitis, but there is no universally applicable algorithm to help choose between them for a given patient. Hence, patients and physicians should utilize shared decision making, discussing efficacy, safety, mode of delivery, monitoring, costs, speed of onset, and other factors to reach individualized treatment decisions. In this review, we try to aid shared decision making by summarizing the efficacy, safety, and monitoring of biologics and oral JAK inhibitors for adults with atopic dermatitis. Network meta-analyses suggest that higher doses of abrocitinib and upadacitinib are more effective than biologics. They also show that, among biologics, dupilumab is likely more effective than tralokinumab and lebrikizumab. Biologics are generally considered safer than JAK inhibitors, although concerns about JAK inhibitors are mainly extrapolated from older generation JAK inhibitors used in higher-risk populations. We also outline evidence and considerations for choosing and using systemic immunomodulatory treatments for special populations including pregnant individuals, those with human immunodeficiency virus (HIV), hepatitis B and C, end stage kidney disease, and older adults.
Similar content being viewed by others
References
Guttman-Yassky E, Waldman A, Ahluwalia J, Ong PY, Eichenfield LF. Atopic dermatitis: pathogenesis. Semin Cutan Med Surg. 2017;36:100–3.
Chiesa Fuxench ZC, Block JK, Boguniewicz M, Boyle J, Fonacier L, Gelfand JM, et al. Atopic dermatitis in america study: a cross-sectional study examining the prevalence and disease burden of atopic dermatitis in the us adult population. J Investig Dermatol. 2019;139:583–90.
Kim DH, Li K, Seo SJ, Jo SJ, Yim HW, Kim CM, et al. Quality of life and disease severity are correlated in patients with atopic dermatitis. J Korean Med Sci. 2012;27:1327–32.
Simpson EL, Bruin-Weller M, Flohr C, Ardern-Jones MR, Barbarot S, Deleuran M, et al. When does atopic dermatitis warrant systemic therapy? Recommendations from an expert panel of the International Eczema Council. J Am Acad Dermatol. 2017;77:623–33.
Musters AH, Mashayekhi S, Harvey J, Axon E, Lax SJ, Flohr C, et al. Phototherapy for atopic eczema. Cochrane Database Syst Rev. 2021;10:CD013870.
Moyle M, Cevikbas F, Harden JL, Guttman-Yassky E. Understanding the immune landscape in atopic dermatitis: the era of biologics and emerging therapeutic approaches. Exp Dermatol. 2019;28:756–68.
Drucker AM, Ellis AG, Bohdanowicz M, Mashayekhi S, Yiu ZZN, Rochwerg B, et al. Systemic immunomodulatory treatments for patients with atopic dermatitis: a systematic review and network meta-analysis. JAMA Dermatol. 2020;156:659–67.
Chan SC, Li SH, Hanifin JM. Increased interleukin-4 production by atopic mononuclear leukocytes correlates with increased cyclic adenosine monophosphate-phosphodiesterase activity and is reversible by phosphodiesterase inhibition. J Investig Dermatol. 1993;100:681–4.
Hamid Q, Naseer T, Minshall EM, Song YL, Boguniewicz M, Leung DY. In vivo expression of IL-12 and IL-13 in atopic dermatitis. J Allergy Clin Immunol. 1996;98:225–31.
Augustin M, Langenbruch A, Blome C, Gutknecht M, Werfel T, Ständer S, et al. Characterizing treatment-related patient needs in atopic eczema: insights for personalized goal orientation. J Eur Acad Dermatol Venereol. 2020;34:142–52.
Boeri M, Sutphin J, Hauber B, Cappelleri JC, Romero W, Di Bonaventura M. Quantifying patient preferences for systemic atopic dermatitis treatments using a discrete-choice experiment. J Dermatol Treat. 2022;33:1449–58.
Thomas C, Raibouaa A, Wollenberg A, Capron J-P, Krucien N, Karn H, et al. Patient preferences for atopic dermatitis medications in the UK, France and Spain: a discrete choice experiment. BMJ Open. 2022;12: e058799.
Abuabara K, Magyari A, McCulloch CE, Linos E, Margolis DJ, Langan SM. Prevalence of atopic eczema among patients seen in primary care: data from the health improvement network. Ann Intern Med. 2019;170:354–6.
Abuabara K, Langan SM. Atopic dermatitis across the life course. Br J Dermatol. 2023;188:709–17.
Lam M, Zhu JW, Maqbool T, Adam G, Tadrous M, Rochon P, et al. Inclusion of older adults in randomized clinical trials for systemic medications for atopic dermatitis: a systematic review. JAMA Dermatol. 2020;156:1240–5.
Drucker AM, Lam M, Flohr C, Thyssen JP, Kabashima K, Bissonnette R, et al. Systemic therapy for atopic dermatitis in older adults and adults with comorbidities: a scoping review and International Eczema Council Survey. Dermatitis. 2022;33:200–6.
Eichenfield LF, DiBonaventura M, Xenakis J, Lafeuille M-H, Duh MS, Fakih I, et al. Costs and treatment patterns among patients with atopic dermatitis using advanced therapies in the United States: analysis of a retrospective claims database. Dermatol Ther. 2020;10:791–806.
