Abstract
Purpose
Point-of-care ultrasound (POCU) is an evolving field in anesthesia. Therefore a systematic review of common diagnoses made by POCU during non-cardiac surgery was conducted. The information obtained from the review may be used to develop POCU curricula for the perioperative setting during non-cardiac surgery.
Source
A systematic review was conducted for perioperative use of transthoracic /transesophageal echocardiography (TTE/TEE) in high-risk patients or in other patients experiencing periods of hemodynamic instability. The diagnoses included segmental wall motion abnormalities (SWMAs), low left ventricular ejection fraction (LVEF), hypovolemia, air embolism, cardiac/aortic thrombus, pulmonary embolus (PE), aortic valve disease, mitral valve disease, tricuspid valve disease, right ventricular (RV) failure, pericardial disease, and patent foramen ovale.
Principal findings
Three hundred twenty-one studies were found using our search terms, and thirteen studies were retained that met our inclusion criteria for review. The studies included 968 patients analyzed as either preoperative exams in high-risk patients (n = 568) or intraoperative exams during times of hemodynamic compromise/cardiac arrest (n = 400). The most common diagnoses in the preoperative exam group were low ejection fraction (25.4%), aortic valve disease (24.4%), mitral valve disease (20.0%), RV failure (6.6%), and hypovolemia (6.3%). In the intraoperative exam group, the most common diagnoses were hypovolemia (33.2%), low ejection fraction (20.5%), RV failure (13.1%), SWMAs (10.1%), and PE (5.8%).
Conclusion
In this systematic review examining the use of TTE or TEE in non-cardiac surgery, the most frequent diagnoses were valvulopathy, low LVEF, hypovolemia, PE, SWMAs, and RV failure. This information should be used to inform evidence-based curricula for POCU in anesthesiology.
Résumé
Objectif
L’échoguidage au chevet est un domaine de l’anesthésie en pleine évolution. Pour cette raison, nous avons réalisé une revue méthodique des diagnostics courants posés par échoguidage au chevet pendant les chirurgies non cardiaques. Les renseignements tirés de cette revue pourraient servir à mettre au point un programme de cours en échoguidage au chevet dans le cadre périopératoire de chirurgies non cardiaques.
Source
Nous avons réalisé une revue méthodique de l’utilisation périopératoire de l’échocardiographie transthoracique / transœsophagienne (ÉTT / ÉTO) chez les patients à risque élevé et chez d’autres patients souffrant d’épisodes d’instabilité hémodynamique. Les diagnostics comprenaient les anomalies segmentaires de contractilité (ASC), une faible fraction d’éjection du ventricule gauche (FEVG), l’hypovolémie, l’embolie gazeuse, le thrombus cardiaque/aortique, l’embolie pulmonaire (EP), la valvulopathie aortique, la valvulopathie mitrale, la valvulopathie tricuspide, l’insuffisance cardiaque droite, les maladies péricardiques et la persistance du foramen ovale.
Constatations principales
Au total, nous avons trouvé 321 études à l’aide de nos termes de recherche, et en avons retenu treize qui répondaient à nos critères d’inclusion pour étude. Les études comprenaient 968 patients au total, dont les examens avaient été réalisés soit en période préopératoire (patients à risque élevé, n = 568) ou en période peropératoire en cas d’instabilité hémodynamique ou d’arrêt cardiaque (n = 400). Les diagnostics les plus fréquents dans le groupe d’examen préopératoire étaient une faible fraction d’éjection (25,4 %), une valvulopathie aortique (24,4 %), une valvulopathie mitrale (20,0 %), une insuffisance cardiaque droite (6,6 %) et l’hypovolémie (6,3 %). Dans le groupe ayant subi un examen peropératoire, les diagnostics les plus fréquemment posés étaient l’hypovolémie (33,2 %), une faible fraction d’éjection (20,5 %), une insuffisance cardiaque droite (13,1 %), des ASC (10,1 %) et des EP (5,8 %).
