Abstract
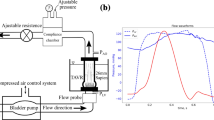
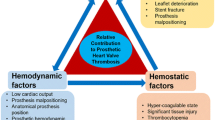
We compare the velocity and shear obtained from particle image velocimetry (PIV) and computational fluid dynamics (CFD) in a pulsatile ventricular assist device (VAD) to further test our thrombus predictive methodology using microscopy data from an explanted VAD. To mimic physiologic conditions in vitro, a mock circulatory loop was used with a blood analog that matched blood’s viscoelastic behavior at 40% hematocrit. Under normal physiologic pressures and for a heart rate of 75 bpm, PIV data is acquired and wall shear maps are produced. The resolution of the PIV shear rate calculations are tested using the CFD and found to be in the same range. A bovine study, using a 50 cc Penn State V-2 VAD, for 30 days at a constant beat rate of 75 beats per minute (bpm) provides the microscopic data whereby after the 30 days, the device is explanted and the sac surface analyzed using scanning electron microscopy (SEM) and, after immunofluorescent labeling for platelets and fibrin, confocal microscopy. Areas are examined based on PIV measurements and CFD, with special attention to low shear regions where platelet and fibrin deposition are most likely to occur. Data collected within the outlet port in a direction normal to the front wall of the VAD shows that some regions experience wall shear rates less than 500 s−1, which increases the likelihood of platelet and fibrin deposition. Despite only one animal study, correlations between PIV, CFD, and in vivo data show promise. Deposition probability is quantified by the thrombus susceptibility potential, a calculation to correlate low shear and time of shear with deposition.










Similar content being viewed by others
References
Balasubramanian, V., and S. M. Slack. The effect of fluid shear and co-adsorbed proteins on the stability of immobilized fibrinogen and subsequent platelet interactions. J. Biomater. Sci. Polym. Ed. 13:543–561, 2002.
Cooper, B. T., B. N. Roszelle, T. C. Long, S. Deutsch, and K. B. Manning. The 12 cc Penn State pulsatile pediatric ventricular assist device: fluid dynamics associated with valve selection. J. Biomech. Eng. 130(4):041019, 2008.
Crowe, C. T., M. Sommerfeld, and Y. Tsuji. Multiphase Flows with Droplets and Particles. Boca Raton, FL: CRC Press, 1998.
Gorbet, M. B., and M. V. Sefton. Biomaterial-associated thrombosis: roles of coagulation factors, complement, platelets and leukocytes. Biomaterials 25:5681–5703, 2004.
Hernandez, A. F., A. M. Shea, C. A. Milano, J. G. Rogers, B. G. Hammill, C. M. O’Connor, K. A. Schulman, E. D. Peterson, and L. H. Curtis. Long-term outcomes and costs of ventricular assist devices among Medicare beneficiaries. JAMA 300(20):2398–2406, 2008.
Hochareon, P., K. B. Manning, A. A. Fontaine, J. M. Tarbell, and S. Deutsch. Fluid dynamic analysis of the 50 cc Penn State artificial heart under physiological operating conditions using particle image velocimetry. J. Biomech. Eng. 126:585–593, 2004.
Hochareon, P., K. B. Manning, A. A. Fontaine, J. M. Tarbell, and S. Deutsch. Correlation of in vivo clot deposition with the flow characteristics in the 50 cc Penn State artificial heart: a preliminary study. ASAIO J. 50(6):537–542, 2004.
Hochareon, P., K. B. Manning, A. A. Fontaine, J. M. Tarbell, and S. Deutsch. Wall shear-rate estimation within the 50 cc Penn State artificial heart using particle image velocimetry. J. Biomech. Eng. 126:430–437, 2004.
Hubbell, J. A., and L. V. McIntire. Visualization and analysis of mural thrombogenesis on collagen, polyurethane and nylon. Biomaterials 7:354–363, 1986.
Jen, C. J., H.-M. Li, J.-S. Wang, H. Chen, and S. Usami. Flow-induced detachment of adherent platelets from fibrinogen-coated surface. Am. J. Physiol. 270 (Heart Circ Physiol 39):H160–H166, 1996.
Kim, J., G. Ryu, I. Shin, K. Lee, D. Han, Y. Kim, and B. Min. Effect of shear rates on protein adsorption in the total artificial heart. ASAIO J. 38:M532–M535, 1992.
Kirklin, J. K., D. C. Naftel, R. L. Kormos, L. W. Stevenson, F. D. Pagani, M. A. Miller, J. T. Baldwin, and J. B. Young. Fifth INTERMACS annual report: risk factor analysis from more than 6,000 mechanical circulatory support patients. J. Heart Lung Transpl. 32(2):141–156, 2013.