Joensuu JT, Aaltonen KJ, Aronen P, Sokka T, Puolakka K, Tuompo R, et al. Cost-effectiveness of biologic compared with conventional synthetic disease-modifying anti-rheumatic drugs in patients with rheumatoid arthritis: a Register study. Rheumatol Oxf Engl. 2016;55:1803–11.
Pharmacoeconomic Report: Dupilumab (Dupixent): (Sanofi Genzyme, a division of sanofi-aventis Canada Inc.): Indication: Indicated for the treatment of patients aged 12 years and older with moderate-to-severe atopic dermatitis whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable [Internet]. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health; 2020 [cited 2023 Dec 24]. Available from:http://www.ncbi.nlm.nih.gov/books/NBK566135/
Boguniewicz M, Fonacier L, Guttman-Yassky E, Ong PY, Silverberg J, Farrar JR. Atopic dermatitis yardstick: practical recommendations for an evolving therapeutic landscape. Ann Allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol. 2018;120:10-22.e2.
Wang C, Kraus CN, Patel KG, Ganesan AK, Grando SA. Real-world experience of dupilumab treatment for atopic dermatitis in adults: a retrospective analysis of patients’ records. Int J Dermatol. 2020;59:253–6.
Harb H, Chatila TA. Mechanisms of dupilumab. Clin Exp Allergy J Br Soc Allergy Clin Immunol. 2020;50:5–14.
Simpson EL, Bieber T, Guttman-Yassky E, Beck LA, Blauvelt A, Cork MJ, et al. Two phase 3 trials of dupilumab versus placebo in atopic dermatitis. N Engl J Med. 2016;375:2335–48.
Zhao Y, Wu L, Lu Q, Gao X, Zhu X, Yao X, et al. The efficacy and safety of dupilumab in Chinese patients with moderate-to-severe atopic dermatitis: a randomized, double-blind, placebo-controlled study. Br J Dermatol. 2022;186:633–41.
de Bruin-Weller M, Thaçi D, Smith CH, Reich K, Cork MJ, Radin A, et al. Dupilumab with concomitant topical corticosteroid treatment in adults with atopic dermatitis with an inadequate response or intolerance to ciclosporin A or when this treatment is medically inadvisable: a placebo-controlled, randomized phase III clinical trial (LIBERTY AD CAFÉ). Br J Dermatol. 2018;178:1083–101.
Blauvelt A, de Bruin-Weller M, Gooderham M, Cather JC, Weisman J, Pariser D, et al. Long-term management of moderate-to-severe atopic dermatitis with dupilumab and concomitant topical corticosteroids (LIBERTY AD CHRONOS): a 1-year, randomised, double-blinded, placebo-controlled, phase 3 trial. Lancet Lond Engl. 2017;389:2287–303.
Deleuran M, Thaçi D, Beck LA, de Bruin-Weller M, Blauvelt A, Forman S, et al. Dupilumab shows long-term safety and efficacy in patients with moderate to severe atopic dermatitis enrolled in a phase 3 open-label extension study. J Am Acad Dermatol. 2020;82:377–88.
Achten R, Bakker D, Ariens L, Lans A, Thijs J, van der Schaft J, et al. Long-term follow-up and treatment outcomes of conjunctivitis during dupilumab treatment in patients with moderate-to-severe atopic dermatitis. J Allergy Clin Immunol Pract. 2021;9:1389-1392.e2.
Agnihotri G, Shi K, Lio PA. A clinician’s guide to the recognition and management of dupilumab-associated conjunctivitis. Drugs RD. 2019;19:311–8.
Faiz S, Giovannelli J, Podevin C, Jachiet M, Bouaziz J-D, Reguiai Z, et al. Effectiveness and safety of dupilumab for the treatment of atopic dermatitis in a real-life French multicenter adult cohort. J Am Acad Dermatol. 2019;81:143–51.
Jang DH, Lee JI, Bae JY, Jung HJ, Park MY, Ahn J. Facial erythema after the treatment of dupilumab in SLE patient. Allergy Asthma Clin Immunol Off J Can Soc Allergy Clin Immunol. 2020;16:60.
Jay R, Rodger J, Zirwas M. Review of dupilumab-associated inflammatory arthritis: an approach to clinical analysis and management. JAAD Case Rep. 2022;21:14–8.
Bettuzzi T, Drucker A, Staumont-Sallé D, Bihan K, Lebrun-Vignes B, Sbidian E. Adverse events associated with dupilumab in the World Health Organization pharmacovigilance database. J Am Acad Dermatol. 2022;86:431–3.
Soria A, Du-Thanh A, Seneschal J, Jachiet M, Staumont-Sallé D, Barbarot S, et al. Development or exacerbation of head and neck dermatitis in patients treated for atopic dermatitis with dupilumab. JAMA Dermatol. 2019;155:1312–5.
Bridgewood C, Sharif K, Freeston J, Saleem B, Russell T, Watad A, et al. Regulation of entheseal IL-23 expression by IL-4 and IL-13 as an explanation for arthropathy development under dupilumab therapy. Rheumatol Oxf Engl. 2021;60:2461–6.
Rajka G, Winkelmann RK. Atopic dermatitis and Sézary syndrome. Arch Dermatol. 1984;120:83–4.
Van Haselen CW, Toonstra J, Preesman AH, Van Der Putte SC, Bruijnzeel-Koomen CA, Van Vloten WA. Sézary syndrome in a young man with severe atopic dermatitis. Br J Dermatol. 1999;140:704–7.