Conclusion
Dans cette revue méthodique examinant l’utilisation de l’ÉTT et de l’ÉTO en chirurgie non cardiaque, les diagnostics les plus fréquemment posés étaient les valvulopathies, une faible FEVG, l’hypovolémie, l’EP, les ASC et l’insuffisance cardiaque droite. Ces informations devraient être utilisées pour guider les programmes de cours fondés sur des données probantes pour l’échoguidage au chevet en anesthésiologie.
Similar content being viewed by others
Ultrasound has become an essential monitor during cardiac surgery; however, the body of evidence supporting its use in non-cardiac surgery is lacking. As the patient population becomes older and more complex, the number of patients with cardiac comorbidities encountered outside the cardiac operating room is increasing. Cardiac ultrasound can be an essential tool in diagnosing the causes of hemodynamic instability in patients.1 Point-of-care ultrasound (POCU) is an evolving field in anesthesia that may have a role in both diagnosis and management of this critically ill population.
Point-of-care ultrasound is the application of ultrasound for real-time goal-focused assessment and intervention in acute care settings.2 Point-of-care ultrasound has experienced rapid growth in the intensive care unit (ICU) or emergency medicine where consultants and residents/fellows alike are trained to be competent in ultrasonography. For example, focused POCU is commonly used in the ICU to identify hypovolemia, left ventricular (LV) and right ventricular (RV) failure, pleural and pericardial effusions, pneumothoraces, etc.3 In trauma surgery, ultrasound has been incorporated as the Focused Assessment with Sonography for Trauma (FAST) exam.4 The FAST exam has even been integrated into the Advanced Trauma Life Support (ATLS) algorithm as a necessary part of the primary survey and has essentially replaced more invasive modalities such as diagnostic peritoneal lavage. It is important to emphasize that the criteria for these exams were derived from a consensus of expert opinion. The current curricula for teaching this skill are directed toward learners in ICU and emergency medicine and are based on consensus guidelines, not on evidence.5,6
Despite the potential benefit of POCU, its use by the anesthesiologist during non-cardiac surgery has not been systematically explored. Widespread use of this perioperative tool is limited due to the specific training and expertise required. While cardiac anesthesiologists receive extensive training in transesophageal echocardiography (TEE), the current training curriculum for anesthesiology trainees as a whole has not been well developed. Instead, training curricula have revolved around small local endeavours largely established through anecdote and consensus but not evidence-based methodology.
Most point-of-care teaching has focused on a limited area of expertise in ultrasound, recognizing that intensivists, surgeons or emergency doctors are not experts in the interpretation of all aspects of ultrasonography. Course teaching is thus limited in scope and training of anesthesiologists in perioperative ultrasound seems to be taking a similar path. It would be informative for educators to understand what diagnoses are commonly seen in the perioperative period, thus facilitating a more focused and evidence-based course curriculum in perioperative ultrasound. Although there are many narrative reviews examining the use of ultrasound in non-cardiac surgery, to date, formal systematic reviews are lacking on this topic.
In order to address this topic, we completed a systematic review of the literature specifically examining the use of transthoracic echocardiography (TTE) and TEE in non-cardiac surgery. Considering that many non-anesthesia practitioners utilize this modality for diagnosis during both elective and emergency situations, we hypothesized that ultrasound has utility in both the preoperative and intraoperative period, particularly during periods of hemodynamic compromise.
Methods
Search strategy and selection criteria
Ethics approval was not required for this review, and an extensive background review of the literature was completed prior to initiating the study. A systematic review of observational studies was then conducted to evaluate the use of TTE and TEE in the preoperative and intraoperative settings for either high-risk patients immediately prior to induction of anesthesia or in all other surgical patients during periods of hemodynamic instability, respectively. The prespecified protocol outlined the research question, search strategy, inclusion/ exclusion criteria, and primary/ secondary diagnoses of interest.
Three investigators and one medical librarian searched PubMed, MEDLINE® (Ovid), EMBASE™, Cochrane, CINAHL, and the reference lists of relevant articles. The search terms included a combination of keywords and MeSH terms related to “transthoracic echocardiography”, “TTE”, “transesophageal echocardiography”, “TEE”, “ultrasound”, “perioperative care/period”, “risk assessment”, “diagnosis”, “predictive value of testing”, and “non-cardiac surgery”. The search strings were developed by the medical librarian and were adapted to the unique lexicons and requirements of each database. The final search was conducted on March 24, 2015.
