Abstract
Purpose
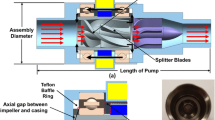
Wave membrane blood pumps (WMBP) are novel pump designs in which blood is propelled by means of wave propagation by an undulating membrane. In this paper, we computationally studied the performance of a new WMBP design (J-shaped) for different working conditions, in view of potential applications in human patients.
Methods
Fluid–structure interaction (FSI) simulations were conducted in 3D pump geometries and numerically discretized by means of the extended finite element method (XFEM). A contact model was introduced to capture membrane-wall collisions in the pump head. Mean flow rate and membrane envelope were determined to evaluate hydraulic performance. A preliminary hemocompatibility analysis was performed via calculation of fluid shear stress.
Results
Numerical results, validated against in vitro experimental data, showed that the hydraulic output increases when either the frequency or the amplitude of membrane oscillations were higher, with limited increase in the fluid stresses, suggesting good hemocompatibility properties. Also, we showed better performance in terms of hydraulic power with respect to a previous design of the pump. We finally studied an operating point which achieves physiologic flow rate target at diastolic head pressure of 80 mmHg.
Conclusion
A new design of WMBP was computationally studied. The proposed FSI model with contact was employed to predict the new pump hydraulic performance and it could help to properly select an operating point for the upcoming first-in-human trials.
















Similar content being viewed by others
Notes
The reader can contact the authors to ask for access to protected information on membrane dimensions and properties.
References
Alauzet, F., B. Fabrèges, M. A. Fernández, and M. Landajuela. Nitsche-XFEM for the coupling of an incompressible fluid with immersed thin-walled structures. Comput. Methods Appl. Mech. Eng. 301:300–335, 2016.
Alba, A. C., and D. H. Delgado. The future is here: Ventricular Assist Devices for the failing heart. Expert Rev. Cardiovasc. Ther. 7(9):1067–1077, 2009.
Allen, L. A., C. K. McIlvennan, J. S. Thompson, S. M. Dunlay, S. J. LaRue, E. F. Lewis, C. B. Patel, L. Blue, D. L. Fairclough, E. C. Leister, et al. Effectiveness of an intervention supporting shared decision making for destination therapy left ventricular assist device: the DECIDE-LVAD randomized clinical trial. JAMA Intern. Med. 178(4):520–529, 2018.
Arora, D., M. Behr, and M. Pasquali. Hemolysis estimation in a centrifugal blood pump using a tensor-based measure. Artif. Organs 30(7):539–547, 2006.
Bartoli, C., and R. Dowling. The next wave of Mechanical Circulatory Support Devices. Card. Interv. Today 13(1):53–59, 2019.
Behbahani, M., M. Behr, M. Hormes, U. Steinseifer, D. Arora, O. Coronado, and M. Pasquali. A review of computational fluid dynamics analysis of blood pumps. Eur. J. Appl. Math. 20(4):363–397, 2009.
Berk, Z. B., J. Zhang, Z. Chen, D. Tran, B. P. Griffith, and Z. J. Wu. Evaluation of in vitro hemolysis and platelet activation of a newly developed maglev LVAD and two clinically used LVADs with human blood. Artif. Organs 43(9):870–879, 2019.
Bertagna, L., S. Deparis, L. Formaggia, D. Forti, and A. Veneziani. The LifeV library: engineering mathematics beyond the proof of concept, 2017. arXiv preprint arXiv:1710.06596.
Bludszuweit, C.: Three-dimensional numerical prediction of stress loading of blood particles in a centrifugal pump. Artif. Organs 19(7):590–596, 1995.
Bluestein, D.: Research approaches for studying flow-induced thromboembolic complications in blood recirculating devices. Expert Rev. Med. Devices 1(1):65–80, 2004.
Bonnemain, J., A. C. I. Malossi, M. Lesinigo, S. Deparis, A. Quarteroni, and L. K. Von Segesser: Numerical simulation of left ventricular assist device implantations: comparing the ascending and the descending aorta cannulations. Med. Eng. Phys. 35(10):1465–1475, 2013.
Botterbusch, C., T. Snyder, P. P. Monticone, L. de Lillers, A. Schmidt, and C. Rasser. CorWave LVAD: insight into device concept and stage of development. In: Mechanical Support for Heart Failure. Cham: Springer, 2020, pp. 587–597.