Park A, Wong L, Lang A, Kraus C, Anderson N, Elsensohn A. Cutaneous T-cell lymphoma following dupilumab use: a systematic review. Int J Dermatol. 2023;62:862–76.
Kozera E, Stewart T, Gill K, De La Vega MA, Frew JW. Dupilumab-associated head and neck dermatitis is associated with elevated pretreatment serum Malassezia-specific IgE: a multicentre, prospective cohort study. Br J Dermatol. 2022;186:1050–2.
Bax CE, Khurana MC, Treat JR, Castelo-Soccio L, Rubin AI, McMahon PJ. New-onset head and neck dermatitis in adolescent patients after dupilumab therapy for atopic dermatitis. Pediatr Dermatol. 2021;38:390–4.
Jo CE, Finstad A, Georgakopoulos JR, Piguet V, Yeung J, Drucker AM. Facial and neck erythema associated with dupilumab treatment: a systematic review. J Am Acad Dermatol. 2021;84:1339–47.
Su Z, Zeng Y-P. Dupilumab-associated psoriasis and psoriasiform manifestations: a scoping review. Dermatol Basel Switz. 2023;239:646–57.
Murphy MJ, Cohen JM, Vesely MD, Damsky W. Paradoxical eruptions to targeted therapies in dermatology: a systematic review and analysis. J Am Acad Dermatol. 2022;86:1080–91.
Kreeshan FC, Al-Janabi A, Warren RB, Hunter HJA. Real-world experience and laboratory monitoring of dupilumab in patients with moderate to severe atopic dermatitis in a tertiary centre. Dermatol Ther. 2021;11:149–60.
Din ATU, Malik I, Arshad D, Din ATU. Dupilumab for atopic dermatitis: the silver bullet we have been searching for? Cureus. 2020;12:e7565.
Popovic B, Breed J, Rees DG, Gardener MJ, Vinall LMK, Kemp B, et al. Structural characterisation reveals mechanism of IL-13-neutralising monoclonal antibody tralokinumab as inhibition of binding to IL-13Rα1 and IL-13Rα2. J Mol Biol. 2017;429:208–19.
Bieber T. Interleukin-13: targeting an underestimated cytokine in atopic dermatitis. Allergy. 2020;75:54–62.
Wollenberg A, Blauvelt A, Guttman-Yassky E, Worm M, Lynde C, Lacour J-P, et al. Tralokinumab for moderate-to-severe atopic dermatitis: results from two 52-week, randomized, double-blind, multicentre, placebo-controlled phase III trials (ECZTRA 1 and ECZTRA 2). Br J Dermatol. 2021;184:437–49.
Silverberg JI, Toth D, Bieber T, Alexis AF, Elewski BE, Pink AE, et al. Tralokinumab plus topical corticosteroids for the treatment of moderate-to-severe atopic dermatitis: results from the double-blind, randomized, multicentre, placebo-controlled phase III ECZTRA 3 trial. Br J Dermatol. 2021;184:450–63.
Gutermuth J, Pink AE, Worm M, Soldbro L, Bjerregård Øland C, Weidinger S. Tralokinumab plus topical corticosteroids in adults with severe atopic dermatitis and inadequate response to or intolerance of ciclosporin A: a placebo-controlled, randomized, phase III clinical trial (ECZTRA 7). Br J Dermatol. 2022;186:440–52.
Simpson EL, Merola JF, Silverberg JI, Reich K, Warren RB, Staumont-Sallé D, et al. Safety of tralokinumab in adult patients with moderate-to-severe atopic dermatitis: pooled analysis of five randomized, double-blind, placebo-controlled phase II and phase III trials. Br J Dermatol. 2022;187:888–99.
Blauvelt A, Thyssen JP, Guttman-Yassky E, Bieber T, Serra-Baldrich E, Simpson E, et al. Efficacy and safety of lebrikizumab in moderate-to-severe atopic dermatitis: 52-week results of two randomized double-blinded placebo-controlled phase III trials. Br J Dermatol. 2023;188:740–8.
Simpson EL, Gooderham M, Wollenberg A, Weidinger S, Armstrong A, Soung J, et al. Efficacy and safety of lebrikizumab in combination with topical corticosteroids in adolescents and adults with moderate-to-severe atopic dermatitis: a randomized clinical trial (ADhere). JAMA Dermatol. 2023;159:182–91.
Corren J, Lemanske RF, Hanania NA, Korenblat PE, Parsey MV, Arron JR, et al. Lebrikizumab treatment in adults with asthma. N Engl J Med. 2011;365:1088–98.
Hanania NA, Korenblat P, Chapman KR, Bateman ED, Kopecky P, Paggiaro P, et al. Efficacy and safety of lebrikizumab in patients with uncontrolled asthma (LAVOLTA I and LAVOLTA II): replicate, phase 3, randomised, double-blind, placebo-controlled trials. Lancet Respir Med. 2016;4:781–96.
Cornelissen C, Lüscher-Firzlaff J, Baron JM, Lüscher B. Signaling by IL-31 and functional consequences. Eur J Cell Biol. 2012;91:552–66.