Study inclusion entailed meeting the following criteria: any study design in any language, adult non-cardiac surgical patients (> 18 yr of age), patients undergoing perioperative ultrasound (either immediately prior to induction or intraoperatively), and reported findings or diagnoses were observed by ultrasound. The non-English studies were translated into English by anesthesiologists who were fluent in the language of the original publication. The studies were read by an echocardiographer with more than one year’s experience in perioperative ultrasound or with certification in perioperative ultrasonography. The studies performed in the pre-assessment clinic were excluded.
Data extraction and outcome definitions
After identifying relevant studies, two independent investigators extracted data into a standardized data collection sheet. Primary outcomes were established a priori, including left ventricular segmental wall motion abnormalities (SWMAs), low left ventricular ejection fraction (LVEF), intracardiac air, thrombus, pulmonary embolism (PE), aortic valve disease (stenosis or insufficiency), mitral valve disease (stenosis or insufficiency), tricuspid valve (TV) disease (stenosis or insufficiency), RV failure, pericardial effusion, and patent foramen ovale (PFO). The secondary outcomes included LV outflow tract obstruction, systolic anterior motion (SAM) of the mitral valve, pulmonary hypertension, vasodilation, and pulmonic valve disease. The disagreements in data extraction were resolved by consensus. Definitions for diagnoses observed by ultrasound were accepted as reported by the authors of the individual included studies. The data are reported as 1) a percent of all diagnoses made for either the preoperative or intraoperative time periods, as patients may have had more than one diagnosis (diagnosis/total diagnoses), and 2) a percent of patients with the diagnosis (diagnosis/total patients) reported as weighted mean and confidence interval (CI).
Statistical analysis
The weighted incidence for each type of diagnosis found during perioperative ultrasound was calculated for the total population across the studies. Since heterogeneity was anticipated, the incidence of each diagnosis was calculated using both the fixed effects model and the random effects model. The fixed effects model provides a true weighted incidence whereby larger studies contribute more weight than smaller studies to the overall estimate of incidence. The random effects model allows the mean incidence from each study to contribute more proportionally to the overall estimate of incidence, similar to a blunt “average of all averages” across studies.
There is no consensus whether the fixed effects or random effects model provides the best indicator for a weighted analysis of single-arm descriptive studies when the purpose of the analysis is to describe “expected incidence” across a population.7,8 The fixed effects model is the model most easily understood as it provides the greatest weight to larger studies. For this reason, the fixed effects model (the typical interpretation of “weighted” analysis for descriptive statistics) is presented.
Results
The search generated 321 studies with abstracts. The abstracts were then reviewed, and 55 full texts were selected for further review. This yielded 13 studies suitable for data extraction. Four of these 13 studies used TTE, eight used TEE, and one9 utilized both TTE and TEE for diagnosis. All echocardiographers were anesthesiologists trained in cardiac ultrasonography (Table 1). One study used the term valvulopathy as a category and was therefore excluded from the analysis for valve disease.10
There were 775 diagnoses identified from these studies.9-20 All the studies were reported as comprehensive examinations, which was reflected in the broad diversity of diagnoses. As described previously, preoperative exams occurred immediately prior to induction of anesthesia and data from pre-assessment clinic exams were not included. From the preoperative echocardiography studies, the most common diagnoses (diagnosis/all diagnoses) were low EF (25.4%), aortic valve disease (24.4%), mitral valve disease (20.0%), and RV failure (6.6%) (Fig. 1, Table 2). Diagnoses that were not originally included as primary outcomes were pulmonary hypertension, vasodilation, pulmonic valve disease, and LV outflow tract obstruction (Table 2). The most common diagnoses seen during intraoperative exams were hypovolemia (33.2%), low EF (20.5%), RV failure (13.1%), SWMA (10.1%), and PE (5.8%) (Fig. 2, Table 2). The incidence of diagnosis based on the number of patients with a given diagnosis (patients diagnosed/total patients) is presented in Table 3 along with 95% confidence intervals using fixed effects modelling. Other outcomes noticed during these exams included myocardial infarction and SAM (Table 3). All other outcomes were diagnosed less than 10% of the time.