Bourque, K., C. Cotter, C. Dague, D. Harjes, O. Dur, J. Duhamel, K. Spink, K. Walsh, and E. Burke. Design rationale and preclinical evaluation of the HeartMate 3 left ventricular assist system for hemocompatibility. ASAIO J. 62(4):375–383, 2016.
Burman, E., M. A. Fernández, and S. Frei. A Nitsche-based formulation for fluid–structure interactions with contact. ESAIM Math. Model. Numer. Anal. 54(2):531–564, 2020.
Chatterjee, A., S. Mariani, J. S. Hanke, T. Li, A. S. Merzah, R. Wendl, A. Haverich, J. D. Schmitto, and G. Dogan. Minimally invasive left ventricular assist device implantation: optimizing device design for this approach. Expert Rev. Med. Devices 17(4):323–330, 2020.
Chen, Z., S. K. Jena, G. A. Giridharan, M. A. Sobieski, S. C. Koenig, M. S. Slaughter, B. P. Griffith, and Z. J. Wu. Shear stress and blood trauma under constant and pulse-modulated speed CF-VAD operations: CFD analysis of the HVAD. Med. Biol. Eng. Comput. 57(4):807–818, 2019.
Den Uil, C. A., S. Akin, L. S. Jewbali, D. dos Reis Miranda, J. J. Brugts, A. A. Constantinescu, A. P. Kappetein, and K. Caliskan. Short-term mechanical circulatory support as a bridge to durable left ventricular assist device implantation in refractory cardiogenic shock: a systematic review and meta-analysis. Eur. J. Cardio-thorac. Surg. 52(1):14–25, 2017.
Down, L. A., D. V. Papavassiliou, and A. Edgar. Significance of extensional stresses to red blood cell lysis in a shearing flow. Ann. Biomed. Eng. 39(6):1632–1642, 2011.
Faggiano, E., L. Antiga, G. Puppini, A. Quarteroni, G. B. Luciani, and C. Vergara. Helical flows and asymmetry of blood jet in dilated ascending aorta with normally functioning bicuspid valve. Biomech. Model. Mechanobiol. 12(4):801–813, 2013.
Faghih, M. M., and M. K. Sharp. Modeling and prediction of flow-induced hemolysis: a review. Biomech. Model. Mechanobiol. 18(4):845–881, 2019.
Faghih, M. M., and M. K. Sharp. Deformation of human red blood cells in extensional flow through a hyperbolic contraction. Biomech. Model. Mechanobiol. 19(1):251–261, 2020.
Formaggia, L., F. Gatti, and S. Zonca. An XFEM/DG approach for fluid–structure interaction problems with contact. Appl. Math. 66(2):183–211, 2021.
Fraser, K. H., M. E. Taskin, T. Zhang, B. P. Griffith, and Z. J. Wu. Comparison of shear stress, residence time and Lagrangian estimates of hemolysis in different ventricular assist devices. In: 26th Southern Biomedical Engineering Conference SBEC 2010, April 30–May 2, 2010, College Park, Maryland, USA. Springer, 2010, pp. 548–551.
Fraser, K. H., T. Zhang, M. E. Taskin, B. P. Griffith, and Z. J. Wu. A quantitative comparison of mechanical blood damage parameters in rotary ventricular assist devices: shear stress, exposure time and hemolysis index. J. Biomech. Eng. 134(8):081002, 2012.
Frei, S., Gerosa, F., Burman, E., Fernández, M.A.: A mechanically consistent model for fluid–structure interactions with contact including seepage
Gerstenberger, A., and W. A. Wall. An extended finite element method/Lagrange multiplier based approach for fluid–structure interaction. Comput. Methods Appl. Mech. Eng. 197(19–20):1699–1714, 2008.
Geuzaine, C., and J. F. Remacle. GMSH: a 3-D finite element mesh generator with built-in pre- and post-processing facilities. Int. J. Numer. Methods Eng. 79(11):1309–1331, 2009.
Ghodrati, M., A. Maurer, T. Schlöglhofer, T. Khienwad, D. Zimpfer, D. Beitzke, F. Zonta, F. Moscato, H. Schima, and P. Aigner. The influence of left ventricular assist device inflow cannula position on thrombosis risk. Artif. Organs 44(9):939–946, 2020.