Ruzicka T, Hanifin JM, Furue M, Pulka G, Mlynarczyk I, Wollenberg A, et al. Anti-interleukin-31 receptor A antibody for atopic dermatitis. N Engl J Med. 2017;376:826–35.
Kabashima K, Matsumura T, Komazaki H, Kawashima M, Nemolizumab-JP01 Study Group. Trial of nemolizumab and topical agents for atopic dermatitis with pruritus. N Engl J Med. 2020;383:141–50.
Liang J, Hu F, Dan M, Sang Y, Abulikemu K, Wang Q, et al. Safety and efficacy of nemolizumab for atopic dermatitis with pruritus: a systematic review and meta-regression analysis of randomized controlled trials. Front Immunol. 2022;13: 825312.
Patterson H, Nibbs R, McInnes I, Siebert S. Protein kinase inhibitors in the treatment of inflammatory and autoimmune diseases. Clin Exp Immunol. 2014;176:1–10.
Furumoto Y, Gadina M. The arrival of JAK inhibitors: advancing the treatment of immune and hematologic disorders. BioDrugs Clin Immunother Biopharm Gene Ther. 2013;27:431–8.
Zhao M-Y, Zhang W, Rao G-W. Targeting Janus kinase (JAK) for fighting diseases: the research of JAK inhibitor drugs. Curr Med Chem. 2022;29:5010–40.
McLornan DP, Pope JE, Gotlib J, Harrison CN. Current and future status of JAK inhibitors. Lancet Lond Engl. 2021;398:803–16.
Cinats A, Heck E, Robertson L. Janus kinase inhibitors: a review of their emerging applications in dermatology. Skin Ther Lett. 2018;23:5–9.
Lin CM, Cooles FA, Isaacs JD. Basic mechanisms of JAK inhibition. Mediterr J Rheumatol. 2020;31:100–4.
O’Shea JJ, Plenge R. JAK and STAT signaling molecules in immunoregulation and immune-mediated disease. Immunity. 2012;36:542–50.
Ferreira S, Guttman-Yassky E, Torres T. Selective JAK1 inhibitors for the treatment of atopic dermatitis: focus on upadacitinib and abrocitinib. Am J Clin Dermatol. 2020;21:783–98.
Silverberg JI, Simpson EL, Thyssen JP, Gooderham M, Chan G, Feeney C, et al. Efficacy and safety of abrocitinib in patients with moderate-to-severe atopic dermatitis: a randomized clinical trial. JAMA Dermatol. 2020;156:863–73.
Blauvelt A, Silverberg JI, Lynde CW, Bieber T, Eisman S, Zdybski J, et al. Abrocitinib induction, randomized withdrawal, and retreatment in patients with moderate-to-severe atopic dermatitis: results from the JAK1 Atopic Dermatitis Efficacy and Safety (JADE) REGIMEN phase 3 trial. J Am Acad Dermatol. 2022;86:104–12.
Shi VY, Bhutani T, Fonacier L, Deleuran M, Shumack S, Valdez H, et al. Phase 3 efficacy and safety of abrocitinib in adults with moderate-to-severe atopic dermatitis after switching from dupilumab (JADE EXTEND). J Am Acad Dermatol. 2022;87:351–8.
Simpson EL, Silverberg JI, Nosbaum A, Winthrop KL, Guttman-Yassky E, Hoffmeister KM, et al. Integrated safety analysis of abrocitinib for the treatment of moderate-to-severe atopic dermatitis from the phase II and phase III clinical trial program. Am J Clin Dermatol. 2021;22:693–707.
Kotyla PJ, Islam MA, Engelmann M. Clinical Aspects of Janus kinase (JAK) inhibitors in the cardiovascular system in patients with rheumatoid arthritis. Int J Mol Sci. 2020;21:7390.
Guttman-Yassky E, Teixeira HD, Simpson EL, Papp KA, Pangan AL, Blauvelt A, et al. Once-daily upadacitinib versus placebo in adolescents and adults with moderate-to-severe atopic dermatitis (Measure Up 1 and Measure Up 2): results from two replicate double-blind, randomised controlled phase 3 trials. Lancet Lond Engl. 2021;397:2151–68.
Reich K, Teixeira HD, de Bruin-Weller M, Bieber T, Soong W, Kabashima K, et al. Safety and efficacy of upadacitinib in combination with topical corticosteroids in adolescents and adults with moderate-to-severe atopic dermatitis (AD Up): results from a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Lond Engl. 2021;397:2169–81.
Guttman-Yassky E, Thyssen JP, Silverberg JI, Papp KA, Paller AS, Weidinger S, et al. Safety of upadacitinib in moderate-to-severe atopic dermatitis: an integrated analysis of phase 3 studies. J Allergy Clin Immunol. 2023;151:172–81.
Kubo S, Nakayamada S, Sakata K, Kitanaga Y, Ma X, Lee S, et al. Janus kinase inhibitor baricitinib modulates human innate and adaptive immune system. Front Immunol. 2018;9:1510.
He H, Guttman-Yassky E. JAK Inhibitors for atopic dermatitis: an update. Am J Clin Dermatol. 2019;20:181–92.
Simpson EL, Lacour J-P, Spelman L, Galimberti R, Eichenfield LF, Bissonnette R, et al. Baricitinib in patients with moderate-to-severe atopic dermatitis and inadequate response to topical corticosteroids: results from two randomized monotherapy phase III trials. Br J Dermatol. 2020;183:242–55.