Discussion
This novel systematic review examines the use of comprehensive POCU in non-cardiac surgery. This review evaluated two groups requiring a cardiac examination. The first group consisted of high-risk patients such as those presenting for surgery with concerning historical factors or physical exam findings that warranted an ultrasound exam. The second group consisted of any other patients who experienced hemodynamic instability or perioperative cardiac arrest.
The diagnoses most frequently recognized in the high-risk preoperative group were aortic valve disease, low EF, and mitral valve disease. Right ventricular failure, SWMAs, and TV disease were also frequently diagnosed. The diagnoses most frequently recognized in the other intraoperative group who had experienced hemodynamic instability were low EF, hypovolemia, RV failure, SWMAs, and PE. All other diagnoses occurred less than 10% of the time for both groups. These data summarize the available evidence base currently available.
In anesthesia practice, the use of ultrasound has been long established with TEE in the cardiac surgical setting involving advanced assessment of cardiac and valvular function. The expansion of ultrasound to non-cardiac surgery has predominately been with TEE. Nevertheless, the growing number of perioperative practitioners with advanced TTE training has allowed studies to be published on the possible diagnoses affecting these patients.21 Importantly, evidence-based curricula for POCU in the perioperative setting have not yet been widely developed.
In the context of POCU, our findings suggest that the intraoperative environment is different compared with the emergency department and ICU with respect to commonly seen pathology. This makes designing a separate curriculum for bedside perioperative echocardiography necessary for adequate training. This also means that any curriculum should be diverse and multipurpose as the practice of anesthesiology occurs in many unique settings, such as in the pre-assessment clinic, during the immediate preoperative assessment, in the perioperative environment, and in the postanesthesia care unit.2,21,22
Therefore, existing POCU curricula may not be adequate for the anesthesiologist. This review suggests that there is a need for more “advanced” training such as that required for diagnosing valvulopathy. There is currently a push to train anesthesiologists to provide basic interpretation of echocardiography to aid in diagnoses, either preoperatively in high-risk and/or emergent patients as well as intraoperatively during hemodynamic deterioration. Such training should focus on common diagnoses in either of these settings. In order to test the incremental effectiveness of POCU in non-cardiac surgery, optimal training programs need to be created with a focus on common diagnoses.
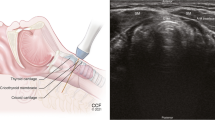
One challenge in creating such curricula is the decision to incorporate TEE, TTE, or both. This study showed that proficiency in both TTE and TEE is advantageous in the perioperative environment. Although TEE readily acquires high-quality images, it is more invasive, and some patients may have contraindications to its application. Conversely, surgical fields, cardiopulmonary resuscitation, etc. may prohibit the use of TTE. The preoperative use of TTE has the benefit of being noninvasive and, accordingly, can be used in awake patients. Nevertheless, TEE does not interfere with most surgical procedures and provides superior imaging, particularly in the tracheally intubated patient.23,24
There were some limitations in our review. For example, the studies in our analysis were completed by physicians with advanced level training in ultrasound, and all completed a comprehensive ultrasound examination. This skill set would be generally considered beyond what is necessary for POCU practice and thus may not be generalizable to the target audience for POCU training. Striking the balance between rapid skill and knowledge acquisition in novices will need to be balanced with the requirement for diagnoses of complex pathologies, including various valvulopathies. Additionally, our results likely reflect a general surgical population, while certain population subsets, such as trauma, may not have been adequately represented.
An additional limitation was associated with the relative paucity of information in the literature on this topic. The majority of studies we found consisted of a small sample size, were observational in nature, and showed heterogeneous results. It is possible, however, that not all relevant studies were found, particularly those that were non-English. Because of these limited data, this review combined the results of both TEE and TTE in this analysis.
Furthermore, this study addressed only echocardiography. Point-of-care ultrasound exists far beyond the domain of echocardiography to include abdominal, lung, and deep vein thrombosis imaging, which is beyond the scope of this review but may be of use to the anesthesiologist.25Nevertheless, the cardiac system per se is complex and pathologies seldom occur in isolation. Therefore, a curriculum incorporating exams of these different body systems may be appropriate.