Graefe, R., A. Henseler, R. Körfer, B. Meyns, and L. Fresiello. Influence of left ventricular assist device pressure-flow characteristic on exercise physiology: assessment with a verified numerical model. Int. J. Artif. Organs 42(9):490–499, 2019.
Hansbo, A., and P. Hansbo. An unfitted finite element method, based on Nitsche’s method, for elliptic interface problems. Comput. Methods Appl. Mech. Eng. 191(47–48):5537–5552, 2002.
Hellums, J. D.: 1993 Whitaker Lecture: biorheology in thrombosis research. Ann. Biomed. Eng. 22(5):445–455, 1994.
Kadakia, S., R. Moore, V. Ambur, and Y. Toyoda. Current status of the implantable LVAD. Gen. Thorac. Cardiovasc. Surg. 64(9):501–508, 2016.
Kannojiya, V., A. K. Das, and P. K. Das. Numerical simulation of centrifugal and hemodynamically levitated LVAD for performance improvement. Artif. Organs 44(2):E1–E19, 2019.
Martinolli, M., J. Biasetti, S. Zonca, L. Polverelli, and C. Vergara. Extended finite element method for fluid–structure interaction in wave membrane blood pump. Int. J. Numer. Methods Biomed. Eng. 2021. https://doi.org/10.1002/cnm.3467.
Mayer, U. M., A. Popp, A. Gerstenberger, W. A. Wall. 3D fluid–structure-contact interaction based on a combined XFEM FSI and dual mortar contact approach. Comput. Mech. 46(1):53–67, 2010.
Moazami, N., K. Fukamachi, M. Kobayashi, N. G. Smedira, K. J. Hoercher, A. Massiello, S. Lee, D. J. Horvath, and R. C. Starling. Axial and centrifugal continuous-flow rotary pumps: a translation from pump mechanics to clinical practice. J. Heart Lung Transplant. 32(1):1–11, 2013.
Molteni, A., Z. P. H. Masri, K. W. Q. Low, H. N. Yousef, J. Sienz, and K. H. Fraser. Experimental measurement and numerical modelling of dye washout for investigation of blood residence time in ventricular assist devices. Int. J. Artif. Organs 41(4):201–212, 2018.
Nobile, F., M. Pozzoli, and C. Vergara. Time accurate partitioned algorithms for the solution of fluid–structure interaction problems in haemodynamics. Comput. Fluids 86:470–482, 2013.
Papanastasiou, C. A., K. G. Kyriakoulis, C. A. Theochari, D. G. Kokkinidis, T. D. Karamitsos, and L. Palaiodimos. Comprehensive review of hemolysis in ventricular assist devices. World J. Cardiol. 12(7):334–341, 2020.
Passerini, T., A. Quaini, U. Villa, A. Veneziani, and S. Canic. Validation of an open source framework for the simulation of blood flow in rigid and deformable vessels. Int. J. Numer. Methods Biomed. Eng. 29(11):1192–1213, 2013.
Pauli, L., J. Nam, M. Pasquali, and M. Behr. Transient stress-based and strain-based hemolysis estimation in a simplified blood pump. Int. J. Numer. Methods Biomed. Eng. 29(10):1148–1160, 2013.
Perschall, M., J. B. Drevet, T. Schenkel, and H. Oertel. The progressive wave pump: numerical multiphysics investigation of a novel pump concept with potential to ventricular assist device application. Artif. Organs 9(36):E179–E190, 2012.
Pozzi, S., M. Domanin, L. Forzenigo, E. Votta, E. Zunino, A. Redaelli, and C. Vergara. A surrogate model for plaque modeling in carotids based on robin conditions calibrated by cine MRI data. Int. J. Numer. Methods Biomed. Eng. 37(5):e3447, 2021.
Quarteroni, A., L. Dedè, A. Manzoni, and C. Vergara. Mathematical Modelling of the Human Cardiovascular System—Data, Numerical Approximation, Clinical Applications. Cambridge: Cambridge University Press, 2019.
Rayz, V., L. Boussel, L. Ge, J. Leach, A. Martin, M. Lawton, C. McCulloch, and D. Saloner. Flow residence time and regions of intraluminal thrombus deposition in intracranial aneurysms. Ann. Biomed. Eng. 38(10):3058–3069, 2010.