Silverberg JI, Simpson EL, Wollenberg A, Bissonnette R, Kabashima K, DeLozier AM, et al. Long-term efficacy of baricitinib in adults with moderate to severe atopic dermatitis who were treatment responders or partial responders: an extension study of 2 randomized clinical trials. JAMA Dermatol. 2021;157:691–9.
Bieber T, Reich K, Paul C, Tsunemi Y, Augustin M, Lacour J-P, et al. Efficacy and safety of baricitinib in combination with topical corticosteroids in patients with moderate-to-severe atopic dermatitis with inadequate response, intolerance or contraindication to ciclosporin: results from a randomized, placebo-controlled, phase III clinical trial (BREEZE-AD4). Br J Dermatol. 2022;187:338–52.
Wollenberg A, Nakahara T, Maari C, Peris K, Lio P, Augustin M, et al. Impact of baricitinib in combination with topical steroids on atopic dermatitis symptoms, quality of life and functioning in adult patients with moderate-to-severe atopic dermatitis from the BREEZE-AD7 Phase 3 randomized trial. J Eur Acad Dermatol Venereol. 2021;35:1543–52.
Simpson EL, Forman S, Silverberg JI, Zirwas M, Maverakis E, Han G, et al. Baricitinib in patients with moderate-to-severe atopic dermatitis: results from a randomized monotherapy phase 3 trial in the United States and Canada (BREEZE-AD5). J Am Acad Dermatol. 2021;85:62–70.
Bieber T, Katoh N, Simpson EL, de Bruin-Weller M, Thaçi D, Torrelo A, et al. Safety of baricitinib for the treatment of atopic dermatitis over a median of 1.6 years and up to 3.9 years of treatment: an updated integrated analysis of eight clinical trials. J Dermatol Treat. 2023;34:2161812.
Iznardo H, Roé E, Serra-Baldrich E, Puig L. Efficacy and safety of JAK1 inhibitor abrocitinib in atopic dermatitis. Pharmaceutics. 2023;15:385.
Sandborn WJ, Feagan BG, Loftus EV, Peyrin-Biroulet L, Van Assche G, D’Haens G, et al. Efficacy and safety of upadacitinib in a randomized trial of patients with Crohn’s disease. Gastroenterology. 2020;158:2123-2138.e8.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Baricitinib. [Updated 2022 Aug 30]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK548012/
Winthrop KL, Harigai M, Genovese MC, Lindsey S, Takeuchi T, Fleischmann R, et al. Infections in baricitinib clinical trials for patients with active rheumatoid arthritis. Ann Rheum Dis. 2020;79:1290–7.
Ytterberg SR, Bhatt DL, Mikuls TR, Koch GG, Fleischmann R, Rivas JL, et al. Cardiovascular and cancer risk with tofacitinib in rheumatoid arthritis. N Engl J Med. 2022;386:316–26.
Polverelli N, Elli EM, Abruzzese E, Palumbo GA, Benevolo G, Tiribelli M, et al. Second primary malignancy in myelofibrosis patients treated with ruxolitinib. Br J Haematol. 2021;193:356–68.
Chen T-L, Lee L-L, Huang H-K, Chen L-Y, Loh C-H, Chi C-C. Association of risk of incident venous thromboembolism with atopic dermatitis and treatment with Janus kinase inhibitors: a systematic review and meta-analysis. JAMA Dermatol. 2022;158:1254–61.
Bieber T, Simpson EL, Silverberg JI, Thaçi D, Paul C, Pink AE, et al. Abrocitinib versus placebo or dupilumab for atopic dermatitis. N Engl J Med. 2021;384:1101–12.
Reich K, Thyssen JP, Blauvelt A, Eyerich K, Soong W, Rice ZP, et al. Efficacy and safety of abrocitinib versus dupilumab in adults with moderate-to-severe atopic dermatitis: a randomised, double-blind, multicentre phase 3 trial. Lancet Lond Engl. 2022;400:273–82.
Blauvelt A, Teixeira HD, Simpson EL, Costanzo A, De Bruin-Weller M, Barbarot S, et al. Efficacy and safety of upadacitinib vs dupilumab in adults with moderate-to-severe atopic dermatitis: a randomized clinical trial. JAMA Dermatol. 2021;157:1047–55.
Watt J, Tricco AC, Straus S, Veroniki AA, Naglie G, Drucker AM. Research techniques made simple: network meta-analysis. J Investig Dermatol. 2019;139:4-12.e1.
Drucker AM, Morra DE, Prieto-Merino D, Ellis AG, Yiu ZZN, Rochwerg B, et al. Systemic immunomodulatory treatments for atopic dermatitis. JAMA Dermatol. 2022;158:523–32.
Gao Q, Zhao Y, Zhang J. Efficacy and safety of abrocitinib and upadacitinib versus dupilumab in adults with moderate-to-severe atopic dermatitis: a systematic review and meta-analysis. Heliyon. 2023;9: e16704.
Silverberg JI, Thyssen JP, Fahrbach K, Mickle K, Cappelleri JC, Romero W, et al. Comparative efficacy and safety of systemic therapies used in moderate-to-severe atopic dermatitis: a systematic literature review and network meta-analysis. J Eur Acad Dermatol Venereol. 2021;35:1797–810.