In these studies, ultrasound guided the anesthesiologist in diagnosis and, in some circumstances, it modified medical care. Nevertheless, although data suggest that POCU changes physician behaviour, there is currently lack of evidence to suggest that it improves patient outcome.2 Therefore, it is important to study this topic on a larger scale and to explore the potential benefit of altering management and improving patient care. One barrier to studying this topic on a larger scale is the infrequent occurrence of refractory hemodynamic instability in the perioperative period. As a result, it will be difficult to acquire a sufficient sample size and thus the power to measure such a treatment effect.
Regardless, the estimates provided in this systematic review should be invaluable for informing the expected baseline incidences and power calculations for future diagnostic studies using perioperative ultrasound. Given the preliminary state of the literature describing the types of observations and diagnoses found on perioperative ultrasound through TEE or TTE, this research serves as a preliminary attempt to clarify the relative incidences of each type of diagnosis. This research is intended to spur further research in the field in order to provide better information regarding expected incidences across populations as well as “priors” for future Bayesian analyses of the observed incidence of diagnoses. It is evident that, as new diagnostic technologies and techniques are introduced into practice, the expected incidences and range of diagnoses often remain unexplored territory, and clinicians are left to fend for themselves with regard to what is “expected” vs what is “unusual” for observed diagnoses. In order to provide better information to all areas of medicine where new diagnostic tools are introduced, investigators should be encouraged to clarify the expected incidence through descriptive research and the eventual culmination of this evidence through weighted meta-analysis.
In conclusion, this systematic review is a first step toward creating an evidence-based POCU curriculum for anesthesiology trainees. Future studies should be larger in scale and multicentred and should have focused outcomes in order to explore this topic in a more rigorous manner. This will ideally lead to the creation of a national or internationally recognized training program based on current evidence with ongoing refinement as new trials are published.
References
Shanewise JS, Cheung AT, Aronson S, et al. ASE/SCA guidelines for performing a comprehensive intraoperative multiplane transesophageal echocardiography examination: recommendations of the American Society of Echocardiography Council for Intraoperative Echocardiography and the Society of Cardiovascular Anesthesiologists Task Force for Certification in Perioperative Transesophageal Echocardiography. Anesth Analg 1999; 89: 870-84.
Royse CF, Canty DJ, Faris J, Haji DL, Veltman M, Royse A. Core review: physician-performed ultrasound: the time has come for routine use in acute care medicine. Anesth Analg 2012; 115: 1007-28.
Beaulieu Y. Bedside echocardiography in the assessment of the critically ill. Crit Care Med 2007; 35(5 Suppl): S235-49.
Scalea TM, Rodriguez A, Chiu WC, et al. Focused Assessment with Sonography for Trauma (FAST): results from an international consensus conference. J Trauma 1999; 46: 466-72.
Mayo PH, Beaulieu Y, Doelken P, et al. American College of Chest Physicians/La Societe de Reanimation de Langue Francaise statement on competence in critical care ultrasonography. Chest 2009; 135: 1050-60.
Expert Round Table on Ultrasound in ICU. International expert statement on training standards for critical care ultrasonography. Intensive Care Med 2011; 37: 1077-83.
Sutton AJ, Abrams KR, Jones DR, Sheldon TA, Song F. Methods for Meta-Analysis in Medical Research. Chichester: John Wiley; 2000 .
Bainbridge D, Martin J, Arango M, Cheng D, Evidence-based Peri-operative Clinical Outcomes Research (EPiCOR) Group. Perioperative and anaesthetic-related mortality in developed and developing countries: a systematic review and meta-analysis. Lancet 2012; 380: 1075-81.
Shillcutt SK, Markin NW, Montzingo CR, Brakke TR. Use of rapid “rescue” perioperative echocardiography to improve outcomes after hemodynamic instability in noncardiac surgical patients. J Cardiothorac Vasc Anesth 2012; 26: 362-70.