Roberts, N., U. Chandrasekaran, S. Das, Z. Qi, and S. Corbett. Hemolysis associated with Impella heart pump positioning: in vitro hemolysis testing and computational fluid dynamics modeling. Int. J. Artif. Organs 43(11):710–718, 2020.
Scheffler, M., N. Mechbal, E. Monteiro, M. Rebillat, and R. Pruvost. Implementation and evaluation of a sensorless, nonlinear stroke controller for an implantable, undulating membrane blood pump. IFAC-PapersOnLine 53(2):8683–8688, 2020.
Thamsen, B., B. Blümel, J. Schaller, C. O. Paschereit, K. Affeld, L. Goubergrits, and U. Kertzscher. Numerical analysis of blood damage potential of the HeartMate II and HeartWare HVAD rotary blood pumps. Artif. Organs 39(8):651–659, 2015.
Theochari, C. A., G. Michalopoulos, E. K. Oikonomou, S. Giannopoulos, I. P. Doulamis, M. A. Villela, and D. G. Kokkinidis. Heart transplantation versus left ventricular assist devices as destination therapy or bridge to transplantation for 1-year mortality: a systematic review and meta-analysis. Ann. Cardiothorac. Surg. 7(1):3–11, 2018.
Topper, S. R., M. A. Navitsky, R. B. Medvitz, E. G. Paterson, C. A. Siedlecki, M. J. Slattery, S. Deutsch, G. Rosenberg, and K. B. Manning. The use of fluid mechanics to predict regions of microscopic thrombus formation in pulsatile VADs. Cardiovasc. Eng. Technol. 5(1):54–69, 2014.
Virani, S. S., A. Alonso, E. J. Benjamin, M. S. Bittencourt, C. W. Callaway, A. P. Carson, A. M. Chamberlain, A. R. Chang, S. Cheng, F. N. Delling, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation 141(9):e139–e596, 2020.
Wang, Y., P. Shen, M. Zheng, P. Fu, L. Liu, J. Wang, and L. Yuan. Influence of impeller speed patterns on hemodynamic characteristics and hemolysis of the blood pump. Appl. Sci. 9(21):4689, 2019.
Xie, A., K. Phan, and T. D. Yan. Durability of continuous-flow left ventricular assist devices: a systematic review. Ann. Cardiothorac. Surg. 3(6):54556–54756, 2014.
Zonca, S., C. Vergara, and L. Formaggia. An unfitted formulation for the interaction of an incompressible fluid with a thick structure via an XFEM/DG approach. SIAM J. Sci. Comput. 40(1):B59–B84, 2018.
Acknowledgments
MM and CV are members of the INdAM Research Group GNCS. The authors wish to acknowledge Charlotte Rasser from CorWave SA for her assistance in manuscript editing and revision.
Funding
This project has received funding from the European Union’s Horizon 2020 Research and Innovation Programme under the Marie Skłodowska-Curie Grant Agreement “ROMSOC - Reduced Order Modelling, Simulation and Optimization of Coupled systems”—No. 765374.
Author Contributions
MM: conceiving of the presented idea, design of the computational framework, implementation of the code, numerical simulations, first draft and writing of the manuscript, discussion of the results. FC: writing of the manuscript, discussion of the results, experimental planning. CV: conceiving of the presented idea, design of the computational framework, writing of the manuscript, discussion of the results, project supervision.
Data Availability
The experimental data used for the validation of the numerical results in Fig. 9 are publically available on Zenodo (https://doi.org/10.5281/zenodo.4964021).
Code Availability
Not available.
Consent for Publication
Not applicable.
Conflict of interest
M. Martinolli and C. Vergara declare that they have no conflict of interest. F. Cornat is employed at Corwave SA, which designed the wave membrane blood pump considered in this work. However, the research has been funded by European Community and not by the company.
Ethical Approval
Not applicable.
Informed Consent
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Igor Efimov oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martinolli, M., Cornat, F. & Vergara, C. Computational Fluid–Structure Interaction Study of a New Wave Membrane Blood Pump. Cardiovasc Eng Tech 13, 373–392 (2022). https://doi.org/10.1007/s13239-021-00584-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-021-00584-1