Drucker AM. Comparing binary efficacy outcomes for systemic immunomodulatory treatments for atopic dermatitis in a living systematic review and network meta-analysis. Unpublished manuscript.
Chu AWL, Wong MM, Rayner DG, Guyatt GH, Martinez JPD, Ceccacci R, et al. Systemic treatments for atopic dermatitis (eczema): systematic review and network meta-analysis of randomized trials. J Allergy Clin Immunol. 2023;152:1470–92.
Pfaller B, José Yepes-Nuñez J, Agache I, Akdis CA, Alsalamah M, Bavbek S, et al. Biologicals in atopic disease in pregnancy: an EAACI position paper. Allergy. 2021;76:71–89.
Shakuntulla F, Chiarella SE. Safety of biologics for atopic diseases during pregnancy. J Allergy Clin Immunol Pract. 2022;10:3149–55.
Lobo Y, Lee RC, Spelman L. Atopic dermatitis treated safely with dupilumab during pregnancy: a case report and review of the literature. Case Rep Dermatol. 2021;13:248–56.
Kage P, Simon JC, Treudler R. A case of atopic eczema treated safely with dupilumab during pregnancy and lactation. J Eur Acad Dermatol Venereol. 2020;34:e256–7.
Kage P, Simon J-C, Treudler R. Case of atopic eczema treated with dupilumab throughout conception, pregnancy, and lactation. J Dermatol. 2021;48:E484–5.
Patruno C, Potestio L, Scalvenzi M, Battista T, Raia F, Picone V, et al. Dupilumab for the treatment of adult atopic dermatitis in special populations. J Dermatol Treat. 2022;33:3028–33.
Gracia-Darder I, Pons De Ves J, Reyero Cortina M, Martín-Santiago A. Patient with atopic dermatitis, hyper IgE syndrome and ulcerative colitis, treated successfully with dupilumab during pregnancy. Dermatol Ther. 2022;35:e15237.
Costley M, Murphy B. Severe atopic dermatitis treated successfully with dupilumab throughout pregnancy. Clin Exp Dermatol. 2022;47:960–1.
Akhtar NH, Khosravi-Hafshejani T, Akhtar D, Dhadwal G, Kanani A. The use of dupilumab in severe atopic dermatitis during pregnancy: a case report. Allergy Asthma Clin Immunol Off J Can Soc Allergy Clin Immunol. 2022;18:9.
Riquelme-Mc Loughlin C, Mascaró JM. Treatment of pemphigoid gestationis with dupilumab. Clin Exp Dermatol. 2021;46:1578–9.
Post-authorization Safety Study in North America to Monitor Pregnancy and Infant Outcomes Following Administration of Dupilumab During Planned or Unexpected Pregnancy—Full Text View—ClinicalTrials.gov [Internet]. [cited 2023 Jul 15]. https://clinicaltrials.gov/ct2/show/NCT04173442
An Observational Retrospective Cohort Study Being Conducted in Women With Atopic Dermatitis (AD)—Full Text View—ClinicalTrials.gov [Internet]. [cited 2023 Jul 15]. https://clinicaltrials.gov/ct2/show/NCT03936335
Dupilumab. Drugs Lact Database Lact [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006 [cited 2023 Sep 23]. http://www.ncbi.nlm.nih.gov/books/NBK500904/
Gisbert JP, Chaparro M. Safety of new biologics (vedolizumab and ustekinumab) and small molecules (tofacitinib) during pregnancy: a review. Drugs. 2020;80:1085–100.
Napolitano M, Caiazzo G, Fabbrocini G, Balato A, Di Caprio R, Scala E, et al. Increased expression of interleukin-23A in lesional skin of patients with atopic dermatitis with psoriasiform reaction during dupilumab treatment. Br J Dermatol. 2021;184:341–3.
Napolitano M, Ruggiero A, Fontanella G, Fabbrocini G, Patruno C. New emergent therapies for atopic dermatitis: a review of safety profile with respect to female fertility, pregnancy, and breastfeeding. Dermatol Ther. 2021;34: e14475.
Pfizer. CIBINQOTM Pregnancy Registry: an observational study of the safety of abrocitinib exposure in pregnant women and their offspring [Internet]. clinicaltrials.gov; 2023 May. Report No.: NCT05721937. https://clinicaltrials.gov/study/NCT05721937
Avallone G, Trunfio M, Giura MT, Siliquini N, Viola R, Orofino G, et al. Dupilumab in HIV-positive patients with atopic dermatitis: a long-term follow-up patient and a literature review. Dermatol Online J. 2021;27.
Nusbaum KB, Kaffenberger BH, Paradiso Bs MM, Sopkovich JA, Daou H, Seminario-Vidal L, et al. Dupilumab for treatment of atopic dermatitis in patients living with HIV: a case series. Int J Dermatol. 2021;60:e344–6.
Ordóñez-Rubiano MF, Rubiano-Mojica PC, Casas M. Young HIV-positive male patient with severe atopic dermatitis on dupilumab and SARS-CoV-2 infection, a pioneer hypothesis. Int J Dermatol. 2021;60:514–5.