Canty DJ, Royse CF. Audit of anaesthetist-performed echocardiography on perioperative management decisions for non-cardiac surgery. Br J Anaesth 2009; 103: 352-8.
Canty DJ, Royse CF, Kilpatrick D, Williams DL, Royse AG. The impact of preoperative focused transthoracic echocardiography in emergency non-cardiac surgery patients with known or risk of cardiac disease. Anaesthesia 2012; 67: 714-20.
Cowie B. Three years’ experience of focused cardiovascular ultrasound in the peri-operative period. Anaesthesia 2011; 66: 268-73.
Cowie B. Focused cardiovascular ultrasound performed by anesthesiologists in the perioperative period: feasible and alters patient management. J Cardiothorac Vasc Anesth 2009; 23: 450-6.
Hofer CK, Zollinger A, Rak M, et al. Therapeutic impact of intraoperative transoesophageal echocardiography during noncardiac surgery. Anaesthesia 2004; 59: 3-9.
Lin T, Chen Y, Lu C, Wang M. Use of transoesophageal echocardiography during cardiac arrest in patients undergoing elective non-cardiac surgery. Br J Anaesth 2006; 96: 167-70.
Memtsoudis SG, Rosenberger P, Loffler M, et al. The usefulness of transesophageal echocardiography during intraoperative cardiac arrest in noncardiac surgery. Anesth Analg 2006; 102: 1653-7.
Schulmeyer C, Farias J, Rajdl E, de La Maza J, Labbe M. Utility of transesophageal echocardiography during severe hypotension in non-cardiac surgery (Portuguese). Rev Bras Anestesiol 2010; 60: 513-21.
Schulmeyer MC, Santelices E, Vega R, Schmied S. Impact of intraoperative transesophageal echocardiography during noncardiac surgery. J Cardiothorac Vasc Anesth 2006; 20: 768-71.
Suriani RJ, Neustein S, Shore-Lesserson L, Konstadt S. Intraoperative transesophageal echocardiography during noncardiac surgery. J Cardiothorac Vasc Anesth 1998; 12: 274-80.
Burrage PS, Shernan SK, Tsen LC, et al. Emergent transesophageal echocardiography in hemodynamically unstable obstetric patients. Int J Obstet Anesth 2015; 24: 131-6.
Markin NW, Gmelch BS, Griffee MJ, Holmberg TJ, Morgan DE, Zimmerman JM. A review of 364 perioperative rescue echocardiograms: findings of an anesthesiologist-staffed perioperative echocardiography service. J Cardiothoracic Vasc Anesth 2015; 29: 82-8.
Canty DJ, Royse CF, Kilpatrick D, Bowman L, Royse AG. The impact of focused transthoracic echocardiography in the preoperative clinic. Anaesthesia 2012; 67: 618-25.
Joseph MX, Disney PJ, Da Costa R, Hutchison SJ. Transthoracic echocardiography to identify or exclude cardiac cause of shock. Chest 2004; 126: 1592-7.
Jakobsen CJ, Torp P, Sloth E. Perioperative feasibility of imaging the heart and pleura in patients with aortic stenosis undergoing aortic valve replacement. Eur J Anaesthesiol 2007; 24: 589-95.
Bouhemad B, Zhang M, Lu Q, Rouby JJ. Clinical review: Bedside lung ultrasound in critical care practice. Crit Care 2007; 11: 205.
Funding
No funding was provided for this review.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
Amanda Jasudavisius, Daniel Bainbridge, and Ramiro Arellano were involved in the study design and data extraction. Amanda Jasudavisius, Daniel Bainbridge, Ramiro Arellano, and Janet Martin were involved in writing and revising the manuscript. Janet Martin was involved in the statistical analysis. Brie McConnell was involved in designing and conducting the literature search and reviewed the manuscript.
Rights and permissions
About this article
Cite this article
Jasudavisius, A., Arellano, R., Martin, J. et al. A systematic review of transthoracic and transesophageal echocardiography in non-cardiac surgery: implications for point-of-care ultrasound education in the operating room. Can J Anesth/J Can Anesth 63, 480–487 (2016). https://doi.org/10.1007/s12630-015-0524-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-015-0524-7