Kreider, J., K. B. Manning, L. A. Oley, A. A. Fontaine, and S. Deutsch. The 50 cc Penn State LVAD: a parametric study of valve orientation flow dynamics. ASAIO J. 52:123–131, 2006.
Long, J. A., A. Undar, K. B. Manning, and S. Deutsch. Viscoelasticity of pediatric blood and its implications of the testing of a pulsatile pediatric blood pump. ASAIO J. 51:63–566, 2005.
Medvitz, R. B., J. W. Kreider, K. B. Manning, A. A. Fontaine, S. Deutsch, and E. G. Paterson. Development and validation of a computational fluid dynamics methodology for simulation of pulsatile left ventricular assist devices. ASAIO J. 53(2):122–131, 2007.
Medvitz, R. B., V. Reddy, S. Deutsch, K. B. Manning, and E. G. Paterson. Validation of a CFD methodology for positive displacement LVAD analysis using PIV data. J. Biomech. Eng. 131(10):111009, 2009.
Mehta, S., W. Pae, G. Rosenberg, A. J. Snyder, W. J. Weiss, J. P. Lewis, D. J. Frank, J. J. Thompson, and W. S. Pierce. The LionHeart LVD-2000: a completely implanted left ventricular assist device for chronic circulatory support. Ann. Thorac. Surg. 71:156–161, 2001.
Milner, K. R., A. J. Snyder, and C. A. Siedlecki. Sub-micron texturing for reducing platelet adhesion to polyurethane biomaterials. J. Biomed. Mater. Res. A 76A(3):561–570, 2006.
Nanna, J. C., M. A. Navitsky, S. R. Topper, S. Deutsch, and K. B. Manning. A fluid dynamics study in a 50 cc pulsatile ventricular assist device: influence of heart rate variability. J. Biomech. Eng. 133(10):101002, 2011.
Nanna, J. C., J. A. Wivholm, S. Deutsch, and K. B. Manning. Flow field study comparing design iterations of a 50 cc left ventricular assist device. ASAIO J. 57(5):349–357, 2011.
Navitsky, M. A., S. Deutsch, and K. B. Manning. A thrombus susceptibility comparison of two pulsatile Penn State 50 cc left ventricular assist device designs. Ann. Biomed. Eng. 41(1):4–16, 2013.
Roger, V. L., A. S. Go, D. M. Lloyd-Jones, R. J. Adams, J. D. Berry, et al. Heart disease and stroke statistics—2011 update, a report from the American Heart Association. Circulation 123:18–209, 2011.
Rosenberg, G., W. M. Phillips, D. L. Landis, and W. S. Pierce. Design and evaluation of the Pennsylvania State University mock circulatory system. ASAIO J. 4:41–49, 1981.
Roszelle B. The 12 cc Penn State pediatric ventricular assist device: a flow visualization study of bridge-to-recovery and weaning. PhD thesis, The Pennsylvania State University. 2010.
Shreenivas, S., J. Rame, and M. Jessup. Mechanical circulatory support as a bridge to transplant or for destination therapy. Curr. Heart Fail Rep. 7:159–166, 2010.
Yamanaka, H., G. Rosenberg, W. J. Weiss, A. J. Snyder, C. M. Zapanta, and C. A. Siedlecki. Multiscale analysis of surface thrombosis in vivo in a left ventricular assist system. ASAIO J. 51(5):567–577, 2005.
Yamanaka, H., G. Rosenberg, W. J. Weiss, A. J. Snyder, C. M. Zapanta, and C. A. Siedlecki. Short-term in vivo studies of surface thrombosis in a left ventricular assist system. ASAIO J. 52(3):257–265, 2006.
Acknowledgments
We would like to acknowledge the National Institutes of Health for their support of this project through NIH NHLBI HL60276. Stephen R. Topper, Michael A. Navitsky, Richard B. Medvitz, Eric G. Paterson, Christopher A. Siedlecki, Margaret J. Slattery, Steven Deutsch, Gerson Rosenberg, and Keefe B. Manning declare that they have no conflict of interest. All institutional and national guidelines for the care and use of laboratory animals were followed and approved by the appropriate institutional committees (Penn State IACUC #97104). No human studies were carried out by the authors for this article.
Conflicts of Interest
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Steven C. George oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Topper, S.R., Navitsky, M.A., Medvitz, R.B. et al. The Use of Fluid Mechanics to Predict Regions of Microscopic Thrombus Formation in Pulsatile VADs. Cardiovasc Eng Tech 5, 54–69 (2014). https://doi.org/10.1007/s13239-014-0174-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-014-0174-x