Olbricht N, Kromer C, Forkel S, Schön MP, Buhl T. Effective treatment of atopic dermatitis with dupilumab in an HIV-positive patient. J Dtsch Dermatol Ges J Ger Soc Dermatol. 2020;18:1488–90.
Lor M, Villa N, Holland V. Safe and effective treatment of atopic dermatitis using dupilumab over 23 months in a patient with HIV. Dermatol Ther. 2020;33: e14271.
Brodska P, Panzner P, Sedlacek D, Terl M, Cetkovska P. Use of dupilumab in a patient with atopic dermatitis, severe asthma, and HIV infection. Dermatol Ther. 2020;33: e14159.
Romagnuolo M, Angileri L, Tavecchio S, Marzano AV, Ferrucci S. Safety and efficacy of dupilumab in a patient with severe atopic dermatitis and HIV infection, with 15 months of follow-up. Clin Exp Dermatol. 2020;45:762–3.
Tanner JF, Knutsen AP, Siegfried E. Safety and efficacy of dupilumab in an atopic adolescent with primary immune deficiency. Dermat Contact Atopic Occup Drug. 2021;32:e91–2.
Naovarat BS, Salazar G, Ishimori M, Williams FM, Reveille JD. Biological treatment usage in patients with HIV and rheumatic disease, 2003–2021: long-term safety and follow-up. RMD Open. 2022;8: e002282.
Gavegnano C, Brehm JH, Dupuy FP, Talla A, Ribeiro SP, Kulpa DA, et al. Novel mechanisms to inhibit HIV reservoir seeding using Jak inhibitors. PLoS Pathog. 2017;13: e1006740.
Ly K, Smith MP, Thibodeaux Q, Beck K, Bhutani T, Liao W. Dupilumab in patients with chronic hepatitis B on concomitant entecavir. JAAD Case Rep. 2019;5:624.
Hong X, Xiao Y, Xu L, Liu L, Mo H, Mo H. Risk of hepatitis B reactivation in HBsAg−/HBcAb+ patients after biologic or JAK inhibitor therapy for rheumatoid arthritis: a meta-analysis. Immun Inflamm Dis. 2023;11: e780.
European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu, European Association for the Study of the Liver. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67:370–98.
Harigai M, Winthrop K, Takeuchi T, Hsieh T-Y, Chen Y-M, Smolen JS, et al. Evaluation of hepatitis B virus in clinical trials of baricitinib in rheumatoid arthritis. RMD Open. 2020;6: e001095.
Veeravalli V, Dash RP, Thomas JA, Babu RJ, Madgula LMV, Srinivas NR. Critical assessment of pharmacokinetic drug–drug interaction potential of tofacitinib, baricitinib and upadacitinib, the three approved Janus kinase inhibitors for rheumatoid arthritis treatment. Drug Saf. 2020;43:711–25.
Wang EQ, Le V, O’Gorman M, Tripathy S, Dowty ME, Wang L, et al. Effects of hepatic impairment on the pharmacokinetics of abrocitinib and its metabolites. J Clin Pharmacol. 2021;61:1311–23.
Trueman S, Mohamed MF, Feng T, Lacerda AP, Marbury T, Othman AA. Characterization of the effect of hepatic impairment on upadacitinib pharmacokinetics. J Clin Pharmacol. 2019;59:1188–94.
Silverberg JI, Brieva J. A successful case of dupilumab treatment for severe uremic pruritus. JAAD Case Rep. 2019;5:339–41.
Elamin S, Murphy B. Dupilumab in the management of atopic dermatitis in an immunosuppressed renal transplant patient. Clin Exp Dermatol. 2022;47:1191–3.
Waldman RA, DeWane ME, Sloan B, Grant-Kels JM, Lu J. Dupilumab for the treatment of dyshidrotic eczema in 15 consecutive patients. J Am Acad Dermatol. 2020;82:1251–2.
Lukac D, Pagani K, McGee JS. Overview of use, efficacy, and safety of dupilumab in complex patients: a retrospective, case-series study from a large, urban academic center. Arch Dermatol Res. 2023;315:1777–81.
Traidl S, Freimooser S, Werfel T. Janus kinase inhibitors for the therapy of atopic dermatitis. Allergol Sel. 2021;5:293–304.
Wojciechowski J, Malhotra BK, Wang X, Fostvedt L, Valdez H, Nicholas T. Population pharmacokinetics of abrocitinib in healthy individuals and patients with psoriasis or atopic dermatitis. Clin Pharmacokinet. 2022;61:709–23.
Mohamed M-EF, Trueman S, Feng T, Anderson J, Marbury TC, Othman AA. Characterization of the effect of renal impairment on upadacitinib pharmacokinetics. J Clin Pharmacol. 2019;59:856–62.
Wang EQ, Le V, Winton JA, Tripathy S, Raje S, Wang L, et al. Effects of renal impairment on the pharmacokinetics of abrocitinib and its metabolites. J Clin Pharmacol. 2022;62:505–19.
Lavan AH, Gallagher P. Predicting risk of adverse drug reactions in older adults. Ther Adv Drug Saf. 2016;7:11–22.
Silverberg JI, Lynde CW, Abuabara K, Patruno C, de Benedetto A, Zhang H, et al. Efficacy and safety of dupilumab maintained in adults ≥ 60 years of age with moderate-to-severe atopic dermatitis: analysis of pooled data from four randomized clinical trials. Am J Clin Dermatol. 2023;24:469–83.
Merola JF, Butler DC, Mark T, Schneider S, Kim Y, Abuabara K. Safety and efficacy of tralokinumab in older adults with moderate-to-severe atopic dermatitis: a secondary analysis. JAMA Dermatol. 2023;159:1119–23.
Nash P, Kerschbaumer A, Dörner T, Dougados M, Fleischmann RM, Geissler K, et al. Points to consider for the treatment of immune-mediated inflammatory diseases with Janus kinase inhibitors: a consensus statement. Ann Rheum Dis. 2021;80:71–87.
Alim K, Bruyère A, Lescoat A, Jouan E, Lecureur V, Le Vée M, et al. Interactions of Janus kinase inhibitors with drug transporters and consequences for pharmacokinetics and toxicity. Expert Opin Drug Metab Toxicol. 2021;17:259–71.
Veeravalli V, Dash RP, Thomas JA, Babu RJ, Madgula LMV, Srinivas NR. Critical assessment of pharmacokinetic drug–drug interaction potential of tofacitinib, baricitinib and upadacitinib, the three approved Janus kinase inhibitors for rheumatoid arthritis treatment. Drug Saf [Internet]. 2020 [cited 2023 Nov 20];43. https://pubmed.ncbi.nlm.nih.gov/32367507/.
Wang X, Dowty ME, Wouters A, Tatulych S, Connell CA, Le VH, et al. Assessment of the effects of inhibition or induction of CYP2C19 and CYP2C9 enzymes, or inhibition of OAT3, on the pharmacokinetics of abrocitinib and its metabolites in healthy individuals. Eur J Drug Metab Pharmacokinet. 2022;47:419–29.
Payne C, Zhang X, Shahri N, Williams W, Cannady E. AB0492 evaluation of potential drug–drug interactions with baricitinib. Ann Rheum Dis. 2015;74:1063–1063.
Schlösser AR, Shareef M, Olydam J, Nijsten TEC, Hijnen DJ. Tralokinumab treatment for patients with moderate-to-severe atopic dermatitis in daily practice. Clin Exp Dermatol. 2023;48:510–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Author Contributions
Megan Lam, Richard W. Kim, and Aaron M. Drucker conducted the literature search and drafted the manuscript. All authors critically revised and approved the final manuscript.
Funding
No funding was received for conducting this study.
Availability of Data and Material
This study did not use any primary data not available from other sources.
Conflicts of Interest
Dr. Drucker has received compensation from the British Journal of Dermatology (reviewer and section editor), American Academy of Dermatology (guidelines writer), National Eczema Association (grant reviewer), Canadian Dermatology Today (manuscript writer), and Canadian Agency for Drugs and Technologies in Health (consultant). Dr. Simpson reports personal fees from Advances in Cosmetic Medical Derm Hawaii LLC, AbbVie, Amgen, AOBiome LLC, Arcutis Biotherapeutics, Arena Pharmaceuticals, Aslan Pharma, Boehringer Ingelheim USA, Inc., Boston Consulting Group, Bristol Myers Squibb—BMS, Collective Acumen LLC (CA), CorEvitas, Dermira, Eli Lilly, Evelo Biosciences, Evidera, ExcerptaMedica, FIDE, Forte Bio RX, Galderma, GlaxoSmithKline, Incyte, Janssen, Johnson & Johnson, Kyowa Kirin Pharmaceutical Development, Leo Pharm, Medscape LLC, Merck, MauiDerm, MLG Operating, MJH holding, Pfizer, Physicians World LLC, PRImE, Regeneron, Revolutionizing Atopic Dermatitis Inc, Roivant, Sanofi-Genzyme, Trevi therapeutics, Valeant, Vindico Medical education, and WebMD. Dr. Drucker has received research grants to his institution from the National Eczema Association, Eczema Society of Canada, Canadian Dermatology Foundation, Canadian Institutes for Health Research, US National Institutes of Health, and Physicians Services Incorporated Foundation. Dr. Abuabara has received research grants to her institution from the National Eczema Association, the US National Institutes of Health, the LEO Foundation, Pfizer, and Cosmetique Internacional SNC. She has received compensation from TARGET RWE. Dr. Simpson reports grants (or serves as principal investigator role) from AbbVie, Acrotech Biopharma Inc, Amgen, Arcutis, Aslan, Castle Biosciences, CorEvitas, Dermavant, Dermira, Eli Lilly, Incyte, Kymab, Kyowa Kirin, National Jewish Health, Leo, Pfizer, Regeneron, Sanofi, and Target RWE. These potential conflicts of interest have been reviewed and managed by Oregon Health and Science University. Mr. Kim and Dr. Lam have no relevant financial or non-financial interests to disclose.
Ethics Approval
This article does not contain animal or human subjects that require approval by an ethics board.
Patient Consent to Participate
This article does not discuss any individuals or materials that would require consent for participation.
Patient Consent to Publish
This article does not discuss any individuals or materials that would require consent for publication.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, R.W., Lam, M., Abuabara, K. et al. Targeted Systemic Therapies for Adults with Atopic Dermatitis: Selecting from Biologics and JAK Inhibitors. Am J Clin Dermatol 25, 179–193 (2024). https://doi.org/10.1007/s40257-023-00837-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-023-00837-w